Abstract
Recent reports of increasing suicide rates among military personnel indicate a need for increased work in understanding processes relevant to suicide risk in the military. Anxiety, along with anxiety-related risk factors have been implicated in suicidality as well as posttraumatic stress disorder (PTSD). One such risk factor, anxiety sensitivity (AS), refers to fear of anxiety-related symptoms. Subfactors of AS, notably the physical and cognitive concerns factors, appear to be relevant to the construct of acquired capability for suicidal behavior, a risk factor for death by suicide postulated by the Interpersonal-Psychological Theory of Suicide (Joiner, 2005; Van Orden et al., 2010). Study 1 examined the interaction of AS-cognitive concerns and AS-physical concerns in an outpatient sample with PTSD symptomatology (N = 128). Analyses were consistent with our a priori model and indicated that the interaction of AS-cognitive concerns by AS-physical concerns predicted previous suicide attempt. Specifically, those with high AS-cognitive concerns and low AS-physical concerns were at increased risk for suicide attempt. Study 2 prospectively examined the associations between AS and suicidal ideation in a sample of military cadets undergoing basic training (N = 1,081). A similar interaction emerged such that high AS-cognitive and low AS-physical scores at Time 1 significantly predicted suicidal ideation several months later, even after controlling for Time 1 suicidal ideation and psychopathology. These findings suggest that suicide potential may be related to interactions between cognitive risk factors for anxiety among individuals with PTSD symptomatology as well as individuals experiencing stressful life events.
Keywords: anxiety sensitivity, PTSD, suicide, Interpersonal-Psychological Theory, military
Suicide is the leading cause of non-accidental injury related death in the United States (CDC, 2010). Death by suicide is most strongly predicted by suicide attempt, which is in turn predicted in part by suicidal ideation (Kessler et al., 1999; Weissman et al., 1989). Over 90% of individuals who die by suicide suffer from mental health disorders (Cavanagh et al., 2003), and some have claimed the figure is 100% (Joiner, 2010).
Posttraumatic stress disorder (PTSD) is consistently linked with suicidal ideation and suicide attempt (Cougle et al., 2009; Sareen et al., 2007). Nock et al. (2010) also found that although many disorders predict suicidal ideation, PTSD was among very few conditions that predict which individuals experiencing suicidal ideation go on to make a suicide plan or attempt. Although major depressive disorder is often comorbid with PTSD and is also a predictor of suicidal behavior, PTSD but not depression was found to be uniquely associated with suicide attempts in a large female sample, after controlling for comorbidity and trauma history (Cougle et al., 2009).
The Interpersonal-Psychological Theory of Suicide (Joiner, 2005; Van Orden et al., 2010) states that a person will not die by suicide unless he or she has both the desire to die and the acquired capability to do so. Desire to die arises from two specific psychological states: perceived burdensomeness (the view that one’s existence burdens family, friends or society) and thwarted belongingness (alienation from others). The second part of the theory, the acquired capability for suicide, involves a fearlessness of death and high tolerance for self-inflicted pain learned through repeatedly experiencing painful and otherwise provocative events (e.g., past suicide attempts, non-suicidal self-injury, combat exposure, numerous physical fights, etc.). In the context of the interpersonal-psychological theory, traumatic events experienced by those with PTSD may account, at least in part, for increased risk of suicide attempts.
Anxiety sensitivity (AS) is a risk factor for Axis I disorders that may partially explain the associations between PTSD and suicidality (Schmidt et al., 2006). AS refers to fear of arousal sensations and is typically assessed using the Anxiety Sensitivity Index (ASI; Reiss et al., 1986), which is comprised of three subscales related to fears of the physical, social, and cognitive features of anxiety. Elevated ASI scores have been found among those with PTSD (Taylor et al., 1992). Schmidt et al. (2001) also found associations between greater AS and suicidal ideation in a sample of patients with panic disorder, even after covarying mood disorder diagnosis and depression symptoms. Further, much of this association was attributable to the ASI-cognitive subscale. The ASI-cognitive subscale consists of items reflecting fears of loss of cognitive control.
At first glance, the association between AS and suicidality might appear inconsistent with the Interpersonal-Psychological Theory of Suicide (Joiner, 2005). Those with high AS may be unlikely to participate in the types of repeated painful and provocative experiences necessary to cultivate acquired capability to enact suicide. However, examination of AS as a unitary construct may obscure multi-faceted relations between AS and suicidality. On the one hand, some research suggests that those high in AS-cognitive concerns are likely to have increased suicidal ideation (Schmidt et al., 2001; Katz et al., 2011). On the other hand, elevated AS has also been negatively associated with fear of pain (Ocanez et al., 2010). This pattern of findings suggests that certain aspects of AS, such as the fear of physical aspects of anxiety, may be protective against suicide attempts. These individuals seem unlikely to seek out the painful and provocative experiences proposed by the interpersonal-psychological theory to be essential in acquiring the capability for suicide. Alternatively, individuals with low AS-physical concerns may be more willing to engage in these arousing activities. Thus, an individual with a combination of low ASI-physical concerns and high ASI-cognitive concerns may be particularly vulnerable to suicide attempts.
Despite the strong and consistent relationships found between PTSD and suicidality (Nepon et al., 2010; Cougle et al., 2009), there is a lack of research on mechanisms underlying this relationship. The role of specific AS subfactors in suicide attempts has also received very little attention. Thus, the aims of the current study were to examine whether: (1) AS is associated with increased suicide attempts among those with significant PTSD symptoms; (2) AS-physical scores and AS-cognitive scores interact to predict suicide attempts among individuals with PTSD symptoms, such that those with low AS-physical and high AS-cognitive scores are at increased risk; and (3) similar interactions would appear in a prospective analysis of individuals undergoing a stressful life event (basic training).
We tested these aims in two separate studies. In Study 1, we tested the unique and interactive relations between ASI subscales and suicide attempts in an outpatient sample of individuals with PTSD symptoms. In Study 2, we tested whether a similar interaction between AS-Physical and AS-Cognitive would act as a prospective vulnerability factor for suicidal ideation among military cadets undergoing basic training.
Study 1 - Method
Sample and Setting
The sample in this study consisted of 128 adult outpatients receiving psychological services at a university clinic who screened positive for PTSD during an initial screening interview. This positive screen for PTSD indicated that the patient endorsed the following 3 questions: 1) Did something terrible ever happen to you that kept coming back to you in some way like nightmares or flashbacks? 2) Do you try to avoid thinking about it? 3) Do you experience physical and anxiety symptoms, such as your heart racing when you think about the event?
Outpatients seeking services at the clinic include community and university students with a wide socioeconomic status range in part due to the clinic’s inexpensive sliding scale fee schedules. In the current study 51.2% of participants were university students. Exclusionary criteria at the clinic are also minimal: individuals are only referred elsewhere if they are suffering from psychotic or bipolar-spectrum disorders and not stabilized on medication, or if an immediate danger to themselves or others. As such, outpatients served by the clinic present with a variety of conditions of ranging severity.
In the present sample, participants’ ages ranged from 18 to 65 (M = 30.93, SD = 11.54). The sample was primarily female (70.3 %) with 65.4% reporting being single, 15.0% married, 17.3% divorced, and 2.4% separated. The ethnic breakdown of the sample was as follows: 71.2% of the sample was White, 17.8% was Black, 7.6% was Hispanic, .8% was Asian/Pacific-Islander, .8% was Alaskan/American Indian and 1% reported being of another ethnic group not listed above.
Procedure
All participants agreed to participate in the FSU Institutional Review Board-approved research conducted at the FSU Psychology Clinic. The self-report data presented in this study were part of a large battery of screening questionnaires, which were completed prior to receiving psychological services. Structured diagnostic assessments administered by clinical psychology graduate students were conducted to assess Axis I and Axis II conditions prior to receiving treatment (SCID-I and SCID-II; First, Spitzer, Gibbon, & Williams, 1995, 1997).
Measures
Anxiety Sensitivity Index (ASI; Reiss, et al., 1986)
The ASI is a 16-item self-report inventory designed to measure the degree to which individuals are concerned about the potential negative effects of experiencing anxiety symptoms. Previous work has revealed three separable, internal factors underlying the ASI: a) fear of physical symptoms (e.g. It scares me when I feel shaky; It scares me when my heart beats rapidly); b) fear of publicly observable (social) anxiety symptoms (e.g. It is important to me not to appear nervous, other people notice when I feel shaky); and c) fear of cognitive dyscontrol (e.g. When I cannot keep my mind on a task I worry that might be going crazy; When I am nervous I worry that I might be mentally ill). This factor structure has been repeatedly replicated across a range of diverse populations (Zinbarg et al., 1999). The scale has been found to have strong psychometric properties (Antony, 2001; Zvolensky et al., 2001). In the present sample, the coefficient alpha for the total scale, physical, social, and cognitive subscales were .90, .88, .85, and .85 respectively, indicating good internal consistency.
History of Suicidal Behavior
As part of the intake procedure, all participants are asked: Have you ever experienced a suicide attempt? This methodology for measuring past suicide attempt is similar to other published studies (e.g., Schmidt et al., 2001).
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First, et al., 1995)
The SCID-I is a well-validated and widely used semi-structured interview designed to assess DSM-IV Axis I diagnoses. The SCID-II is a semi-structured interview that was also conducted to assess the presence of personality disorder pathology on the basis of DSM-IV criteria (First et al., 1997).
Positive and Negative Affect Schedule – Negative Affect (PANAS; Watson et al., 1988)
The PANAS is a 20-item self-report inventory designed to measure global emotional states at the time of assessment. Items fall into two 10-item subscales that assess positive and negative affect (PA and NA, respectively). Coefficient alpha for the PANAS-NA in this sample was .89, indicating good internal consistency.
Study 1 - Results
History of a suicide attempt was found in 36.7% of the sample. In terms of diagnostic co-occurrence, 31.9% of previous attempters received a Major Depressive Disorder (MDD) diagnosis compared with 40.7% of non-attempters (χ2 (1, n = 128) = .65, p = .421). A significantly higher percentage of past attempters received a personality disorder diagnosis (42.6%) than did non-attempters (12.3%; χ2 (1, n =128) = 13.49, p < .001).
Bivariate correlations between the measures are shown in Table 1. As expected due to the similarity of the constructs, all measures were significantly correlated. The PANAS-NA was most strongly correlated with the AS-cognitive subfactor (r = .59). Next, analyses were conducted to examine whether there were group differences between past attempters and non-attempters in anxiety related cognitive measures. These results are displayed in Table 2. Similar to Schmidt et al. (2001), there were no significant differences between the groups on these measures.
Table 1.
Study 1 - Summary of Intercorrelations, Means, and Standard Deviations for Scores on the ASI, ASI – subscales, and the PANAS-NA scale
| Measure | 1 | 2 | 3 | 4 | M | SD |
|---|---|---|---|---|---|---|
| 1. ASI Total | - | 28.55 | 13.51 | |||
| 2. ASI Cognitive | .84 | - | 7.13 | 4.62 | ||
| 3. ASI Physical | .94 | .65 | - | 12.95 | 8.08 | |
| 4. ASI Social | .70 | .47 | .53 | - | 8.47 | 2.98 |
| 5. PANAS – NA | .61 | .59 | .53 | .41 | 30.50 | 8.11 |
Note. All items intercorrelated at p < .01. ASI = Anxiety sensitivity index.
PANAS – NA = Positive affect negative affect scales – negative affect scale.
Table 2.
Study 1 - Suicide Attempt Status and Anxiety Related Cognitive Measures
| Measure | Previous Attempt
|
t | |
|---|---|---|---|
| + M (SD) | − M (SD) | ||
| ASI Total | 27.62 (11.83) | 29.09 (14.44) | .59 |
| ASI Cognitive | 7.00 (4.27) | 7.20 (4.83) | .23 |
| ASI Physical | 11.98 (7.26) | 13.52 (8.51) | 1.04 |
| ASI Social | 8.64 (3.06) | 8.37 (2.95) | −.49 |
| Negative Affect | 30.87 (7.47) | 30.37 (8.49) | −.34 |
Note. ASI = Anxiety sensitivity index
Direct logistic regression was performed to assess the impact of a number of factors on the likelihood that patients would report a past suicide attempt. The model contained 8 independent variables (negative affect, MDD diagnosis, Personality Disorder (PD) diagnosis, Alcohol Use Disorder (AUD) diagnosis, Substance Use Disorder (SUD) diagnosis, ASI cognitive, ASI physical, ASI cognitive X ASI physical interaction). Negative affect was included to control for general mood/anxiety pathology. Based on recent studies of PTSD and suicidality (Nepon et al., 2010; Cougle et al., 2009), MDD and PD diagnoses were added to the regression model to determine if the result was confounded by these factors. MDD diagnosis was included because of the significant comorbidity between PTSD and MDD (Cougle et al., 2009). PD diagnosis was added because of the high rate of suicide attempts among those diagnosed with a personality disorder (Nepon et al., 2010). Similar to Nepon et al. (2010), all personality disorders were included to be as comprehensive as possible. Finally, AUD diagnosis and SUD diagnoses were predictive of suicide attempt history in a recent epidemiological study (Nock et al., 2010). The full model containing all predictors (negative affect, MDD diagnosis, PD diagnosis, AUD diagnosis, SUD diagnosis, ASI-physical, ASI-cognitive and ASI-physical X ASI-cognitive interaction) was statistically significant, χ2 (df =8, n = 128) = 24.437, p = .002. The results of the logistic regression are shown in Table 3. Personality disorder diagnosis was the most robust predictor of past suicide attempt (OR = 5.99, Wald = 12.432, p < .001). After adding the additional covariates, the ASI-cognitive X ASI-physical interaction remained significant (OR = .987, Wald = 4.48, p = .03).
Table 3.
Study 1 - Logistic Regression Analyses Predicting Suicide Attempt Controlling for Negative Affect, PD Diagnosis, MDD Diagnosis, AUD Diagnosis and SUD Diagnosis
| Variable | B | SE B | OR | 95% CI | Wald | p |
|---|---|---|---|---|---|---|
| Negative Affect | −.02 | .03 | .98 | [.92, 1.05] | .24 | .63 |
| PD Diagnosis | 1.79 | .51 | 5.99 | [2.21, 16.27] | 12.34 | .00** |
| MDD Diagnosis | −.57 | .45 | .57 | [.24, 1.37] | 1.59 | .21 |
| AUD Diagnosis | .64 | .67 | 1.90 | [.51, 7.03] | .93 | .34 |
| SUD Diagnosis | −.75 | .81 | .48 | [.99, 2.31] | .85 | .36 |
| ASI Physical | −.01 | .04 | 1.00 | [.92, 1.07] | .01 | .92 |
| ASI Cognitive | .10 | .07 | 1.10 | [.97, 1.25] | 2.02 | .15 |
| ASI Phy X ASI Cog | −.01 | .01 | .99 | [.97, .99] | 4.48 | .03* |
p < .05.
p < .01.
PD = Personality disorder. MDD = Major depressive disorder. AUD = Alcohol use disorder. SUD = Substance use disorder. ASI = Anxiety sensitivity index. ASI Phy X ASI Cog = Interaction between ASI-physical subfactor and ASI-cognitive subfactor.
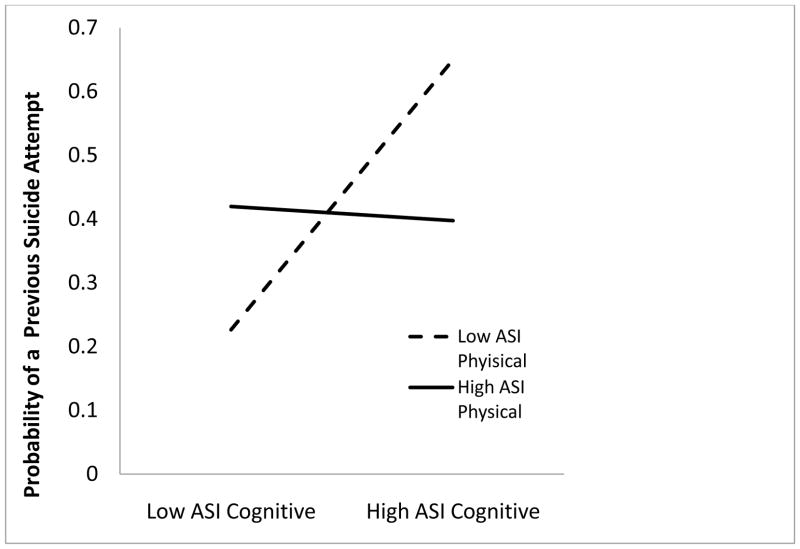
In the next step, we probed the hypothesized 2-way interaction between ASI-physical X ASI-cognitive (See Figure 1). As predicted, at low levels of ASI-physical (1 SD below the mean) the effect of ASI-cognitive was significant (OR = 1.23, Wald = 4.36, p = .037) such that at low levels of ASI-physical and high levels of ASI-cognitive an individual was significantly more likely to have attempted suicide. Again, the effect of ASI-cognitive at high levels of ASI physical was not significant as predicted. Adding ethnicity or gender to the regression models did not change the pattern of results.
Figure 1.
Effect of ASI-cognitive on ASI-physical in predicting previous suicide attempt among clinical outpatients screening positive for PTSD (Study1). This analysis controlled for negative affect, diagnosis of a personality disorder, diagnosis of major depressive disorder, diagnosis of an alcohol use disorder, and diagnosis of a substance use disorder. ASI = Anxiety Sensitivity Index.
Study 2
One limitation of the findings from Study 1 is that the data are cross-sectional, so no inferences can be made about causality. As a more stringent test of the AS-suicidality association, we prospectively evaluated whether baseline levels of the AS subscales interacted to predict changes in suicidal ideation in a military sample undergoing a stressful life event.
Study 2 - Method
Participants and Procedure
Participants included 1,081 first year cadets from the United States Air Force Academy (USAFA; see Schmidt et al. [1997] for more details on admission criteria of the USAFA). The cadets begin military training upon arrival with basic cadet training (BCT). BCT consists of five weeks of training, designed to continuously expose cadets to a variety of unpredictable and uncontrollable physical and mental stressors. Cadets are not given schedules and have no access to clocks or watches. New stressors are continually introduced to ensure that each cadet is overtaxed.
Data for the present study were gathered during a group administration of measures to the entire class of cadets during the first few days of BCT (Time 1) and five weeks later at the end of BCT (Time 2). Participants were told that the study was evaluating the impact of BCT on physical and emotional functioning. Prior to the administration of measures, cadets were assured that USAFA would not have access to information collected. Furthermore, code numbers were used on all forms to ensure anonymity. Written informed consent was also obtained. The Time 1 assessment battery consisted of measures of anxiety sensitivity, history of spontaneous panic, trait anxiety, anxiety symptoms, depression and hopelessness, as well as indexes tapping the functional impairment created by anxiety. The Time 2 assessment battery was identical to the Time 1 battery with the exception that the Time 2 battery also included measures of spontaneous panic, panic frequency, and panic related worry during BCT as well as indexes of physical and mental disability. Schmidt, et al. (1997) found that total ASI scores predicted clinically significant distress and impairment in this sample. However, they did not examine interactions of ASI subfactors or associations with suicidal ideation.
In this sample, participants’ ages ranged from 17 to 22 (M = 18.02, SD = .93). The sample was primarily male (81.7 %). The racial breakdown of the sample was as follows: 83.7% White, 3.6% Black, 5.6% Hispanic, 4.3% Asian/Pacific-Islander, 1.2% American Indian, and 1.7% reported being of another racial group not listed above.
Measures
Anxiety Sensitivity Index (ASI)
See previous description of measure.
Beck Depression Inventory (BDI)
Depressive symptoms experienced during the past week were assessed with the BDI minus question 9. BDI question 9 was used to assess suicidal ideation. This procedure has been previously used to measure suicidal ideation (e.g., Schmidt et al., 2001). The BDI is a psychometrically sound measure of depressive symptomatology (Beck, et al., 1988).
Beck Anxiety Inventory (BAI)
The BAI is a well-validated measure of anxiety symptoms consisting of 21 self-report items designed to assess level of subjective anxiety within the past week. Responses are rated on a likert-type scale with values ranging from 0 (not at all) to 3 (severely, I could barely stand it). Scores range from 0 to 63, with higher scores indicating higher levels of self-reported anxiety symptoms. The BAI has demonstrated excellent internal consistency and high concurrent validity with other measures of anxiety (Beck, et al, 1988a).
Study 2 - Results
Time 2 suicidal ideation was found in 7.3% of the sample. T2 suicidal ideators were significantly higher on baseline depressive symptoms (t (86.63) = −6.49, p < .001), anxiety (t (94.75) = −5.08, p = < .001) and T1 suicidal ideation (t (84.70) = −9.56, p < .001). Bivariate correlations between the measures are shown in Table 4. As expected due to the similarity of the constructs, all measures were significantly correlated.
Table 4.
Study 2 - Bivariate correlations, Means and Standard Deviations among Baseline and Predictor Variables
| Measure | 1 | 2 | 3 | 4 | 5 | M | SD |
|---|---|---|---|---|---|---|---|
| 1. Anxiety | - | 17.55 | 10.50 | ||||
| 2. Ideation | .18* | - | .14 | .38 | |||
| 3. Depression | .61* | .38* | - | 9.35 | 7.07 | ||
| 4. ASI Total | .31* | .15* | .25* | - | 4.01 | 2.85 | |
| 5. ASI Physical | .35* | .13* | .26* | .82* | - | 1.16 | 1.85 |
| 6. ASI Cognitive | .23* | .19* | .28* | .56* | .30* | .30 | .77 |
p < .01.
ASI = Anxiety sensitivity index.
Direct logistic regression was performed to assess the impact of a number of factors on the likelihood that patients would report suicidal ideation at T2. The model contained 6 independent variables (T1 depressive symptoms, T1 anxiety, T1 suicidal ideation, T1 ASI- cognitive, T1 ASI-physical, T1 ASI-cognitive X ASI-physical interaction). Time 1 depressive symptoms, T1 anxiety, and T1 suicidal ideation were included in the model to control for the effect of these variables on the prediction of T2 suicidal ideation because of significant differences found in these baseline variables between suicide ideators and non-ideators. The full model containing all predictors (T1 depressive symptoms, T1 anxiety, T1 suicidal ideation, T1 ASI-cognitive, T1 ASI-physical, T1 ASI-cognitive X ASI-physical interaction) was statistically significant, χ2 (6, n = 1081) = 146.54, p < .001. The results of the logistic regression are shown in Table 5. Among covariates, T1 suicidal ideation was a robust predictor of T2 suicidal ideation (OR = 11.14, Wald = 75.62, p < .001) as was ASI-cognitive concerns (OR = 1.66, Wald = 8.26, p = .004). As predicted, the ASI-cognitive X ASI-physical interaction was significant (OR = .79, Wald = 13.69, p < .001).
Table 5.
Study 2 - Results of Logistic Regression predicting T2 Suicidal Ideation from Anxiety Sensitivity Interaction
| Variable | B | SE B | OR | 95% CI | Wald | p |
|---|---|---|---|---|---|---|
| T1 Depression | .05 | .02 | 1.05 | [1.00, 1.09] | 3.79 | .05 |
| T1 Anxiety | .02 | .02 | 1.02 | [.98, 1.05] | 1.01 | .31 |
| T1 Ideation | 2.41 | .28 | 11.11 | [6.46, 19.12] | 75.62 | .00** |
| T1 ASI Physical | .08 | .08 | 1.08 | [.93, 1.25] | 1.06 | .30 |
| T1 ASI Cognitive | .51 | .18 | 1.66 | [1.17, 2.34] | 8.26 | .00** |
| ASI Phy X ASI Cog | −.24 | .06 | .79 | [.70, .89] | 13.69 | .00** |
p < .05.
p < .01.
ASI = Anxiety sensitivity index. ASI Phy X ASI Cog = Interaction between ASI physical subfactor and ASI Cognitive subfactor.
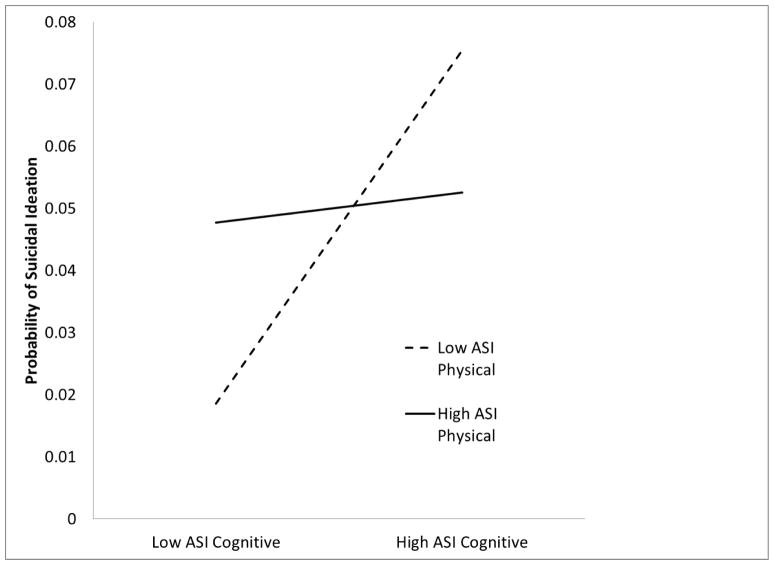
As a second step, we probed the hypothesized 2-way interaction between ASI-physical X ASI-cognitive (See Figure 2). As predicted, at low levels of ASI-physical (1 SD below the mean) the effect of ASI-cognitive was significant (OR = 2.57, Wald = 14.74, p < .001), such that at low levels of ASI-physical and high levels of ASI-cognitive an individual was significantly more likely to have T2 suicidal ideation. Also as predicted, the effect of ASI-cognitive at high levels of ASI-physical (1 SD above mean) was not significant. Adding ethnicity or gender to the regression models did not change the pattern of findings.
Figure 2.
Interaction of T1 AS physical X AS cognitive controlling for T1 Depressive symptoms, T1 anxiety and T1 suicidal ideation on T2 suicidal ideation in a sample of Air Force cadets after completion of basic cadet training (Study2).
Thirty recruits developed suicidal ideation during BCT. Logistic regression was performed to assess the impact of AS related factors on incidence of suicidal ideation by excluding participants with prior suicidal ideation. The new model contained 5 independent variables (T1 depressive symptoms, T1 anxiety, T1 ASI-cognitive, T1 ASI-physical, T1 ASI-cognitive X ASI-physical interaction). The full model was statistically significant χ2 (5, n = 946) = 21.25, p = .001. Among covariates, T1 depressive symptoms (OR = 1.11, Wald = 10.00, p = .002) but not T1 anxiety (p = .576) significantly predicted new suicidal ideation. All ASI related predictors were marginally significant predictors of suicidal ideation incidence, including T1 ASI-cognitive (OR = 1.48, Wald = 2.94, p = .086), T1 ASI-physical (OR = 1.16, Wald = 2.65, p = .103), and their interaction (OR = .88, Wald = 2.86, p = .091).
Discussion
The findings of this study suggest that a combination of low physical AS concerns and high cognitive AS concerns are associated with increased rates of suicide attempt among those with significant PTSD symptoms and are a risk factor for suicidal ideation among individuals undergoing a stressful life event. Our results from Study 2 are consistent with those from Schmidt et al. (2001), who found that AS-cognitive was highly predictive of suicidal ideation in a sample of patients with panic disorder. In addition, consistent with Schmidt et al. (2001), our Study 1 data revealed that when the AS subscales are considered separately, there were no significant associations with prior suicide attempts.
Our findings that fears of the cognitive and physical symptoms of anxiety interacted to predict suicide attempts suggest that complex factors may be at work to account for the associations between AS and suicidality. Higher AS-cognitive concerns may reflect fears of loss of control over mental capacities and increased susceptibility to a positive feedback loop leading from suicidal ideation to suicide attempt (Katz et al., 2011). When this is combined with fearlessness regarding painful and provocative experiences, which lower AS-physical scores may represent, individuals may be at heightened risk for suicide attempt. These findings are consistent with the literature linking emotion dysregulation and greater pain tolerance to suicide attempt (Brown, et al., 2002; Orbach, Palgi et al., 1996). Additionally, these findings are consistent with the Interpersonal-Psychological Theory of Suicide.
The results of this investigation implicate mechanisms that may account for increased suicide risk among a population that is at high risk for death by suicide. Encouragingly, AS has been shown to be amenable to amelioration. Very brief interventions featuring interoceptive exposure exercises have consistently reduced total ASI and ASI subfactors (Schmidt et al., 2007; Feldner et al. 2008). Clinicians may benefit from implementing these exercises with PTSD clients who endorse elevated suicide risk as well as elevated ASI-cognitive scores. Caution may also be warranted when implementing AS reduction interventions with this population, since the current study’s findings suggest that elevated ASI-physical scores may be protective in certain cases. One possibility is to target ASI-cognitive concerns with cognitive therapy; however, interoceptive exposure exercises are recommended for the majority of cases and have been shown to decrease all ASI subfactors (Schmidt et al., 2007). It is worth pointing out that individuals with both low ASI-physical concerns and low ASI-cognitive concerns were at the lowest risk for previous suicide attempt in the current study. Institutions such as the military, which deal with higher than average rates of PTSD and suicide, may find targeting AS through interoceptive exposure exercises a simple but effective intervention.
The finding that the percentage of suicide attempters in Study 1 was comparable or even higher than in other recent investigations of PTSD suggests that our sample was quite severe in overall psychopathology and suicidality. Epidemiological studies have found that between 19.5% and 30.4% of those with PTSD had attempted suicide (Davidson, et al., 1991; Nepon et al., 2010). The percentage of suicide attempters in comparable clinical samples of those with PTSD has ranged from 9.6% – 30% (Tarrier & Gregg, 2004; Warshaw et al., 1993). The rate of a comorbid MDD diagnosis in our sample (37.5%) was nearly identical to other studies of PTSD (37.2%; Sareen et al., 2007). Additionally, in those with comorbid PTSD symptoms and MDD we found 31.3% (n = 15) reporting a past suicide attempt. This was comparable to the NESARC sample (26.5%). The rate of comorbid personality disorder diagnoses (23.4%) in our sample was comparable to the clinical sample from the Collaborative Longitudinal Personality Disorders Study (CLPDS; 21.3%). Finally, although the presence of comorbid MDD and PD was comparable to other samples investigating PTSD, it is important to note we statistically covaried for both in Study 1 to rule out the possibility that these diagnoses were responsible for the current findings.
It is important to note a few limitations of the studies. First, although Study 1 used a clinical, treatment-seeking sample with PTSD symptomatology, only 13% of participants were also diagnosed with PTSD using a structured clinical interview. This is comparable to a recent investigation of psychiatric patients, where 91% screened endorsed experiencing a traumatic event but only 7% were diagnosed with PTSD (Floen & Elkit, 2007). Additionally, the brief PTSD screen we used in Study 1 is similar to the Primary Care PTSD screen (Prins et al., 2003), that has been used in previous studies examining PTSD symptomatology (Stewart & White, 2008; Ford, et al., 2007). Although the majority of the sample was not diagnosed with PTSD, all individuals endorsed evidence of key DSM PTSD criteria. A limitation in both studies is the possibility that the identified interaction between ASI-cognitive concerns and ASI-physical concerns would not predict actual death by suicide. However, suicide attempt is the strongest predictor of death by suicide (Suominen et al., 2004), and has been consistently used in previous studies examining suicidality (Schmidt et al., 2001; Sareen et al., 2007; Cougle et al., 2009). Third, the design of Study 1 precluded us from examining the causal roles of AS subfactors in suicide attempt. More specifically, we were unable to ascertain whether these high-risk ASI scores preceded suicide attempts or whether modification of AS might reduce suicide risk. Future large-scale prospective studies may help clarify these relationships. The inclusion of Study 2 is a first step in this regard. Fourth, the ASI was developed to measure AS as a unitary construct. Although the ASI is used frequently to examine AS subfactors (Schmidt et al., 2001; Stewart et al., 1997, Schmidt et al., 1999), it would have been ideal to measure the AS subfactors with the Anxiety Sensitivity Index-3 (Taylor et al., 2007).
Our findings are likely to be generalizable to those suffering from increased suicidality and PTSD symptoms. The Study 1 sample was fairly large and made up of clinical outpatients. MDD, PD, AUD, and SUD diagnoses were assigned using structured diagnostic interviews. These diagnoses have been found to affect suicidality and were statistically covaried in the analyses. Although suicidal ideation was very low in the Study 2 sample, the results show that AS significantly predicted future occurrence of suicidal ideation after experiencing a stressful life event. Given that as many as 70% of suicide attempters suffer from an anxiety disorder (Nepon et al., 2010), future studies should also examine if this interaction is relevant in other diagnoses. Future research may also examine whether targeting AS reduces suicidal ideation in patients with PTSD and elevated suicide risk.
Acknowledgments
We have no acknowledgements for the current manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antony MM. Measures for panic disorder and agoraphobia. In: Antony MM, Orsillo, Susan M, Roember L, editors. Practitioner’s guide to empirically based measures of anxiety. New York, NY: Kluwer Academic/Plenum Publishers; 2001. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the beck depression inventory - 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Brown G, Epstein N, Steer RA. An inventory for measuring clinical anxiety - psychometric properties. Journal of Consulting and Clinical Psychology. 1988a;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- CDC. 10 Leading Causes of Injury Related Death. Center for Disease Control; 2010. http://www.cdc.gov/injury/wisqars/pdf/Violence_2007-a.pdf. [Google Scholar]
- Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychological Medicine. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Keough ME, Riccardi CJ, Sachs-Ericsson N. Anxiety disorders and suicidality in the National Comorbidity Survey-Replication. Journal of Psychiatric Research. 2009;43:825–829. doi: 10.1016/j.jpsychires.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. PTSD, depression, and their comorbidity in relation to suicidality: Cross-sectional and prospective analyses of a national probability sample of women. Depression and Anxiety. 2009;26:1151–1157. doi: 10.1002/da.20621. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Hughes D, Blazer DG, George LK. Posttraumatic-stress-disorder in the community - An epidemiologic-study. Psychological Medicine. 1991;21:713–721. doi: 10.1017/s0033291700022352. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Babson K, Leen-Feldner EW, Schmidt NB. An integrated approach to panic prevention targeting the empirically supported risk factors of smoking and anxiety sensitivity: Theoretical basis and evidence from a pilot project evaluating feasibility and short-term efficacy. Journal of Anxiety Disorders. 2008;22:1227–1243. doi: 10.1016/j.janxdis.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for the DSM-IV axis I disorders-patient edition (SCID-I/P-version 2) New York State Psychiatric Institute, Biometrics Research Division; 1995. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured clinical interview for DSM-IV personality disorders (SCID-II) Washington, DC: American Psychiatric Publishing; 1997. [Google Scholar]
- Floen SK, Elklit A. Psychiatric diagnoses, trauma, and suicidiality. Annals of General Psychiatry. 2007;6:12. doi: 10.1186/1744-859X-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Hawke J, Alessi S, Ledgerwood D, Petry N. Psychological trauma and PTSD symptoms as predictors of substance dependence treatment outcomes. Behaviour Research and Therapy. 2007;45:2417–2431. doi: 10.1016/j.brat.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner TE. Myths about suicide. Cambridge, MA: Harvard University Press; 2010. [Google Scholar]
- Katz C, Yaseen ZS, Mojtabai R, Cohen LJ, Galynker II. Panic as an independent risk factor for suicide attempt in depressive illness: findings from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2011 doi: 10.4088/JCP.10m06186blu. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the national comorbidity survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Nepon J, Belik SL, Bolton J, Sareen J. The relationship between anxiety disorders and suicide attempts: Findings from the national epidemiologic survey on alcohol and related conditions. Depression and Anxiety. 2010;27:791–798. doi: 10.1002/da.20674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ocanez KLS, McHugh RK, Otto MW. A meta-analytic review of the association between anxiety sensitivity and pain. Depression and Anxiety. 2010;27:760–767. doi: 10.1002/da.20681. [DOI] [PubMed] [Google Scholar]
- Orbach I, Palgi Y, Stein D, HarEven D, LotemPeleg M, Asherov J, et al. Tolerance for physical pain in suicidal subjects. Death Studies. 1996;20:327–341. doi: 10.1080/07481189608252786. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJG. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69:242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K, Bates M. Evaluating panic-specific factors in the relationship between suicide and panic disorder. Behaviour Research and Therapy. 2001;39:635–649. doi: 10.1016/s0005-7967(00)00034-6. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Stewart LP, White PM. Sensory filtering phenomenology in PTSD. Depression and Anxiety. 2008;25:38–45. doi: 10.1002/da.20255. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. Journal of Anxiety Disorders. 1997;11:179–200. doi: 10.1016/s0887-6185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: A 37-year follow-up study. American Journal of Psychiatry. 2004;161:562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Gregg L. Suicide risk in civilian PTSD patients - Predictors of suicidal ideation, planning and attempts. Social Psychiatry and Psychiatric Epidemiology. 2004;39:655–661. doi: 10.1007/s00127-004-0799-4. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Taylor S, Koch WJ, McNally RJ. How does anxiety sensitivity vary across the anxiety disorders. Journal of Anxiety Disorders. 1992;6:249–259. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The Interpersonal Theory of Suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Fierman E, Pratt L, Hunt M, Yonkers KA, Massion AO, et al. Quality of life and dissociation in anxiety disorder patients with histories of trauma or PTSD. American Journal of Psychiatry. 1993;150:1512–1516. doi: 10.1176/ajp.150.10.1512. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect - the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Mohlman J, Hong NN. Dimensions of anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Psychology Press; 1999. [Google Scholar]
- Zvolensky MJ, Goodie JL, McNeil DW, Sperry JA, Sorrell JT. Anxiety sensitivity in the prediction of pain-related fear and anxiety in a heterogeneous chronic pain population. Behaviour Research and Therapy. 2001;39:683–696. doi: 10.1016/s0005-7967(00)00049-8. [DOI] [PubMed] [Google Scholar]