Lipomas of the digestive tract are rare and most often found incidentally during a colonoscopy, computed tomography (CT) scan, surgery, or autopsy.1–3 Lipomas of the colon were first reported by Bauer in 1757 and are most often located in the ascending colon near the cecum.4 These fatty tumors are rarely greater than 2 cm in size and are rarely symptomatic. The most common presentations of symptomatic patients with lipomas greater than 2 cm in size include abdominal pain, hemorrhage, diarrhea, or constipation.4 Lipomas that grow more than 4 cm in size can lead to obstruction and intussusception requiring surgical or endoscopic resection.3–6 These benign tumors are often difficult to diagnose because of their asymptomatic nature or the intermittent nature of patients' symptoms. On plain radiograph, these lesions may produce a radiolucent area above the region of affected bowel. Barium studies are nondiagnostic unless changes in the lipoma's shape and size are seen via a diagnostic test (the squeeze sign).4 More commonly, definitive diagnosis is made after the lipoma is removed and subjected to histopathologic staining.7 Surgical resection is recommended to alleviate symptoms and to rule out malignancy.7 In this case report, we describe an intussuscepted, transverse colonic lipoma that caused intermittent bowel obstruction.
Case Report
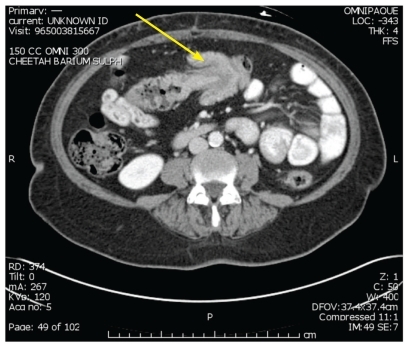
A 58-year-old, otherwise healthy woman presented to an ambulatory clinic complaining of left-sided abdominal pain, intermittent bloating, nausea, and bright red blood per rectum. The patient underwent a colonoscopy, which revealed a large ulcerated mass in the transverse colon that encompassed more than 50% of the bowel lumen. An endoscopic biopsy showed reactive changes without evidence of dysplasia or malignancy. A CT scan revealed a concentric mass in the distal transverse colon with evidence of colonic intussusception (Figure 1). The patient's hemoglobin level measured 11.4 g/dL, and her carcinoembryonic antigen level was normal. Because of the size of the mass and the inability to rule out a malignant intussusception, the patient was taken to the operating room, where a large mass was palpated in the mid-transverse colon. She underwent a successful transverse colectomy primary anastomosis. Gross examination of the specimen revealed a large pedunculated mass, and histologic examination showed mature adipocytes in the submucosa, with mucosal ulceration consistent with a benign lipoma (Figure 2). The patient had an uneventful postoperative course and was discharged home on the fifth postoperative day.
Figure 1.
A computed tomography scan of the abdomen showing colonic intussusception (yellow arrow).
Figure 2.
Gross surgical pathology at the time of resection revealed a large pedunculated mass.
Discussion
Lipomas represent the most common nonepithelial-derived tumor of the gastrointestinal tract.7 These tumors are more prevalent in women than in men and have a peak incidence in patients between 50 and 60 years of age.5,8 Several studies have shown that the most common site of colonic lipomas is the ascending colon (45%), although tumors may occur in the sigmoid colon (30.3%), descending colon (15.2%), and transverse colon (9.1%).2,4,9–12 Thus, the least common location of a colonic lipoma is the transverse colon, which was the site of the tumor in this case report.3,12,13 Our finding is only the seventh report of a transverse colonic lipoma published in the literature (Table 1).
Table 1.
Cases of Transverse Colonic Lipomas Published in the Literature
| Reference | Year | Age (years) | Gender | Symptoms | Size (cm) | Treatment |
|---|---|---|---|---|---|---|
| Liessi G, et al2 | 1996 | 50 | Male | Abdominal pain, nausea, and cramping | 5 | Right hemicolectomy |
| Stone C, Weber HC9 | 2001 | 60 | Male | Constipation | 5 | Endoscopic removal |
| Rogers SO Jr, et al10 | 2002 | 45 | Female | Abdominal pain and diarrhea | 5 | Surgical resection |
| Atila K, et al11 | 2007 | 56 | Female | Acute abdominal pain, nausea, and vomiting | 5 | Right hemicolectomy |
| Mnif L, et al12 | 2009 | 67 | Female | Abdominal pain | 5 | Surgical resection |
| Mason R, et al4 | 2010 | 51 | Female | Intermittent colicky abdominal pain | 4.5 | Right hemicolectomy |
The diagnosis of a colonic lipoma can be established radiographically, endoscopically, or surgically. The pathognomonic sign of a colonic lipoma is the squeeze sign, in which a radiolucent, spherical filling defect with well-defined margins can be shown to change size and shape in response to peristalsis during administration of a barium enema.12 Ninety percent of colonic lipomas are localized to the submucosa; colonic lipomas are rarely found in other layers of the bowel wall.12,13 Due to this location, 3 endoscopic signs can aid in the diagnosis of a lipoma: the “cushion” sign, which occurs when forceps press into the mass, resulting in a depression or pillowing; the “tenting” sign, which occurs when mucosa is grabbed over the lesion and pulled away, resulting in a tent-like appearance; and the “naked fat” sign, which occurs when fat is grossly extruded after biopsy.14 Furthermore, the submucosal location of these tumors has led to several techniques for endoscopic removal, including endoloop excision, nylon loop-assisted removal, endoclipping, and sectioning of the overlying mucosa via segmental cuts.9,15–17 One of the most common and feared complications of endoscopic removal is colonic perforation, although its true incidence is likely underestimated due to the rarity of lipomas.
The clinical diagnosis of a lipoma can be very difficult. In fact, several cases of lipomas with overlying villous adenomas or other presentations mimicking carcinomas have been reported in the literature.18–20 In most cases, segmental surgical resection is the most appropriate treatment, as it ensures proper collection of lymph nodes for appropriate staging of presumed colonic carcinoma. According to Jiang and colleagues, surgical intervention is warranted when the lipoma is more than 4 cm in size; there is an unclear preoperative diagnosis; the lipoma has associated morbidity (intussusception) and the patient is symptomatic; there is involvement of the muscular or serosal layer; or the lesion cannot be radically resected endoscopically.3
Recently, Tamura and colleagues reported a case of a giant colonic lipoma, and they proposed that accessible pedunculation and normal complete blood counts, blood chemistry, and carcinoembryonic antigen levels warrant endoscopic rather than surgical resection.21 Tamura and coworkers used indigo carmine to demonstrate normal colonic pitting and to detect the submucosal location of the tumor.21 They also used endoscopic ultrasonography to demonstrate the presence of a hyperechoic mass, which was consistent with a lipoma. Examination of the tumor's base is the key for providing sufficient indication for endoscopic resection. Histologically, hematoxylin and eosin staining will generally show adipose tissue located in the submucosa with numerous fibra intervals.12
Based on the diagnostic criteria proposed by Jiang and associates and oncologic principles, we chose to perform surgical resection of the transverse colon.3 This decision allowed for complete staging if the tumor was found to be malignant.
In summary, large symptomatic colonic lipomas should be excised either surgically or endoscopically. Small lipomas (<4 cm) with pedunculated bases in patients with normal blood counts and tumor markers may be amenable to endoscopic resection. Lesions that are greater than 4 cm in size and/or lesions found in patients in whom malignancy cannot be reasonably ruled out should undergo segmental resection.
References
- 1.Pfeil SA, Weaver MG, Abdul-Karim FW, Yang P. Colonic lipomas: outcome of endoscopic removal. Gastrointest Endosc. 1990;36:435–438. doi: 10.1016/s0016-5107(90)71110-8. [DOI] [PubMed] [Google Scholar]
- 2.Liessi G, Pavanello M, Cesari S, Dell'Antonio C, Avventi P. Large lipomas of the colon: CT and MR findings in three symptomatic cases. Abdom Imaging. 1996;21:150–152. doi: 10.1007/s002619900032. [DOI] [PubMed] [Google Scholar]
- 3.Jiang L, Jiang LS, Li FY, et al. Giant submucosal lipoma located in the descending colon: a case report and review of the literature. World J Gastroenterol. 2007;13:5664–5667. doi: 10.3748/wjg.v13.i42.5664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mason R, Bristol JB, Petersen V, Lyburn ID. Education and imaging. Gastrointestinal: lipoma induced intussusception of the transverse colon. J Gastroenterol Hepatol. 2010;25:1177. doi: 10.1111/j.1440-1746.2010.06360.x. [DOI] [PubMed] [Google Scholar]
- 5.Ryan J, Martin JE, Pollock DJ. Fatty tumours of the large intestine: a clinico-pathological review of 13 cases. Br J Surg. 1989;76:793–796. doi: 10.1002/bjs.1800760809. [DOI] [PubMed] [Google Scholar]
- 6.Sarker SK. Lipoma of the descending colon causing acute large-bowel intussusception. Internet J Surgery. 2010;22 http//www.ispub.com/journal/the_internet_ journal_of_surgery/volume_22_number_1_1/article/lipoma-of-the-descending-colon-causing-acute-large-bowel-intussusception.html Modified January 9, 2010. [Google Scholar]
- 7.Bardají M, Roset F, Camps R, Sant F, Fernández-Layos MJ. Symptomatic colonic lipoma: differential diagnosis of large bowel tumors. Int J Colorectal Dis. 1998;13:1–2. doi: 10.1007/s003840050122. [DOI] [PubMed] [Google Scholar]
- 8.Michowitz M, Lazebnik N, Noy S, Lazebnik R. Lipoma of the colon. A report of 22 cases. Am Surg. 1985;51:449–454. [PubMed] [Google Scholar]
- 9.Stone C, Weber HC. Endoscopic removal of colonic lipomas. Am J Gastroenterol. 2001;96:1295–1297. doi: 10.1111/j.1572-0241.2001.03718.x. [DOI] [PubMed] [Google Scholar]
- 10.Rogers SO, Jr, Lee MC, Ashley SW. Giant colonic lipoma as lead point for intermittent colo-colonic intussusception. Surgery. 2002;131:687–688. doi: 10.1067/msy.2002.116409. [DOI] [PubMed] [Google Scholar]
- 11.Atila K, Terzi C, Obuz F, Yilmaz T, Füzün M. Symptomatic intestinal lipomas requiring surgical interventions secondary to ileal intussusception and colonic obstruction: report of two cases. Ulus Travma Acil Cerrabi Derg. 2007;13:227–231. [PubMed] [Google Scholar]
- 12.Mnif L, Amouri A, Masmoudi MA, et al. Giant lipoma of the transverse colon: a case report and review of the literature. Tunis Med. 2009;87:398–402. [PubMed] [Google Scholar]
- 13.Ghidirim G, Mishin I, Gutsu E, Gagauz I, Danch A, Russu S. Giant submucosal lipoma of the cecum: report of a case and review of literature. Room J Gastroenterol. 2005;14:393–396. [PubMed] [Google Scholar]
- 14.De Beer RA, Shinya H. Colonic lipomas. An endoscopic analysis. Gastrointest Endosc. 1975;22:90–91. doi: 10.1016/s0016-5107(75)73710-0. [DOI] [PubMed] [Google Scholar]
- 15.Raju GS, Gomez G. Endoloop ligation of a large colonic lipoma: a novel technique. Gastrointest Endosc. 2005;62:988–990. doi: 10.1016/j.gie.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Murray MA, Kwan V, Williams SJ, Bourke MJ. Detachable nylon loop assisted removal of large clinically significant colonic lipomas. Gastrointest Endosc. 2005;61:756–759. doi: 10.1016/s0016-5107(04)02650-1. [DOI] [PubMed] [Google Scholar]
- 17.Katsinelos P, Chatzimavroudis G, Zavos C, Paroutoglou G, Papaziogas B, Kountouras J. A novel technique for the treatment of a symptomatic giant colonic lipoma. J Laparoendosc Adv Surg Tech A. 2007;17:467–469. doi: 10.1089/lap.2006.0208. [DOI] [PubMed] [Google Scholar]
- 18.Huh KC, Lee TH, Kim SM, et al. Intussuscepted sigmoid colonic lipoma mimicking carcinoma. Dig Dis Sci. 2006;51:791–795. doi: 10.1007/s10620-006-3208-x. [DOI] [PubMed] [Google Scholar]
- 19.Capra F, Zorcolo L, Scintu F, Mascia R, Casula G. Giant sigmoid lipoma covered by a villous adenoma. Int J Colorectal Dis. 2007;22:563–564. doi: 10.1007/s00384-005-0754-1. [DOI] [PubMed] [Google Scholar]
- 20.Martin P, Sklow B, Adler DG. Large colonic lipoma mimicking colon cancer and causing colonic intussusception. Dig Dis Sci. 2008;53:2826–2827. doi: 10.1007/s10620-008-0202-5. [DOI] [PubMed] [Google Scholar]
- 21.Tamura S, Yokoyama Y, Morita T, Tadokoro T, Higashidani Y, Onishi S. “Giant” colon lipoma: what kind of findings are necessary for the indication of endoscopic resection? Am J Gastroenterol. 2001;96:1944–1946. doi: 10.1111/j.1572-0241.2001.03909.x. [DOI] [PubMed] [Google Scholar]