Abstract
Parental feeding practices have been associated with children’s weight status, but results have been inconsistent across populations. Research is needed to elucidate the relationship between parental feeding practices and adiposity in diverse populations. The present study tested if: (1) parental feeding practices differed by race/ethnicity (2) parental pressure to eat and parental restriction were associated with adiposity levels, and (3) to investigate the relationship between parental feeding practices and/or child adiposity with socioeconomic status (SES). Structural equations modeling was conducted to test the model in 267 children aged 7–12 years self-identified as African American (AA), European American (EA), or Hispanic American (HA) from economically diverse backgrounds. Dual energy X-ray absorptiometry and Computed Tomography scanning were used to determine body composition and abdominal fat distribution, respectively.
Parental restriction was a significant predictor of child adiposity while parental pressure to eat had an inverse relationship with child adiposity. HA parents reported significantly higher levels of restriction and pressure to eat, whereas EA parents reported the lowest. SES was positively associated with child adiposity and inversely related to parental restriction and pressure to eat.
Thus, parental feeding practices differ across racial/ethnic groups and SES and may contribute to population differences in child adiposity.
Keywords: obesity, restriction, pressure to eat, fat, race, ethnicity, diverse, admixture
Introduction
The prevalence of childhood obesity has been increasing over the last thirty years, with the most recent reports indicating an increase in both the degree and severity (Ogden et al., 2010). Research indicates that obese children are more likely to become obese adults (Magarey et al., 2003), and this tracking of pediatric obesity into adulthood may have detrimental implications for long term health (Field et al., 2001; Whitaker et al., 1997; Magarey et al., 2003).
Parental beliefs and practices regarding child feeding play a significant role in shaping eating behaviors. Parental feeding practices, particularly restriction of palatable foods and pressure to eat, have been related to children’s body weight and energy intakes. Parental restriction has been positively related with child body mass index (BMI), overeating, and weight gain (Fisher & Birch, 2002; Francis et al., 2001; Joyce & Zimmer-Gembeck, 2009; Birch & Fisher, 2000; Faith et al., 2004). It has been hypothesized that parental restriction may limit a child’s ability to self regulate energy intake and focus children’s attention on restricted foods, which may lead to overconsumption when the restricted foods become freely available (Fisher JO & Birch L.L., 1999). In contrast, parental pressure to eat has been associated with decreased preference and consumption of the pressured food, lower fruit and vegetable intake, picky eating, and lower weight in children (Galloway AT et al., 2005; Galloway et al., 2006). However, the relationships between parental feeding practices and adiposity are not consistent across studies. Studies from Australia and the United Kingdom have found no association between parental restriction and child weight (Webber et al., 2010; Campbell et al., 2010; Carnell & Wardle, 2007) and longitudinal studies have shown no association between pressure to eat and child adiposity measures (Webber et al., 2010; Spruijt-Metz et al., 2006). Although it has been theorized that parental beliefs and practices may be modifiable determinants to prevent pediatric obesity and excessive adiposity (Savage J.S. et al., 2007), it is evident that the relationships between parental feeding practices and risk for obesity in children are complex, and do not appear to carry the same effect among all individuals.
The etiology of reported marked differences in obesity prevalence among members of diverse racial/ethnic groups in the United States is not clearly understood (Flegal et al., 2010). Research aimed at understanding the role of parental feeding practices in diverse populations, including those with lower socio-economic status (SES), is limited and the contribution of SES to child feeding practices remains inconclusive (Mulder et al., 2009; Webber et al., 2010; Carnell & Wardle, 2007; Hennessy et al., 2010; Spruijt-Metz et al., 2006; Spruijt-Metz et al., 2002). As minority and low-income populations continue to be disproportionately affected by overweight and obesity (Shrewsbury & Wardle, 2008; Ogden et al., 2010), clarifying the contribution of SES to parental feeding practices in minority and low-income populations will be important in developing interventions and treatment for pediatric obesity.
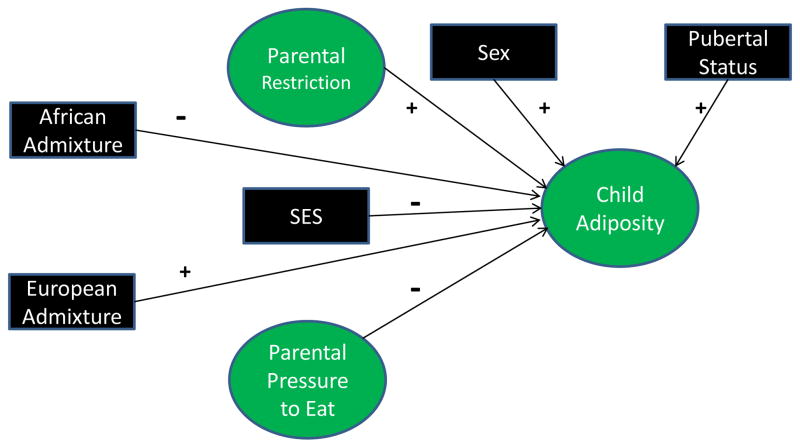
The objectives of this study were to test a model that focuses on the relationship between parental feeding practices on child adiposity in a socioeconomically and ethnically diverse population (Figure 1). This model is based on prior research in a homogenous sample (Fisher J.O. & Birch L.L., 1999; Fisher & Birch L.L., 2002; Galloway et al., 2006) and was inspired by the Social Determinants of Health and Environmental Health Promotion model (Schulz & Northridge, 2004). We hypothesized that (1) parental feeding practices would differ by race/ethnicity, (2) parental pressure to eat would be inversely associated and parental restriction would be positively associated with adiposity levels, and (3) SES would be inversely associated with parental restriction, pressure to eat, and/or child adiposity in a multi-ethnic sample of children from economically diverse backgrounds.
Figure 1.
Theoretical model depicting influences of parental feeding practices and socioeconomic status with child adiposity.
Methods
Subjects
This paper utilizes secondary data analysis from a cross-sectional study evaluating genetic and environmental factors underlying pediatric racial/ethnic differences in body composition and insulin-related outcomes. Participants were 267 children aged 7–12 years self-identified as AA (n=91), EA (n=116), or HA (n=60) from the Birmingham, Alabama area. Children were recruited at schools, churches, health fairs, and through newspapers, parent magazines, radio, and participant referrals. The children were peripubertal (pubertal stage ≤3 as assessed by a pediatrician according to the criteria of Marshall and Tanner) (Marshall WA & Tanner JM, 1969; Marshall WA & Tanner JM, 1970), and had no medical diagnosis or medications contraindicated for study participation (i.e. medication known to affect body composition, metabolism, cardiac function). Prior to study participation, the children and parents provided informed assent and consent, respectively, to the protocol, which was approved by the Institutional Review Board for human subjects at the University of Alabama at Birmingham. All measurements were performed at the General Clinical Research Center (GCRC) and the Department of Nutrition Sciences at the University of Alabama at Birmingham between 2005 and 2008.
Protocol
Subjects participated in two visits. On the first visit, pubertal status, anthropometric assessment, questionnaire data, and body composition were measured. Within thirty days the children and their parents returned for the second visit, where blood for genetic admixture analysis was drawn.
Anthropometric measures
Anthropometric measurements for all participants were obtained by the same registered dietitian. Participants were weighed (Scale-tronix 6702W; Scale-tronix, Carol Stream, IL) to the nearest 0.1 kg (in minimal clothing without shoes). A single measure of height was recorded to the nearest 0.1 cm without shoes using a digital stadiometer (Heightronic 235; Measurement Concepts, Snoqualmie, WA). Children’s BMI-for-age percentiles were calculated as indicated by the Center for Disease Control and Prevention guidelines (Kuczmarski RJ et al., 2002).
Body Composition and Fat Distribution
Body composition was measured by dual-energy x-ray absorptiometry (DXA) using a GE Lunar Prodigy densitometer (GE LUNAR Radiation Corp., Madison, WI). Participants were scanned in light clothing, while lying flat on their backs with arms at their sides. DXA scans were performed and analyzed with pediatric software encore 2002 version 6.10.029. DXA has been found to be highly reliable for body composition assessment in children (Elberg et al., 2004). For the purpose of this study, only trunk fat (kg) was used in the analysis. Total abdominal adipose tissue (TAAT; cm2) was measured by computed tomography (CT) scanning with a HiLight/Advantage Scanner (General Electric, Milwaukee) as previously described (Kekes-Szabo T et al., 1994). A 5mm abdominal scan was taken at the level of the umbilicus. Scans were analyzed for cross-sectional area (cm2) of adipose tissue using the density contour program with Hounsfield units for adipose tissue set at −190 to −30. CT has been shown to provide accurate measurements of body fat distribution in children (Fox K et al., 1993). The indicators of total abdominal adipose tissue, trunk fat mass, and BMI-for-age percentile were chosen for the Child Adiposity latent construct because they have been related to metabolic outcomes and obesity in children and adults (Bjorntorp P, 1988; Rexrode K et al., 1998; Casazza K et al., 2009; Edyta Suliga, 2009; Magarey et al., 2003).
Parental Feeding Practices
The Child Feeding Questionnaire (CFQ) was developed by Birch et al. to measure parental feeding practices in EA children (Birch et al., 2001) and has been used previously in children of this age group (Spruijt-Metz et al., 2006; Campbell et al., 2010; Spruijt-Metz et al., 2002). For this study, the modified CFQ was given, which used questions from the original CFQ which were validated for use in HA and AA (Anderson et al., 2005). Restriction and pressure to eat were measured by a five-point Likert scale and responses ranged from agree (coded as a 5) to disagree (coded as a 1). The questions measuring parental restriction (RES1a, RES1b, and RES4a) were “I have to make sure my child does not eat too many sweets”, “I have to be sure that my child does not eat too many high fat foods”, and “I have to be sure that my child does not eat too much of his/her favorite foods”, respectively. The questions measuring “pressure to eat” (PE1, PE2, and PE3) were “My child should always eat everything on his/her plate”, “I have to be especially careful to make sure my child eats enough”, and “If I did not guide or regulate my child’s eating, he/she would eat much less than he/she should”, respectively. Higher scores are indicative of higher engagement in feeding practices while low scores reflect little participation in child feeding practices. All parents participated in the questionnaire, and the Cronbach alpha for restriction and pressure to eat were 0.83 and 0.69, respectively.
Socioeconomic Status
Socioeconomic status was measured with the Hollingshead 4-factor index of social class (Hollingshead AB, 1975), which combines the educational attainment and occupational prestige for working parents in the child’s family. Scores range from 8 to 66, with higher scores indicating higher theoretical social status.
Pubertal Status
Tanner staging is an objective measure of pubertal development. Direct observation for the assessment of pubertal stage by the same pediatrician, was used for differentiating among the five stages of maturity (Marshall WA & Tanner JM, 1969; Marshall WA & Tanner JM, 1970). The staging based on the criteria of Marshall and Tanner is according to both breast and pubic hair development in girls and genitalia and pubic hair development in boys. One composite number is assigned for Tanner staging, representing the higher of the two values defined by breast/genitalia and pubic hair development (Malina RM & Bouchard C, 1991). Given that pubertal stage and biological sex plays a role in adiposity accrual and distribution (Goulding et al., 1996; Demerath et al., 2006), both were included as covariates in the analysis.
Genetic admixture
Genetic admixture more accurately reflects genetic components of race/ethnicity than self-report (Fernandez & Shriver, 2004) and has been shown to influence body composition in children (Cardel et al., 2011; Casazza K et al., 2010). We used estimates of ancestral genetic admixture to adjust for the genetic contribution to body composition. Genetic admixture estimates were obtained for each child’s blood sample from genotyping ~142 ancestry informative markers (AIMs) across the human genome for European, African and Amerindian parental ancestry. Genotyping for the measures of genetic admixture was performed at Prevention Genetics (www.preventiongenetics.org) using the McSNP method and agarose gel electrophoresis, as previously described (Cardel et al., 2011). Individual admixture estimates were derived using maximum likelihood (ML) method, which estimate the proportion of genetic ancestry for each individual, using a range of proportions from 0 to 1 and identifies the most probable value of admixture based on the observed genotypes, as previously described (Fernandez & Shriver, 2004; Shaffer JR et al., 2007).
Statistical Analysis
Correlations were conducted for all variables of interest and descriptive statistics were analyzed among ethnic groups using analysis of variance (ANOVA) with Tukey’s post-hoc analysis. The normality of the distribution of values was evaluated and non-normal variables were log-transformed. Means for restriction and pressure to eat between ethnic groups were analyzed with analysis of covariance (ANCOVA). The covariates are child sex, pubertal status (as assessed by tanner), African admixture, and European admixture. All above analyses were done using Statistical Analysis Software (SAS; version 9.1).
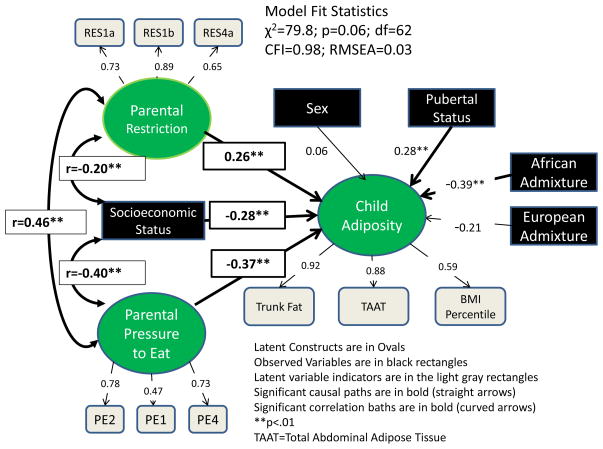
Structural equations modeling (SEM) using Mplus software (Muthen and Muthen, Los Angeles, CA) with ML estimation was used to model the relationships between parental feeding practices, SES, and child adiposity. SEM allows for latent variables and for simultaneous evaluation of multiple regression equations, providing estimates of the direct and indirect effects, while adjusting for covariates and colinearity among all variables. In the model (Figure 3), ovals are shown to represent latent variables. The black boxes represent observed variables and the gray boxes represent the indicators used to measure the latent variables. Direct paths between the variables are indicated by single-headed arrows estimated by linear regression coefficients. Correlations between the variables are shown by double-headed arrows. Significance for all relationships was set a level of p≤0.05. Standard fit indices were used to test the fit of the model (Rex B.Kline, 2005): chi-square (χ2) test of model fit, its p-value and degrees of freedom (df); CFI (comparative fit index; good fit is >0.90); and RMSEA (root mean square error of approximation; good fit is <0.05).
Figure 3.
Structural equations model investigating the effects of parental feeding practices and socioeconomic status on child adiposity
Results
Parental and Child Characteristics
Descriptive statistics are reported in {Table 1}. Socioeconomic status differed by race/ethnicity with EA having the highest level and HA having the lowest level. Indices of child adiposity differed by groups with HA children having a higher BMI-forage percentile, greater TAAT, trunk fat mass, total fat, and percent fat when compared to EA and AA children. AA children had greater lean mass and were reproductively more mature relative to EA and HA children. A correlation matrix of key variables is described in {Table 2}.
Table 1.
Descriptive characteristics by racial/ethnic groups (mean, SD or n%)
| AA (n=100) | EA (n=119) | HA (n=86) | |
|---|---|---|---|
| Age (y) | 9.7 (1.4) | 9.7(1.6) | 9.4 (1.5) |
| % Female | 45.3 | 48.4 | 47.7 |
| Tanner 3 (%) | 23.6a | 7.4b | 9.3b |
| SES | 38.2 (10.7)b | 49.0 (9.8)a | 26.0 (12.1)c |
| BMI % | 63.0 (27.7)b | 59.7 (27.1)b | 77.2 (19.5)a |
| % fat | 20.5 (9.6) b | 22.3 (8.4) b | 28.2 (8.4) a |
| TAAT (cm2) | 10.6 (9.5)b | 12.1 (9.4)b | 16.5 (8.4)a |
| EUADM | 0.15±0.01c | 0.96±0.01a | 0.35±0.02b |
| AFADM | 0.82±0.01a | 0.01±0.00c | 0.09±0.01b |
superscripts indicate significant differences among self-identified racial/ethnic category
EA=European American; AA=African American; HA=Hispanic American; SES=Socioeconomic status; BMI%=BMI-for-age percentile, TAAT=Total Abdominal Adipose Tissue; EURADM=European admixture; AFADM=African Admixture
Table 2.
Correlation Matrix between key variables
| RES | P2E | Trunk Fat | TAAT | BMI% | Sex | Tanner | AFADM | EUADM | SES | |
|---|---|---|---|---|---|---|---|---|---|---|
| RES | 1 | |||||||||
| P2E | 0.33* | 1 | ||||||||
| Trunk Fat | 0.16* | −0.08 | 1 | |||||||
| TAAT | 0.06 | −0.10 | 0.82* | 1 | ||||||
| BMI% | 0.17* | −0.02 | 0.55* | 0.53* | 1 | |||||
| Sex | 0.06 | 0.03 | 0.10 | 0.17** | −0.01 | 1 | ||||
| Tanner | 0.08 | 0.01 | 0.28* | 0.14 | 0.09 | 0.17* | 1 | |||
| AFADM | 0.14* | 0.19** | −0.12 | −0.20* | −0.02 | −0.01 | 0.29* | 1 | ||
| EUADM | −0.34* | −0.43* | −0.02 | 0.05 | −0.12 | 0.01 | −0.24* | −0.81* | 1 | |
| SES | −0.20* | −0.40* | −0.21* | −0.18** | −0.23* | 0.01 | −0.06 | −0.15** | 0.50* | 1 |
Res=Restriction construct; P2E=Pressure to Eat construct; TAAT=Total abdominal adipose tissue; BMI%=BMI-for-age percentile; AFADM=African Admixture; EUADM=European Admixture; SES=Socioeconomic Status
p<0.05
p<0.01
Parental feeding practice scores by race/ethnicity are described in {Figure 2}. HA parents reported significantly higher levels of restriction and pressure to eat, whereas EA parents reported the lowest levels of restriction and pressure to eat.
Figure 2.
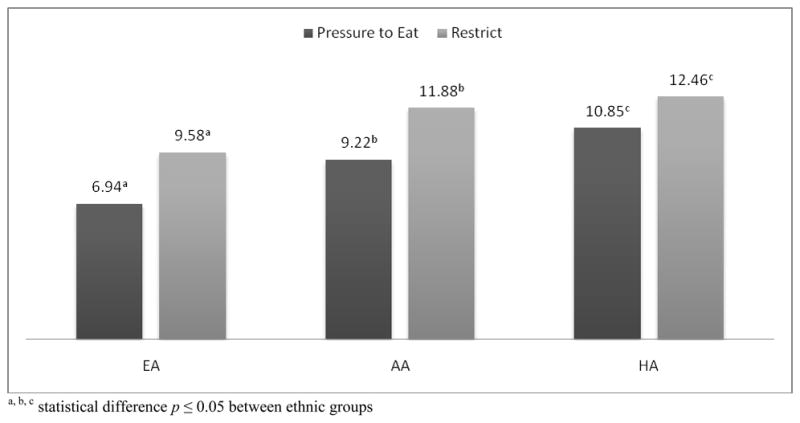
Mean Parental Feeding Questionnaire Scores by race/ethnicity
SEM Model
The generally accepted statistical fit cutoffs (Rex B.Kline, 2005), indicate that the model was a good fitting model (χ2=79.80, df=62, p=0.06, CFI=0.98, RMSEA=0.03) {Figure 3}. Pubertal status and AFADM were significant covariates in the model. Child sex and EUADM were not significant predictors of Child Adiposity, when accounting for all other pathways in the model.
The standardized parameter estimates after adjustment for all other covariates in the model are displayed in {Figure 3}. These standardized path coefficients can be interpreted the same way one would interpret standardized β weights in regression analyses. Restriction was a significant predictor of child adiposity (β=0.26, p<0.0001), meaning that a 1 standard deviation (SD) shift in Restriction would result in a 0.26 SD increase in Child Adiposity, after adjusting for the contributions of genetic admixture, SES, child sex, and pubertal status. Pressure to Eat was inversely associated with Child Adiposity (β=−0.37, p=<.0001), where a 1 SD increase in Pressure to Eat results in a 0.37 SD decrease in Child Adiposity, after controlling for all other factors in the model. There was a significant correlation between Pressure to Eat and Restriction (r=0.46; p<.0001). SES was inversely associated with Child Adiposity (β=0–.28, p<.0001), where a 1 SD increase in SES resulted in a −0.28 SD shift in Child Adiposity, after adjusting for all other predictors. SES was inversely associated with both Pressure to Eat (r=−0.40; p<.0001) and Restriction (r=−0.20; p<.0001).
Discussion and Conclusions
The overall purpose of this study was to investigate whether parental feeding practices differed by race/ethnicity and evaluate the effects of parental feeding practices and SES on child adiposity. Our findings indicate that parental feeding practices differ across racial/ethnic groups, and parental pressure to eat and restriction were associated with adiposity levels. Compared with children of higher SES, the use of controlling parental feeding practices was more prevalent in lower SES homes.
Pressure to eat has been reported to cause chaos and stress during mealtimes and to negatively impact children’s associations with food (Galloway et al., 2006). Given that negative associations with food may influence eating behavior and child weight, investigating whether pressure to eat contributes to child adiposity is paramount. Children that are pressured to eat at mealtimes tend to eat less and make more negative comments about food than meals where pressure to eat does not occur (Galloway et al., 2006). Previous research has shown that pressure to eat may not be limited to an acute response and has long term effects that promote picky eating, food aversions, and lower fruit and vegetable consumption during childhood and young adulthood (Batsell et al., 2002; Batsell & Brown, 1998; Galloway et al., 2005). Although studies have detailed the influence of pressure to eat and how this impacts eating behavior, studies investigating the relationship of these factors to BMI are inconsistent. Studies in children from European descent have reported that pressure to eat was correlated with decreased child BMI-for-age percentiles in the United States, (Faith et al., 2004; Matheson et al., 2006; Savage J.S. et al., 2007; Galloway et al., 2006) whereas in children from the United Kingdom no associations with weight were detected (Webber et al., 2010). These data suggest that the influence of pressure to eat on BMI in children may be mediated by cultural and/or geographical factors. While studies have found that pressure to eat is associated with decreased BMI (and, consequently, body weight), a different relationship has been observed with other adiposity measures, such as fat mass in EA children (Spruijt-Metz et al., 2006). To the extent that individual measurement of fatness is better represented by a latent variable for child adiposity, our results show that pressure to eat is related to decreased adiposity among multi-ethnic children.
Previous studies have used BMI-for-age percentiles as a surrogate for pediatric adiposity, and our results support the positive association between parental restriction and BMI-for-age percentiles reported (Fisher & Birch, 2002; Francis et al., 2001; Birch & Fisher, 2000; Faith et al., 2004). It has been hypothesized that controlling a child’s food intake may limit a child’s ability to self- regulate consumption by hindering hunger and satiety cues, potentially leading to eating in the absence of hunger (EAH) (Huon GF, 1994; Fisher & Birch, 2002; Fisher J.O. & Birch L.L., 1999). EAH has been associated with pediatric obesity (Moens et al., 2007), and longitudinal analysis in EA girls indicate higher parental restriction at age five relates to EAH by age seven and greater fat mass accrual over time (Fisher & Birch, 2002). However, it is important to note other studies have not found an association between parental restriction and child weight (Webber et al., 2010; Campbell et al., 2010; Carnell & Wardle, 2007; Gregory et al., 2010). A possible explanation for these observations may be that there is a bilateral relationship between child weight and parental restriction. In this context, parents are hypothesized to increase food restriction in children perceived to be at risk for overweight. Rifas-Shiman and colleagues have demonstrated that maternal restriction of food in children at one year of age was positively associated with child BMI at age three before, but not after, adjusting for weight for length at age one (Rifas-Shiman et al., 2011). These data support the hypothesis which relates parental restriction of food intake in infants who are already overweight. As researchers increase their understanding of factors relating behavioral practices to obesity prevention, it will be critical to explore how the complex relationships among parental feeding practices, adiposity, weight regulation and health risk factors interact with diverse contexts of culture, geographical locations and social class.
A most relevant aspect of this study is the inclusion of participants from various racial/ethnic groups with a broad range of socio-economic factors. Our study benefits from a multi-ethnic pediatric cohort and helps clarify the relationship between parental feeding practices and adiposity across diverse populations (Hennessy et al., 2010; Spruijt-Metz et al., 2006; Spruijt-Metz et al., 2002; Mulder et al., 2009). In our cohort, feeding practices differed across racial/ethnic groups, with HA parents reporting higher levels of Pressure to Eat and Restriction relative to AA and EA parents. Parental perceptions regarding appropriate child feeding has been shown to vary across groups, with some parents reporting concern about diet quality and others focusing on satiety (Sherry et al., 2004), and suggest that the underlying feeding/food related dynamics are different among HA, AA and EA parents. Furthermore, self-reported racial/ethnic classifications are complex and reflect biological and nonbiological factors which may influence adiposity and health-related outcomes that are both behaviorally and physiologically driven. Our study has addressed this possible confounding by including estimates of genetic admixture which account for the biological factors underlying such classification and bring validity to our findings by reducing potential spurious associations driven by ancestral genes influencing body composition, independent of parental practices.
When investigating the role of SES to pediatric adiposity, we found an inverse association between SES and both parental Pressure to eat and Restriction. Nationally representative data has demonstrated that children from low income homes are at higher risk for becoming overweight compared to those of middle income families (Ogden et al., 2010) and studies have reported SES to be inversely related to BMI-for-age percentile (Mikolajczyk & Richter, 2008; Goodman, 1999). Our findings are consistent with Ogden et al. and indicate that parental feeding practices are inversely related to adiposity in low income populations. Further research is needed to investigate if parental feeding practices contribute to the increased prevalence of pediatric obesity in low income populations.
The findings of this research are pertinent in several regards. First, we studied a multi- ethnic and economically diverse group of children. Second, robust measures of body composition were used to assess adiposity. We controlled for the role of genetic admixture on adiposity, which is important given that genetic admixture has been shown to contribute to body composition differences in children (Cardel et al., 2011; Casazza K et al., 2010). Additionally, the use of structural equations modeling allowed the model to look at many relationships at once, though; this study is limited because of the inability to stratify the model by race/ethnicity due to sample size limitations. Though our study is cross-sectional, and causality cannot be implied, it is important to note the possibility of reverse associations or bi-directionality in parental feeding practices, namely that child adiposity may elicit parental (attempts at) restraint or pressure to eat (Campbell et al., 2010).
In conclusion, the results of this investigation provide support that specific parental feeding practices, such as parental restriction or pressure to eat, are associated with child adiposity. Our findings suggest that Hispanic parents differ from AA and EA parents in their feeding practices and further research is needed to investigate if controlling feeding practices differentially impact adiposity in diverse populations. SES was inversely related to child adiposity and low income families report higher levels of parental feeding practices, a possible contributor to child overweight. Thus, parental feeding practices appear to differ across racial/ethnic groups and socioeconomic levels and may be associated with population differences in child adiposity.
Highlights.
Effects of race/ethnicity and socioeconomic status on parental feeding practices and adiposity
Parental restriction was positively associated with child adiposity
Parental pressure to eat was inversely associated with child adiposity
Hispanics report more controlling parental feeding practices than blacks or whites
Lower SES is associated with increased restriction, pressure to eat, and child adiposity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Anderson CB, Hughes SO, Fisher JO, Nicklas TA. Cross-cultural equivalence of feeding beliefs and practices: The psychometric properties of the child feeding questionnaire among Blacks and Hispanics. Preventive Medicine. 2005;41:521–531. doi: 10.1016/j.ypmed.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Batsell R, Brown A, Ansfield M, Paschall G. “You Will Eat All of That!”: A retrospective analysis of forced consumption episodes. Appetite. 2002;38:211–219. doi: 10.1006/appe.2001.0482. [DOI] [PubMed] [Google Scholar]
- Batsell WR, Brown AS. Human flavor-aversion learning: A comparison of traditional aversions and cognitive aversions. Learn Motiv. 1998;29:383–396. [Google Scholar]
- Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. American Journal of Clinical Nutrition. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- Bjorntorp P. Abdominal obesity and the development of noninsulin-dependent diabetes mellitus. Diabetes Metab Rev. 1988;4:615–622. doi: 10.1002/dmr.5610040607. [DOI] [PubMed] [Google Scholar]
- Campbell K, Andrianopoulos N, Hesketh K, Ball K, Crawford D, Brennan L, et al. Parental use of restrictive feeding practices and child BMI z-score. A 3-year prospective cohort study. Appetite. 2010;55:84–88. doi: 10.1016/j.appet.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Cardel M, Higgins PB, Willig AL, Keita AD, Casazza K, Gower BA, et al. African genetic admixture is associated with body composition and fat distribution in a cross-sectional study of children. Int J Obes. 2011;35:60–65. doi: 10.1038/ijo.2010.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnell S, Wardle J. Associations between multiple measures of parental feeding and children’s adiposity in United Kingdom preschoolers. Obesity. 2007;15:137–144. doi: 10.1038/oby.2007.513. [DOI] [PubMed] [Google Scholar]
- Casazza K, Dulin-Keita A, Gower B, Fernandez JR. Intrabdominal fat is related to metabolic risk factors in Hispanic Americans, African Americans and in girls. Acta Paediatrica. 2009;98:1965–1971. doi: 10.1111/j.1651-2227.2009.01474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casazza K, Thomas O, Dulin-Keita A, Fernandez Adiposity and genetic admixture, but not race/ethnicity, influences bone mineral content in peripubertal children. Journal of Bone Mineral Metabolism. 2010;28:424–432. doi: 10.1007/s00774-009-0143-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demerath EW, Schubert CM, Maynard LM, Sun SS, Chumlea WC, Pickoff A, et al. Do Changes in Body Mass Index Percentile Reflect Changes in Body Composition in Children? Data From the Fels Longitudinal Study. Pediatrics. 2006;117:e487–e495. doi: 10.1542/peds.2005-0572. [DOI] [PubMed] [Google Scholar]
- Suliga Edyta. Visceral adipose tissue in children and adolescents: a review. Nutrition Research Reviews. 2009;22:137–147. doi: 10.1017/S0954422409990096. [DOI] [PubMed] [Google Scholar]
- Elberg J, McDuffie JR, Sebring NG, Salaita C, Keil M, Robotham D, et al. Comparison of methods to assess change in children’s body composition. American Journal of Clinical Nutrition. 2004;80:64–69. doi: 10.1093/ajcn/80.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental Feeding Attitudes and Styles and Child Body Mass Index: Prospective Analysis of a Gene-Environment Interaction. Pediatrics. 2004;114:e429–e436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- Fernandez JR, Shriver MD. Using genetic admixture to study the biology of obesity traits and to map genes in admixed populations. Nutr Rev. 2004;62:S69–S74. doi: 10.1111/j.1753-4887.2004.tb00091.x. [DOI] [PubMed] [Google Scholar]
- Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of Overweight on the Risk of Developing Common Chronic Diseases During a 10-Year Period. Archives of Internal Medicine. 2001;161:1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. American Journal of Clinical Nutrition. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. American Journal of Clinical Nutrition. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. American Journal of Clinical Nutrition. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and Trends in Obesity Among US Adults, 1999–2008. JAMA: The Journal of the American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Fox K, Peters D, Armstrong N, Sharpe P, Bell M. Abdominal fat deposition in 11-year-old children. Int J Obes. 1993;17:11–16. [PubMed] [Google Scholar]
- Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: maternal and child characteristics. Appetite. 2001;37:231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- Galloway AT, Fiorito L, Lee Y, Birch LL. Parental Pressure, Dietary Patterns, and Weight Status among Girls Who Are “Picky Eaters”. J Am Diet Assoc. 2005;105:541–548. doi: 10.1016/j.jada.2005.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway AT, Fiorito L, Lee Y, BIRCH LL. Parental pressure, dietary patterns, and weight status among girls who are “picky eaters”. J Am Diet Assoc. 2005;105:541–548. doi: 10.1016/j.jada.2005.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway AT, Fiorito LM, Francis LA, Birch LL. ‘Finish your soup’: Counterproductive effects of pressuring children to eat on intake and affect. Appetite. 2006;46:318–323. doi: 10.1016/j.appet.2006.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents’ health. American Journal of Public Health. 1999;89:1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulding A, Taylor RW, Gold E, Lewis-Barned NJ. Regional body fat distribution in relation to pubertal stage: a dual- energy X-ray absorptiometry study of New Zealand girls and young women. The American Journal of Clinical Nutrition. 1996;64:546–551. doi: 10.1093/ajcn/64.4.546. [DOI] [PubMed] [Google Scholar]
- Gregory JE, Paxton SJ, Brozovic AM. Maternal feeding practices, child eating behaviour and body mass index in preschool-aged children: A prospective analysis. International Journal of Behavioral Nutrition and Physical Activity. 2010:7. doi: 10.1186/1479-5868-7-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy E, Hughes SO, Goldberg JP, Hyatt RR, Economos CD. Parent behavior and child weight status among a diverse group of underserved rural families. Appetite. 2010;54:369–377. doi: 10.1016/j.appet.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University Press; 1975. [Google Scholar]
- Huon GF. Dieting, binge eating, and some of their correlates among secondary school girls. Int J Eat Disord. 1994;15:159–164. doi: 10.1002/1098-108x(199403)15:2<159::aid-eat2260150207>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Joyce JL, Zimmer-Gembeck MJ. Parent feeding restriction and child weight. The mediating role of child disinhibited eating and the moderating role of the parenting context. Appetite. 2009;52:726–734. doi: 10.1016/j.appet.2009.03.015. [DOI] [PubMed] [Google Scholar]
- Kekes-Szabo T, Hunter GR, Nyikos I, Nicholson C, Snyder S, Berland L. Development and validation of computed tomography derived anthropometric regression equations for estimating abdominal adipose tissue distribution. Obesity Research. 1994;2:450–457. doi: 10.1002/j.1550-8528.1994.tb00092.x. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Gummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord. 2003;27:505–513. doi: 10.1038/sj.ijo.0802251. [DOI] [PubMed] [Google Scholar]
- Malina RM, Bouchard C. Growth, Maturation, and Physical Activity. Champaign: Human Kinetics Books; 1991. [Google Scholar]
- Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45:13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson DM, Robinson TN, Varady A, Killen JD. Do Mexican-American Mothers’ Food-Related Parenting Practices Influence Their Children’s Weight and Dietary Intake? Journal of the American Dietetic Association. 2006;106:1861–1865. doi: 10.1016/j.jada.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Mikolajczyk R, Richter M. Associations of behavioural, psychosocial and socioeconomic factors with over- and underweight among German adolescents. International Journal of Public Health. 2008;53:214–220. doi: 10.1007/s00038-008-7123-0. [DOI] [PubMed] [Google Scholar]
- Moens E, Braet C, Soetens B. Observation of family functioning at mealtime: a comparison between families of children with and without overweight. J Pediatr Psychol. 2007;32:52–63. doi: 10.1093/jpepsy/jsl011. [DOI] [PubMed] [Google Scholar]
- Mulder C, Kain J, Uauy R, Seidell J. Maternal attitudes and child-feeding practices: relationship with the BMI of Chilean children. Nutrition Journal. 2009;8:37. doi: 10.1186/1475-2891-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of High Body Mass Index in US Children and Adolescents, 2007–2008. JAMA: The Journal of the American Medical Association. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Kline Rex B. Principles and Practice of Structural Equation Modeling. New York, NY: The Guilford Press; 2005. [Google Scholar]
- Rexrode K, Carey V, Hennekens C, Walters E, Colditz G, Stampfer M, et al. Abdominal adiposity and coronary heart disease in women. JAMA: The Journal of the American Medical Association. 1998;280:1843–1848. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- Rifas-Shiman SL, Sherry B, Scanlon K, Birch LL, Gillman MW, Taveras EM. Does maternal feeding restriction lead to childhood obesity in a prospective cohort study? Archives of Disease in Childhood. 2011;96:265–269. doi: 10.1136/adc.2009.175240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage JS, Fisher JO, Birch LL. Parental Influence on Eating Behavior: Conception to Adolescence. The Journal of Law, Medicine & Ethics. 2007;35:22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz A, Northridge ME. Social Determinants of Health: Implications for Environmental Health Promotion. Health Education & Behavior. 2004;31:455–471. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- Shaffer JR, Kammerer CM, Reich D, McDonald G, Patterson N, Goodpaster B, et al. Genetic markers for ancestry are correlated with body composition traits in older African Americans. Osteoporos Int. 2007;18:733–741. doi: 10.1007/s00198-006-0316-6. [DOI] [PubMed] [Google Scholar]
- Sherry B, McDivitt J, Birch LL, Cook FH, Sanders S, Prish JL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc. 2004;104:215–221. doi: 10.1016/j.jada.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Shrewsbury V, Wardle J. Socioeconomic Status and Adiposity in Childhood: A Systematic Review of Cross-sectional Studies 1990–2005. Obesity. 2008;16:275–284. doi: 10.1038/oby.2007.35. [DOI] [PubMed] [Google Scholar]
- Spruijt-Metz D, Li C, Cohen E, Birch L, Goran M. Longitudinal influence of mother’s child-feeding practices on adiposity in children. The Journal of Pediatrics. 2006;148:314–320. doi: 10.1016/j.jpeds.2005.10.035. [DOI] [PubMed] [Google Scholar]
- Spruijt-Metz D, Lindquist CH, Birch LL, Fisher JO, Goran MI. Relation between mothers’ child-feeding practices and children’s adiposity. American Journal of Clinical Nutrition. 2002;75:581–586. doi: 10.1093/ajcn/75.3.581. [DOI] [PubMed] [Google Scholar]
- Webber L, Cooke L, Hill C, Wardle J. Child adiposity and maternal feeding practices: a longitudinal analysis. The American Journal of Clinical Nutrition. 2010;92:1423–1428. doi: 10.3945/ajcn.2010.30112. [DOI] [PubMed] [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting Obesity in Young Adulthood from Childhood and Parental Obesity. The New England Journal of Medicine. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]