Abstract
Objective
To examine the differential morbidity/mortality associated with evacuation versus sheltering in place for nursing home (NH) residents exposed to the 4 most recent Gulf-hurricanes
Methods
Observational study using Medicare claims, and NH data sources. We compared the differential mortality/morbidity for long-stay residents exposed to 4 recent hurricanes (Katrina, Rita, Gustav, and Ike) relative to those residing at the same NHs over the same time periods during the prior 2 non-hurricane years as a control. Using an instrumental variable analysis, we then evaluated the independent effect of evacuation on outcomes at 90 days.
Results
Among 36,389 NH residents exposed to a storm, the 30 and 90 day mortality/hospitalization rates increased compared to non-hurricane control years. There were a cumulative total of 277 extra deaths and 872 extra hospitalizations at 30 days. At 90 days, 579 extra deaths and 544 extra hospitalizations were observed. Using the instrumental variable analysis, evacuation increased the probability of death at 90 days from 2.7-5.3% and hospitalization by 1.8-8.3%, independent of other factors.
Conclusion
Among residents exposed to hurricanes, evacuation significantly exacerbated subsequent morbidity/mortality.
Background
In the wake of the publicity over the 78 deaths at Louisiana nursing homes (NH) following Hurricane Katrina, public policy explicitly changed to require universal evacuation of all “at risk” facilities prior to landfall by state and local emergency management organizations.1, 2 In interviews conducted following Hurricane Gustav (2008) with many of the same NH administrators that experienced Hurricane Katrina 3 years earlier, Blanchard et al. noted that many administrators felt “external pressure from state and local agencies to evacuate their residents.”3 This perceived pressure is perhaps best evidenced by the absolute number of NHs that evacuated prior to recent Gulf storms; 30 homes evacuated in 2005 prior to Katrina. Less than a month later, 72 facilities evacuated in the same region prior to Hurricane Rita.4 In 2008, 119 facilities evacuated prior to Hurricane Gustav and 81 facilities evacuated prior to Hurricane Ike, even though it made landfall far south of the evacuated Louisiana facilities.i
Despite the policy requiring evacuation, there is controversy as to whether universal evacuation is best from the perspective of protecting NH residents.1, 2, 5 The majority of the nation’s 1.6 million NH residents are frail, lack mobility, have difficulties with vision/hearing, and have signficant cognitive impairment and other health comorbidities that can complicate a safe evacuation.6-9 Previous research has spotlighted the dangers inherent with transitions of care under non-disaster conditions. Capezuti et al noted a 2-3 fold increase in the rate of falls after a forced relocation from one home to another.10
The purpose of this study is to document the mortality and morbidity effects of the last four major hurricane disasters (Hurricanes Katrina, Rita, Gustav, and Ike) on NH residents in the Gulf States and to test the effect of evacuation vs. sheltering in place on the morbidity/mortality experienced by those residents.
METHODS
Data Sources
Prior to beginning work, the Institutional Review Boards at Brown University and the University of South Florida approved the research protocol. We drew upon multiple data sources for the current study, ranging from clinical data to Medicare claims and enrollment records as well as information about each NH’s geographic location, structural and staffing characteristics prior to the storm and, detailed meterological information about each storm. Resident level data from the Minimum Data Set (MDS) for the years 2003-2008 was matched to the Medicare denominator files and hospital claims using the Residential History File methodology described elsewhere 11, 12 The MDS is a federally mandated assessment for all NH residents that includes demographics, diagnoses, treatments and measures of both physical and cognitive functions.13 The Centers for Medicare and Medicaid Services (CMS) Standard Analytic Files for part A claims contain information to evaluate inpatient hospitalization, hospice, home health, and outpatient services for residents in each cohort. The Medicare enrollment data includes date of death.
NH characteristics were derived from the Online Survey Certification Automated Record (OSCAR) which records the results of annual state regulatory inspections including information about NH ownership, size, staffing levels, aggregated resident characteristics as well as the facilities’ address. Facilities included in the study had to be operational (serving residents with MDS data) for at least two years prior to the storm. Each facility was geo-coded using the mailing address identified in the OSCAR database.
Hurricane Characteristics
Hurricane damage results from high winds, heavy rainfall that causes flooding, and storm surge. Wind damage from hurricanes is a function of how close a facility is to the actual path and whether the facility is east or west of the path. The hurricane’s northeast quadrant contains its strongest winds making it the “dirty-side” of the hurricane. 14Storm surge occurs when the low pressure of the storm causes the sea level to rise and, strong winds pushes high waves associated with a hurricane, onto the shore.14 As such, distance from the shore and elevation of the facility are important factors when considering whether to evacuate.
Data about each hurricane were downloaded from the National Weather Service Tropical Cyclone Advisory Archive. For each storm the geo-coordinates of the projected 24-, 48-, and 72-hour path and the actual hurricane path, were used to generate shape files entered into ARC GIS (ESRI, 2006). Information on shoreline was downloaded from the National Oceanic and Atmospheric Administration (NOAA) website.15 Elevation data about each facility was (Raster Files) downloaded from the WorldClim- Global Climate Data website using the individual NH’s geographic location. 16 Then, using the Near tool in ARC GIS, we calculated the distance of each facility to the 24-, 48-, 72-hour, and actual path, the distance of the facility to the shoreline, the elevation of the building and whether the storm was on the east or west side of the projected and actual paths.
Subject Sample
For each of the four storms (Hurricanes Katrina and Rita in 2005, and Hurricanes Gustav and Ike in 2008), an exposure cohort of long stay (>90 days), Medicare fee for service beneficiaries were identified. Exposed residents included those residing in at-risk homes at least 3 calendar months before the date of the hurricane landfall. At-risk NHs were defined as those homes located in parishes/counties that were included in the National Weather Service’s initial Hurricane Watch at 48 hrs and the subsequent warning zone at 24 hrs.17 Additional NHs were included if they were located in parishes/counties where at least one NH was known to have evacuated based on lists provided by state NH associations. Finally, NHs from counties/parishes where there were no known evacuations were removed.4 The geographic exposure region for each of the four storms is available from the author.
The exposed resident cohort was then compared to non-hurricane exposed cohorts residing in the same NHs during the same time period in each of the prior 2 calendar years (e.g. 2003 and 2004 for Hurricanes Katrina/Rita; 2006 and 2007 for Hurricanes Gustav/Ike). Facilities were excluded if they did not have data from all three years.
Resident Outcomes
Information on the date of death came from the Medicare denominator file. Using data from Medicare files, the pre-hurricane period (3 months prior to landfall to 4 days prior to landfall), 30-day, and 90-day mortality and hospitalization rates were established for exposed patients. A date four days prior to each storm was selected due to potential morbidity/ mortality associated with evacuations that commenced on or after that date but before storm landfall. To our knowledge, no homes evacuated before that date. The exposure groups were then compared to control populations residing in the same NHs during the same time period for the two non-hurricane years.
Independent variables characterizing NH residents (e.g. demographics, health characteristics) were obtained from the Minimum Data Set (MDS). In addition to age, gender and race, we adjusted mortality and hospitalization outcomes for cognitive status (Cognitive Performance Scale),18 functional status (Activities of Daily Living Scale),19 and comorbidity (The Changes in Health, End-stage disease and Signs and Symptoms (CHESS) Comorbidity Index)20--all validated measures contained in the MDS.
Shelter versus Evacuation Data
Residents were considered to have evacuated if they resided in facilities that completely evacuated prior to the date of landfall for each storm. Data on a facility’s evacuation status was obtained from the Texas Department of Aging & Disability Services, Mississippi Department of Health, and the Lousiana Department of Health and Hospitals. NHs that evacuated after the date of landfall were considered to have sheltered in place.
Statistical Analysis
Differences in the rates of mortality and hospitalization were determined across the three annual cohorts of long-stay NH residents from the same facilities. Outcomes from both the 2005 and 2008 cohorts–treated as exposed to one of the 4 hurricanes—were contrasted to outcomes from residents residing in the same NHs during non-hurricane years (2003 and 2004 for 2005 storms; 2006 and 2007 for 2008 storms). Since all outcome variables were defined as dichotomous, Chi-square tests of statistical significance were performed to determine differences in outcome.
To evaluate the effect of the decision to evacuate on the mortality/morbidity of the population, we utilized an instrumental variable approach for each storm using methodology previously utilized.21-23 Instrumental variable modelling, unlike more traditional statistical approaches such as multivariate logistic regression, serve to help reduce unmeasured confounding in cases where it is impossible to randomize patients or account for all confounders23. As such, the instrumental variable approach was utilized to mitigate the influence of potential “omitted-variable bias” on the effect of evacuation. The equation estimated was:
| (1') |
where Evaĉn was the variable that is predicted using the instrument. Geographic characteristics related to the location of the facility relative to the storm were utilized as instrumental variables. The key assumption is that these variables (e.g., perpendicular distance from the facility to the path of the storm 48 hours before landfall ( Dist48 )) will cause variations in evacuation status across facilities that are unrelated to any omitted variable from the regression of patients’ outcomes (mortality and hospitalization). In particular, the assumption is that the correlation between Dist48 and uin equals zero. Since we have more than one instrumental variable, the model is considered to be “over-identified”. We used Hansen’s J-statistic to test the hypothesis that the model is correctly specified (i.e., the validity of the restriction that the instrumental variable does not belong in the equation 1′ as a separate covariate).24 The statistic is distributed as a Chi-square. The probability of rejecting the null hypothesis increases as the value of the statistic increases.
Although the actual instrumental variables used differed across storms, the perpendicular distance between the NH and the path of the storm at 48 hours before landfall was consistent in models for all storms. Details of the specific variables used can be found in Table 2. The second stage of the model estimated the effect of evacuation on the outcomes of death and hospitalization at 90 days. In addition to storm parameters such as the wind speed at landfall and the distance of the home to the actual path of the storm, the second stage model included indicators of patient acuity (e.g. Congestive heart failure, Cancer, Diabetes, Feeding Tube, CPS Score 18,CHESS score20, facility level-Acuity Index25, gender, race and other factors predictive of hospitalization). These clinical indicators of patient acuity were selected based on qualitative data derived from previous interviews with nursing home administrators following Hurricanes Katrina and Rita who noted particular difficulties in moving/managing certain patients with complex medical needs.3, 26
Table 2.
Effect of Evacuation Decision on Morbidity and Mortality
| 2005 Storms | 2008 Storms | |||
|---|---|---|---|---|
| Katrina | Rita | Gustav | Ike | |
| Death at 90 days | ||||
| Evacuation | 0.053** | 0.038** | 0.027** | 0.034*** |
| (0.021) | (0.017) | (0.013) | (0.012) | |
| CHF | 0.028*** | 0.024*** | 0.027** | 0.035*** |
| (0.010) | (0.009) | (0.011) | (0.010) | |
| Feeding Tubes | 0.036*** | 0.014 | 0.038** | 0.032** |
| (0.014) | (0.013) | (0.017) | (0.014) | |
| Overid test: Hansen’s J statistic and chi-2(3) p-value in parenthesis |
5.6 (0.22) |
2.66 (0.44) |
8.9 (0.19) |
2.90 (0.41) |
| Hospitalization at 90 days | ||||
| Evacuation | 0.083*** | 0.051* | 0.040* | 0.018 |
| (0.030) | (0.028) | (0.023) | (0.025) | |
| CHF | 0.059*** | 0.057*** | 0.115*** | 0.075*** |
| (0.011) | (0.012) | (0.020) | (0.013) | |
| Feeding Tubes | 0.053*** | 0.096*** | 0.083*** | 0.079*** |
| (0.019) | (0.016) | (0.025) | (0.016) | |
| Overid test: Hansen’s J statistic and chi-2(3) p-value in parenthesis |
1.7 (0.78) |
3.6 (0.3) |
13.6 (0.06) |
6.06 (0.11) |
| F-statistic from first stage | 15 | 64 | 11 | 12 |
Notes: All standard errors robust to heteroskedasticity and clustered within nursing home. For Katrina, the instrumental variables included a quartic polynomial in the perpendicular distance from facility to path of storm 48 hours, and elevation. For Gustav, perpendicular distance from facility to path of storm 24, 48, and 72 hours before landfall, elevation, and a cubic polynomial in the distance from the home to the shore. For Rita, the instrumental variables were perpendicular distance from facility to path of storm 48 hours before landfall, elevation, and the maximum wind speed at the points where perpendicular lines from the nursing home intersects the line depicting the 24 and 72 hour (before landfall) paths respectively. Finally, for Ike, the instrumental variables were the perpendicular distance from facility to path of storm 48 hours before landfall and 72 hours before landfall, distance from facility to shore, and the square of that distance.
To estimate the effects of storm intensity on outcome for those sheltering in place, we assumed that those closer to the center of the storm experienced more of an effect than did those who were further away. Given that hurricanes are actually strongest in the northeast quadrant of the storm, we modeled distance as either east or west of the storm.
We also compare the relative magnitude of the evacuation coefficient with other more meaningful clinical measures. For example, we test the equality of the evacuation coefficient (estimated coefficient on evacuation) and (say) (estimated coefficient for coronary heart failure). A failure to reject the equality of coefficients suggests that we cannot reject the null hypothesis that evacuation had the same effect on the outcomes (mortality/ hospitalization rates) as the presence of coronary heart failure.
The estimated value of the coefficient of evacuation was reasonably stable across alternate formulations of the first stage instruments, although the confidence intervals around the evacuation variable varied with the instrumental variables used. Nonetheless, the instrumental variable coefficient was very robust to the configuration of independent variables included in the second-stage. In the case of Katrina, a substantial number of homes evacuated after the storm’s landfall. While the results shown in Table 2 were based upon the original decision (pre-evacuation), the estimated model also included a dummy variable if the home was evacuated after landfall. This latter coefficient was also significantly related to the outcomes. We conducted additional sensitivity analyses dropping the post-evacuation dummy variable, and found that the pre-evacuation coefficient roughly doubles- reflecting the tautological correlation between pre- and post-evacuation status. Statistical measurements were conducted using SAS 9.3 and STATA 11.0
RESULTS
A total of 36,389 residents were exposed to one of the 4 storms. Table 1a presents the descriptive characteristics of the exposed cohorts for each of the 2005 storms compared to the non exposed cohorts residing at the same facility in the 2 years prior. Table 1b presents the same descriptive characteristics for the 2008 storms, as compared to cohorts in the same homes in the prior two years when no significant hurricanes occurred in the region. For each storm, the characteristics of the exposed cohorts were statistically similar to the non-exposed cohorts with the exception of a statistically signficant increase in the percentage of moderate dementia cases (Cognitive Performance Scores of 3-4) among those exposed to Hurricanes Katrina, Rita, and Gustav.
Table 1a.
Baseline Demographics and Health Characteristics of Long-Stay Nursing Home Residents among the Three Cohorts for the 2005 Storms
| Resident Characteristics | HURICANE KATRINA | HURICANE RITA | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-Exposed | Exposed | Non-Exposed | Exposed | |||||
| 2003 Cohort (N=9589) |
2004 Cohort (N=9475) |
2005 Cohort (N=9056) |
P-value* | 2003 Cohort (N=11491) |
2004 Cohort (N=11945) |
2005 Cohort (N=11521) |
P- value* |
|
| Demographics: | ||||||||
| Female | 75.3 | 75.2 | 75.6 | 0.776 | 75.8 | 75.7 | 75.4 | 0.741 |
| Age: | 0.336 | 0.750 | ||||||
| 65-74 | 17.9 | 17.8 | 18.8 | 17.9 | 17.7 | 18.4 | ||
| 75-84 | 38.8 | 39.0 | 39.0 | 38.4 | 38.5 | 38.5 | ||
| 85+ | 43.3 | 43.1 | 42.2 | 43.7 | 43.8 | 43.2 | ||
| Race/ethnicity: | 0.860 | 0.001 | ||||||
| Caucasian | 77.1 | 77.0 | 76.4 | 76.4 | 75.7 | 74.1 | ||
| Black | 21.5 | 21.6 | 22.1 | 18.3 | 18.9 | 19.9 | ||
| Hispanic | 1.0 | 0.9 | 1.0 | 4.4 | 4.3 | 4.7 | ||
| Other | 0.4 | 0.5 | 0.5 | 0.9 | 1.1 | 1.3 | ||
| Comorbidities: | ||||||||
| CHESS Comorbidity | 0.99±1.04 | 1.02±1.05 | 1.03±1.06 | 0.052 | 0.86±1.03 | 0.86±1.02 | 0.84±1.00 | 0.139 |
| Index (0-5) | ||||||||
| ADL Scale (0-28) | 15.1±9.6 | 15.1±9.5 | 15.1±9.5 | 0.950 | 15.4±9.7 | 15.2±9.6 | 15.3±9.5 | 0.305 |
| CPS Scale | <0.001 | <0.001 | ||||||
| 0-2 | 40.0 | 39.2 | 38.0 | 40.2 | 40.1 | 39.6 | ||
| 3-4 | 37.6 | 39.5 | 40.9 | 36.1 | 37.4 | 39.1 | ||
| 5-6 | 22.4 | 21.3 | 21.1 | 23.7 | 22.5 | 21.3 | ||
Table 1b.
Baseline Demographics and Health Characteristics of Long-Stay Nursing Home Residents among the Three Cohorts for the 2008 Storms
| Resident Characteristics | HURICANE GUSTAV | HURICANE IKE | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-Exposed | Exposed | Non-Exposed | Exposed | |||||
| 2006 Cohort (N=7091) |
2007 Cohort (N=6914) |
2008 Cohort (N=6464) |
P-value* | 2006 Cohort (N=10596) |
2007 Cohort (N=9595) |
2008 Cohort (N=9348) |
P-value* | |
| Demographics: | ||||||||
| Female | 74.1 | 73.6 | 72.8 | 0.244 | 73.9 | 73.5 | 73.7 | 0.853 |
| Age: | 0.132 | 0.328 | ||||||
| 65-74 | 18.1 | 18.6 | 19.5 | 17.6 | 18.6 | 18.6 | ||
| 75-84 | 39.3 | 38.5 | 37.4 | 38.7 | 37.8 | 38.0 | ||
| 85+ | 42.6 | 42.9 | 43.1 | 43.7 | 43.6 | 43.5 | ||
| Race/ethnicity: | 0.520 | 0.513 | ||||||
| Caucasian | 79.8 | 79.0 | 78.7 | 69.0 | 68.5 | 67.8 | ||
| Black | 18.4 | 19.1 | 19.0 | 17.8 | 18.1 | 18.2 | ||
| Hispanic | 1.1 | 1.1 | 1.4 | 11.7 | 12.1 | 12.5 | ||
| Other | 0.7 | 0.8 | 0.9 | 1.5 | 1.4 | 1.4 | ||
| Comorbidities: | ||||||||
| CHESS Comorbidity | 0.88±1.02 | 0.88±1.01 | 0.87±0.99 | 0.982 | 0.86±1.03 | 0.85±1.02 | 0.83±1.00 | 0.146 |
| Index (0-5) | ||||||||
| ADL Scale (0-28) | 14.4±9.2 | 14.7±9.2 | 14.6±9.2 | 0.065 | 15.4±9.2 | 15.7±8.9 | 15.9±8.9 | 0.002 |
| CPS Scale | 0.002 | 0.092 | ||||||
| 0-2 | 41.5 | 39.9 | 39.7 | 39.7 | 39.2 | 38.5 | ||
| 3-4 | 40.1 | 42.4 | 43.4 | 40.0 | 41.2 | 41.9 | ||
| 5-6 | 18.5 | 17.7 | 16.9 | 20.4 | 19.7 | 19.6 | ||
Chi-square test for categorical variables and one way AVOVA test of statistical significance for continuous variables; CHESS= The Changes in Health, End-stage disease and Signs and Symptoms Comorbidity Index; ADL=Activities of Daily Living; CPS=Cognitive Performance Scale
Mortality Rates
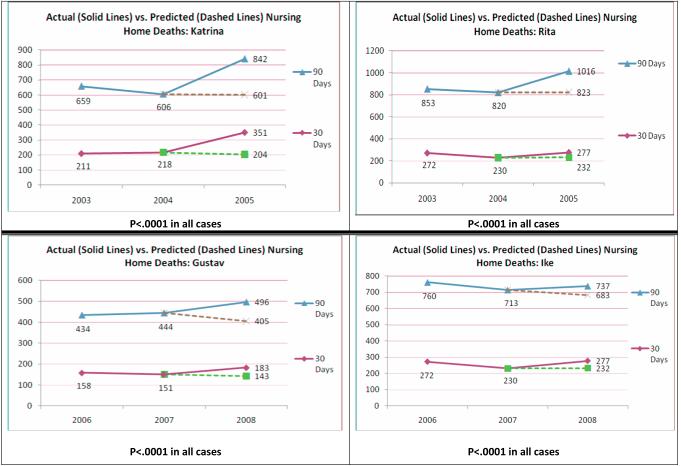
Figure 1 presents the actual versus predicted mortality rates among residents for each of the 4 storms at 30 and 90 days post hurricane. Predicted mortality was calculated as the simple average of the mortality rates at 30 and 90 days for non-exposure years multiplied by the number of residents during the exposure year. There were a cumulative total of 277 (7.6 per 1000) extra deaths at 30 days. At 90 days, a total of 579 (15.9 per 1000) extra deaths were observed. The additional mortality effects were sustained with multivariate adjustment for changes in case mix over the three year periods.
Figure 1.
Actual versus Predicted Mortality Rates Associated with Hurricane Exposure among Nursing Home Residents
Hospitalization Rates
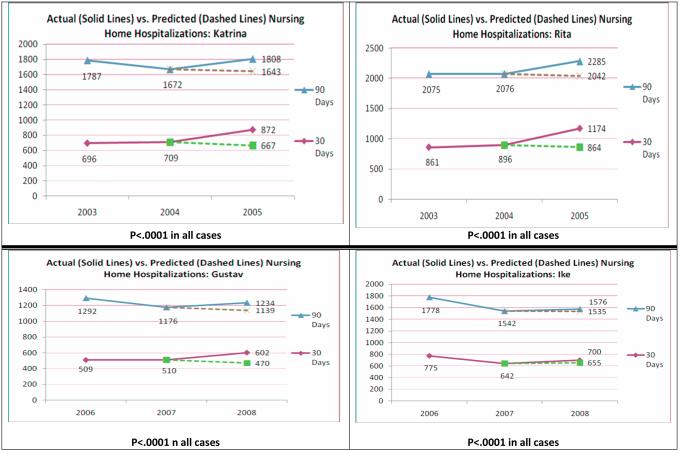
Figure 2 presents the hospitalization rate differences among residents in each of the three years for each of the 4 storms at 30 and 90 days post hurricane. There were a cumulative total of 872 (23.9 per 1000) extra hospitalizations at 30 days. At 90 days, 544 (14.9 per 1000) extra hospitalizations were observed. As with mortality, the additional hospitalizations observed among exposed residents were sustained despite case mix adjustment using multivariate regression.
Figure 2.
Actual versus Predicted Hospitalization Rates Associated with Hurricane Exposure among Nursing Home Residents
Sheltering versus Evacuation
Table 2 presents the estimated value of the instrumental variable coefficients. In general, the results suggest that evacuation led to more mortality and hospitalizations by 90 days relative to residents who sheltered in place. Mortality rates increased from 2.7% (Gustav) to 5.4% (Katrina) as a function of evacuation. Hospitalization rates also increased from 1.8% (Ike) to 8.3% (Katrina). Thirty day mortality and hospitalization rates relative to evacuation were also obtained and were generally consistent with the 90 day results.
In order to ascertain what these results meant clinically, we also compared the estimated effect of evacuation among patients with several commonly encountered medical conditions such as Congestive Heart Failure (CHF) and having a feeding tube in place. The results are also presented in Table 2 and suggest that the estimated effect of evacuation on mortality and morbidity was similar to the effects of having a CHF diagnosis and having a feeding tube in place. In results that can be obtained from the authors upon request, we also show that the effect of evacuation on outcomes is, in general, stronger than the effect of other co-morbid conditions such as diabetes, renal failure, obesity, and severe cognitive impairment.
DISCUSSION
While CMS regulations required a generic facility evacuation plan prior to Hurricane Katrina, NHs were rarely incorporated into regional emergency planning efforts. After the 2005 hurricane season, several government reports and research papers identified deficiencies in preparedness prompting a reevaluation of evacuation strategy.2, 5, 9, 26 Moreover, well publicized tragedies at several nursing homes severely affected by Hurricane Katrina increased public demand to protect frail elders through an “evacuate-all” stance during future perceived hurricane threats.27, 28 However well-intentioned this policy of universal evacuation is, this study demonstrates that there is a clear increase in hospitalization and mortality associated with the evacuation of frail elders up and above the effects of the storm itself.
This is not to say that these storms don’t have an adverse effect on the NH population. Each one of the four Gulf storms resulted in significant increases in morbidity and mortality. In aggregate, there were 277 additional hurricane-related deaths within 30 days of the four hurricane events. This translates to a rate of 7.6 additional deaths (over and beyond the normal death rate) per 1000 residents. Indicative of the sustain effect of being exposed to a storm, we observed that at 90 days post exposure, a total of 579 additional lives (an additional 15.9 deaths/1000) were lost. Importantly, deaths are not the only consequence and cost of evacuation. Among the survivors the rates of additional hospitalizations were also significant with 692 extra hospitalizations (19.0 additional hospitalizations per 1000 residents) at 30 days and 543 extra hospitalizations (14.9 per 1000 residents) at 90 days.
Nonetheless, given the current policy of universal evacuation, it is important to note that many of the deaths and hospitalizations occurred downstream from the immediate effects of the storm. For example, the Morbidity and Mortality Weekly Report estimated that there were 78 deaths of NH residents during Katrina.29, 30 Our data suggests that 147 Katrina-related deaths occurred within 30 days of landfall and 241 deaths occurred within 90 days when compared to death rates in the same homes during non-hurricane years. It is likely that many of these additional deaths went unnoticed—perhaps disguised by geography (many NH residents left the immediate area) or by nursing home residents’ already high rates of mortality.
Looking across all four storms, our data suggests that the act of evacuation itself compounded morbidity and mortality. Based on instrumental variable analysis, the increased risk of death due to evacuation ranged from nearly 2.7 to 5.3% for the 4 storms at 90 days. Evacuation also increased hospitalization from 1.8 to 8.3% at 90 days independent of other factors. These findings strongly suggest a need to reconsider the current mass evacuation standard which has emerged since the 2005 storms. While it is important to ensure that NH residents are kept out of “harm’s way”, having all residents evacuate prior to each hurricane appears to have its own consequences. For example, a total of 119 facilities (82% of those identified as “at risk”) evacuated the Gulf region for Hurricane Gustav—a storm that eventually had relatively minimal impact on land. It is reasonable to suppose and our statistical modeling confirms, that many of the excess deaths and hospitalizations that occurred relative to earlier years were attributable to evacuation and not the relatively minor storm effects. Since it is not unusual for storms to weaken as they approach landfall or change direction, the future impact of universal evacuation policies on frail elderly persons when such “false alarms” occur could cumulatively be far greater than the effect of the storms themselves. However, since such transfer trauma deaths would not be as dramatic as those directly caused by a storm, the effects would be much more subtle, although still considerable.
Obviously, some evacuations are appropriate given storm severity and facility location. Residents that are at highest risk for storm surge flooding should certainly evacuate. Facilities that are likely to be affected by the stronger, easterly side of Category 3, 4, and 5 hurricanes should also probably evacuate. Future research is needed, however, to better understand which aspects of evacuation (e.g. distance evacuated, transit time, receiving facility capacity, etc.) are associated with increased resident morbidity/mortality in order to minimize future transfer trauma. Furthermore, identifying residents most likely to experience adverse outcomes due to evacuation (e.g. dialysis patients, residents with congestive heart failure, etc.) might prompt earlier efforts to evacuate such individuals, leaving the facility more time to decide whether to evacuate more robust patients more proximal to landfall.
Lastly, the findings from this study raise the question of whether NHs that care for frail elders should be rebuilt in areas prone to frequent hurricane evacuation.31-33 Given that the evacuation of NH residents during storms is linked to increased morbidity and mortality, the policy to allow construction of facilities in flood-prone areas at high risk for storm surge damage should be reexamined.
Limitations
There are several limitations to this research. First, the geographic region outlined in this study was intended to capture the effects of each storm individually. Although, these storms were largely distinct, there is some overlap in Western Lousiana where outcomes experienced by residents exposed to Rita might also reflect some previous exposure to Katrina. Secondly, it is well known that there are geographic differences (e.g. differential flu rates, etc.) that account for changes in annual mortality/morbidity rates. Though unlikely--due to similarities in the non exposure and exposure cohorts during the 90 day prestorm period and the results of our instrumental variable approach, it is possible that some other unmeasured confounders might have contributed to adverse outcomes during exposure years. Additionally, some of the increases in mortality/morbidity might be partially attributable to the regional disruption in the health care system that occurred following Katrina. Determining how much of the mortality/morbidity was related to the storm and how much was related to the disruption in health care that followed is not possible. Nevertheless, we did find that evacuation related morbidity and mortality remained present for storms (e.g. Hurricane Rita and Gustav) where core infrastructure was not as affected.
Finally, our estimates of morbidity and mortality measured the effects of the evacuation decision on all residents of the facility. It was generally assumed that residents remained with their homes (unless they were discharged) and that the homes that evacuated moved these residents to safer places where they were not as severely affected by the intensity of the storm. Although we know of no case reports in the press where residents of an evacuating facility were moved to a more dangerous locations (i.e. moving into the storm), this assumption cannot be directly tested because of the lack of data about the location of individual residents during the days that followed the storm.
CONCLUSION
Frail NH residents are adversely affected by hurricane disasters. While there is significant increased morbidity and mortality related to exposure, there is added risk in evacuation. While it is important that facilities, public health and emergency management officials evacuate homes likely to flood during a hurricane, in light of the significant increase in mortality and morbidity associated with evacuation, the policy of universal evacuation of facilities requires careful reconsideration.
Acknowledgements
This project was supported in part by grants from the National Institutes of Aging (RO1AG030619-01A2) and the Veteran’s Administration HSR&D (Dosa-CDA-08-280), and the John A. Hartford Foundation (#2006-0172).
Funding Agencies: National Institutes of Aging (RO1AG030619-01A2); Veteran’s Administration HSR&D (CDA 08-280); John A. Hartford Foundation (#2006-0172)
Footnotes
Based on data obtained directly from the Texas Department of Aging & Disability Services, Mississippi Department of Health, and the Lousiana Department of Health and Hospitals.
None of the authors report conflicts of interests related to this research. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. All authors had key roles all aspects of the study from design to manuscript preparation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dosa D, Hyer K, Brown L, Artenstein A, Polivka-West L, Mor V. The Controversy Inherent in Managing Frail Nursing Home Residents during Complex Hurricane Emergencies. J Am Med Dir Assoc. 2008;9:599–604. doi: 10.1016/j.jamda.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 2.United States Government Accountability Office Disaster preparedness: Limitations in federal evacuation assistance for health facilities should be addressed. Report to Congressional Committees. Jul, 2006. pp. 1–52. In: GAO-06-826.
- 3.Blanchard G, Dosa D. A Comparison of the Nursing Home Evacuation Experience between Hurricanes Katrina (2005) and Gustav (2008) J Am Med Dir Assoc. 2009;10:639–43. doi: 10.1016/j.jamda.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dosa D, Feng Z, Hyer K, Brown LM, Thomas K, Mor V. The Effects of Hurricane Katrina on Nursing Home Resident Mortality, Hospitalizations and Functional Decline. Disaster Med Public Health Prep. 2010;4:1–5. doi: 10.1001/dmp.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of Inspector General Nursing home emergency preparedness and response during recent hurricanes: OEI-06-06-00020. Aug, 2006. Report No.: OEI-06-06-00020.
- 6.Eldar R. Vulnerability of disabled and elderly in disasters: case-study of Israel during ‘Desert Storm’. Medicine & War. 1991;7:269–74. doi: 10.1080/07488009108409002. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez LS, Byard D, Lin CC, et al. Frail elderly as disaster victims: emergency management strategies. Prehospital & Disaster Medicine. 2002;17:67–74. doi: 10.1017/s1049023x00000200. [DOI] [PubMed] [Google Scholar]
- 8.Hyer K, Brown LM, Berman A, Polivka-West L. Establishing And Refining Hurricane Response Systems For Long-Term Care Facilities. Health Affairs. 2006;25:w407–11. doi: 10.1377/hlthaff.25.w407. [DOI] [PubMed] [Google Scholar]
- 9.Root ED, Amoozegar JB, Bernard S. Nursing Homes in Public Health Emergencies: Special Needs and Potential Roles. Agency for Healthcare Research and Quality; Rockville, MD: 2007. Prepared by RTI International under Contract No. 290-00-0018. AHRQ Publication No. 07-0029-1. [Google Scholar]
- 10.Capezuti E, Boltz M, Renz S, Hoffman D, Norman RG. Nursing home involuntary relocation: clinical outcomes and perceptions of residents and families. J Am Med Dir Assoc. 2006;7:486–92. doi: 10.1016/j.jamda.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Intrator O, Berg K, Hiris V, et al. Development and validation of the Medicare-MDS Residential History File. Gerontologist. 2003;43:30–1. [Google Scholar]
- 12.Intrator O, Hirris J, Berg K, Miller SC, Mor V. The Residential History File: Studying Nursing Home Residents’ Long-Term Care Histories. Health Serv Res. 2011;46:120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris JN, Hawes C, Fries BE, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30:293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed February 20, 2010];National Weather Service JetStream Online School for Weather:Learning Lesson: Quadraphonic Wind. 2010 at http://www.srh.noaa.gov/jetstream/tropics/ll_quadwind.htm.
- 15. [Accessed February 9, 2011];NOAA’s Coastal Geospatial Data Project. at http://coastalgeospatial.noaa.gov/back_gis.html.
- 16. [Accessed February 9, 2011];WorldClim - Global Climate Data. at http://worldclim.org/current.
- 17. [Accessed Febuary 11, 2011];National Hurricane Center Archive. 2011 at http://www.nhc.noaa.gov/archive/
- 18.Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. Journal of Gerontology. 1994;49:M174–82. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 19.Morris JN, Fries BE, Morris SA, Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1999;54:M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 20.Hirdes JP, Frijters DH, Teare GF. The MDS-CHESS Scale: A New Measure to Predict Mortality in Institutionalized Older People. J Am Geriatr Soc. 2003;51:96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- 21.Mcclellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? analysis using instrumental variables. JAMA. 1994;272:859–66. [PubMed] [Google Scholar]
- 22.Newhouse JP, McClellan M. Econometrics in outcomes research:the use of instrumental variables. Annu Rev Public Health. 1998;19:17–34. doi: 10.1146/annurev.publhealth.19.1.17. [DOI] [PubMed] [Google Scholar]
- 23.Xian Y, Holloway RG, Chan PS, et al. Association Between Stroke Center Hospitalization for Acute Ischemic Stroke and Mortality. JAMA. 2011;305:373–80. doi: 10.1001/jama.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hansen L. Large sample properties of the generalized method of moments estimators. Econometrica. 1982;50:1029–54. [Google Scholar]
- 25.Feng Z, Grabowski DC, Intrator O, Mor V. The effect of state medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006;41:1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dosa DM, Grossman N, Wetle T, Mor V. To evacuate or not to evacuate: lessons learned from Louisiana nursing home administrators following Hurricanes Katrina and Rita. J Am Med Dir Assoc. 2007;8:142–9. doi: 10.1016/j.jamda.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Harris G. In NH, a Fight Lost to Rising Waters. New York Times. 2005 September 7; Sect. A1. [Google Scholar]
- 28.Hull A, Struck D. At NH, Katrina Dealt Only the First Blow. Washington Post. 2005 September 23;:A01. [Google Scholar]
- 29.Brunkard J, Namulanda G, Ratard R. Hurricane Katrina deaths, Louisiana, 2005. Disaster Med Public Health Prep. 2008;2:215–23. doi: 10.1097/DMP.0b013e31818aaf55. [DOI] [PubMed] [Google Scholar]
- 30.CDC Public Health Response to Hurricanes Katrina and Rita --- Louisiana, 2005. MMWR. 2006;55:29–30. [PubMed] [Google Scholar]
- 31. [Accessed March 15, 2011];Chateau De Notre Dame Nursing Home Recuperates From Katrina With Help From Fema Fund. 2007 at http://www.fema.gov/news/newsrelease.fema?id=34915.
- 32. [Accessed March 15, 2011];St. Margaret’s Daughters’ Nursing Home Reopens 2007. at http://www.fema.gov/news/newsrelease.fema?id=40372.
- 33. [Accessed March 15, 2011];Additional Millions Provided To Rebuild Orleans Nursing Home. 2009 at http://www.fema.gov/news/newsrelease.fema?id=49357.