Abstract
Numerous national surveys and surveillance programs have shown a substantial rise in the abuse of prescription opioids over the past 15 years. Accessibility of these drugs to non-patients is the result of their unlawful channeling from legal sources to the illicit marketplace (diversion). Empirical data on diversion remain absent from the literature. This paper examines abusers’ sources of diverted drugs from two large studies: 1) a national sample of opioid treatment clients (N=1983), and 2) a South Florida study targeting diverse populations of opioid abusers (N=782). The most common sources of diverted medications were dealers, sharing/trading, legitimate medical practice (e.g., unknowing medical providers), illegitimate medical practice (e.g., pill mills), and theft, in that order. Sources varied by users’ age, gender, ethnicity, risk-aversiveness, primary opioid of abuse, injection drug use, physical health, drug dependence, and either access to health insurance or relative financial wealth. Implications for prescription drug control policy are discussed.
Introduction
Numerous national surveys, prescription drug abuse surveillance programs and other federally supported monitoring systems have shown a substantial rise in the abuse/misuse of prescription opioids over the past 15 years (Bergman & Dahl-Puustinen, 1989; Blumenschein, 1997; Borsack, 1986–1987; Cooper, Czechowicz, Petersen, & Molinari, 1992; Inciardi, Surratt, Stivers, & Cicero, 2009; Manchikanti, Fellows, Ailinani, & Pampati, 2010; McCabe, Teter, & Boyd, 2004; Monheit, 2010; Ruetsch, 2010; Simoni-Wastila & Tompkins, 2001; Strassels, 2009; Wilford, Finch, Czechowicz, & Warren, 1994; Zacny et al., 2003). The accessibility of these drugs to non-patients is the result of their unlawful channeling from legal sources to the illicit marketplace, which is commonly referred to as “drug diversion”. The Drug Enforcement Administration (DEA) has estimated that prescription drug diversion is a $25 billion-a-year industry (The U.S. General Accountability Office [GAO], 2003).
It is generally believed that the major mechanisms of diversion include: the illegal sale and recycling of prescriptions by physicians and pharmacists; “doctor shopping” by individuals who visit numerous physicians to obtain multiple prescriptions; theft, forgery, or alteration of prescriptions by patients; robberies and thefts from manufacturers, distributors, and pharmacies; and thefts of institutional drug supplies (Weathermon, 1999). Furthermore, there is growing evidence that the diversion of significant amounts of prescription analgesics and benzodiazepines occurs through residential burglaries (aNational Association of Drug Diversion Investigators [NADDI], 2005a b c d) as well as cross-border smuggling at both retail and wholesale levels (Inciardi, 2005; Inciardi & Surratt, 2005). In addition, recent research by the current investigators, and others in the prescription drug abuse field, has documented diversion through such other channels as: pain clinics (Rigg, March, & Inciardi, 2010); “shorting” (under counting) and pilferage by pharmacists and pharmacy employees; medicine cabinet thefts by cleaning and repair personnel in residential settings; theft of guests’ medications by hotel housekeeping staff; and Medicare and Medicaid fraud by patients, pharmacies, and street dealers (Inciardi & Surratt, 2005; Leiderman, 2006). Finally, a number of observers consider the Internet to be a significant source for illegal purchases of prescription drugs (The National Center on Addiction and Substance Abuse [CASA], 2004), although this is highly controversial (Inciardi et al., 2010).
Empirical data on the scope and magnitude of diversion are largely unavailable and remain absent from the literature. In fact, at two recent meetings sponsored by the College on Problems of Drug Dependence focusing on the “Impact of Drug Formulation on Abuse Liability, Safety, and Regulatory Decisions” and “Risk Management and Post-Marketing Surveillance of CNS Drugs,” the proceedings of which have been published (Dart, 2009; Dasgupta & Schnoll, 2009; Johanson et al., 2009; Liederman, 2009; McCormick, 2006; Sapienza, 2006), representatives from government regulatory agencies, the pharmaceutical industry, and the research community agreed that: a) there are no data on the magnitude of particular types of diversion; b) there are no systematic data on how the massive quantities of abused prescription drugs are reaching the streets; and, c) there are no empirical data that might be used for making regulatory decisions and for developing prescription drug prevention and risk management plans. In addition, although a number of studies have addressed the patterns of prescription drug abuse and diversion among health care professionals (Hollinger & Dabney, 2002; Inciardi et al., 2009; Trinkoff, Storr, & Wall, 1999; Trinkoff, Zhou, Storr, & Soeken, 2000; Weir, 2000), very little is known about the magnitude and mechanisms of diversion among other types of prescription drug misusers (e.g., street addicts, methadone clients and so forth) or whether the type of drug being misused influences the means of diversion (e.g., OxyContin® vs. methadone).
Within this context, this paper examines the nature, scope, and magnitude of prescription drug diversion in two different but complementary study samples: First, self-administered, brief paper surveys of a very large sample (N=1,983) of opioid dependent patients entering primarily (>70%) private treatment programs around the country; and, second, a more traditional, focused, interview-based study of diverse samples of prescription opioid abusers in South Florida (N=782) using standardized instruments.
Methods
Survey of Key Informants’ Patients (SKIP)
The nation-wide survey, termed the Survey of Key Informants’ Patients (SKIP), is a key element of the post-marketing surveillance system known as Researched Abuse, Diversion and Addiction-Related Surveillance (RADARS®). The detailed methodology can be found elsewhere (see, Cicero, Surratt, & Inciardi, 2007; Cicero, Ellis, Paradis, & Ortbal, 2010), but briefly, the SKIP program consists of nearly 100 treatment centers, balanced geographically with a good representation of large urban, suburban and rural treatment centers. Each of the treatment centers were asked to recruit as many patients/clients as possible who had a diagnosis of prescription opioid analgesic abuse or dependence using the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV). Inclusion criteria were very broad: first, subjects had to be 18 years of age or older; and second, as mentioned above, they needed to meet DSM-IV criteria for substance abuse, with their primary drug a prescription opioid (i.e., not heroin). Overall, 85% of the patients approached by the treatment counselors completed surveys and submitted them.
The patients were asked to complete a detailed survey instrument, covering demographics, licit and illicit patterns of drug use, diagnostic criteria for alcohol and opioid abuse or dependence (DSM-IV criteria; [e.g., loss of control of drinking or drugging, disruption of everyday activities as a consequence of use, family and friend complaints about abuse, withdrawal, craving, and so forth]), chronic non-withdrawal bodily pain and its intensity (scale of 1–10 with 1 being none and 10 the worst possible pain), and, whether they were currently being treated for a psychiatric condition. Participants received a $25 gift card to Wal-Mart or other designated store for their participation.
Completed survey instruments were identified solely by a unique case number and were mailed by the participant directly to Washington University School of Medicine in St. Louis. The treatment specialists did not see the detailed responses of their patients/clients.
The protocol was approved by the Washington University Institutional Review Board (IRB).
South Florida Study
Participants
To be eligible for the study, individuals needed to be 18 years of age or older and report the misuse of at least one prescription drug five or more times in the previous 90 days. From this population, only those who chose a prescription opioid as their most frequently misused drug were included for the analyses (n=782).
Measures
The Global Appraisal of Individual Needs (GAIN); (Dennis, Titus, White, Unsicker, & Hodgkins, 2002) was the primary instrumentation for the study. The GAIN (Dennis et al., 2002) has eight core sections (background, substance use, physical health, risk behaviors, mental health, environment, legal and vocational), with each containing questions on the recency of problems, breadth of symptoms, and recent prevalence in days or times, as well as lifetime service utilization. The items are combined into over 100 scales and subscales that can be used for DSMIV based diagnoses. Psychometric studies have found Cronbach’s alphas between .9 and .8; all have alphas over .7. Similarly, behavior questions have demonstrated test-retest correlations of .7 to .8. For this study, questions were added to the GAIN: 1) to increase the number of prescription drug categories so as to separately distinguish the major prescription drugs of abuse; and, 2) to assess mechanisms of access to the diverted drugs. To assist study respondents in making accurate reports of their prescription drug abuse histories, the investigators developed a comprehensive pictorial guide depicting brand name and generic drugs on the market by dosage size.
Participants were assessed on several demographic characteristics including age, gender, and race/ethnicity (African-American, Hispanic/Latino, White, Other). They were asked whether, in the past 90 days, they had any form of health insurance, whether they experienced severe pain, and whether physical health problems limited their ability to undertake vigorous activities; response choices were dichotomous (yes/no).
The assessment instrument captured a complete illicit and prescription (non-prescribed) drug use history in number of days each substance was used in the past 90 days, and also whether the participant injected endorsed drugs in the past 90 days. Prescription drugs included fentanyl, hydrocodone, hydromorphone, immediate (IR) and extended (ER) release oxycodone, morphine, and methadone, as well as alprazolam, diazepam and clonazepam.
Participants were also asked what method they used to obtain each diverted prescription drug they misused in the past 90 days. Diversion methods included script doctor (“pill” mill), doctor shopping, regular doctor, pharmacist, theft, dealer, sharing or trading, family, transport from another country, or internet purchase; response choices were dichotomous (yes/no).
Procedures
Recruitment
A variety of purposive sampling strategies were used to locate study participants. Print media advertisements and the posting or manual distribution of cards and flyers were largely used, but other techniques such as chain-referrals with incentives, presentations at community organizations, and referrals from methadone clinic and drug treatment center staffs were also used. The study was conducted in the investigators’ research field offices or in treatment centers located in Broward, Lee, Miami-Dade, and Palm Beach Counties.
Screening
All participants were screened for eligibility before they were asked to participate in a single standardized face-to-face interview. Participants called the study phone number and were screened over the phone by research staff. If eligible, interested street drug users were then scheduled for an interview at a research field office. Eligible methadone clients were scheduled to be interviewed for an interview at the methadone clinic that they regularly attended. Eligible public and private-pay treatment clients were screened by treatment center staff and scheduled to be interviewed at the treatment facility.
Interviewing
Before administering the computer-assisted face-to-face interviews, each participant was re-screened to ensure eligibility, followed by informed consent. Interviews were conducted in private offices and lasted 1 ½ to 2 hours. Participants received a $30 monetary incentive for their participation. All study protocols and instruments were reviewed and approved by the University of Delaware’s Institutional Review Board.
Data Analyses
Data from the SKIP self-administered surveys and the interview questionnaires from the South Florida study were analyzed using Predictive Analytics Software (PASW, formerly SPSS) version 18. Descriptive statistics were calculated to describe both samples in terms of demographics, physical health, substance use and dependence, and primary prescription opioid of abuse. Primary prescription opioid was determined by the specific opioid class (hydrocodone, IR oxycodone, ER oxycodone, methadone, morphine, hydromorphone or fentanyl) that each participant used most often in the past 90 days (South Florida) or self-reported to be their primary drug (SKIP). Because the highest potency prescription opioids (hydromorphone, morphine, and fentanyl) were reported by few participants to be their primary prescription opioid of abuse, these three medications were combined into a single “high potency opioid” category. Buprenorphine and Tramadol were also reported by very few participants (<2% of the total population in both studies), and accordingly, they have been excluded from the analysis.
The diversion sources through which each participant obtained their primary prescription opioid in the most recent 30 or 90 day period were then determined from the data base. Except for one question in the SKIP survey which asked for the one primary means of diversion, in all other cases participants were asked to report all sources for diverted medication. Thus, the participants’ primary prescription opioid may have been obtained through more than one source. In the analyses presented here, certain diversion sources were combined or eliminated. For the SKIP and South Florida study, Internet purchases and transportation from another country were very rare sources of diverted drugs (< 1% in both studies) and were dropped from the analyses. Sharing/trading and friends/family members were combined into one diversion category because of their similarity and frequent overlap. Theft, forged prescriptions and other illegal activities were also combined into a single category since their frequency was quite low. The SKIP survey only asked whether a doctor’s prescription was the source of drugs. Thus, types of physician sources were collectively grouped into a category “medical practice,” along with use of an emergency room physician. For the South Florida study, diversion sources related to the health care system were more specifically delineated. Cases where the prescribing physician was most likely unaware that their patients were misusing the drug in question (regular doctor and doctor shopping) were combined into a new category called “legitimate medical sources.” Sources related to the health care system where the medical professionals involved were almost certainly aware that their patients were misusing the opioid medication (pharmacies and script doctors (“pill mills”) were combined into a new category called illegitimate medical sources.
Bivariate logistic regression models were developed to predict use of each diversion source by demographics, by physical health status, by primary opioid, by injection drug use status, by relative wealth (SKIP), by access to health insurance (South Florida) and by DSM-IV drug dependence criteria (South Florida).
Results: The SKIP Population
Demographics
The mean age of the sample was 34.1 (SD 10.6; range 18–72). There were almost equal numbers of males and females. The sample was overwhelmingly white (82.5%) with extremely low yearly incomes: 70% earned less than $25,000 annually. Moderate to severe pain was prevalent in 59.2% of the patients, most of whom used a doctor’s prescription as their source of drugs (Table 1).
Table 1.
Characteristics of Prescription Opioio-Dependent Treatment Clients (N=1983)
| N | % | |
|---|---|---|
| Demographics | ||
| Age (mean, SD) | 34.1 (10.6) | |
| Age Groups: | ||
| 18–24 | 386 | 19.5 |
| 25–34 | 790 | 39.8 |
| 35–44 | 437 | 22.0 |
| 45+ | 370 | 18.7 |
| Male, gender | 974 | 49.1 |
| Ethnicity: | ||
| Hispanic | 83 | 4.2 |
| African American/Caribbean | 103 | 5.2 |
| White | 1636 | 82.5 |
| Other/unknown | 161 | 8.1 |
| Yearly Income: | ||
| <10,000 | 930 | 47.7 |
| 10,000–24,999 | 455 | 23.4 |
| 25,000–39,999 | 326 | 16.7 |
| 40,000 or more | 237 | 12.2 |
| Physical Health | ||
| Moderate to Severe Pain—past 7 days | 1154 | 59.2 |
| Substance Use (past 30 days) | ||
| Cocaine (powder) | 585 | 30.2 |
| Crack cocaine | 366 | 18.9 |
| Heroin | 172 | 8.7 |
| Rx benzodiazepines | 1033 | 53.4 |
| Inject primary drug | 459 | 25.3 |
| Primary opioid used: | ||
| Hydrocodone | 516 | 26.0 |
| IR oxycodone | 299 | 15.1 |
| ER oxycodone | 699 | 35.2 |
| Methadone | 207 | 10.4 |
| High potency (hydromorphone/fentanyl/morphine) | 262 | 13.2 |
Illicit and Licit Drug Abuse
In addition to opioids, other licit and illicit drug use in the past 30 days was common. After prescription opioids, the most commonly used licit drugs were benzodiazepines with over 53% of the population using them in the past 30 days.
General Patterns of Diversion
Figure 1 shows the percent of the SKIP sample whose diversion source was dealers, sharing, medical practice and theft. The data are shown in two ways: patients were asked to either report a primary diversion mechanism, or to list all diversion sources they utilized (single or multiple options). Clearly, when limited to their primary means of diversion, dealers were the single most common source of prescription opioids, being twice as common as any other means of diversion. Next in importance were medical practice—i.e. prescriptions by a doctor (25%) —and then sharing/trading (20%). Theft was very rare, chosen by less than 5% of the sample. When patients were allowed to check all sources of diversion they had used, dealers were again the overwhelming choice, but doctor’s prescriptions and sharing were the next closest choices by narrow margins. Again, the frequency of overt criminal activity remained quite low in this sample.
Figure 1.
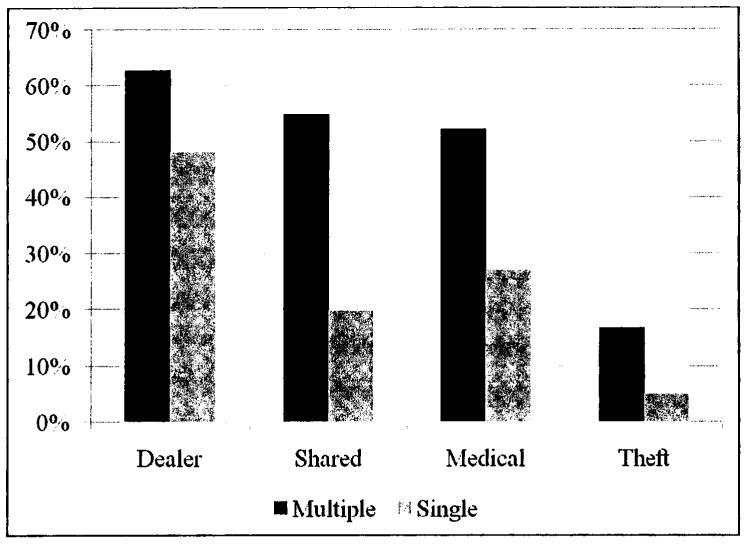
Sources of Primary Diverted Opioid-Opioid Dependent Treatment Clinics
Gender, Age, Ethnicity, and Socioeconomic Status
Table 2 shows the odds ratios, 95% confidence intervals and p values for all predictors of diversion, with statistically significant findings in boldface type. Women were significantly less likely to use dealers to obtain prescription opioids than men, but significantly more likely to use doctor’s prescription, sharing, and, marginally, theft. Age also determined method of diversion. Young abusers 18–24 years of age were far more likely to use dealers (OR=2.003) and theft (OR=1.333) as their sources of drug, whereas those 45 years of age or older were three times less likely to use a dealer (OR=0.333) and 30% less likely to share/trade (OR=0.736), but far more likely to use a medical source (OR=2.298). In terms of ethnicity, whites were significantly less likely to report sharing as a source than were non-whites. We found that the poorest participants (<$ 10,000 annually) were more likely to use dealers, sharing and theft as diversion sources when compared to “wealthier” (>$40,000) participants. For medical practice sources, precisely the opposite pattern was observed, with the “wealthier” much more likely to obtain opioids from a doctor’s prescription than their poorer counterparts.
Table 2.
Bivariate Logistic Regressions Predicting Sources of Diverted Primary Opioid (Opioid Treatment Clients N=1983)
| DIVERSION SOURCE [Odds ratio (95% CI)p value]
| ||||
|---|---|---|---|---|
| Dealer | Sharing/Trading | Medical Practice | Theft | |
| Demographics | ||||
| Age (mean) | 0.948 (0.939, 0.956) .000 | 0.986 (0.978, 0.995) .001 | 1.045 (1.036, 1.054) .000 | 0.980 (0.968, 0.992) .001 |
| Age Groups: | ||||
| 18–24 | 2.003 (1.559, 2.574) .000 | 1.173(0.937, 1.469) .164 | 0.367 (0.290, 0.464) .000 | 1.333 (1.005, 1.767) .046 |
| 25–34 | 1.711 (1.414, 2.071) .000 | 1.132 (0.944, 1.356) .180 | 0.857 (0.716, 1.026) .092 | 1.184 (0.933, 1.503) .164 |
| 35–t4 | 0.733 (0.591, 0.910) .005 | 0.956 (0.773, 1.184) .682 | 1.497 (1.207, 1.858) .000 | 0.760 (0.563, 1.026) .073 |
| 45+ | 0.333 (0.264,0.419) .000 | 0.736 (0.587,0.922) .008 | 2.298 (1.808, 2.921) .000 | 0.734 (0.531, 1.016) .062 |
| Gender | ||||
| Male gender | 1.439 (1.198,1.728) .000 | 0.668 (0.559,0.798) .000 | 0.795 (0.666.0.948) .011 | 0.787 (0.621,0.997) .047 |
| Ethnicity: | ||||
| Hispanic | 0.850 (0.544, 1.330) .477 | 1.258 (0.803, 1.971)316 | 1.407 (0.899, 2.205) .135 | 1.006 (0.559, 1.809) .985 |
| African American | 0.754 (0.505, 1.126) .167 | 1.259 (0.840, 1.887) .265 | 0.823 (0.553, 1.224) .336 | 0.978 (0.574, 1.669) .936 |
| White | 1.121 (0.884, 1.421) .348 | 0.692 (0.546, 0.878) .002 | 1.074 (0.852, 1.354) .545 | 1.242 (0.897, 1.721) .192 |
| Yearly Income: | ||||
| <10,000 | 1.216 (1.011, 1.462) .038 | 1.199 (1.003, 1.435) .047 | 0.715 (0.598, 0.855) .000 | 1.379 (1.087, 1.750) .008 |
| 10,000–24,999 | 0.992 (0.798, 1.232) .942 | 0.971 (0.786, 1.199) .783 | 1.174 (0.951, 1.450) .136 | 0.708 (0.524, 0.956) .024 |
| 25,000–39,999 | 1.021 (0.798, 1.307) .867 | 1.123 (0.883, 1.429) .343 | 0.987 (0.778, 1.253) .917 | 0.947 (0.687, 1.306) .739 |
| 40,000 or more | 0.635 (0.483, 0.835) .001 | 0.593 (0.451, 0.780) .000 | 1.721 (1.299, 0.280) .000 | 0.867 (0.595, 1.263) .457 |
| Physical Health | ||||
| Moderate to Severe Pain—7 days | 0.914 (0.757, 1.102) .344 | 0.878 (0.732, 1.053) .161 | 1.896 (1.579, 2.277) .000 | 0.985 (0.773, 1.254) .899 |
| Substance Use (past 30 days) | ||||
| Injected Primary Drug | 1.736 (1.377, 2.190) .000 | 0.830 (0.671, 1.026) .086 | 0.599 (0.484, 0.742) .000 | 1.515 (1.163, 1.975) .002 |
| Primary opioid used: | ||||
| Hydrocodone | 0.532 (0.434, 0.652) .000 | 1.099 (0.898, 1.345) .361 | 1.775 (1.445, 2.180) .000 | 1.124 (0.864, 1.463) .385 |
| IR oxycodone | 1.007 (0.781, 1.299) .956 | 1.136 (0.886, 1.456) .316 | 1.048 (0.819, 1.340) .712 | 0.966 (0.693, 1.346) .839 |
| ER oxycodone | 2.022 (1.655, 2.470) .000 | 1.079 (0.896, 1.298) .423 | 0.631 (0.524, 0.760) .000 | 1.010 (0.789, 1.292) .938 |
| Methadone | 0.783 (0.584, 1.048) .100 | 0.613 (0.459, 0.819) .001 | 1.419 (1.058, 1.902) .019 | 0.500 (0.310, 0.805) .004 |
| High potency2 | 0.939 (0.719, 1.227) .645 | 0.952 (0.734, 1.236) .714 | 0.693 (0.534, 0.901) .006 | 1.305 (0.941, 1.811) .111 |
The odds ratios. 95% confidence intervals and p values for those predictors that were statistically significant are shown in boldface type.
hydromorphone/fentanyl/morphine
Role of Primary Drug and Route of Administration
As shown in Table 2, those who injected their primary drug in the last 30 days were much more likely than non-injectors to use dealers and theft as sources of prescription opioids and much less likely to use a doctor. The selection of a primary drug also influenced the method of diversion. For example, those who used extended release oxycodone as their primary drug (35% of the SKIP population) obtained the drug from a dealer much more frequently than users of other opioids and much less frequently from a doctor. Conversely, users of the second most common primary drug—hydrocodone—were more likely to use a doctor’s prescription and less likely to use dealers to obtain this medication. Primary methadone users were also more likely to use doctor’s prescriptions and less likely to report sharing/trading and theft as sources. Finally, users of high potency opioids, were much less likely to obtain these medications through a doctor’s prescription than those using other opioids.
The South Florida Study
Demographics
Demographic, health, and substance use characteristics of the sample are shown in Table 3. The mean age was 34.6 years (SD 10.6; range 18–59); 56% of respondents were male. The racial/ethnic makeup of the sample reflects the broad diversity of South Florida’s population: 25.8% were African-American/African-Caribbean; 15.7% Hispanic/Latino, 53.6% white and 4.9% other race. Fewer than half (45.5%) of participants reported having any type of health insurance, but a majority (57%) said that their physical health problems limited their ability to carry out vigorous activities, and almost two-thirds (63.3%) reported severe pain in the past 90 days.
Table 3.
Characteristics of Prescription Opioid Abusers in South Florida (N=782)
| N | % | |
|---|---|---|
| Demographics | ||
| Age (mean, SD) | 34.6(10.6) | |
| Male gender | 443 | 56.6 |
| Ethnicity: | ||
| Hispanic | 123 | 15.7 |
| African American/Caribbean | 202 | 25.8 |
| White | 419 | 53.6 |
| Other | 38 | 4.9 |
| Physical Health | ||
| Any health insurance | 356 | 45.5 |
| Health currently limits activities | 447 | 57.2 |
| Severe pain—past 90 days | 494 | 63.3 |
| Substance Use (past 90 days) | ||
| Cocaine (powder) | 477 | 61.0 |
| Crack cocaine | 385 | 49.2 |
| Heroin | 138 | 17.6 |
| Rx benzodiazepines | 627 | 80.2 |
| Injection drug use | 167 | 21.4 |
| Primary opioid used: | ||
| Hydrocodone | 121 | 15.5 |
| IR oxycodone | 454 | 58.1 |
| ER oxycodone | 142 | 18.2 |
| Methadone | 43 | 5.5 |
| High potency (hydromorphone/fentanyl/morphine) | 22 | 2.8 |
| DSM-IV past year dependence | 218 | 27.9 |
| Source(s) of Diverted Primary Opioid | ||
| Dealer | 521 | 66.6 |
| Sharing/Trading | 427 | 54.6 |
| Legitimate Medical Practice | 108 | 13.8 |
| Illegitimate Medical Practice | 98 | 12.5 |
| Theft | 87 | 11.1 |
Illicit and Licit Drug Abuse
Powder cocaine use was reported by 61.0% of respondents, and crack cocaine by 49.2%; illicit substance use, including cocaine as one of the substances, was an eligibility requirement for street users and MSM. Heroin use was reported by only 17.6% of the sample; primary heroin users were not included in the sample analyzed for this paper because of the problematic overlap/substitution with prescription opioids. Current (past 90 day) injection drug use was reported by 21.4% of the sample.
The most commonly reported primary prescription opioid of abuse was immediate release oxycodone, reported by 58.1% of all respondents. Extended release oxycodone was the second most common primary prescription opioid (18.2% of respondents). Hydrocodone was the primary abused prescription opioid for 15.5% of respondents, and the remaining two opioid categories, methadone and high potency opioids medications, were reported to be the primary opioids for few respondents, at 5.5% and 2.8% of the sample respectively. DSM-IVR criteria for substance dependence were met by 27.9% of respondents.
General Patterns of Diversion
Sources through which respondents obtained their primary prescription opioid were diverse, but majorities reported using dealers (66.6%) and sharing or trading with family or friends (54.6%). Just 13.8% of respondents reported obtaining their abused opioids through legitimate medical sources (by doctor shopping or from their regular doctor), likely without the medical provider knowing their patient misused the medications. A somewhat lower proportion (12.5%) of the sample obtained their primary opioid from medical sources who most likely knew that the patient was abusing the drug sources (pharmacies or script doctors). Theft was reported as a diversion source by 11.1% of respondents.
Dealers
The results of bivariate logistic regression models predicting each diversion source for participants’ primary opioid are shown in Table 4. Study respondents who said they used dealers to obtain their primary opioid in the past 90 days were younger, more likely (1.779 times) to be white, and less likely (0.653 times) to be African American than those who did not access their diverted medications through dealers. Primary hydrocodone users were about half (0.444 times) as likely to use dealers to obtain their primary drug compared to respondents who reported other opioids as their primary drug. Those reporting current drug injection were over three (3.537) times, and those meeting DSM-IVR criteria for drug dependence about 50% (1.458 times), more likely to obtain their primary opioid from dealers.
Table 4.
Bivariate Logistic Regressions Predicting Sources of Diverted Primary Opioid (South Florida Opioid Abusers N=782)
| DIVERSION SOURCE [Odds ratio (95% CI) p value]
| |||||
|---|---|---|---|---|---|
| Dealer | Sharing/Trading | Legit. Medical | Illegit. Medical | Theft | |
| Demographics | |||||
| Age (mean) | 0.966 (0.952,0.979) .000 | 0.998 (0.985,1.011) .744 | 1.006 (0.987,1.025) .550 | 1.004 (0.984,1.024) .727 | 0.948 (0.925,0.971) .000 |
| Male gender | 1.147 (0.850,1.547) .370 | 0.902 (0.679,1.199) .478 | 1.037 (0.687,1.563) .864 | 0.771 (0.505,1.179) .230 | 1.095 (0.697,1.721) .694 |
| Ethnicity: | |||||
| Hispanic | 0.778 (0.522,1.158) .216 | 0.555 (0.376,0.819) .003 | 1.084 (0.627,1.873) .773 | 0.506 (0.247,1.033) .061 | 0.669 (0.336,1.332) .253 |
| African American | 0.653 (0.469,0.910) .012 | 1.076 (0.779,1.485) .658 | 0.657 (0.396,1.091) .104 | 1.042 (0.645,1.685) .866 | 0.517 (0.285,0.938) .030 |
| White | 1.779 (1.317,2.401) .000 | 1.262 (0.951,1.674) .107 | 1.307 (0.865,1.974) .203 | 1.501 (0.972,2.320) .067 | 1.850 (1.157,2.960) .010 |
| Physical Health | |||||
| Any health insurance | 0.805 (0.597,1.085) .155 | 0.971 (0.731,1.288) .836 | 1.733 (1.149,2.613) .009 | 1.112 (0.728,1.700) .622 | 0.663 (0.418,1.050) .080 |
| Health limits activities | 0.673 (0.496,0.913) .011 | 1.102 (0.829,1.465) .503 | 1.751 (1.135,2.701) .011 | 1.920 (1.213,3.039) .005 | 0.910 (0.581,1.425) .680 |
| Severe pain—90 days | 1.027 (0.755,1.398) .864 | 1.166 (0.871,1.561) .303 | 1.998 (1.252,3.189) .004 | 2.055 (1.256,3.360) .004 | 1.504 (0.922,2.453) .102 |
| Substance Use—90 days | |||||
| Injected drugs | 3.537 (2.244,5.575) .000 | 1.057 (0.750,1.492) .751 | 2.073 (1.330,3.228) .001 | 1.391 (0.856,2.259) .183 | 3.030 (1.905,4.848) .000 |
| Primary opioid used: | |||||
| Hydrocodone | 0.444 (0.300,0.658) .000 | 0.997 (0.676,1.472) .989 | 1.814 (1.104,2.980) .019 | 0.736 (0.389,1.393) .346 | 0.770 (0.396,1.496) .440 |
| IR oxycodone | 1.342 (0.994,1.812) .055 | 1.292 (0.971,1.719) .078 | 1.059 (0.701,1.601) .785 | 1.221 (0.790,1.887) .369 | 1.803 (1.112,2.922) .017 |
| ER oxycodone | 1.403 (0.938,2.098) .100 | 0.798 (0.554,1.148) .224 | 0.470 (0.245,0.902) .023 | 0.864 (0.489,1.527) .615 | 0.771 (0.415,1.432) .410 |
| Methadone | 1.313 (0.663,2.601) .435 | 0.709 (0.383,1.314) .275 | 0.812 (0.313,2.112) .670 | 0.914 (0.351,2.381).854 | -----------------------------2 |
| High potency1 | 0.490 (0.210,1.146) .490 | 0.685 (0.293,1.606) .385 | 0.985 (0.286,3.387) .981 | 1.574 (0.522,4.752) .421 | 0.794 (0.182,3.457) .759 |
| DSM-IV dependence | 1.458 (1.034,2.056) .031 | 1.025 (0.749,1.403) .877 | 1.048 (0.669,1.644) .837 | 1.164 (0.734,1.846) .519 | 1.117 (0.685,1819) .658 |
hydromorphone/fentanyl/morphine
there were 0 cases of theft for primary methadone users
Sharing
Only one of the measures examined as a predictor of diversion methods was statistically significant for sharing or trading medications to obtain abused opioids: those reporting Hispanic ethnicity were about half (0.555 times) as likely to report this method as non-Hispanics.
Medical Sources
Respondents who reported obtaining their primary opioid from legitimate medical sources were more likely (1.733 times) to have health insurance, and also more likely (1.751 times) to report physical health problems and about twice (1.998 times) as likely to report recent severe pain than those who did not get their abused medications from legitimate medical sources. Those who injected drugs and those whose primary opioid was hydrocodone were also more likely to obtain their abused medications from legitimate medical sources. Primary ER oxycodone abusers were about half (0.470 times) as likely to get their primary opioid from legitimate medical sources compared to participants who reported other primary opioids. Respondents who obtained their primary opioid from illegitimate medical sources (pharmacies and script doctors) were about twice as likely to report physical health limitations and recent severe pain as those who did not use those sources.
Theft
Study respondents who said they used theft to obtain their primary opioid in the past 90 days were younger, more likely (1.850 times) to be white, and less likely (0.517 times) to be African American than those who did not access their diverted medications through theft, the same characteristics as those who obtained their diverted medications from dealers. Drug injectors were about three times as likely to steal their primary opioid as those who did not recently inject drugs. Respondents whose primary opioid was IR oxycodone were more likely (1.803 times) to obtain their drugs by theft than those who reported other opioids as their primary abused opioid.
Discussion
In this paper we explored the factors that influence the diversion of prescription opioids in two studies: first, a nationally-based self-administered brief survey of treatment patients (SKIP); and, second, a highly focused and detailed interview based survey in a number of distinct populations of drug users in South Florida. These studies complement one another and overcome limitations in both, such as the often criticized use of self-administered questionnaires, rather than direct interviews, and the presumed lack of generalizability in focused regional analyses (Aquilino, 1994; Aquilino & LoSciuto, 1990; Hochstim, 1967; Manchikanti et al., 2010; Monheit, 2010; Okamoto et al., 2002; Robling et al, 2010; Ruetsch, 2010; Strassels, 2009; Tourangeau & Smith, 1996). Our results suggest very comparable results between the two distinctly different studies, thus validating the use of both paradigms in drug abuse related studies.
As mentioned above, there has been a surge in the non-therapeutic use of prescription opioids in the past 15 years (Inciardi et al., 2009; Monheit, 2010; Manchikanti et al., 2010; Ruetsch, 2010; Strassels, 2010; Zacny et al., 2003). Since it is rare for legitimate patients to abuse their opioid medications, the appetite for these drugs is primarily driven by non-patients who seek them for their mood-altering or other non-therapeutic effects. Thus, the accessibility of these drugs to the abuser is the result of their diversion from legal sources to the illicit market place. Previous research has suggested a variety of diversion mechanisms (CASA, 2004; Inciardi, 2005; Inciardi & Surratt, 2005; Leiderman, 2006; NADDI [abed], 2005; Weathermon, 1999); however, there is limited systematic evidence to support each of these diversion channels, and there are no empirical data on the magnitude of particular types of diversion and the factors that influence the diversion method selected (Dart, 2009; Dasgupta & Schnoll, 2009; Johanson et al., 2009; Liederman, 2009; McCormick, 2006; Sapienza, 2006). The present studies provide the first empirical data on the scope and magnitude of diversion among a nationally representative sample of dependent (DSM-IV) misusers entering drug treatment programs and a diverse population of dependent and non-dependent individuals in South Florida.
In general terms, the SKIP data indicate that dependent prescription opioid abusers used dealers as their primary source (>50%) followed at some distance by sharing and doctor’s prescriptions. However, when asked to list all methods of diversion in the past 30 days—dealers, sharing, and doctor’s prescriptions were selected with almost equal frequency. Surprisingly, despite wide-spread reports and speculation, particularly from the DEA and a great deal of media coverage (GAO, 2003), SKIP respondents rarely resorted to theft, forged prescriptions or other illegal activities to obtain their drugs of choice. These data are consistent with the view that risk-aversiveness is a prominent trait of prescription opioid abusers quite unlike that observed with users of illicit opioids, crack, methamphetamines and other illicit drugs. This was true even among the South Florida sample, which included many illicit drug abusers.
While the general conclusions outlined above apply to the overall population of prescription opioid abusers, our studies indicate substantial differences in diversion by age, gender, route of administration and the selection of a primary drug.
In terms of the likelihood of using various methods of diversion, it appears, as mentioned above, that risk aversiveness may play a prominent role. For example, older people and non-injectors avoided dealers and theft, but preferred physician practices as their source of drugs. These data are consistent with many studies suggesting that younger age is associated with higher levels of risk taking (Haase & Silbereisen, 2010).
Both studies presented here also showed similar socioeconomic and health predictors of abusers’ sources of diverted medications. Those with access to resources—health insurance in the South Florida study, and higher income in the SKIP study—were more likely to obtain abused opioid medications from medical system sources. Those with severe pain and physical health problems were also more likely to go to physicians, legitimate or not, for their opioid drugs.
The other major theme emerging from our studies is that the choice of a primary drug strongly influences the method of diversion. Perhaps, the clearest examples of this are evident with the two most commonly abused opioids in this country: OxyContin (35% of the SKIP sample) and hydrocodone (26% of the sample). In both studies, for those for whom OxyContin was their drug of choice, dealers were more likely to be reported (not quite reaching the .05 level of significance in the South Florida study) and doctors were less likely to be reported. Precisely the opposite pattern was observed for hydrocodone users in which dealers were rarely used, but doctors were commonly used. While the factors underlying these differences may be numerous, the most probable ones are cost, availability, and a physician’s willingness to prescribe the medication. Hydrocodone products are the most widely prescribed opioid analgesics in this country, outpacing oxycodone by more than 2 to 1. Thus, doctors are obviously willing to prescribe it and, even with a relatively small percent of diversion from medical to non-medical channels, supplies are large in both the licit and illicit market place. Thus, there may be little reason for users to resort to a dealer’s “marked-up” prices when hydrocodone can be easily and safely obtained elsewhere, particularly from a doctor or friends and family at relatively little cost.
The latter point may also explain the pattern of diversion for OxyContin users. Doctors have grown wary of prescribing OxyContin given the media coverage of its abuse and overdose deaths (Sproule, Brands, Li, & Catz-Biro, 2009). Perhaps more importantly, insurance companies have become increasingly unwilling to pay for expensive OxyContin, as a brand name with no currently available generic, when there are far cheaper opioid alternatives (e.g. hydrocodone) and, increasingly, methadone. Thus, doctors may no longer be as reliable a diversion source for OxyContin as they once were and, as a result the decline in its medical use makes the drug less available from friends or families for sharing. As a consequence, dealers may have become a more reliable outlet for OxyContin, which retains its popularity as a “street drug” because it contains up to 10–15 times more active ingredient than IR oxycodone or all hydrocodone products. Ironically, in our capitalistic system the great demand for OxyContin has driven prices to extremely high levels (e.g., $ 1 per milligram) making this drug far more expensive than heroin in most communities, generating a dangerous anomaly not seen before in the opioid abuse field: Heroin has become a secondary drug when the preferred drug—OxyContin—is unaffordable or in short supply (Spiller, Bailey, Dart, & Spiller, 2010; Sproule et al., 2009).
As mentioned above, the reluctance of doctors to use the widely abused OxyContin and the unwillingness of insurance companies to pay for it has had the unintended consequence of increasing the use and abuse of methadone (Cai, Crane, Poneleit, & Paulozzi, 2010; Paulozzi et al., 2009). Aside from making doctors the primary source of methadone for substance abusers, this has led to a marked increase in the abuse of methadone, previously rarely abused, and an unfortunate increase in fatal overdoses (Paulozzi et al., 2009; Braden et al., 2010; Sale, Thielke, & Topolovec-Vranic, 2010). The latter is probably due to the lack of knowledge of the pharmacology and toxicology by both users and doctors.
As mentioned above, the two studies described in this paper were undertaken to provide complimentary empirical data on the methods of diversion used by prescription opioid users entering treatment (SKIP) and in the broader spectrum of opioid misusers either in or out of treatment in the South Florida study. Thus, the later study assesses diversion in both dependent and recreational users, whereas the SKIP study consists solely of only dependent individuals. Interestingly, when examining only dependent individuals the two studies yielded almost identical results: dealers were by far the primary mode of diversion. On the other hand, non-dependent individuals tend to use dealers less frequently, apparently preferring sharing, trading, and doctor’s prescriptions as sources of their drugs. In addition to this important distinction, the complementary nature of the two studies validates that the use of self-administered surveys produces results almost identical to those achieved with direct interviews. While some prior investigations have suggested this to be the case, many more investigators believe self-administered surveys are not credible (Aquilino, 1994; Aquilino & LoSciuto, 1990; Hochstim, 1967; Okamoto et al., 2002; Robling et al., 2010; Tourangeau & Smith, 1996), particularly with respect to drug abuse and misuse studies. However, the latter conclusion has rarely been based on direct comparisons between the two methodologies as has been done in the current studies. Thus, we believe our results indicate that both self-administered and interview based studies produce valid data. Additionally, focused studies in one city or region are often criticized for lack of generalizability to a national sample (Aquilino, 1994; Aquilino&LoSciuto, 1990;Hochstim, 1967; Okamotoetal., 2002; Robling et al., 2010; Tourangeau & Smith, 1996). Once again our results suggest that this criticism may be overstated given the close correspondence between our results.
In conclusion, our data clearly indicate that the use of the term diversion to describe the access of non-patients to prescribed medications is a misnomer since it is not a unitary concept. Rather, there appears to be almost as many methods of “diversion” as there are groups of people who misuse opioid medications. This information is important as we consider prevention and intervention strategies for reigning in the national epidemic of prescription drug abuse: a one size fits-all approach to limiting access through diversion will clearly not address the illegal channeling of opioids from medical non-medical channels.
Acknowledgments
This study was supported by a grant from Denver Health and Hospital Authority, under the auspices of the Researched Abuse, Diversion and Addiction-Related Surveillance (RADARS®) program and by Grant #R01DA021330 from the National Institute on Drug Abuse.
Biographies
Theodore J. Cicero, Ph.D., serves as a Professor of Psychiatry at Washington University School of Medicine. His research is focused on the nature and characteristics of the abuse and diversion of prescription opioid analgesics.
Steven P. Kurtz, Ph.D., is Senior Scientist and Associate Director of the Coral Gables, Florida office of the Center for Drug and Alcohol Studies at the University of Delaware. He is a NIDA-funded investigator with a research focus on the development of HIV and substance abuse prevention interventions.
Hilary L. Surratt, Ph.D., is a Senior Scientist, Center for Drug and Alcohol Studies, University of Delaware. She is Principal Investigator of a NIDA-funded epidemiologic study of antiretroviral medication diversion among HIV+ substance abusers in Miami, and has published widely in the areas of HIV/AIDS, substance abuse, and drug diversion.
Matthew S. Ellis is a graduate student in the Masters of Psychiatric Epidemiology program at Washington University in St. Louis and has worked closely with Dr. Theodore J. Cicero for several years, recently publishing works with him on the abuse of prescription opiates.
Gladys E. Ibañez is an Associate Scientist with the Center for Drug and Alcohol Studies at the University of Delaware. She served as project manager for the South Florida Health Study. Her current research interests include HIV prevention among Latino populations, prescription drug misuse, and women’s health.
Maria A. Levi-Minzi, MA, is a Research Associate at the Center for Drug and Alcohol Studies at the University of Delaware. She is project director for the South Florida Health Survey, a NIDA funded study of prescription drug abuse and diversion.
James A. Inciardi, Ph.D., was Professor in the Department of Sociology and Criminal Justice and Founding Director of the Center for Drug and Alcohol Studies at the University of Delaware.
References
- Aquilino W. Interview mode effects in surveys of drug and alcohol use. Public Opinion Quarterly. 1994;54:362–395. [Google Scholar]
- Aquilino W, LoSciuto L. Effect of interview mode on self-reported drug use. Public Opinion Quarterly. 1990;58:210–240. [Google Scholar]
- Bergman U, Dahl-Puustinen ML. Use of prescription forgeries in a drug abuse surveillance network. European Journal of Clinical Pharmacology. 1989;36(6):621–623. doi: 10.1007/BF00637747. [DOI] [PubMed] [Google Scholar]
- Blumenschein K. Prescription drug diversion: Fraudulent tactics utilized in the community pharmacy. American Journal of Pharmaceutical Education. 1997;61(2):184–188. [Google Scholar]
- Borsack S. Hospital drug diversion: The verdict is in. Health Matrix. 1986–87;4(4):27–31. [PubMed] [Google Scholar]
- Braden JB, Russo J, Fan MY, Edlund MJ, Martin BC, DeVries A, Sullivan MD. Emergency department visits among recipients of chronic opioid therapy. Archives of Internal Medicine. 2010;170(16):1425–1432. doi: 10.1001/archinternmed.2010.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai R, Crane E, Poneleit K, Paulozzi L. Emergency department visits involving nonmedical use of selected prescription drugs in the United States, 2004–2008. Journal of Pain and Palliative Care Pharmacotherapy. 2010;24(3):293–297. doi: 10.3109/15360288.2010.503730. [DOI] [PubMed] [Google Scholar]
- CASA (The National Center on Addiction and Substance Abuse at Columbia University) “You’ve got drugs!”: Prescription drug pushers on the Internet [Online] 2004 Retrieved October 31, 2010 from http://www.casacolumbia.org/Absolutenm/articlefiles/you_ve_got_drugs.pdf.
- Cicero TJ, Ellis MS, Paradis A, Ortbal Z. Determinants of fentanyl and other potent μ opioid agonist misuse in opioid-dependent individuals. Pharmacoepidemiology and Drug Safety. 2010;19(1):1–7. doi: 10.1002/pds.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Surratt H, Inciardi JA. Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban and urban locations in the United States. Pharmacoepidemiology and Drug Safety. 2007;16(8):827–840. doi: 10.1002/pds.1452. [DOI] [PubMed] [Google Scholar]
- Cooper JR, Czechowicz DJ, Petersen RC, Molinari SP. Prescription drug diversion control and medical practice. Journal of the American Medical Association. 1992;268(10):1306–1310. [PubMed] [Google Scholar]
- Dart RC. Monitoring risk: Post marketing surveillance and signal detection. Drug and Alcohol Dependence. 2009;105(Suppl 1):S26–S32. doi: 10.1016/j.drugalcdep.2009.08.011. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Schnoll SH. Signal detection in post-marketing surveillance for controlled substances. Drug and Alcohol Dependence. 2009;105(Suppl 1):S33–S41. doi: 10.1016/j.drugalcdep.2009.05.019. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker JI, Hodgkins D. Global Appraisal of Individual Needs - Initial (GAIN-I) Bloomington, IL: Chestnut Health Systems; 2002. [Google Scholar]
- General Accounting Office, U.S. OxyContin Abuse and Diversion and Efforts to Address the Problem [Report to Congressional Requesters, #GAO-04-110] Washington, DC: U.S. Government Printing Office; 2003. [Google Scholar]
- Haase CM, Silbereisen RK. Effects of positive affect on risk perceptions in adolescence and young adulthood. Journal of Adolescence. 2010;34(1):29–37. doi: 10.1016/j.adolescence.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Hochstim J. A critical comparison of three strategies of collecting data from households. Journal of the American Statistical Association. 1967;62:976–989. [Google Scholar]
- Hollinger RC, Dabney DA. Social factors associated with pharmacists’ unauthorized use of mind-altering prescription medications. Journal of Drug Issues. 2002;32(1):231–264. [Google Scholar]
- Inciardi JA. Trends in the Diversion of Prescription Drugs. Paper presented at the 16th Annual Training Conference of the National Association of Drug Diversion Investigators; Myrtle Beach, SC. 2005. [Google Scholar]
- Inciardi JA, Surratt HL. Researching the Abuse and Diversion of Prescription Drugs. Paper presented at the Abbott Laboratories Symposium on Prescription Drug Abuse; Chicago. 2005. [Google Scholar]
- Inciardi JA, Surratt HL, Cicero TJ, Rosenblum A, Ahway C, Bailey JE, Dart RC, Burke JJ. Prescripton drugs purchased through the Internet: who are the end users? Drug and Alcohol Dependence. 2010;110(1–2):21–29. doi: 10.1016/j.drugalcdep.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Stivers Y, Cicero TJ. FDA approvals of generic drugs: Impact on the diversion of opioid analgesics with a potential for abuse. Journal of Opioid Management. 2009;5(2):81–87. doi: 10.5055/jom.2009.0009. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Balster RL, Henningfield JE, Schuster CR, Anthony JC, Barthwell AG, Coleman JJ, Dart RC, Gorodetzky CW, O’Keeffe CO, Sellers EM, Vocci F, Walsh SL. Risk management and post-marketing surveillance for the abuse of medications acting on the central nervous system: Expert panel report. Drug and Alcohol Dependence. 2009;105(Suppl 1):S33–S41. doi: 10.1016/j.drugalcdep.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiderman DB. Risk management of drug products and the U. S. Food and Drug Administration: Evolution and context. Drug and Alcohol Dependence. 2009;105(Suppl 1):S9–S13. doi: 10.1016/j.drugalcdep.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapuetic use, abuse and nonmedical use of opioids: A ten-year perspective. Pain Physician. 2010;13(5):401–435. [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. The use, misuse and diversion of prescription stimulants among middle and high school students. Substance Use and Misuse. 2004;39(7):1095–1116. doi: 10.1081/ja-120038031. [DOI] [PubMed] [Google Scholar]
- McCormick CG. Regulatory challenges for new formulations of controlled substances in today’s environment. Drug and Alcohol Dependence. 2006;83(Suppl 1):S63–S67. doi: 10.1016/j.drugalcdep.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Monheit B. Prescription drug misuse. Australian Family Physician. 2010;39(8):540–546. [PubMed] [Google Scholar]
- NADDI, National Association of Drug Diversion Investigators. RxPatrol Alert: Delivered Drugs Stolen- Wisconsin. 2005a. Mar 7, 2005. [Google Scholar]
- NADDI, National Association of Drug Diversion Investigators. RxPatrol Alert: Stolen Prescription Blanks-Texas. 2005b. Mar 2, 2005. [Google Scholar]
- NADDI, National Association of Drug Diversion Investigators. RxPatrol Alert: Pharmacy Robbery-Florida, North Melbourne. 2005c. Mar 2, 2005. [Google Scholar]
- NADDI, National Association of Drug Diversion Investigators. RxPatrol Alert: Pharmacy Burglary-Massachusetts, Peabody. 2005d. Mar 2, 2005. [Google Scholar]
- Okamoto K, Ohsuka K, Shiraishi T, Hukazawa E, Wakasugi S, Furuta K. Comparability of epidemiological information between self- and interviewer-administered questionnaires. Journal of Clinical Epidemiology. 2002;55(5):505–511. doi: 10.1016/s0895-4356(01)00515-7. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction. 2009;104(9):1541–1548. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- Rigg KK, March SJ, Inciardi JA. Prescription drug abuse & diversion: Role of the pain clinic. Journal of Drug Issues. 2010;40(3):681–702. doi: 10.1177/002204261004000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robling MR, Ingledew DK, Greene G, Sayers A, Shaw C, Sander L, Russell IT, Williams JG, Hood K. Applying an extended theoretical framework for data collection mode to health services research. BMC Health Services Research. 2010;10:180. doi: 10.1186/1472-6963-10-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruetsch C. Empirical view of opioid dependence. Journal of Managed Care Pharmacy. 2010;16(1 Suppl B):S9–S13. doi: 10.18553/jmcp.2010.16.S1-B.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sale JE, Thielke S, Topolovec-Vranic J. Who is addicted to, and dying from, prescription opioids? Journal of the American Geriatrics Society. 2010;58(7):1401–1402. doi: 10.1111/j.1532-5415.2010.02902.x. [DOI] [PubMed] [Google Scholar]
- Sapienza FL. Abuse deterrent formulations and the Controlled Substances Act (CSA) Drug and Alcohol Dependence. 2006;83(Suppl 1):S23–S30. doi: 10.1016/j.drugalcdep.2005.11.028. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, Tompkins C. Balancing Diversion Control and Medical Necessity: The Case of Prescription Drugs with Abuse Potential. Substance Use and Misuse. 2001;36(9&10):1275–1296. doi: 10.1081/ja-100106227. [DOI] [PubMed] [Google Scholar]
- Spiller H, Bailey JE, Dart RC, Spiller SS. Investigation of temporal changes of abuse and misuse of prescription opioids. Journal of Addictive Diseases. 2010;29(1):78–83. doi: 10.1080/10550880903436036. [DOI] [PubMed] [Google Scholar]
- Sproule B, Brands B, Li S, Catz-Biro L. Changing patterns in opioid addiction: Characterizing users of oxycodone and other opioids. Canadian Family Physician. 2009;55(1):68–69. 69.el-5. [PMC free article] [PubMed] [Google Scholar]
- Strassels SA. Economic Burden of prescription opioid misuse and abuse. Journal of Managed Care Pharmacy. 2009;15(7):556–562. doi: 10.18553/jmcp.2009.15.7.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourangeau R, Smith TW. Asking sensitive questions: The impact of data collection mode, question format, and question context. Public Opinion Quarterly. 1996;60:275–304. [Google Scholar]
- Trinkoff AM, Storr CL, Wall MP. Prescription-type drug misuse and workplace access among nurses. Journal of Addictive Diseases. 1999;18(1):9–17. doi: 10.1300/J069v18n01_02. [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Zhou Q, Storr CL, Soeken KL. Workplace access, negative proscriptions, job strain, and substance use in registered nurses. Nursing Research. 2000;49(2):83–90. doi: 10.1097/00006199-200003000-00004. [DOI] [PubMed] [Google Scholar]
- Weathermon RA. Controlled substances diversion: Who attempts it and how. US Pharmacist. 1999;24(12):32–47. [Google Scholar]
- Weir E. Substance abuse among physicians. Journal of Ayub Medical College. 2000;162(12):1730. [PMC free article] [PubMed] [Google Scholar]
- Wilford BB, Finch J, Czechowicz DJ, Warren D. An overview of prescription drug misuse and abuse: Defining the problem and seeking solutions. The Journal of Law, Medicine & Ethics. 1994;22(3):197–203. doi: 10.1111/j.1748-720x.1994.tb01295.x. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on problems of drug dependence taskforce on prescription opioid non-medical use and abuse: Position statement. Drug and Alcohol Dependence. 2003;69(3):215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]


