Metastatic lesions in the pancreas are uncommon, accounting for only 5% of all pancreatic malignancies. Renal cell carcinomas (RCCs) account for 2% of all cancers and have a predilection to metastasize to rare locations, including the pancreas. RCC is the most common primary tumor leading to solitary pancreatic metastasis. Although the majority of metastases occur within 3 years of radical nephrectomy, the appearance of metastatic disease many years after nephrectomy is a well-known feature of RCC. Since most pancreatic metastases are asymptomatic, routine long-term radiologic surveillance is necessary. We present a case of metastatic RCC to the pancreas that occurred 13 years postnephrectomy.
Case Report
A 67-year-old asymptomatic woman was referred to our institution for evaluation of a new mass in the tail of the pancreas that had been identified via computed tomography (CT). Her past medical history was significant for diabetes mellitus, hypertension, peripheral vascular disease, carotid artery stenosis, coronary artery disease status post—bypass surgery, and a 5.5-cm RCC of the left kidney, for which she had undergone a left nephrectomy in 1997 (approximately 13 years earlier). Routine, noncontrast CT surveillance found interval growth of a previously noted right renal mass lesion and development of a new mass in the pancreatic tail. A repeat CT scan performed with intravenous contrast showed 2 cystic lesions in the right kidney and a 5.8-cm × 4.9-cm × 3.6-cm mass in the tail of the pancreas. The pancreatic mass appeared isodense to the pancreas prior to contrast administration, was markedly hypervascular on arterial phase imaging, and was noted to extend into the adjacent splenic vein with an enhancing thrombus.
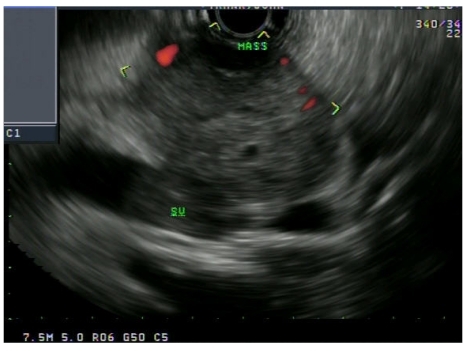
Endoscopic ultrasound was performed at our institution and revealed a well-defined, hypoechoic, homogeneous, vascular, lobulated mass measuring 4.2 cm × 3.8 cm in the tail of the pancreas. The mass appeared to invade the splenic vein (Figure 1). Fine-needle aspiration of the mass showed clusters of suspicious cells with mucin.
Figure 1.
An endoscopic ultrasound image showing a hypervascular mass in the tail of the pancreas invading the splenic vein (SV).
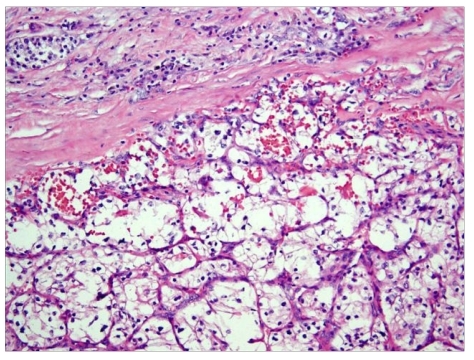
The patient subsequently underwent a distal pancreatectomy with splenectomy. The final surgical pathology showed metastatic clear-cell RCC among pancreatic islet cells infiltrating focally into peripancreatic adipose tissue and into the splenic vein with intravascular tumor nodule formation (Figure 2). Three peripancreatic lymph nodes, the splenic artery, and pancreatic resection margins were free of the tumor.
Figure 2.
A low-power image showing a metastatic clear-cell renal cell carcinoma among pancreatic islet cells (hematoxylin and eosin stain).
Discussion
RCC accounts for approximately 2% of all cancers in the United States, with an annual incidence rate of over 30,000 new cases per year; this rate has been steadily rising over the past 2 decades.1,2 It is estimated that approximately one third of patients with RCC have metastases at presentation and that another 20—30% of patients with localized RCC will relapse after radical nephrectomy.3 Approximately 85% of recurrences occur within 3 years of resection.1,4 The most common sites of metastasis from RCC include the lung (50—60%), bone (30—40%), liver (30—40%), and brain (5%).1 RCC also has a tendency to metastasize to rare sites, such as the pancreas, thyroid, skeletal muscle, skin, or soft tissue.1,5
Metastasis to the pancreas is uncommon and accounts for 5% of all pancreatic malignancies.5 Pancreatic metastases usually arise from breast cancer, colon cancer, non-small cell lung cancer, melanoma, or RCC.6 In several case series, RCC has been cited as the most common primary tumor leading to solitary pancreatic metastasis, representing 0.25—3% of all resected pancreatic specimens.1,4,7 Additionally, pancreatic metastases of RCC are often the sole site of distant spread.2 The lesions can be multifocal in approximately 30% of patients and are resectable in approximately 80% of cases.7
RCC can recur any number of years after nephrec-tomy. The appearance of metastatic disease many years after nephrectomy is a well-known feature of RCC and is associated with a more favorable outcome than early recurrences, which tend to have more rapid progression of disease.4,5 One study found that 11% of patients who survived 10 years or more after nephrectomy developed metastases, with an interval of up to 32 years in some reports.7,8,9
The mode of RCC spread to the pancreas remains controversial, although RCC has a predilection for both venous and lymphatic spread. Direct spread to the pancreas is not thought to occur.1,2 Hematogenous spread may occur along the draining collateral veins via preexisting portacaval shunts.1,10 Lymphogenous spread may occur via retrograde lymph flow through lymphatic routes from the head of the pancreas to the dorsal side of the renal artery.10
Patients may present with a variety of gastrointestinal symptoms, including abdominal pain, biliary obstruction, an abdominal mass, pancreatic exocrine/endocrine dysfunction, weight loss, and/or gastrointestinal bleeding secondary to hemosuccus pancreaticus.1 Since pancreatic metastasis from RCC may be asymptomatic in up to 50% of cases, long-term follow-up surveillance with routine imaging is indicated.10
The radiologic features of metastatic RCC lesions closely resemble the appearance of primary RCC. CT imaging shows hyperenhancing lesions that are most pronounced in the early arterial phases of enhancement, which reflects the hypervascular nature of these tumors.1,4,10 This feature aids in detecting RCC as well as distinguishing it from primary adenocarcinoma of the pancreas, which is typically hypovascular and appears nonenhancing on CT imaging.1,4,10 Although radiologic features and clinical history can be strongly suggestive of RCC, histologic verification is mandatory. However, the risk of bleeding with fine-needle aspiration is increased due to the vascular nature of the tumor.10
Surgical treatment of isolated pancreatic metastases from neoplasms other than RCC carries a poor prognosis, as these metastases typically indicate disseminated meta-static disease.11 Approximately 2—6% of patients with metastatic RCC present with isolated metastatic lesions amenable to surgical resection.3 Surgical resection of metastatic disease limited to the pancreas has a 5-year survival rate of 29—35%.1,4,10 Patients with isolated pancreatic metastases from RCC represent a unique group of patients with a more indolent course of RCC. A prolonged interval from nephrectomy to the appearance of metastasis is associated with a more favorable prognosis.10 Radical lymph node dissection is not necessary, as peripancreatic lymph node involvement is uncommon, which may be one of the factors that explains the favorable outcomes achieved with surgery. 1,2,10,11
References
- 1.Kassabian A, Stein J, Jabbour N, et al. Renal cell carcinoma metastatic to the pancreas: a single-institution series and review of the literature. Urology. 2000;56:211–215. doi: 10.1016/s0090-4295(00)00639-7. [DOI] [PubMed] [Google Scholar]
- 2.Karimi KM, McFadden DW. Pancreatic resection for metastatic renal cell carcinoma to the pancreas. Am Surg. 2007;73:1158–1160. [PubMed] [Google Scholar]
- 3.Sohn TA, Yeo CJ, Cameron JL, Nakeeb A, Lillemoe KD. Renal cell carcinoma metastatic to the pancreas: results of surgical management. J Gastrointest Surg. 2001;5:346–351. doi: 10.1016/s1091-255x(01)80060-3. [DOI] [PubMed] [Google Scholar]
- 4.Ghavamian R, Klein KA, Stephens DH, et al. Renal cell carcinoma metastatic to the pancreas: clinical and radiological features. Mayo Clin Proc. 2000;75:581–585. doi: 10.4065/75.6.581. [DOI] [PubMed] [Google Scholar]
- 5.Tanis PJ, van der Gaag NA, Busch OR, van Gulik TM, Gouma DJ. Systematic review of pancreatic surgery for metastatic renal cell carcinoma. Br J Surg. 2009;96:579–592. doi: 10.1002/bjs.6606. [DOI] [PubMed] [Google Scholar]
- 6.Thompson LD, Heffess CS. Renal cell carcinoma to the pancreas in surgical pathology material. Cancer. 2000;89:1076–1088. doi: 10.1002/1097-0142(20000901)89:5<1076::aid-cncr17>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 7.Wente MN, Kleeff J, Esposito I, et al. Renal cell metastasis into the pancreas: a single-center experience and overview of the literature. Pancreas. 2005;30:218–222. doi: 10.1097/01.mpa.0000153337.58105.47. [DOI] [PubMed] [Google Scholar]
- 8.Bassi C, Butturini G, Falconi M, Sargenti M, Mantovani W, Pederzoli P. High recurrence rate after atypical resection for pancreatic metastases from renal cell carcinoma. Br J Surg. 2003;90:555–559. doi: 10.1002/bjs.4072. [DOI] [PubMed] [Google Scholar]
- 9.McNichols DW, Segura JW, De Weerd JH. Renal cell carcinoma: long-term survival and late recurrence. J Urol. 1981;126:17–23. doi: 10.1016/s0022-5347(17)54359-1. [DOI] [PubMed] [Google Scholar]
- 10.Faure JP, Tuech JJ, Richer JP, Pessaux P, Arnaud JP, Carretier M. Pancreatic metastasis of renal cell carcinoma: presentation, treatment and survival. J Urol. 2001;165:20–22. doi: 10.1097/00005392-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Sellner F, Tykalsky N, De Santis M, Pont J, Klimpfinger M. Solitary and multiple isolated metastases of clear cell renal carcinoma to the pancreas: an indication for pancreatic surgery. Ann Surg Oncol. 2006;13:75–85. doi: 10.1245/ASO.2006.03.064. [DOI] [PubMed] [Google Scholar]