Abstract
Mumps virus (MuV) causes an acute infection in humans characterized by a wide array of symptoms ranging from relatively mild manifestations, such as parotitis, to more-severe complications, such as meningitis and encephalitis. Widespread mumps vaccination has reduced mumps incidence dramatically; however, outbreaks still occur in vaccinated populations. The V protein of MuV, when expressed in cell culture, blocks interferon (IFN) expression and signaling and interleukin-6 (IL-6) signaling. In this work, we generated a recombinant MuV incapable of expressing the V protein (rMuVΔV). The rescued MuV was derived from a clinical wild-type isolate from a recent outbreak in the United States (MuVIowa/US/06, G genotype). Analysis of the virus confirmed the roles of V protein in blocking IFN expression and signaling and IL-6 signaling. We also found that the rMuVIowa/US/06ΔV virus induced high levels of IL-6 expression in vitro, suggesting that V plays a role in reducing IL-6 expression. In vivo, the rMuVIowa/US/06ΔV virus was highly attenuated, indicating that the V protein plays an essential role in viral virulence.
INTRODUCTION
Mumps virus (MuV) is a paramyxovirus that causes acute inflammatory reactions in humans (2). MuV is highly neurotropic. Approximately half of all clinical cases have evidence of virus invasion of the central nervous system; aseptic meningitis occurs in approximately 10% of cases and encephalitis in less than 1% (2). Two-dose mumps vaccination programs have dramatically reduced disease incidence; however, large outbreaks still occur, even in vaccinated populations. While definitive causes for the outbreaks are unknown, waning immunity and antigenic differences between vaccine strains and circulating strains have been cited as likely factors (3, 15, 24, 34, 40, 42). The vaccine strain used in the United States and most of the Western Hemisphere is a genotype A virus, whereas recent outbreaks in these regions have invariably been identified as genotype G members (19, 20, 30, 41).
The RNA genome of MuV is 15,384 nucleotides long (2). It encodes nine known viral proteins. The V protein of MuV has 224 amino acid residues and contains a cysteine (Cys)-rich C terminus that is conserved among all paramyxoviruses. The V protein interrupts the interferon (IFN) signaling pathway through degradation of STAT1, a critical transcription factor for IFN-activated gene expression (10). A tryptophan-rich motif within the Cys-rich C terminus of the MuV V protein is essential in the ubiquitination and degradation of STAT1 (10, 11, 23) through the N-terminal region of STAT1 (44). The V protein has also been demonstrated to associate with receptor-activated C kinase (RACK1), which contains Trp-Asp (WD) repeats and mediates interactions between the IFN receptor and STAT1. The V-RACK1 interaction results in the disassociation of STAT1 and RACK1, contributing to the blockade of IFN signaling by V protein (10). This interaction may be important to block IFN signaling before the complete degradation of STAT1 occurs (12). The V protein of MuV also interacts with MDA5, a RNA helicase that plays a critical role in the activation of IFN expression in infected cells (1) and blocks the activation of IFN expression. The Cys-rich C terminus of V protein is essential for its interaction with MDA5 through its helicase C domain (25, 28). The V protein can serve as a substrate for inhibitor of κB kinase ε (IKKe)/tumor necrosis factor receptor-associated factor (TRAF) family member-associated NF-κB activator (TANK)-binding kinase 1 (TBK1), resulting in inhibition of the activation of interferon regulatory factor 3 (IRF3). The interaction between V protein and TBK1/IKKe inhibits the activation of IRF3, a critical transcription factor for IFN expression, resulting in the blockade of IFN expression (17). The V protein causes degradation of STAT3, a critical transcription factor for interleukin-6 (IL-6)-mediated signaling and oncogenesis (39). A point mutation within the V protein (E to D at position 95) results in a V protein that is capable of STAT1 degradation without affecting its ability to target STAT3 for degradation. The ability of V protein to block IFN signaling is thought to be important for viral pathogenesis (29). In this work, we have generated a recombinant MuV that it was no longer capable of expressing the V protein (rMuVIowa/US/06ΔV). The rescued MuV was derived from a clinical wild-type (WT) isolate from a recent outbreak in the United States (MuVIowa/US/06, G genotype). This is the first study of the functions of the V protein of MuV in the context of viral infection.
MATERIALS AND METHODS
Plasmids, viruses, and cells.
The MuV strain, MuVIowa/US/06, was obtained from a patient during the 2006 Midwest mumps outbreak in the United States. A full-length cDNA clone of the virus (pMuVIowa/US/06) was constructed as previously described (43). This plasmid was modified to not express the V protein by changing the editing site of the P/V gene (GGGGGG) to GAGGAGGG and the addition of another four base pairs (CTAG) to the 3′ untranslated region (3′UTR) of the gene to comply with “the rule of six” (9). Primer sequences, detailed cloning strategies, and entire cDNA sequences of MuVIowa/US/06 are available upon request.
To rescue an infectious virus, plasmid pMuVIowa/US/06ΔV (5 μg), along with plasmids pCAGGS-L (1 μg), pCAGGS-NP (1.5 μg), and pCAGGS-P (200 ng), were transfected into BSRT-7 cells. Three days later, transfected BSRT-7 cells were mixed with Vero cells at 1:1. Ten to 14 days later, when syncytium formation was observed, supernatants containing rMuVIowa/US/06ΔV were collected and plaque purified in Vero cells. Plaques (developing 4 to 7 days postinfection [dpi]) were amplified in Vero cells, and their genomes were sequenced. The rescue procedure was repeated to produce independent stocks of rMuVIowa/US/06ΔV.
Vero, HeLa, MDBK, and L929 cells were maintained in Dulbecco's modified Eagle medium (DMEM) with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin (P/S) (Mediatech Inc., Holu Hill, FL). BSRT-7 cells were maintained in DMEM supplemented with 10% FBS, 1% P/S, and 10% tryptose phosphate broth (TPB), plus 400 μg/ml Geneticin G418 antibiotic. Cells were cultured at 37°C with 5% CO2 and passaged the day before infection or transfection at appropriate dilution factors to achieve 80 to 90% confluence the next day. For virus infection, cells were inoculated with viruses in DMEM plus 1% bovine serum albumin (BSA) at a multiplicity of infection (MOI) of 0.01, 3, or 5 and incubated for 1 to 2 h at 37°C with 5% CO2. The inocula were then replaced with DMEM supplemented with 2% FBS and 1% P/S. Cells were transfected with plasmids using PLUS and Lipofectamine reagents (Invitrogen, Carlsbad, CA) following the manufacturer-provided protocols.
All mumps viruses were grown in Vero cells and were harvested at 4 to 7 dpi. Virus titers were measured in Vero cells by plaque assay as described previously (6, 8). Parainfluenza virus 5 (PIV5) and recombinant PIV5 lacking the expression of the C terminus of the V protein (rPIV5VΔC) were grown as described before (7).
Sequencing of viruses.
Viral RNA was extracted from cell culture supernatants by using the QIAamp viral RNA extraction minikit (Qiagen Inc., Valencia, CA) following manufacturer's protocol. Isolated viral RNA was reverse transcribed into cDNA by using SuperScript III reverse transcriptase with random hexamers (Invitrogen). Synthesized cDNA then served as templates for PCR using mumps virus genome-specific primers and Taq polymerase (Invitrogen). Fifteen sets of primers, each containing a forward and reverse primer, were designed to divide the genome into 15 overlapping fragments. The primers were then used for the subsequent sequencing of the PCR products (14). Leader and trailer sequences were sequenced following the standard protocol of rapid amplification of cDNA ends (RACE) (13). Primer sequences are available upon request.
Flow cytometry and TUNEL assay.
Flow cytometry was performed as previously described (36). HeLa or Vero cells in 6-well plates were mock infected or infected with rMuVIowa/US/06ΔV, rMuVIowa/US/06, or MuVIowa/US/06 at an MOI of 0.1 or 0.5. At 24 h postinfection (hpi), 48 hpi, 72 hpi, or 96 hpi, attached cells were trypsinized and combined with floating cells in the culture media. Cells were centrifuged and resuspended in 0.5% paraformaldehyde in phosphate-buffered saline (PBS) for 1 h at 4°C. The fixed cells were then washed with PBS and permeabilized in 50% fetal calf serum (FCS)-50% DMEM plus three volumes of 70% ethanol overnight. Permeabilized cells were subjected to either terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick end labeling (TUNEL) staining or MuVIowa/US/06-NP, MuVIowa/US/06-P, or MuVIowa/US/06-HN staining for protein expression level. For NP staining, monoclonal MuVIowa/US/06-NP antibody was diluted 1:200; for P staining, monoclonal MuVIowa/US/06-P antibody (43) was diluted 1:50 followed by fluorescein isothiocyanate (FITC) anti-mouse secondary antibody (Jackson ImmunoResearch) staining at a dilution of 1:10,000. For HN staining, polyclonal MuVIowa/US/06-HN was diluted 1:50 followed by FITC anti-rabbit secondary antibody staining at a dilution factor of 1:10,000. TUNEL staining was performed as described before following the manufacturer's protocol (Roche) (35, 37).
Immunoblotting.
Vero cells in 6-well plates at approximately 90% confluence were mock infected or infected with rMuVIowa/US/06 or rMuVIowa/US/06ΔV at an MOI of 0.01 or 0.5. Cells were lysed and collected at different time points postinfection in 0.5 ml WCEB buffer (50 mM Tris-HCl [pH 8.0], 120 mM NaCl, 0.5% NP-40, 0.00076% EGTA, 0.2 mM EDTA, 10% glycerol) with a mixture of protease inhibitors as described previously (31, 32). Cell lysates were briefly centrifuged to remove cell debris and loaded onto a 10% or 17.5% polyacrylamide gel and subjected to SDS-PAGE. Proteins were transferred to an Immobilon-FL transfer membrane (Millipore, Billerica, MA), incubated with primary antibody (anti-MuVIowa/US/06 V, 1:500; anti-MuVIowa/US/06 NP, 1:5,000; anti-MuVIowa/US/06 P, 1:2,000 [43], anti-STAT1, 1:200 [#B2410; Santa Cruz Biotechnology, Inc., Santa Cruz, CA[; anti-STAT2, 1:200 [#07-224]; Millipore, Billerica, MA]; anti-STAT3, 1:200 [#F300; Santa Cruz Biotechnology, Inc., Santa Cruz, CA]) and corresponding secondary antibodies conjugated to horseradish peroxidase, and detected using an Amersham ECL Western blotting detection kit (GE Healthcare Bioscience, Piscataway, NJ).
Growth curve of rMuVIowa/US/06ΔV and rMuVIowa/US/06.
Cells in 6-cm plates or 6-well plates were infected with rMuVΔV or rMuV at an MOI of 0.01. One milliliter (6-cm plates) or 100 μl (6-well plates) of supernatant were collected at 0 h, 24 h, 48 h, and 72 h (24 h, 48 h, 72 h, 120 h, 168 h, 216 h, and 264 h in HeLa) postinfection, supplemented with 1% BSA, and stored at −80°C. Virus titers were determined by plaque assay using Vero cells in 6-well plates in triplicate. After 1- to 2-h incubations with the viruses, the growth medium was changed to DMEM with 2% FBS, 1% P/S, and 1% low-melting-point agarose. Four to 7 dpi, 6-well plates of Vero cells were stained with Giemsa stain, and plaques were counted.
ELISA for IFN-β and IL-6.
HeLa cells or 293T cells were mock infected or infected with PIV5-WT (MOI 5), rPIV5-VΔC (MOI- 5), rMuVIowa/US/06 (MOI 0.5), or rMuVIowa/US/06ΔV (MOI 0.5) virus in 12-well plates. The supernatants were collected at 24 h and 48 h postinfection. The amount of secreted IL-6 in the medium was measured using the OptEIA human IL-6 enzyme-linked immunosorbent assay (ELISA) kit (BD Biosciences, San Jose, CA), and IFN-β was measured using the VeriKine human IFN-β ELISA kit as described before (16, 18) (PBL InterferonSource, Piscataway, NJ) according to the manufacturer's instructions.
Neurotoxicity test.
The neurovirulence phenotype of the rescued viruses was assessed by measuring the extent of MuV-induced hydrocephalus, the major neuropathologic outcome of MuV infection in rats, as previously described (32). Briefly, 3 litters of 8 to 10 newborn Lewis rats were inoculated intracerebrally with 10 μl of DMEM containing 100 PFU of each of the two virus stocks rescued from plasmid pMuVIowa/US/06 and each of the two virus stocks rescued from plasmid pMuVIowa/US/06ΔV. On day 30 postinoculation, the rats were humanely sacrificed by CO2 asphyxiation following the NIH Guidelines for the Care and Use of Laboratory Animals (22). Brains were removed and immersion fixed in 10% neutral-buffered formalin at 4°C for 4 to 5 days, followed by paraffin embedding. Sagittal sections obtained at a standard distance from either side of the rostral-caudal midline were stained with hematoxylin and eosin. The neurovirulence score was determined by calculating the ratio between the cross-sectional area of the brain (excluding the cerebellum) and the cross-sectional area of the lateral ventricle (which is enlarged following infection with neurovirulent MuV strains), measured using Image Pro Plus image analysis software (Media Cybernetics, Silver Spring, MD). The mean ratio (given in percent) of these two measurements on each of the two tissue sections per rat brain is the neurovirulence score for that particular brain. The neurovirulence score for each virus is the mean neurovirulence score for all brains within the treatment group. All comparisons were made using a t test or, with nonnormal data (failed Shapiro-Wilk test), the Mann-Whitney rank sum test (α = 0.05).
RESULTS
Recovery of a recombinant MuV lacking expression of V protein (rMuVΔV).
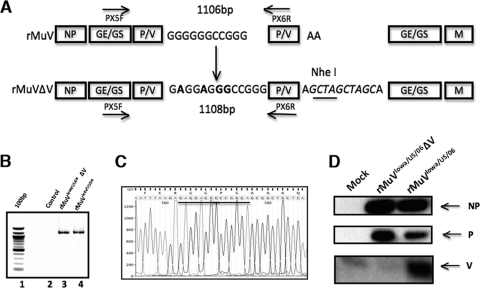
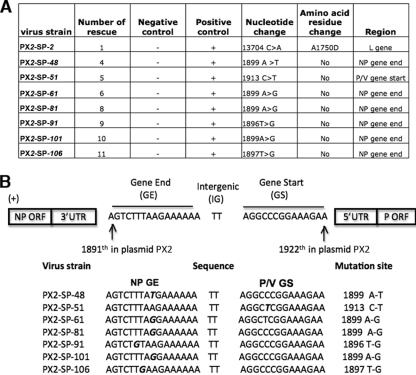
To investigate the role of the V protein in viral pathogenesis in the context of viral infection, we constructed a cDNA of the MuVIowa/US/06 genome containing mutations to ablate the V protein expression (pMuVIowa/US/06ΔV) (the accession number for MuVIowa/US/06 genome is JN012242) (43). Ablation of the V protein expression from the genome was achieved by changing the editing site (GGGGGG) in the P/V gene into GAGGAGGG. Therefore, only a transcript encoding the P protein is generated from P/V gene transcription (Fig. 1A). Infectious viruses abolishing the expression of the V protein (rMuVIowa/US/06ΔV) were rescued from the cloned DNA through transfection of pMuVIowa/US/06ΔV into BSRT-7 cells. Rescued viruses were further plaque purified and amplified in Vero cells. To confirm the presence of the genetic changes to shut off the V protein expression in the rescued virus genome, viral RNAs were extracted from virus stocks and reverse transcribed into cDNA for sequencing (Fig. 1B and C). Sequencing of the genome of the rescued virus revealed the presence of nucleotide substitutions in the NP gene end (GE) sequence and at the P/V gene start (GS) sequence comparing to input cDNA sequence as well as the changes that would ablate the expression of the V protein (Fig. 1C). We performed immunoblotting of infected cells to confirm the absence of the V protein expression in rMuVIowa/US/06ΔV-infected Vero cells (Fig. 1D). To further investigate, we rescued the virus from the cDNA plasmid seven more times (Fig. 2A). Viruses from seven out of the total eight rescued viruses contained a point mutation at either the NP GE (six) or P/V GS region (one), while one contained a point mutation in the L gene (Fig. 2B). All of the rescued rMuVIowa/US/06ΔV viruses contained at least one point mutation in their genome, and the most frequent point mutation was at position 1899 in the genome; thus, this virus was used as a representative virus and designated as rMuVIowa/US/06ΔV for this work, unless otherwise noted.
Fig 1.
Generation of a MuVIowa/US/06 lacking V protein (rMuVIowa/US/06ΔV). (A) Schematic of rMuVIowa/US/06ΔV. The GGGGGG editing site in the P/V gene of MuVIowa/US/06 was changed to GAGGAGGG to eliminate expression of the V protein. To maintain the genome length of rMuVIowa/US/06ΔV to be a multiple of six, 4 bp was added to the P/V gene 3′ UTR. (B) Confirmation of the rescue of rMuVIowa/US/06ΔV. Viral RNAs extracted from rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected cells were reverse transcribed into cDNA, followed by reverse transcription (RT)-PCR using two primers flanking the P/V gene. Lanes: 1, 100-bp DNA ladder; 2, negative control (PCR without polymerase); 3 and 4, PCR products from rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected cells, respectively. (C) Confirmation of rMuVIowa/US/06ΔV. PCR products shown in Fig. 1B were sequenced. (D) Expression of the V protein in rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected cells. Vero cells were mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06. Cell lysates were immunoblotted using anti-NP, -P, or -V.
Fig 2.
Whole-genome sequencing of rescued rMuVIowa/US/06ΔV. (A) Summary of changes found in rescued rMuVIowa/US/06ΔV. The leftmost panel shows the names of individual rMuVIowa/US/06ΔV strains from 8 successful virus rescues. (B) A schematic of the changes that occurred in the NP GE and P/V GS regions. Changes that occurred during virus rescue of rMuVIowa/US/06ΔV are indicated as bold, italic letters. The “TT” in the middle of the sequence alignment is the gene junction sequence between the NP and P/V genes in MuVIowa/US/06.
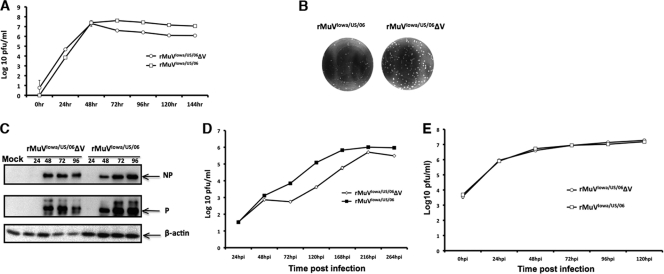
Analysis of rMuVΔV in tissue culture cell lines.
To analyze the growth rate of rMuVIowa/US/06ΔV in cell lines, Vero cells or HeLa cells were infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.01, medium was collected at multiple time points postinfection, and viral titers were determined using plaque assay (Fig. 3A). rMuVIowa/US/06ΔV grew at a rate comparable to that of rMuIowa/US/06V in Vero cells during the first 48 h postinfection (hpi), and then the growth of rMuVIowa/US/06ΔV decreased and remained approximately 1 log lower in titer than rMuVIowa/US/06 throughout the studied time course (Fig. 3A). Plaque size of rMuVIowa/US/06ΔV in Vero cells showed no significant differences from that of rMuVIowa/US/06 (Fig. 3B). Protein expression levels of rMuVIowa/US/06ΔV or rMuVIowa/US/06 low-MOI-infected Vero cells were examined by immunoblotting with anti-NP, P, and V or anti-β-actin (Fig. 3C). Consistent with the time course, the viral protein expression levels of rMuVIowa/US/06ΔV were similar to those of rMuVIowa/US/06 at 48, 72, and 96 hpi (adjusting for the levels of β-actin). In HeLa cells, the growth of rMuVIowa/US/06ΔV was reduced (Fig. 3D). The absence of a functional V protein reduced the virus titer of rMuVIowa/US/06ΔV by almost 2 log10 from 72 hpi to 168 hpi compared with rMuVIowa/US/06. Nevertheless, the both viruses reached similar titers at later time points.
Fig 3.
Growth rates and viral protein expression of rMuVIowa/US/06ΔV, rMuVIowa/US/06, and MuVIowa/US/06. (A) Growth rates of rMuVIowa/US/06ΔV and rMuVIowa/US/06 in Vero cells. Vero cells were mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.01. Supernatants were collected for plaque assay. (B) Plaques of rMuVIowa/US/06ΔV and rMuVIowa/US/06 in Vero cells. rMuVIowa/US/06ΔV or rMuVIowa/US/06 was plated onto Vero cells. The plaques were stained with Giemsa at 6 dpi. (C) Viral protein expression of rMuVIowa/US/06ΔV and rMuVIowa/US/06 in Vero cells. Vero cells were infected as in panel A. Viral protein levels were examined by immunoblotting with anti-NP and P. β-Actin was used as a loading control. (D) Growth rates of rMuVIowa/US/06ΔV and rMuVIowa/US/06 in HeLa cells. HeLa cells were infected as in panel A. (E) Growth rates of rMuVIowa/US/06ΔV and rMuVIowa/US/06 in 293T cells. 293T cells were mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.5. Supernatants were collected for plaque assay.
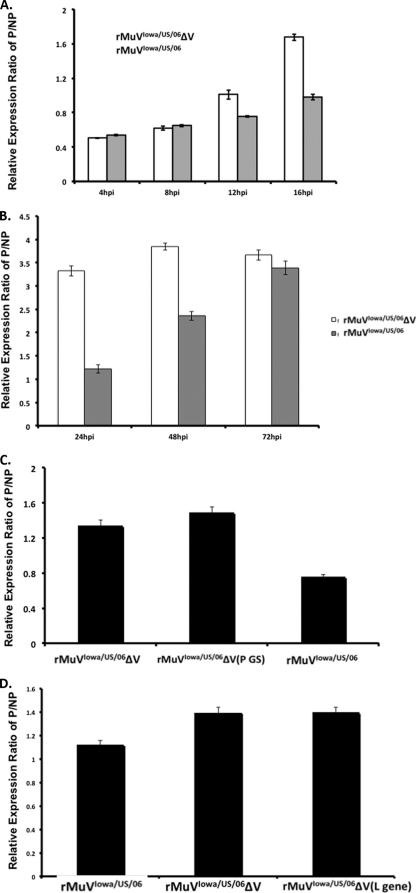
Expression of viral genes in rMuVIowa/US/06ΔV-infected cells.
Mutations at either the NP GE or P/V GS in recovered rMuVIowa/US/06ΔV viruses suggested that a modulation of viral protein expression levels between NP and P might be critical for the recovery of rMuVIowa/US/06ΔV from cDNA. To investigate the viral protein expression pattern in rMuVIowa/US/06ΔV, Vero cells infected with a high MOI were stained for NP and P proteins at different time points postinfection and assessed by flow cytometry (Fig. 4). To quantify the possible changes in the NP and P expression pattern, P protein expression levels were normalized to that of the corresponding NP levels (Fig. 4A and B). The P/NP ratio of rMuVΔV was significantly higher than that of rMuV at 12, 16, 24, and 48 hpi, indicating an elevated P protein expression in the rMuVIowa/US/06ΔV virus. This difference was no longer evident by 72 hpi.
Fig 4.
Ratios of NP and P in rMuVIowa/US/06ΔV-infected cells. (A) NP and P expression levels in rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected Vero cells during early time points postinfection. Vero cells were mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.5. Vero cells were collected and examined for NP and P expression using flow cytometry. Ratios of mean fluorescence intensity (MFI) of P over NP are shown. P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV at 12 and 16 hpi were calculated using Student's t test and are less than 0.05. (B) NP and P expression levels in rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected Vero cells during late time points postinfection. Ratios of MFI of P over NP at multiple time points postinfection were examined as in panel A. P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV at 24 and 48 hpi are less than 0.05. (C) NP and P expression ratios of rMuVIowa/US/06ΔV (P GS). Ratios of MFI of P over NP in rMuVIowa/US/06ΔV (P GS)-infected Vero cells, at an MOI of 0.5, were examined at 24 hpi. P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV (P GS) are less than 0.05. (D) NP and P expression ratio of rMuVIowa/US/06ΔV (L gene). Ratios of MFI of P over NP in rMuVIowa/US/06ΔV (L gene)-infected Vero cells, at an MOI of 0.5, were examined at 24 hpi. P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV (L gene) are less than 0.05.
To investigate if this altered NP and P expression pattern was unique for this rMuVIowa/US/06ΔV strain, an rMuVIowa/US/06ΔV containing a P GS mutation (rMuVIowa/US/06ΔV [P GS]) and an rMuVIowa/US/06ΔV containing a L open reading frame (ORF) mutation (rMuVIowa/US/06ΔV [L gene]) were also examined (Fig. 4C and D). Similar to rMuVIowa/US/06ΔV, both rMuVIowa/US/06ΔV (P GS) and rMuVIowa/US/06ΔV (L gene) had a P protein expression level greater than that of rMuVIowa/US/06, suggesting that this altered NP and P expression pattern was typical for the recovered rMuVIowa/US/06ΔV viruses.
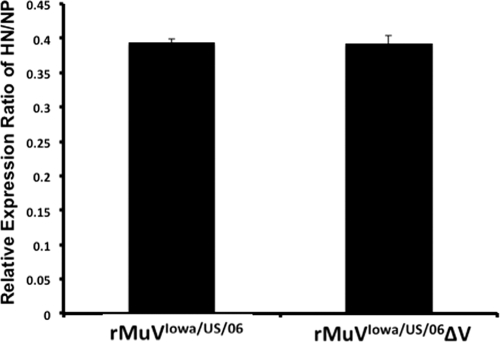
To examine if downstream viral protein expression was affected by either deletion of the V protein or the point mutation in NP GE, HN expression levels were examined using flow cytometry. Vero cells were either mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.5, and then cells were collected at 24 hpi and subjected to NP and HN staining (Fig. 5). No significant changes in the HN-to-NP ratio were observed.
Fig 5.
HN expression level in rMuVIowa/US/06ΔV. Vero cells were mock infected or infected with rMuVΔV or rMuV at an MOI of 0.5. Cells were collected at 24 hpi and stained for HN using flow cytometry.
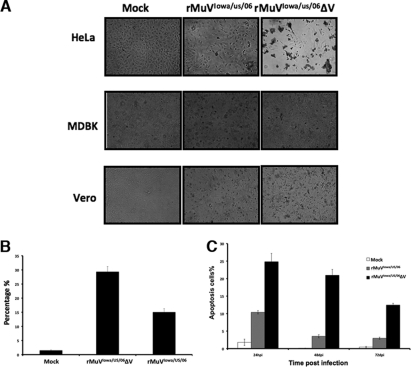
rMuVIowa/US/06ΔV-induced accelerated CPE in tissue culture cell lines.
We compared rMuVIowa/US/06ΔV-induced cytopathic effects (CPE) in three different cell culture lines from three different organisms. HeLa (human), Vero (monkey), and MDBK (bovine) cells were infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.5, and the cells were photographed at 72 hpi. rMuVIowa/US/06ΔV caused the most-severe CPE in HeLa cells. We observed more and larger syncytia in rMuVIowa/US/06ΔV-infected HeLa cells, which may be a major contributing factor to cell death (Fig. 6A). To examine whether the cell death was caused by apoptosis, the TUNEL assay was performed (Fig. 6B). HeLa cells infected with rMuVIowa/US/06ΔV at an MOI of 0.5 showed at least a 2-fold higher level of apoptosis than cells infected with rMuV. Similarly, rMuVIowa/US/06ΔV induced a higher level of apoptosis in Vero cells (Fig. 6C). That the lack of V led to an increase in apoptosis in infected cells suggests that the V protein might play a role in blocking induction of apoptosis in infected cells.
Fig 6.
Induction of cell death by rMuVIowa/US/06ΔV. (A) rMuVIowa/US/06ΔV induced a greater cytopathic effect in cell lines. HeLa cells, MDBK cells, or Vero cells were mock infected or infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 at an MOI of 0.5 and photographed at 72 hpi. (B) Induction of apoptosis by rMuVΔV in HeLa cells. HeLa cells were infected as in panel A. At 24 hpi, cells were collected for TUNEL assay. Percentages of TUNEL-positive cells out of total cells are shown. The P value of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV is less than 0.05. (C). Induction of apoptosis in Vero cells. The Vero cells were infected with 0.5 MOI of viruses and processed for TUNEL assay as in panel B. P values between the wild type and rMuVIowa/US/06ΔV are less than 0.05.
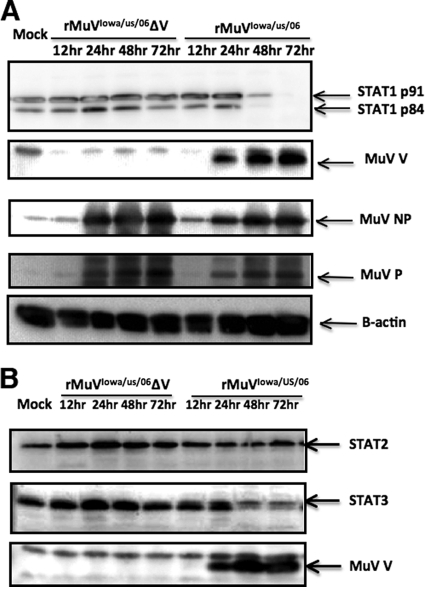
Status of STAT proteins in MuVIowa/US/06-infected cells.
Previous studies have shown that the V protein is involved in blocking the IFN signaling pathway by targeting STAT proteins for degradation. To determine whether MuVIowa/US/06 V protein is the only virus-encoding antagonist of the IFN pathway, we examined the STAT family protein levels in Vero cells infected with rMuVIowa/US/06ΔV or rMuVIowa/US/06 (Fig. 7A and B). Consistent with previous in vitro transfection studies, STAT1 and STAT3, but not STAT2, were completely degraded in rMuVIowa/US/06-infected Vero cells, while rMuVIowa/US/06ΔV, which lacks expression of the V protein, failed to target any STAT proteins for degradation, indicating that the V protein might be essential and necessary for STAT protein degradation by MuVIowa/US/06. There is a time lag between the occurrence of a detectable V protein and the degradation of STAT protein (Fig. 7A and B), implying that the degradation of STATs might require accumulation of the V protein.
Fig 7.
Degradation of STAT1 and STAT3 in MuVIowa/US/06-infected cells. (A) rMuVIowa/US/06ΔV failed to degrade STAT1 in Vero cells. Vero cells were infected at an MOI of 0.5. Cell lysates were immunoblotted with anti-NP, -P, -V, and anti-STAT1 recognizing both STAT1 isoforms (STAT1α and STAT1β). β-Actin was used as a loading control. (B) rMuVIowa/US/06ΔV failed to degrade STAT3 in Vero cells. Cell lysates were immunoblotted with anti-NP, -P, -V, -STAT3, and -STAT2.
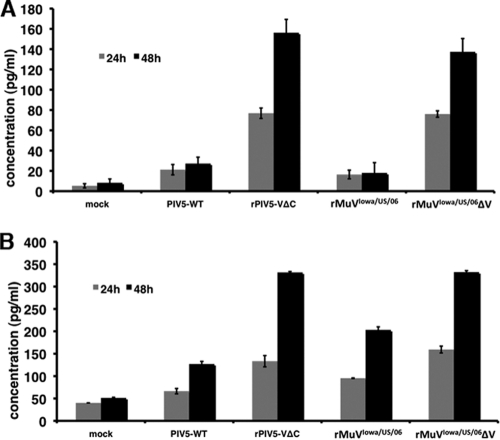
PIV5, a paramyxovirus closely related to MuV, prevents induction of IFN-β in infected cells, while recombinant PIV5 lacking the expression of the conserved C terminus of the V protein does not (7, 27). To compare IFN-β inductions by rMuVIowa/US/06ΔV and rMuVIowa/US/06, we measured IFN-β concentration in the medium of infected 293T cells by using ELISA. At 48 hpi, rMuVIowa/US/06ΔV induced IFN-β production higher than that induced by rMuVIowa/US/06 (Fig. 8A), indicating that the V protein of MuVIowa/US/06 plays a role in limiting IFN- β expression.
Fig 8.
Induction of IFN-β and IL-6 by rMuVIowa/US/06ΔV. (A) Induction of IFN-β production by rMuVIowa/US/06ΔV virus. 293T cells were infected with wild-type PIV5, rPIV5VΔC, rMuVIowa/US/06, or rMuVIowa/US/06ΔV or mock infected. The cellular supernatants were collected at 24 and 48 hpi and analyzed for IFN-β production by ELISA. The graph shows the average of three independent experiments, and error bars represent the standard deviation (SD). P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV at 24 and 48 hpi are less than 0.05. (B) Induction of IL-6 production by rMuVIowa/US/06ΔV virus. HeLa cells were infected with wild-type PIV5, rPIV5VΔC, rMuVIowa/US/06, or rMuVIowa/US/06ΔV or mock infected. The cellular supernatants were collected at 24 and 48 hpi and analyzed for IL-6 production by ELISA. The test samples were diluted to 1:10 in a sample diluent provided in the kit. The graph shows the average of two independent experiments, and error bars represent the SD. P values of rMuVIowa/US/06 versus rMuVIowa/US/06ΔV at 24 and 48 hpi are less than 0.05.
rMuVIowa/US/06ΔV led to a higher level of IL-6 induction.
To investigate whether the absence of a functional V protein in MuVIowa/US/06 infection would lead to induction of other cytokines, IL-6 production levels in the medium of rMuVIowa/US/06ΔV- and rMuVIowa/US/06-infected cells were examined. At 48 hpi, rMuVIowa/US/06ΔV led to a higher level of IL-6 production than rMuVIowa/US/06 in HeLa cells (Fig. 8B), indicating that IL-6 induction was reduced by the presence of the V protein. Intriguingly, rMuVIowa/US/06 infection also induced a significant amount of IL-6 production. This is consistent with MuV being an inflammatory disease.
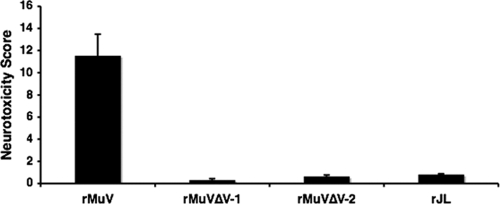
Neurotoxicity of rMuVIowa/US/06ΔV.
To examine the effect of the V protein on virus neurovirulence, viruses from two independent rescues using plasmid pMuVIowa/US/06ΔV (rMuVIowa/US/06ΔV) (Fig. 2A) were tested in rats, along with rMuVIowa/US/06 and the highly attenuated Jeryl Lynn (JL) vaccine virus as controls. As shown in Fig. 9, the ΔV viruses were highly attenuated compared to rMuVIowa/US/06 and JL vaccine virus.
Fig 9.
Neurotoxicity of rMuVIowa/US/06ΔV in vivo. The severity of hydrocephalus in rats inoculated with rMuVIowa/US/06 or rMuVIowa/US/06ΔV (rMuVΔV-1 is rMuVIowa/US/06 ΔV rescue #4, PX2-SP-48, and rMuVΔV-2 is rMuVIowa/US/06 ΔV rescue #5, PX2-SP-51) (Fig. 2) was measured as described in Materials and Methods. P values of rMuV versus rMuVΔV-1 or rMuVΔV-2 are less than 0.05. The P value of rJL versus rMuVΔV-1 is less than 0.05. n = 36 for MuV, n = 16 for rMuVΔV-1, and n = 18 for rMuVΔV-2.
DISCUSSION
The roles of V protein in blocking IFN expression and signaling have been reported previously. Our results confirm these findings through the study of a recombinant virus derived from a clinical isolate (genotype G) ablating the expression the V protein in the context of in vitro infection. We have found that the lack of V protein expression also led to the induction of a higher level of IL-6, a proinflammatory cytokine, suggesting that the V protein plays a role in suppressing IL-6 expression. We speculate that the lack of V protein expression in infected cells resulted in the attenuation of this strain in an animal model, suggesting that the V protein plays an essential role in viral virulence. It is possible that the inability of rMuVIowa/US/06ΔV to counter IFN action limited the replication of the virus in vivo, and the induction of a higher level of IL-6 by rMuVIowa/US/06ΔV attracted monocytes to clear the infection quickly, resulting in the attenuation of rMuVIowa/US/06ΔV in vivo.
Genetically, the closest virus to MuV is parainfluenza virus 5 (PIV5). The V proteins of MuV and PIV5 share many identical functions, including blocking IFN expression through MDA5, blocking IFN signaling through degradation of STAT1, and inhibiting expression of IL-6 in virus-infected cells. Interestingly, a recombinant PIV5 lacking the entire V protein has never been obtained in tissue culture cells, suggesting that the V protein of PIV5 plays a more critical role in virus replication (5, 7) than the V protein does for MuV. The viability of rMuVIowa/US/06ΔV suggests that the role of MuVIowa/US/06 V protein in virus replication is dispensable, at least in tissue culture cells.
The most widely used mumps vaccine, Jeryl Lynn (JL) vaccine, was introduced in the United States in 1967 and shortly thereafter globally. The effectiveness of the vaccine has been estimated at 80% for one dose and 90% for two doses (4). Vaccine effectiveness has been found to be similar for other strains (4), but unlike the JL strain, nearly all other strains have been associated with aseptic meningitis (31) and thus are not widely used. Recent outbreaks of mumps in vaccinated populations have highlighted the relatively lower effectiveness of mumps vaccines as compared to other vaccines, such as measles, and have stimulated interest in development of new mumps vaccines. For instance, In the 2009-2010 mumps outbreak in the state of New York and the state of New Jersey in the United States, 88% of the patients had one dose of mumps vaccine and 75% of the patients had two doses of vaccine (21). All live attenuated MuV vaccines are obtained through serial passages of virus in embryonic eggs and/or cells. This is a time-consuming process and a strategy with a poor record of generating safe vaccines with the exception of JL vaccine.
In this work, using a reverse genetics system for MuV based on a clinical isolate from a recent outbreak, we have generated a recombinant virus incapable of producing the V protein (rMuVIowa/US/06ΔV). We have found that this virus grew to titers similar to those for wild-type virus in Vero cells, a cell line that is used for vaccine production, as well as in other cell types. Most importantly, the virus exhibited low neurotoxicity in rats, suggesting that it may be a possible vaccine candidate. Further examination of the immunogenicity and safety of the virus in vivo will be needed to determine the suitability of this virus as a vaccine candidate.
The V/P gene of MuV encodes three proteins, V, I, and P, through a process of “RNA editing,” in which nontemplate G residues are inserted into mRNA during transcription at a specific site to generate mRNAs that can be translated into three different ORFs (33). The V protein is translated from the “unedited” copy of mRNA, P from the mRNA with two G residue insertions, and the I protein from the mRNA with one or four G residue insertions. All of these proteins have identical N termini of 155 amino acid residues. The P protein has 391 amino acid residues and plays an essential role in viral RNA synthesis. The I protein has 170 amino acid residues, and its function is unclear. It is possible that the I mRNA is a by-product of RNA editing and it may not have any significant functions. The strategy we used to generate rMuVIowa/US/06ΔV also eliminated expression of the I protein. Because the mRNA for I counts only for less than 2% of total V, I, and P transcripts, and its sequence is very similar to the N termini of V and P (I has about 170 amino acid residues and 155 of them are identical to the N termini of V and P) (26, 38), we attribute the phenotypes of rMuVIowa/US/06ΔV to the lack of V protein. However, we cannot exclude the possibility that the I protein is also responsible.
All changes except the one in the L gene occurred in the gene junction between NP and P/P genes to generate viable infectious MuV incapable of expressing the V protein. It is interesting that a mutation in the L gene was able to allow the rescue of a virus lacking the V protein. While we cannot exclude the possibility that the mutation in the L gene occurred fortuitously and is immaterial to the function of L, we speculate that the particular mutation may play a role in modulating interactions between NP-P and L, considering that all other viruses rescued had mutations to modulate the levels of NP and P. Further analysis of the virus may lead to a better understanding of the function of L.
ACKNOWLEDGMENTS
We appreciate the comments, suggestions, and technical help from members of the He lab. We are thankful to Anthony Schmitt for the anti-HN antibodies. We are grateful to Kaori Sakamoto for carefully reading the manuscript prior to submission.
This work has been supported by grants from NIH (K02 065795) and National Natural Science Foundation of China Funds for Distinguished Young Scholar—B Plan (No. 30928001 to B.H. and J.W.)
Footnotes
Published ahead of print 16 November 2011
REFERENCES
- 1. Andrejeva J, et al. 2004. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-{beta} promoter. Proc. Natl. Acad. Sci. U. S. A. 101:17264–17269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carbone KM, Wolinsky JS. 2001. Mumps virus, p 1381–1400. In Knipe DM, Howley PM. (ed), Fields virology, 4th ed, vol 1 Lippincott Williams and Wilkins, Philadelphia, PA [Google Scholar]
- 3. Crowley B, Afzal MA. 2002. Mumps virus reinfection–clinical findings and serological vagaries. Commun. Dis. Public Health 5:311–313 [PubMed] [Google Scholar]
- 4. Dayan GH, Rubin S. 2008. Mumps outbreaks in vaccinated populations: are available mumps vaccines effective enough to prevent outbreaks? Clin. Infect. Dis. 47:1458–1467 [DOI] [PubMed] [Google Scholar]
- 5. Dillon PJ, Parks GD. 2007. Role for the phosphoprotein P subunit of the paramyxovirus polymerase in limiting induction of host cell antiviral responses. J. Virol. 81:11116–11127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. He B, Lamb RA. 1999. Effect of inserting paramyxovirus simian virus 5 gene junctions at the HN/L gene junction: analysis of accumulation of mRNAs transcribed from rescued viable viruses. J. Virol. 73:6228–6234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. He B, et al. 2002. Recovery of paramyxovirus simian virus 5 with a V protein lacking the conserved cysteine-rich domain: the multifunctional V protein blocks both interferon-beta induction and interferon signaling. Virology 303:15–32 [DOI] [PubMed] [Google Scholar]
- 8. He B, Paterson RG, Ward CD, Lamb RA. 1997. Recovery of infectious SV5 from cloned DNA and expression of a foreign gene. Virology 237:249–260 [DOI] [PubMed] [Google Scholar]
- 9. Kolakofsky D, et al. 1998. Paramyxovirus RNA synthesis and the requirement for hexamer genome length: the rule of six revisited. J. Virol. 72:891–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kubota T, Yokosawa N, Yokota S, Fujii N. 2002. Association of mumps virus V protein with RACK1 results in dissociation of STAT-1 from the alpha interferon receptor complex. J. Virol. 76:12676–12682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kubota T, Yokosawa N, Yokota S, Fujii N. 2001. C terminal CYS-RICH region of mumps virus structural V protein correlates with block of interferon alpha and gamma signal transduction pathway through decrease of STAT 1-alpha. Biochem. Biophys. Res. Commun. 283:255–259 [DOI] [PubMed] [Google Scholar]
- 12. Kubota T, et al. 2005. Mumps virus V protein antagonizes interferon without the complete degradation of STAT1. J. Virol. 79:4451–4459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li Z, et al. 2011. Function of the small hydrophobic protein of J paramyxovirus. J. Virol. 85:32–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Z, et al. 2006. Beilong virus, a novel paramyxovirus with the largest genome of non-segmented negative-stranded RNA viruses. Virology 346:219–228 [DOI] [PubMed] [Google Scholar]
- 15. Lim CS, Chan KP, Goh KT, Chow VT. 2003. Hemagglutinin-neuraminidase sequence and phylogenetic analyses of mumps virus isolates from a vaccinated population in Singapore. J. Med. Virol. 70:287–292 [DOI] [PubMed] [Google Scholar]
- 16. Lin Y, et al. 2007. Inhibition of interleukin-6 expression by the V protein of parainfluenza virus 5. Virology 368:262–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lu LL, Puri M, Horvath CM, Sen GC. 2008. Select paramyxoviral V proteins inhibit IRF3 activation by acting as alternative substrates for inhibitor of kappaB kinase epsilon (IKKe)/TBK1. J. Biol. Chem. 283:14269–14276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Luthra P, Sun D, Silverman RH, He B. 2011. Activation of IFN-beta expression by a viral mRNA through RNase L and MDA5. Proc. Natl. Acad. Sci. U. S. A. 108:2118–2123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marin M, et al. 2008. Mumps vaccination coverage and vaccine effectiveness in a large outbreak among college students–Iowa, 2006. Vaccine 26:3601–3607 [DOI] [PubMed] [Google Scholar]
- 20. MMWR 2006. Mumps epidemic–United Kingdom, 2004–2005. MMWR Morb. Mortal. Wkly. Rep. 55:173–175 [PubMed] [Google Scholar]
- 21. MMWR 2010. Update: mumps outbreak - New York and New Jersey, June 2009-January 2010. MMWR Morb. Mortal. Wkly. Rep. 59:125–129 [PubMed] [Google Scholar]
- 22. National Research Council 2011. Guide for the care and use of laboratory animals, 8th ed National Academics Press, Washington, DC [Google Scholar]
- 23. Nishio M, Garcin D, Simonet V, Kolakofsky D. 2002. The carboxyl segment of the mumps virus v protein associates with stat proteins in vitro via a tryptophan-rich motif. Virology 300:92. [DOI] [PubMed] [Google Scholar]
- 24. Otto W, et al. 2010. Ongoing outbreak of mumps affecting adolescents and young adults in Bavaria, Germany, August to October 2010. Euro Surveill. 15(50):pii=19748 [PubMed] [Google Scholar]
- 25. Parisien JP, et al. 2009. A shared interface mediates paramyxovirus interference with antiviral RNA helicases MDA5 and LGP2. J. Virol. 83:7252–7260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Paterson RG, Lamb RA. 1990. RNA editing by G-nucleotide insertion in mumps virus P-gene mRNA transcripts. J. Virol. 64:4137–4145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poole E, He B, Lamb RA, Randall RE, Goodbourn S. 2002. The V proteins of simian virus 5 and other paramyxoviruses inhibit induction of interferon-beta. Virology 303:33–46 [DOI] [PubMed] [Google Scholar]
- 28. Ramachandran A, Horvath CM. 2010. Dissociation of paramyxovirus interferon evasion activities: universal and virus-specific requirements for conserved V protein amino acids in MDA5 interference. J. Virol. 84:11152–11163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rosas-Murrieta NH, Herrera-Camacho I, Palma-Ocampo H, Santos-Lopez G, Reyes-Leyva J. 2010. Interaction of mumps virus V protein variants with STAT1-STAT2 heterodimer: experimental and theoretical studies. Virol. J. 7:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rota JS, et al. 2009. Investigation of a mumps outbreak among university students with two measles-mumps-rubella (MMR) vaccinations, Virginia, September-December 2006. J. Med. Virol. 81:1819–1825 [DOI] [PubMed] [Google Scholar]
- 31. Rubin SA, Afzal MA. 2011. Neurovirulence safety testing of mumps vaccines–historical perspective and current status. Vaccine 29:2850–2855 [DOI] [PubMed] [Google Scholar]
- 32. Rubin SA, et al. 2000. Evaluation of a neonatal rat model for prediction of mumps virus neurovirulence in humans. J. Virol. 74:5382–5384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saito H, et al. 1996. Isolation and characterization of mumps virus strains in a mumps outbreak with a high incidence of aseptic meningitis. Microbiol. Immunol. 40:271–275 [DOI] [PubMed] [Google Scholar]
- 34. Strohle A, Bernasconi C, Germann D. 1996. A new mumps virus lineage found in the 1995 mumps outbreak in western Switzerland identified by nucleotide sequence analysis of the SH gene. Arch. Virol. 141:733–741 [DOI] [PubMed] [Google Scholar]
- 35. Sun D, Luthra P, Li Z, He B. 2009. PLK1 down-regulates parainfluenza virus 5 gene expression. PLoS Pathog. 5:e1000525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sun D, Luthra P, Xu P, Yoon H, He B. 2011. Identification of a phosphorylation site within the P protein important for mRNA transcription and growth of parainfluenza virus 5. J. Virol. 85:8376–8385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sun M, et al. 2004. Conserved cysteine-rich domain of paramyxovirus simian virus 5 V protein plays an important role in blocking apoptosis. J. Virol. 78:5068–5078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Takeuchi K, et al. 1990. Detection and characterization of mumps virus V protein. Virology 178:247–253 [DOI] [PubMed] [Google Scholar]
- 39. Ulane CM, Rodriguez JJ, Parisien JP, Horvath CM. 2003. STAT3 ubiquitylation and degradation by mumps virus suppress cytokine and oncogene signaling. J. Virol. 77:6385–6393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Utz S, et al. 2004. Phylogenetic analysis of clinical mumps virus isolates from vaccinated and non-vaccinated patients with mumps during an outbreak, Switzerland 1998–2000. J. Med. Virol. 73:91–96 [DOI] [PubMed] [Google Scholar]
- 41. Watson-Creed G, et al. 2006. Two successive outbreaks of mumps in Nova Scotia among vaccinated adolescents and young adults. CMAJ 175:483–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Whelan J, et al. 2010. Ongoing mumps outbreak in a student population with high vaccination coverage, Netherlands, Euro Surveill. 15(17):pii=19554 [DOI] [PubMed] [Google Scholar]
- 43. Xu P, et al. 2011. Rescue of wild-type mumps virus from a strain associated with recent outbreaks helps to define the role of the SH ORF in the pathogenesis of mumps virus. Virology 417:126–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yokosawa N, Yokota S, Kubota T, Fujii N. 2002. C-terminal region of STAT-1alpha is not necessary for its ubiquitination and degradation caused by mumps virus V protein. J. Virol. 76:12683–12690 [DOI] [PMC free article] [PubMed] [Google Scholar]