Summary
Background and objectives
This study measured the association between the Acute Kidney Injury Network (AKIN) diagnostic and staging criteria and surrogates for baseline serum creatinine (SCr) and body weight, compared urine output (UO) with SCr criteria, and assessed the relationships between use of diuretics and calibration between criteria and prediction of outcomes.
Design, setting, participants, & measurements
This was a retrospective cohort study using prospective measurements of SCr, hourly UO, body weight, and drug administration records from 5701 patients admitted, after cardiac surgery, to a cardiac intensive care unit between 1995 and 2006.
Results
More patients (n=2424, 42.5%) met SCr diagnostic criteria with calculated SCr assuming a baseline estimated GFR of 75 ml/min per 1.73 m2 than with known baseline SCr (n=1043, 18.3%). Fewer patients (n=484, 8.5%) met UO diagnostic criteria with assumed body weight (70 kg) than with known weight (n=624, 10.9%). Agreement between SCr and UO criteria was fair (κ=0.28; 95% confidence interval 0.25–0.31). UO diagnostic criteria were specific (0.95; 0.94–0.95) but insensitive (0.36; 0.33–0.39) compared with SCr. Intravenous diuretics were associated with higher probability of falling below the UO diagnostic threshold compared with SCr, higher 30-day mortality (relative risk, 2.27; 1.08–4.76), and the need for renal support (4.35; 1.82–10.4) compared with no diuretics.
Conclusions
Common surrogates for baseline estimated GFR and body weight were associated with misclassification of AKIN stage. UO criteria were insensitive compared with SCr. Intravenous diuretic use further reduced agreement and confounded association between AKIN stage and 30-day mortality or need for renal support.
Introduction
The Acute Dialysis Quality Initiative group developed the risk, injury, failure, loss, and end-stage kidney staging criteria (also known as RIFLE) (1) based on changes in serum creatinine (SCr) and urine output (UO). These criteria were modified by the Acute Kidney Injury Network (AKIN) (Table 1) (2). More than 50 original studies have aimed to validate these criteria but the retrospective nature of the majority limits the collection of certain data, requiring the use of surrogates for unknown clinical parameters.
Table 1.
AKIN diagnostic and staging criteria
| AKIN Stage | SCr Criteria | UO Criteria |
|---|---|---|
| 1 | SCr increase ≥0.3 mg/dl or SCr ≥1.5- to 2-fold increase from baseline | <0.5 ml/kg per hour for >6 h |
| 2 | SCr >2- to 3-fold increase from baseline | <0.5 ml/kg per hour for >12 h |
| 3 | SCr >3-fold increase from baseline or SCr ≥4 mg/dl (with acute increase of ≥0.5 mg/dl within 24 h) or initiation of RRT (irrespective of stage at time of initiation) | <0.3 ml/kg per hour for 24 h or anuria for 12 h |
A diagnosis is made if at least stage 1 is reached within a 48-hour period; severity is described by the maximum stage reached within a 7-day timeframe. It is assumed that the patient is volume replete (to exclude prerenal azotemia) and that urinary obstruction has been excluded. Details regarding AKIN are available in Mehta et al. (2). AKIN, Acute Kidney Injury Network; SCr, serum creatinine, UO, urine output; RRT, renal replacement therapy.
The Acute Dialysis Quality Initiative group recommended calculation from an assumed estimated GFR (eGFR) using the Modification of Diet in Renal Disease (MDRD) equation in situations in which baseline SCr is unknown (1). Although utilized in previous studies (3–7), only recently has the clinical validity of this assumption been questioned (8) and shown to result in significant bi-directional misclassification (6).
Hourly UO data are difficult to estimate retrospectively. The use of UO criteria has been frequently omitted or unspecified (4,5,9–16). One systematic review found only 12% of the available population to have both SCr and UO criteria included in analyses (17). Two of the largest studies (7,18) having only 24-hour cumulative UO values were forced to modify AKIN criteria, with one also normalizing urine flow rates to an assumed body weight of 70 kg (7). Uncertainty remains over how well UO and SCr criteria are calibrated. A further unanswered question is the effect of diuretics on UO criteria. The rationale of this study was to question the accuracy of calibration and the validity of common assumptions and to establish whether these tools have any utility in prospective clinical and research settings.
We hypothesized that the use of surrogate assumptions about baseline creatinine and body weight as well as the use of diuretics would be associated with misclassification in AKIN staging. This study aimed to test this hypothesis in a cohort of patients after cardiac surgery and to show how well SCr and UO criteria calibrated in their capacity for AKI staging. We also discuss the utility of this tool in prospective clinical and research settings.
Materials and Methods
Study Design
This is a retrospective cohort study using data collected prospectively over a 12-year period from a homogeneous cohort of patients admitted to an intensive care unit (ICU) after cardiac surgery with a known time of insult.
Participants
We studied electronic health records from patients admitted to the adult cardiothoracic ICU at Freeman Hospital, Newcastle upon Tyne, United Kingdom, after nontransplant, cardiac surgery. Data were extracted from three sources (Table 2) with eligibility criteria applied sequentially (Figure 1). Linked records, extracted with scripts written in perl programming language (www.perl.org), were combined into a single database for further analysis. Accuracy was confirmed by checking a random sample against source records and by tallying total numbers of observations. We excluded patients with a baseline SCr of ≤25 µmol/L to allow calculation of a clinically meaningful eGFR using the four-variable MDRD formula (19).
Table 2.
Sources of data and fields extracted from each source
| Source | Description | Fields |
|---|---|---|
| 1 | Ward admissions database (records extracted via queries using SQL)a | Hospital number |
| Date of admission | ||
| Age at admission (yr) | ||
| Weight at admission (kg) | ||
| Diabetic at admission (yes/no) | ||
| Operation (coded) | ||
| Died during stay in ICU (yes/no) | ||
| 2 | Hospital patient administration system (records extracted via queries using SQL) | Hospital number |
| Sex | ||
| Ethnicity (coded) | ||
| Date of death (for calculation of 30-d mortality rate) | ||
| 3 | Daily ICU observations (records extracted from structured text files using perl scripts)b | Date of observation |
| Hospital number | ||
| Urine output (hourly volume) | ||
| Serum creatinine (and time of sample) | ||
| Renal replacement therapy | ||
| Drug administrations (drug, date, time, dose, route), chosen from “pick lists” or entered as free text |
SQL, structured query language; ICU, intensive care unit.
Populated from paper forms completed by nursing staff, validated by a consultant anaesthetist, and keyed into a database by a departmental secretary.
Electronic bedside data recording.
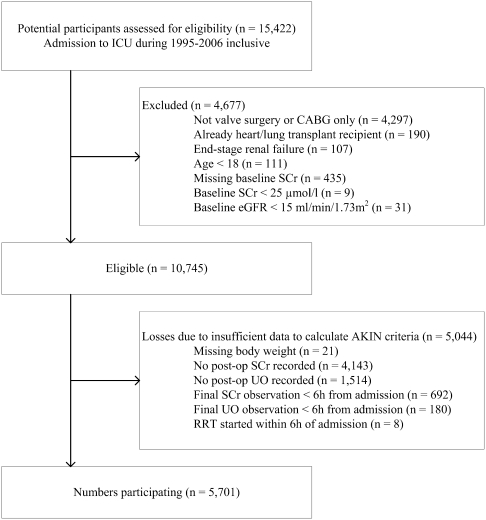
Figure 1.
Flow diagram showing how many patients were excluded for each eligibility criterion and the number lost because of insufficient data available to apply the AKIN criteria. Some patients did not meet more than one eligibility criterion and some were lost because of insufficiency of more than one type of observation. ICU, intensive care unit; CABG, coronary artery bypass graft surgery; SCr, serum creatinine; eGFR, estimated GFR; AKIN, Acute Kidney Injury Network; SCr, serum creatinine, UO, urine output; RRT, renal replacement therapy.
AKIN criteria were applied to a period of continuous observation starting from admission to the ICU and ending at the earliest of (1) the last in a series of SCr measurements (starting with baseline SCr) each separated by ≤48 hours from the previous one; (2) the final in a series of postoperative UO measurements, each separated by ≤6 hours from the previous one; and (3) the earliest initiation of renal replacement therapy (RRT).
This approach recognized that in normal practice, observations are sometimes missed or not recorded. Periods of extended missing observations that prevented correct application of the AKIN criteria caused termination of the continuous observation period.
Reclassification of AKIN Stage with Assumed Baseline eGFR and Assumed Body Weight
A baseline eGFR of 75 ml/min per 1.73 m2 was used to derive an assumed baseline SCr using the inverted MDRD formula with known age, sex, and ethnicity. Proportions of patients meeting each AKIN SCr criteria, with actual and assumed baseline SCr, were compared by calculating relative risk (RR). Each UO criteria was assessed by calculating UO per kilogram per hour, with known body weight versus an assumed body weight of 70 kg.
Association between Reclassification of AKIN Stage and Outcomes: RRT and 30-Day Mortality
Thirty-day mortality rates (from time of ICU admission) and proportions of patients on whom RRT was initiated during their ICU stay for each AKIN stage were calculated for actual and assumed baseline eGFR and body weight.
Calibration of UO Criteria Relative to SCr and Its Association with Diuretic Use
Proportions of patients classified into each AKIN stage or falling below the diagnostic threshold, by each set of criteria, were compared using RR. The κ statistic was used to calculate the level of agreement from a cross-tabulation with ordered nominal scales from 0 (below diagnostic threshold) to 3 (AKIN stage 3). Sensitivity, specificity, and positive and negative predictive values were calculated using SCr as the reference.
Each patient was assigned to one of four categories according to type of relevant drug administration: 0, no diuretics (n=2694); 1, oral diuretics (n=7); 2, intravenous dopamine or dopexamine only (n=55); or 3, intravenous diuretics (n=2945), for any dose, for any time during the period of continuous observation.
Drugs considered as diuretics included the following: acetazolamide, bendroflumethiazide, bumetanide, co-amilofruse, eplerenone, furosemide, mannitol, metolazone, and spironolactone. Patients in categories 1 and 2 comprised approximately 1% of the analyzed population and thus were excluded from further analysis. The accuracy of capture of free text drug entries (Table 2) was assessed by manual cross-checking of an extracted list of unique drug names, created and sorted using structured query language text-processing statements, by two co-authors (N.S.K. and A.J.S.).
The RR was used to compare the association between diuretic use and proportions of patients classified into different AKIN stages by the SCr (with known baseline SCr) and UO (with known body weight) criteria, as well as its association with the need for RRT and 30-day mortality.
Results
Participants
The number of admissions that met each eligibility criterion and for which sufficient observations were recorded to apply AKIN criteria was 5701 (Figure 1). Of these, 74% were men and 13% had diabetes; 70% had coronary artery bypass graft surgery (CABG) only, 18% had valve repair or replacement surgery only, and the remainder had both coronary artery bypass graft surgery and valve repair/replacement surgery. The mean age was 65.4 years (range, 20–94 years). Mean (SD) baseline eGFR was 59.1 (14.5) ml/min per 1.73 m2 (Figure 2) and measured body weight was 79.2 (15.3) kg (Figure 3).
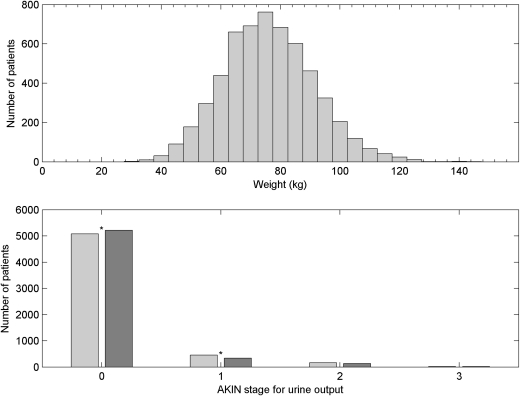
Figure 2.
Reclassification of AKIN stage with assumed baseline estimated GFR (eGFR). (Top) Distribution of eGFR in the study population (n=5701) calculated with the Modification of Diet in Renal Disease formula (1,19) from measurements of serum creatinine (SCr) taken preoperatively. (Bottom) Acute Kidney Injury Network (AKIN) (2) staging for SCr criteria with measured preoperative SCr (light shading) compared with stage calculated with a baseline eGFR of 75 ml/min per 1.73 m2 (dark shading). Differences in the proportion of patients meeting the diagnostic criteria (stages 1, 2, or 3) and meeting the criteria for stages 1, 2, and 3 individually are significant at the 95% confidence level. Significant differences are marked with asterisks.
Figure 3.
Reclassification of AKIN stage with assumed body weight. (Top) Distribution of body weight at admission in the study population (n=5701). (Bottom) Acute Kidney Injury Network (AKIN) (2) stage for urine output criteria calculated with known body weight (light shading) compared with staging calculated with an assumed body weight of 70 kg (dark shading). Differences in the proportion of patients meeting the diagnostic criteria for urine output (stages 1, 2, or 3) and meeting the urine output criteria for stage 1 are significant at the 95% confidence level. Significant differences are marked with asterisks.
Reclassification of AKIN Stage with Assumed Baseline eGFR and Assumed Body Weight
With assumed baseline SCr, AKI could be diagnosed in 2424 (42.5%) patients and 1043 (18.3%) with actual baseline (Figure 2). This difference was significant with a RR (assumed/actual baseline) of 2.32 (95% confidence interval [95% CI], 2.18–2.47).
Significant differences in the proportions of patients placed into each AKIN stage were also found, with a RR of 2.11 (95% CI, 1.96–2.27) for stage 1, 2.60 (2.19–3.08) for stage 2, and 4.77 (3.54–6.42) for stage 3.
Assumed body weight resulted in significantly fewer patients meeting UO diagnostic criteria (n=484 [8.5%] versus n=624 [10.9%] using actual weight; RR, 0.78 [95% CI, 0.69–0.87]) and significantly reduced proportions reaching AKI stage 1 by UO criteria (RR [assumed/actual weight], 0.75 [0.66–0.86]) but not stages 2 or 3 (Figure 3).
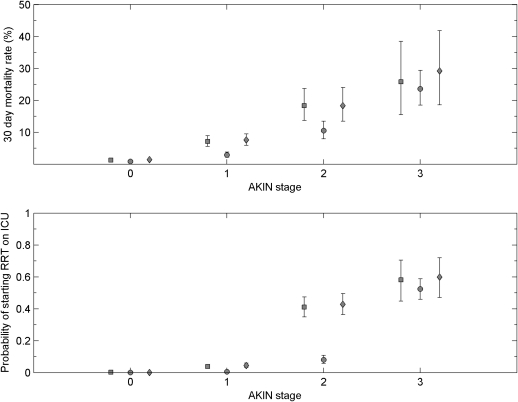
Association between Reclassification of AKIN Stage and Outcomes: RRT and 30-Day Mortality
Higher stage was associated with higher 30-day mortality (Figure 4). Assumed baseline eGFR caused significant errors in estimates of 30-day mortality risk for AKIN stages 1 and 2 compared with known baseline eGFR (RR, 0.41 [95% CI, 0.29–0.58] for stage 1; and RR, 0.57 [0.40–0.83] for stage 2).
Figure 4.
Association between reclassification of AKIN stage and outcomes. (Top) Estimated 30-day mortality rate for each Acute Kidney Injury Network (AKIN) stage (2) for all eligible patients (n=5701). (Bottom) Estimated probability of initiating renal replacement therapy during ICU stay for each AKIN stage (2). No assumptions of body weight or preadmission estimated GFR (filled squares), assumed pre-admission eGFR of 75 ml/min per 1.73 m2 (filled circles), and assumed body weight of 70 kg (filled diamonds). Error bars are 95% confidence intervals of the proportion. RRT, renal replacement therapy; ICU, intensive care unit.
Higher stage was associated with higher probability of receiving RRT (Figure 4). Assumed baseline eGFR caused significant errors in estimates of probability of receiving RRT compared with known baseline for AKIN stage 1 (RR, 0.16 [95% CI, 0.08–0.31]) and stage 2 (RR, 0.20 [0.14–0.27]).
Calibration of UO Criteria Relative to SCr and Its Association with Diuretic Use
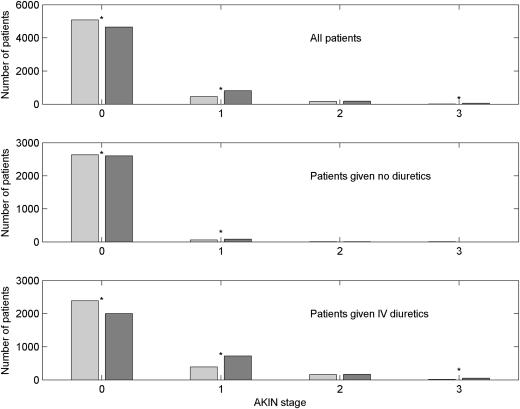
Significant differences in proportions (UO criteria/ SCr criteria) were detected (Figure 5) for stage 0 (RR [95% CI], 1.09 [1.07–1.11]), stage 1 (RR, 0.56 [0.50–0.62]), and stage 3 (RR, 0.21 [0.11–0.40]). From the cross-tabulation of AKIN stage (Table 3), the κ coefficient (20,21) was 0.28 (95% CI, 0.25–0.31), which was considered, conventionally, as “fair agreement.” For diagnostic criteria alone, with SCr as a reference, the sensitivity (95% CI) of the UO criteria was 0.36 (0.33–0.39), specificity was 0.95 (0.94–0.95), positive predictive value was 0.60 (0.56–0.63), and negative predictive value was 0.87 (0.86–0.88).
Figure 5.
Number of patients who met Acute Kidney Injury Network (AKIN) criteria 1, 2, and 3 (2) and the number not meeting diagnostic criteria (stage 0) for urine output (light shading) and for serum creatinine (dark shading) separately. (Top) All eligible patients (n=5701). (Middle) patients given no diuretics (n=2694). (Bottom) Patients given intravenous (IV) diuretics (n=2945). Significant differences are marked with asterisks.
Table 3.
Cross-tabulation for the comparison of AKIN stage for SCr and UO criteria for all patients
| AKIN Stage (UO criteria) | AKIN Stage (SCr Criteria) | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | Total | |
| 0 | 4405 | 589 | 68 | 15 | 5071 |
| 1 | 225 | 169 | 45 | 14 | 453 |
| 2 | 27 | 55 | 56 | 22 | 160 |
| 3 | 1 | 3 | 6 | 1 | 11 |
| Total | 4658 | 816 | 175 | 52 | 5701 |
AKIN, Acute Kidney Injury Network; SCr, serum creatinine, UO, urine output.
For those patients given no diuretics (Figure 5), there was a statistically significant, but clinically insignificant, difference in the proportion classified at stage 0 by the two criteria (RR [UO criteria/SCr criteria], 1.01; 95% CI, 1.00–1.02) and a significant difference between the proportions at stage 1 (RR, 0.70; 0.51–0.98). No significant differences were found at stages 2 or 3. For those who received intravenous diuretics, a significantly greater proportion of patients fell below the diagnostic criteria for UO compared with SCr (RR, 1.19; 95% CI, 1.16–2.23); smaller proportions of patients (UO/SCr) were classified at stage 1 (RR, 0.54; 0.48–0.60) and stage 3 (0.19; 0.10–0.38).
Of 2945 patients given intravenous diuretics, 156 died (30-day mortality rate, 5.3%; 95% CI, 4.5%–6.2%) compared with 34 of 2694 given no diuretics (30-day mortality rate, 1.3%; 95% CI, 0.9%–1.8%). The use of intravenous diuretics was associated with significantly increased risk of 30-day mortality (RR, 4.20; 95% CI, 2.91–6.06). For those patients who met AKIN diagnostic criteria, 125 patients of 1141 given intravenous diuretics died (30-day mortality rate, 11.0%; 95% CI, 9.2%–12.9%) compared with 7 of 145 patients given no diuretics (30-day mortality rate, 4.8%; 95% CI, 2.0%–9.7%). In this group, there was a significantly increased risk of 30-day mortality associated with being given intravenous diuretics (RR, 2.27; 95% CI, 1.08–4.76).
Of those given intravenous diuretics, 175 started RRT (proportion, 0.059; 95% CI, 0.051–0.069) compared with eight given no diuretics (proportion, 0.003; 0.001–0.006). The use of intravenous diuretics was associated with significantly increased risk of receiving RRT (RR, 20.01; 95% CI, 9.87–40.57). For those who met AKIN diagnostic criteria, 171 patients of 1141 given intravenous diuretics received RRT (0.150; 95% CI, 0.130–0.172) compared with five patients of 145 given no diuretics (proportion, 0.035; 95% CI, 0.011–0.079) with a RR of 4.35 (95% CI, 1.82–10.40).
Discussion
Reclassification of AKIN Stage with Assumed Baseline eGFR and Assumed Body Weight
The recommendation to use an assumed SCr as baseline when the actual value is unavailable has not been fully validated (1), with researchers of the only study published to date concluding that, in CKD, the incidence of AKI is overestimated by nearly 20% (8). In this study, an assumed baseline eGFR of 75 ml/min per 1.73 m2 at least doubled the likelihood of an AKI diagnosis, with similar findings for AKIN staging. Our population’s mean baseline eGFR was significantly lower than that used in other studies (1,5,7,14), but would be clinically compatible with the population at risk of both cardiac disease and AKI. We showed that the recommended surrogate eGFR was invalid for our cardiothoracic surgical population and may be invalid for other, similar populations.
A study by Bagshaw et al. (7) only had access to 24-hour UO values. Body weight was also unavailable and thus a 70-kg estimate was used. In our study, use of an assumed body weight was associated with significantly fewer patients meeting diagnostic criteria for UO with a similar finding for the proportion meeting UO criteria for stage 1. Assumptions about body weight seem to be invalid, at least in our population.
Association between Reclassification of AKIN Stage and Outcomes: RRT and 30-Day Mortality
Higher stage was associated with higher 30-day mortality, but an assumed baseline eGFR introduced significant errors in the estimate of 30-day mortality for stages 1 and 2. Higher stage was associated with increased likelihood of initiating RRT during ICU stay. An assumed baseline eGFR erroneously reduced this estimate in stages 1 and 2 as a consequence of more patients being placed at a higher stage.
Calibration of UO Criteria Relative to SCr and Its Association with Diuretic Use
Those staged with SCr criteria have poorer outcomes compared with UO criteria (3,6,17,22), but there remains a lack of studies calibrating UO against SCr criteria (23). Using hourly observations of UO and exact AKIN criteria, we found that the UO criterion was a specific but not sensitive diagnostic test for AKI compared with SCr. Explanations include the stress response to surgery or trauma, which is known to reduce UO without an effect on renal function, per se (24), or AKIN diagnostic criteria for UO being poorly calibrated with SCr criteria.
In our study population, the use of intravenous diuretics placed a significant proportion of patients below the diagnostic threshold for UO criteria compared with SCr. No clinically significant differences in the proportion meeting the diagnostic threshold between UO and SCr criteria were observed for patients who received no diuretics. We believe that this is the first study to examine the association between diuretic use and likelihood of meeting UO criteria.
For patients meeting the diagnostic threshold, we found a significant association between the use of diuretics and both the risk of 30-day mortality and the likelihood of RRT. The limitations of this study mean that confounding by indication cannot be excluded.
Clinical Relevance of the Findings of This Study
First, we have shown that intravenous diuretics significantly reduce the calibration between criteria. Second, our results demonstrate the importance of good data collection, with baseline eGFR and body weight being essential to correct application of the criteria. Finally, even in a data-rich ICU setting with electronic records, almost half of the eligible patients were lost to follow-up because of insufficient observations. This incidental finding calls into question whether the AKIN criteria are a practicable means of predicting AKI in a clinical setting.
Our study is ideally placed to measure the association between common confounders and retrospective staging of AKI; the mechanism of AKI in cardiac surgery is well recognized, the population is relatively homogeneous, and the timing of the insult is definable. Real-time electronic charting created a prospectively collected database of SCr, UO, and drug administration, allowing valid, direct comparison between criteria and association with diuretic use. This study confirmed the fragility of surrogate assumptions and measured the strength of their association with AKIN stage.
Our study has limitations. Patient homogeneity and the study’s single-center nature limit applicability to other populations, and the specific relationship between postcardiac surgery AKI and AKIN criteria may not be transferrable to other mechanisms of AKI. Of those lost to follow-up, most patients (82%) had no recorded postoperative SCr, consistent with them being predominantly straightforward early discharges. This risks biasing estimates of 30-day mortality and the need for RRT. Because premorbid status was not available from electronic records, baseline SCr in some patients (e.g., those hospitalized preoperatively) may have been elevated compared with earlier measurements. Because of the observational design of this study, associations between diuretic use and outcome may have been subject to confounding by indication. Finally, the low incidence of RRT prevented firm conclusions about the relative associations between AKIN stage and intravenous diuretic use and change in SCr for the subgroup of patients receiving RRT.
Our study adds to the evidence (25) that assuming baseline SCr misclassifies severity of AKI; we found that this assumption significantly overestimates the predicted 30-day mortality and requirement for RRT in AKIN stages 1 and 2. We speculate that this assumption will prove invalid in other at-risk populations such as non-ICU groups and patients in the community.
To our knowledge, this is the first study to measure the association between intravenous diuretic use and likelihood of meeting UO criteria. We found that intravenous diuretic use was associated with poorer calibration between criteria and, in addition to assumptions about baseline eGFR, was associated with key outcomes (need for RRT and 30-day mortality). Further research is warranted on the effect of dose and timing of diuretic administration on AKIN staging.
There is a need to assess AKIN criteria in different populations using comprehensive, prospectively collected data. In addition to defining optimal internal calibration within this and similar future diagnostic and staging systems, there is also a need for validation against novel biomarkers of AKI. Further research is needed into the effect of alternative assumptions about baseline SCr and body weight, such as the use of face-value test results and nadir SCr during the first 48 hours of admission.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup: Acute renal failure: Definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8: R204–R212, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute Kidney Injury Network: Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care 11: R31, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz DN, Bolgan I, Perazella MA, Bonello M, de Cal M, Corradi V, Polanco N, Ocampo C, Nalesso F, Piccinni P, Ronco C. North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI) Investigators: North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI): Targeting the problem with the RIFLE criteria. Clin J Am Soc Nephrol 2: 418–425, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Ostermann M, Chang RW: Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med 35: 1837–1843, quiz 1852, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C: An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med 34: 1913–1917, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA: RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Crit Care 10: R73–R82, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagshaw SM, George C, Bellomo R. ANZICS Database Management Committe: A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant 23: 1569–1574, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Bagshaw SM, Uchino S, Cruz D, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators: A comparison of observed versus estimated baseline creatinine for determination of RIFLE class in patients with acute kidney injury. Nephrol Dial Transplant 24: 2739–2744, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Lopes JA, Jorge S, Resina C, Santos C, Pereira A, Neves J, Antunes F, Prata MM: Prognostic utility of RIFLE for acute renal failure in patients with sepsis. Crit Care 11: 408, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopes JA, Fernandes J, Jorge S, Neves J, Antunes F, Prata MM: An assessment of the RIFLE criteria for acute renal failure in critically ill HIV-infected patients. Crit Care 11: 401, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coca SG, Bauling P, Schifftner T, Howard CS, Teitelbaum I, Parikh CR: Contribution of acute kidney injury toward morbidity and mortality in burns: a contemporary analysis. Am J Kidney Dis 49: 517–523, 2007 [DOI] [PubMed] [Google Scholar]
- 12.O’Riordan A, Wong V, McQuillan R, McCormick PA, Hegarty JE, Watson AJ: Acute renal disease, as defined by the RIFLE criteria, post-liver transplantation. Am J Transplant 7: 168–176, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W, Macleod A: Incidence and outcomes in acute kidney injury: A comprehensive population-based study. J Am Soc Nephrol 18: 1292–1298, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Guitard J, Cointault O, Kamar N, Muscari F, Lavayssière L, Suc B, Ribes D, Esposito L, Barange K, Durand D, Rostaing L: Acute renal failure following liver transplantation with induction therapy. Clin Nephrol 65: 103–112, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Costantini TW, Fraga G, Fortlage D, Wynn S, Fraga A, Lee J, Doucet J, Bansal V, Coimbra R: Redefining renal dysfunction in trauma: Implementation of the Acute Kidney Injury Network staging system. J Trauma 67: 283–287, discussion 287–288, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML: Incidence and outcomes of acute kidney injury in intensive care units: A Veterans Administration study. Crit Care Med 37: 2552–2558, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Cruz DN, Ricci Z, Ronco C: Clinical review: RIFLE and AKIN—Time for reappraisal. Crit Care 13: 211, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, Metnitz PG: Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35: 1692–1702, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F. Chronic Kidney Disease Epidemiology Collaboration: Using standardized serum creatinine values in the Modification of Diet in Renal Disease study equation for estimating glomerular filtration rate. Ann Intern Med 145: 247–254, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Cohen J: A coefficient of agreement for nominal scales. Educ Psychol Meas 20: 37–46, 1960 [Google Scholar]
- 21.Hanley JA: Standard error of the kappa statistic. Psychol Bull 102: 315–321, 1987 [Google Scholar]
- 22.Hoste EA, Kellum JA: Acute kidney injury: Epidemiology and diagnostic criteria. Curr Opin Crit Care 12: 531–537, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Macedo E, Malhotra R, Claure-Del Granado R, Fedullo P, Mehta RL: Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol Dial Transplant 26: 509–515, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powell-Tuck J, Gosling P, Lobo DN, Allison SP, Carlson GL, Gore M, Lewington AJ, Pearse RM, Mythen MG: British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients (GIFTASUP), London, Intensive Care Society, 2011 [Google Scholar]
- 25.Siew ED, Matheny ME, Ikizler TA, Lewis JB, Miller RA, Waitman LR, Go AS, Parikh CR, Peterson JF: Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int 77: 536–542, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]