Abstract
Guided by a stress process conceptual model, this study examines social and psychological determinants of complicated grief symptoms focusing on family conflict, intrapsychic strains, and the potential moderating effect of care quality and hospice utilization. Relying on data from 152 spouse and adult child lung cancer caregiver survey respondents, drawn from an ancillary study of the Assessment of Cancer CarE and SatiSfaction (ACCESS) in Wisconsin, hierarchical multiple regression analysis was used to examine determinants of complicated grief. After controlling for contextual factors and time since death, complicated grief symptoms were higher among care-givers with less education, among families with lower prior conflict but higher conflict at the end-of-life, who had family members who had difficulty accepting the illness, and who were caring for patients with greater fear of death. Additionally, hospice utilization moderated the effect of fear of death on complicated grief. Findings suggest that family conflict, intrapsychic strains, and hospice utilization may help to explain the variability found in complicated grief symptoms among bereaved caregivers. Implications for enhancing complicated grief assessment tools and preventative interventions across the continuum of cancer care are highlighted.
INTRODUCTION
Every year approximately 160,000 persons, primarily elders, die from lung cancer; the leading cause of cancer mortality in the United States (American Cancer Society, 2009). Given the rapid deteriorating course of illness, prevalence of uncontrolled symptoms (Griffin, Koch, Nelson, & Cooley, 2007), and stigma associated with lung cancer that is reported by smokers and non-smokers (Chapple, Ziebland, & McPherson, 2004), it is not surprising that these families report high levels of distress during the dying process (Cameron, Franche, Cheung, & Stewart, 2002). Compared to the general population, significant others of lung cancer patients score lower on psychological well-being and experience a decline in family functioning over the course of illness that continues after the death (Persson, Östlund, Wennman-Larsen, Wengström, & Gustavsson, 2008). Little research has been done on how family conflict and experiences during treatment and at the end-of-life may influence the bereavement outcomes of family caregivers.
There is tremendous variability in how individuals adapt following the death of a family member; the vast majority of whom are adequately supported, and do not benefit from intervention (Jordan & Neimeyer, 2003). Given the high risk of suicide and other adverse mental and physical health outcomes (Latham & Prigerson, 2004), understanding what contributes to complicated grief symptomatology is necessary to identify caregivers at risk and to develop relevant interventions. Preliminary evidence suggests that family conflict and intrapsychic strains at the end-of-life that are commonly experienced by family members of persons with lung cancer (Cameron et al., 2002), may contribute to bereavement adjustment difficulties (Kramer, Boelk, & Auer, 2006). The purpose of this article was to examine the predictors of complicated grief symptoms focusing on the role of family conflict, intrapsychic strains, and the potential moderating effect of care quality and hospice utilization.
Theoretical Framework
Stress process theories have been influential in informing an extensive body of research on the impact of family caregiving (Kramer & Vitaliano, 1994), and more recently caregiving and bereavement outcomes (Burton, Haley, Small, Finley, Dillinger-Vasille, & Schonwetter, 2008). Aside from background and contextual considerations, the stress process model is made up of four primary domains: primary stressors, secondary stressors, moderators, and outcomes (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995; Pearlin, Mullan, Semple, & Skaff, 1990).
Primary Stressors
Patient Clinical Care Needs
Primary stressors are the difficult circumstances experienced by family care-givers that stem from the patient’s care needs (Pearlin et al., 1990). Lung cancer patients have a high prevalence of uncontrolled distressing physical symptoms; the most common are pain, shortness of breath, nausea or vomiting, and fatigue (Griffin et al., 2007). These symptoms exacerbate co-occurring psychological symptoms such as patient depression and anxiety (Portenoy, Payne, & Jacobson, 1999), and family distress (McMillan & Small, 2007). Caregivers experience better bereavement adjustment when these symptoms are minimized and quality of life is enhanced (Grande, Farquhar, & Barclay, 2004).
Secondary Stressors
Role Strains
“Secondary stressors are the ways that primary stressors influence and disrupt other areas of the caregiver’s life” (Gustavsson & Dal Santo, 2008, p. 292), and are associated with worse bereavement outcomes (Bernard & Guarnaccia, 2003). Pearlin and colleagues (1990) identified family conflict as a central role strain that may arise in caregiving families. Based on prior research, suggesting that greater bereavement distress among family caregivers is more likely among families in conflict (Kramer et al., 2006) and who have poorer family functioning (Kissane, Bloch, Miach, Smith, Seddon, & Keks, 1997), it is hypothesized that family conflict will be associated with more complicated grief symptoms.
Intrapsychic Strains
Intrapsychic strains are psychological difficulties occurring within the mind that may be influenced by primary stressors. Two intrapsychic strains that may be particularly relevant to lung cancer caregivers are difficulty accepting a highly stigmatized illness and the patient’s fear of death, that is distressing to witness (Chapple et al., 2004). “Acceptance” has been put forth as an essential component of illness adjustment, and a growing body of literature has focused on the correlates of acceptance among patients with acute and chronic heath conditions (Stuifbergen, Becker, Blozis, & Beal, 2008). Grieving may be hampered when one has difficulty accepting illness and related feelings of loss (Prigerson & Maciejewski, 2008). Although an extensive body of literature has developed investigating the predictors and outcomes of death anxiety among elders, the seriously ill and professional caregivers (Neimeyer, Wittkowski, & Moser, 2004), and personal fear of death as associated with bereavement outcomes (Barr & Cacciatore, 2008), little attention has been given to how the patient’s fear of death might influence caregiver bereavement. Compared to other cancer patient populations, lung cancer patients exhibit the highest rates of psychological disorders, and existential distress is elevated closer to death (Lichtenthal, Nilsson, Zhang, Trice, Kissane, & Prigerson, 2009). Emotional distress is higher among caregivers of patients perceived to have death anxiety (Morita, Akechi, Ikenaga, Inoue, Kohara, Matsubara, et al., 2007). It is hypothesized that difficulty accepting the illness and patient fear of death will contribute to complicated grief symptoms.
Moderators
Resources
Resources are the various supports that one has to manage stressful experiences and these are thought to moderate the relationship between stressors and outcomes (Pearlin et al., 1990). Two resources that are particularly salient to the needs of lung cancer patients and families are quality of care and hospice utilization. Better care quality is associated with higher quality of life for care-givers of patients with lung cancer (Ryan, Howell, Jones, & Hardy, 2008), and bereaved family members who are adequately supported by health care providers experience lower levels of psychiatric illness following hospital deaths (Siegel, Hayes, Vanderwerker, Loseth, & Prigerson, 2008). Support received prior to death, is a stronger predictor of bereavement adjustment than support received after death (Bass, Bowman, & Noelker, 1991), and perceptions of care quality are associated with better bereavement adjustment (Grande et al., 2004).
Hospice programs are specifically designed to provide end-of-life care in order to manage distressing symptoms, maximize patient quality of life, address needs of family, and is touted as the optimal care model for patients with advanced lung cancer (Griffin, Koch, Ackerman, & Cole, 2003). Family members report greater satisfaction with hospice care than care in other settings (Yancey, Greger, & Coburn, 1990), and improved family well-being and functioning (Godkin, Krant, & Doster, 1983–84). Findings regarding hospice utilization and the influence on bereavement outcomes are mixed. Some find utilization to have a positive influence (Christakis & Iwashyna, 2003; Steele, 1990), but others report no relationship (Grande et al., 2004; Yancey, Greger, & Coburn, 1990). According to the stress process model, we hypothesize that the impact of family conflict and intrapsychic strains on complicated grief symptoms will be intensified when resources are low and diminished when they are plentiful.
Outcomes
Complicated Grief Symptoms
Salient outcomes of the stress process include psychological well-being indicators related to the individual’s “ability to sustain themselves in their social roles” (Pearlin et al., 1990, p. 590). Complicated grief symptoms interfere with daily life and the fulfillment of social roles (Prigerson, Maciejewski, Reynolds, Bierhals, Newsom, Fasiczka, et al., 1995) and are experienced by 10%–20% of the population (Prigerson & Jacobs, 2001). Although there are important features that distinguish it from bereavement related depression, anxiety and Posttraumatic Stress Disorder (PTSD) (Zhang, El-Jawahri, & Prigerson, 2006), one study reports as many as 75% of complicated grievers also meet criteria for PTSD (Tolstikova, Fleming, & Chartier, 2005). Given that complicated grievers experience intense, persistent emotional and functional impairment (Schulz, Boerner, Shear, Zhang, & Gitlin, 2006), identifying the contributing factors of this particular outcome is an important goal of bereavement research.
Background and Context—Control Variables
Pearlin et al. (1990, p. 585) propose that the effects of “ascribed statuses, such as age, gender, ethnicity, along with education … and economic attainments are expected to be threaded throughout the entire stress process,” influence the primary and secondary stressors individuals are exposed to, the resources they have access to, and the outcomes they experience. As such it is important to control for these and other contextual variables. Other contextual variables include advanced care planning and the family context. Among several forms of advanced care planning, discussions with significant others is considered an essential component of the planning process (Hammes & Rooney, 1998). Stress and post-death depression and anxiety among relatives may be reduced when caregivers know the patient’s preferences for care (Detering, Hancock, Reade, & Silvester, 2010; Tilden, Tolle, Garland, & Nelson, 1995), and evidence suggests that “end-of-life discussions may have cascading benefits for patients and their caregivers” including better caregiver bereavement adjustment (Wright, Zhang, Ray, Mack, Trice, Balboni, et al., 2008, p. 1670). Although little attention has been given to the family context, higher bereavement risk was found among those with young children at home (Beckwith, Beckwith, Gray, & Micsko, 1990) and a history of conflict was associated with guilt following death which negatively effects bereavement adaptation (Mullan, 1992). In addition, a history of conflict is a strong predictor of family conflict at the end-of-life (Kramer, Kavanaugh, Trentham-Dietz, Walsh, & Yonker, 2009), and needs to be taken into consideration in order to understand how conflict at the end-of-life might influence bereavement outcomes.
This study will identify and control for the background and contextual variables that are significantly associated with complicated grief among care-givers of deceased lung cancer patients and will test the following two hypotheses, which were generated from this review of the literature and the stress process model.
Hypothesis 1: After controlling for time since death, history of family conflict, and other contextual and primary stressor variables, secondary stressors (i.e., family conflict at the end-of-life, family member difficulty accepting the illness, and patient fear of death) will significantly predict complicated grief symptoms.
Hypothesis 2: The quality of care provided to the patient and family and hospice utilization will moderate the effect of secondary stressors on complicated grief symptoms.
METHODS
Data Sources
The results reported here are drawn from an ancillary mail survey of family members of persons who died with lung cancer, drawn from the larger Assessment of Cancer CarE and SatiSfaction (ACCESS) study conducted in the state of Wisconsin. Sampling and survey methods from the ACCESS and ancillary lung cancer family study are described in detail by Trentham-Dietz and Walsh (2008) and Kramer et al. (2009) respectively. In brief, of 358 primary family caregivers of persons who died with lung cancer, who were identified in a statewide registry and who had contact information available, 205 (57%) agreed to receive the study questionnaire, and 169 returned surveys (82% of those who received the survey; 47% of total contacted). Consistent with the national profile of informal end-of-life caregivers (Wolff, Dy, Frick, & Kasper, 2007), the majority, 158 (93%) of respondents were spouses (n = 141) or adult children (n = 17). The analytic sample is confined to 152 of these respondents. These included 148 who answered all of the complicated grief items, and four others who had completed 50% or more of the items. In these cases we used the person mean substitution method (Downey & King, 1998) found to be the optimal technique for imputing missing data when half of the items are present (Hawthorne & Elliott, 2005). The time between death and completion of the surveys averaged 19 months (SD = 7.37), and ranged from .9 to 34 months.
Measures
Dependent Variable—Complicated Grief
In 1995 the Inventory of Complicated Grief (ICG) was introduced as the first measure to assess maladaptive grief symptoms (Prigerson et al., 1995), and has since been well validated and widely used. The ICG-revised (ICG-R) is a more contemporary version of the ICG further refined by an expert consensus panel (Prigerson & Jacobs, 2001). Using 5-point scales to represent increasing levels of symptom severity respondents rated nine items addressing symptoms of yearning and longing for the deceased, trouble accepting the death, difficulty trusting people, bitterness over the death, inability to move forward, sense of emotional numbness, sense of edginess, feeling the future holds no prospect for fulfillment without the deceased, and feeling life is empty or meaningless without the deceased. This measure is highly correlated with clinical assessments of complicated grief and distinguishes complicated grief from typical grief symptoms in terms of the prediction of morbidity, persistence and intensity (Prigerson & Maciejewski, 2005). A mean score was calculated. Cronbach’s α was .90.
Primary Stressors
Two measures of patient clinical care needs were assessed. An index of four common physical symptoms associated with lung cancer was assessed by asking: “Did your family member have: a) pain; b) shortness of breath; c) nausea or vomiting; or d) severe tiredness or fatigue during or after any of his/her cancer treatments?” Cronbach’s α was .66. A psychological symptoms index was assessed by asking “Did your family member experience: a) loss of hope or depression; and/or b) anxiety during or after any of his/her cancer treatments?” Cronbach’s α was .57.
Secondary Stressors
Role strains
A four-item Family Conflict at the End-of Life (FC-EOL) scale was developed for this study, based on findings from a prior qualitative study (Kramer et al., 2006), a literature review, and prior clinical experience. Respondents were asked to use a 5-point scale (1 = not at all to 5 = very much) to answer the following four questions “As you think about the decisions that your family member and the rest of the family faced near the end-of-life, how much did any family members: Disagree or argue with one another? Feel resentment toward one another? Feel anger toward one another? Insult or yell at one another?” A mean score for family conflict was calculated. Cronbach’s α was .93; item to total correlations ranged from .72 to .88.
Intrapsychic strains
Family difficulty accepting the illness was assessed with response to the question “How much did any family members find it hard to accept the illness?” using a 5-point continuum to indicate the degree of difficulty (0 = not at all to 4 = very much). Patient fear of death was measured by a 5-point rating of agreement (1 = strongly disagree to 5 = strongly agree) with the statement “After his/her lung cancer diagnosis, my family member was afraid to die.”
Moderators—Resources
Patient quality of care was assessed using nine items adapted from the Toolkit of Instruments to Measure End-of-Life Care (Teno, 2004). Using a 5-point response set (0 = not at all to 5 = very much), respondents rated the extent to which the patient was treated with kindness and respect, and their physical, psychological, spiritual, and informational needs were adequately addressed. Cronbach’s α was .86. Family quality of care was assessed using five items adapted from the Toolkit of Instruments (Teno, 2004) to rate family care quality. Respondents rated the extent to which the treatment staff included them in decisions, were sensitive to their feelings, paid attention to their wishes for care, and were helpful in explaining the patient’s condition, using a 5-point response set (0 = not at all to 5 = very much). Cronbach’s α was .84. Hospice utilization was determined with the question “Was hospice involved in the medical care of your family member?” (0 = no; 1 = yes).
Background and Context
Demographic characteristics included sociodemographic variables such as age (continuous variable that was dichotomized; 0 = under 65; 1 = 65 or over), gender (0 = male; 1 = female), race (0 = Non-Hispanic White; 1 = Black), income (four income categories included less than $12,000, $15,000–$29,999, $30,000–$49,999, and $50,000+), education (two categories that include high school or less, and some college or advanced degree), and relationship to the deceased (0 = adult child; 1 = spouse). Care preferences specified was ascertained by asking: “Did your family member have specific wishes or plans about the types of medical treatment he/she wanted while dying?” (0 = no; 1 = yes). Regarding family context we assessed presence of children in the home (0 = no; 1 = yes), and history of family conflict prior to illness with a two-item scale developed by (first author). Respondents were asked “Prior to [the decedent’s] illness, how much did any of your family members: ‘have serious arguments with one another;’ and ‘insult or yell at one another’?” Response categories range from 0 = not at all to 4 = very much. Cronbach’s α was .94.
Analytic Plan
Details regarding strategies for handling missing data are reported elsewhere (Kramer et al., 2009). The analysis has four parts. First, we present descriptive statistics and the results of the two-tailed t tests and F tests comparing the means for complicated grief on all values of the categorical background and contextual variables. Second, we present the descriptives and bivariate correlations for the analytic variables. Third, to test the first hypothesis, we used hierarchical multiple regression analysis to control for the time since death, contextual variables, and primary stressors. Given the limited sample size and the number of independent variables, aside from time since death and history of family conflict, only the variables that were significantly correlated with complicated grief were chosen for the analysis to allow for a more parsimonious model. Omitted contextual variables were analyzed as covariates in an exploratory regression analysis, and their presence did not alter appreciably the relationships between conflict, intra-psychic strains, and complicated grief. Finally, to test hypothesis 2 and examine the extent to which resources would have a stress-buffering effect, interaction terms were computed by multiplying each of the selected secondary stressor variables by each of the three resources variables, which were centered before forming the multiplicative terms (Jaccard, Turrisi, & Wan, 1990). Separate regression analyses were run to identify any significant interactions. One interaction was a significant predictor of complicated grief and as such, the regression analysis included two additional blocks to control for resources and this interaction effect respectively. The more conservative two-tailed tests of significance were used to interpret the results.
RESULTS
Sample Characteristics and Contextual Correlates of Complicated Grief
Sample characteristics and complicated grief means for categorical background and contextual variables are described in Table 1. The majority of respondents were female, Non-Hispanic White, spouses, with less than a college education. The sample fell fairly evenly into the under and over age 65 groupings. Consistent with the national profile of end-of-life caregivers, the mean age was 63 for family members (Wolff et al., 2007), and 66 for patients (SD = 8.82; range = 43–80), indicating that this was primarily an older sample. Less than half of the patients had expressed specific wishes for end-of-life care (39%) and the majority (68%) received hospice care. Complicated grief symptom were greater among those who were younger (t = 2.96, p ≤ .01), less educated (t = 2.65, p ≤ .01), and who had more children in the home (t = 2.49, p ≤ .01). No differences were found by gender, race, income, or relationship, and grief was higher among those caring for patients who had expressed their end-of-life care wishes (t = 2.52, p ≤ .01).
Table 1.
Sample Characteristics and Complicated Grief Means for Categorical Background and Contextual Variables (N = 152)
| N | % | Complicated grief a |
||
|---|---|---|---|---|
| Mean | SD | |||
| Age | ||||
| Less than 65(b=1) | 74 | (49.0) | 2.59 | (.97)** |
| 65+(b=2) | 78 | (51.0) | 2.19 | (.69) |
| Gender | ||||
| Male | 31 | (20.4) | 2.35 | (.84) |
| Female | 121 | (79.6) | 2.39 | (.87) |
| Race | ||||
| Non-Hispanic White(b=2) | 148 | (97.4) | 2.37 | (.86) |
| Black | 4 | (2.6) | 2.83 | (.71) |
| Income | ||||
| Less than $15,000 | 17 | (11.2) | 2.23 | (.81) |
| $15,000 to $29,999 | 32 | (21.1) | 2.28 | (.81) |
| $30,000 to $49,999 | 56 | (36.8) | 2.45 | (.88) |
| $50,000+ | 36 | (23.7) | 2.50 | (.92) |
| Missing | 11 | (7.2) | ||
| Education | ||||
| High school grad or less(b=3) | 94 | (61.8) | 2.53 | (.93)** |
| Some college or advanced degree | 58 | (38.2) | 2.15 | (.68) |
| Relationship to patient | ||||
| Spouse | 136 | (89.5) | 2.40 | (.85) |
| Adult child | 16 | (10.5) | 2.22 | (.98) |
| Expressed end-of-life care wishes | ||||
| Care preferences specified | ||||
| No(b=4) | 95 | (61.3) | 2.24 | (.44) |
| Yes | 60 | (38.7) | 2.60 | (1.01)** |
| Family context | ||||
| Presence of children in home | ||||
| No(b=4) | 142 | (93.4) | 2.31 | (.82) |
| Yes | 10 | (6.6) | 3.19 | (.95)** |
p-Values reported for F test or t tests for significant difference in complicated grief.
Refers to the number of missing respondents who were included in this category.
p ≤ .01.
Table 2 presents the means and standard deviations of the analytic variables as well as the zero-order correlations among them. Complicated grief symptoms were not correlated with a history of family conflict, but were significantly correlated with physical (r = .28, p ≤ .001) and psychological symptoms of the patient (r = .34, p ≤ .001).
Table 2.
Correlations and Descriptives for Analytic Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Complicated grief | — | |||||||||||||
| 2 Caregiver age | −.23** | — | ||||||||||||
| 3 Caregiver education | −.21** | −.02 | — | |||||||||||
| 4 Care preferences specified | .20** | −.18* | −.02 | — | ||||||||||
| 5 Presence of children in home | .25** | −.22** | .12 | .06 | — | |||||||||
| 6 History of family conflict | .10 | −.13 | .01 | .09 | .22** | — | ||||||||
| 7 Patient physical symptoms | .28*** | −.26*** | .16* | .16* | .26*** | .26*** | — | |||||||
| 8 Patient psych symptoms | .34*** | −.38*** | .10 | .14 | .24** | .32*** | .51*** | — | ||||||
| 9 Family conflict at end-of-life | .27*** | −.19* | .08 | .21** | .23** | .62*** | .23** | .31*** | — | |||||
| 10 Difficulty accepting illness | .42*** | −.08 | −.09 | .03 | .21** | .15 | .16* | .14† | .20 | — | ||||
| 11 Patient fear of death | .17* | −.07 | −.02 | −.12 | .02 | −.10 | .15† | .30*** | .01 | .02 | — | |||
| 12 Patient quality of care | −.30*** | .10 | −.06 | −.08 | −.21** | −.16* | −.34*** | −.35*** | −.19* | −.04 | −.10 | — | ||
| 13 Family quality of care | −.25** | .03 | −.08 | −.09 | −.15† | −.17* | −.28*** | −.20* | −.10 | −.07 | −.05 | .72*** | — | |
| 14 Hospice utilization | .08 | −.12 | −.14† | −.16* | .02 | .01 | .07 | .11 | .03 | −.02 | −.06 | .00 | −.02 | — |
| M | 2.39 | .51 | .38 | .39 | .07 | .36 | 2.1 | .86 | .38 | 2.12 | 2.72 | 28.86 | 15.22 | .67 |
| SD | .86 | .50 | .49 | .49 | .25 | .71 | 1.35 | .81 | .76 | 1.35 | 1.17 | 7.06 | 5.00 | .47 |
| Range | 1–4.6 | 0–1 | 0–1 | 0–1 | 0–1 | 0–4 | 0–4 | 0–2 | 0–4 | 0–4 | 1–5 | 0–36 | 0–20 | 0–1 |
p ≤ .10;
p ≤ .05;
p ≤ .01;
p ≤ .001.
Secondary Stressors and Complicated Grief: Hypothesis 1
We hypothesized that after controlling for time since death and a history of family conflict, and other contextual and primary stressor variables, that higher levels of family conflict at the end-of-life, family member difficulty accepting the illness and patient fear of death will contribute to complicated grief symptoms. Table 3 presents the results of the regression analysis for complicated grief. As shown in Step 3, after controlling for contextual and primary stressor variables, secondary stressors uniquely explained 15% of the variance in complicated grief symptoms, the most important two being family conflict at the end-of-life (b = .23, p ≤ .01) and family member difficulty accepting the illness (b = .34, p ≤ .001).
Table 3.
Hierarchical Regression Analysis for Complicated Grief Symptoms
| Variables | Betas
|
||||
|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | |
| Background and Context | |||||
| Time since death | .01 | .03 | −.03 | −.03 | −.03 |
| Caregiver age | −.14† | −.05 | −.04 | −.06 | −.04 |
| Caregiver education | −.24** | −.28*** | −.25*** | −.25*** | −.25*** |
| Care preferences specified | .16* | .13† | .12† | .12† | .13† |
| Presence of children in home | .23* | .19* | .11† | .10 | .10 |
| History of family conflict | .01 | −.08 | −.26** | −.24** | −.21* |
| Primary Stressors | |||||
| Patient physical symptoms | .16† | .13 | .08 | .09 | |
| Patient psychological symptoms | .22* | .16† | .12 | .15† | |
| Secondary Stressors | |||||
| Family conflict at end-of-life | .23** | .22** | .21* | ||
| Family member difficulty accepting illness | .33*** | .33*** | .33*** | ||
| Patient fear of death | .10 | .10 | .15* | ||
| Resources | |||||
| Patient quality of care | −.12 | −.11 | |||
| Family quality of care | −.10 | −.08 | |||
| Hospice utilization | .01 | .02 | |||
| Interaction-Moderating Process | |||||
| Patient fear of death × hospice utilization | −.16* | ||||
| Total R2 | .17 | .25 | .40 | .43 | .45 |
| R2 change | .17 | .08 | .15 | .03 | .02 |
| F for R2 change | 5.03*** | 7.20** | 10.75*** | 2.58† | 4.80* |
p ≤ .10;
p ≤ .05;
p ≤ .01;
p ≤ .001.
Moderators of Complicated Grief Symptoms: Hypothesis 2
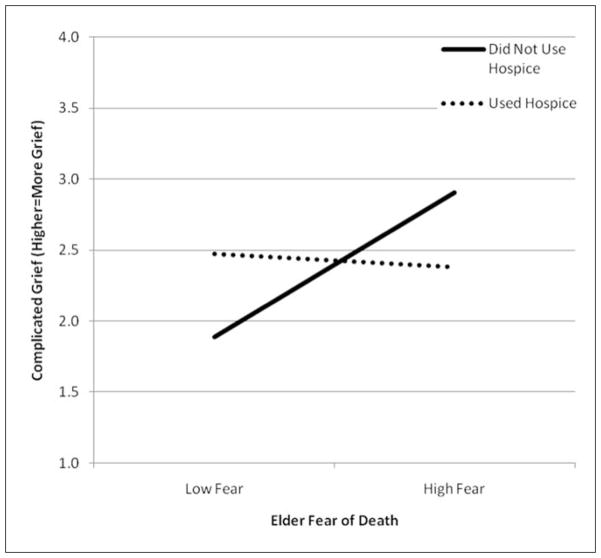
We hypothesized that the quality of care provided to the patient and family and hospice utilization will buffer the effect of secondary stressors on complicated grief symptoms. As shown in the final model of Table 3, net of the other predictors, an interaction between patient fear of death and hospice care utilization significantly predicted complicated grief symptoms (b = −.16, p ≤ .05). We graphed this interaction using the estimated regression coefficients for combinations of low and high patient fear of death by hospice or no hospice status; all other variables evaluated at their mean (see Figure 1 for a portrayal of this interaction effect). Patient fear of death contributed to complicated grief when hospice care was not utilized, and supports the stress-buffering hypothesis.
Figure 1.
Interaction between patient fear of death and hospice utilization on complicated grief.
The regression equation explained 45% of the total variance in complicated grief symptoms. In the final model, in addition to the moderator variable (i.e., patient fear of death by hospice utilization), significantly more complicated grief symptoms were found among caregivers without college education (b = −.25, p ≤ .001), who were caring for patients who had specified their end-of-life care preferences (b = .13, p ≤ .10), and had more psychological symptoms (b = .15, p ≤ .10), and fear of dying (b = .15, p ≤ .05), who had family members who expressed difficulty accepting the illness (b = .33, p ≤ .001), and who had low levels of a history of family conflict (b = −.21, p ≤ .05), but higher levels of family conflict near the end-of-life (b = .21, p ≤ .05).
DISCUSSION
The most compelling findings from this study concern the importance of secondary stressors in predicting complicated grief symptoms and hospice utilization in moderating the stress process. Secondary stressors uniquely explained 15% of the variance in complicated grief symptoms and both family conflict and the two intrapsychic strains were significant predictors in the final model. Kissane and colleagues (Kissane & Bloch, 2002; Kissane, McKenzie, Bloch, Moskowitz, McKenzie, & O’Neill, 2006) have well documented a relationship between “maladaptive family functioning” and bereavement outcomes. Our results suggest that although not very common, as evidenced by the strong correlation between prior conflict and conflict at the end-of-life (i.e., r = .62), that families with lower levels of prior conflict and higher levels of conflict associated with difficult decisions at the end-of-life may be at most risk. Developing and testing interventions to meet the needs of families at risk of experiencing conflict at the end-of-life (see Kramer et al., 2009), to better support families during critical junctures in decision making, and in the aftermath of unresolved conflict across the continuum of cancer care are important goals for future research and practice.
National guidelines and preferred practices for palliative care have been established that emphasize the importance of assessing and treating social and psychological responses to illness that often contribute to patient and family suffering (Hultman, Keene-Reder, & Dahlin, 2008). Our findings suggest that assessment and treatment of these needs should not be relegated to palliative care only. Family difficulty accepting illness and patient fear of death both represent psychological needs that may be present very soon after the diagnosis. Oncologists, family physicians, and other interdisciplinary care providers need to be mindful of the intrapsychic strains that are stimulated by a lung cancer diagnosis and consider psychotherapeutic interventions or referrals to address them. Cognitive-existential group therapy has been used successfully to address death anxiety among cancer patients (Kissane et al., 1997). Similar models might be employed to support lung cancer patients and family members to address fear of death and difficulty accepting the illness.
Although no direct bivariate relationship was found between hospice utilization and complicated grief, hospice enrollment did serve to buffer the effect of patient fear of death and the outcome. The decedent’s fear of death, as reported by the survivor, did not lead to complicated grief when hospice was used, but did have a negative effect on bereavement outcomes for those not enrolled. Hospice professionals are found to have less death anxiety and more death related experience than other health care professionals (Carr & Merriman, 1995–1996), and may have greater competency to address fear of death among patients. Of course this is an empirical question, but may help to explain our findings. Hospice care is recommended as the optimal care model of patients with advanced lung cancer (Griffin et al., 2003), but is typically underutilized by lung cancer patients (McCarthy, Burns, Davis, & Phillips, 2003). In addition to encouraging efforts to promote timely hospice referral, other initiatives to increase the knowledge, skills, and competencies of oncology and other health care providers for routinely assessing and treating patient fear of death may help prevent complicated bereavement.
Not surprisingly, bivariate analysis revealed strong relationships between lower quality of care of the patient and family and higher levels of complicated grief. Given the documented concerns regarding care quality for lung cancer patients and their families (Krishnasamy, Wilkie, & Haviland, 2001), this is an important finding. The relationship between care quality and complicated grief was no longer statistically significant in the multivariate model when contextual and stressor variables were included and care quality did not moderate the effect of stressors on grief. Routine care may not sufficiently address the distinctive problems associated with secondary stressors. More intensive and targeted interventions to meet these distinctive needs may be required.
Several limitations should be acknowledged when interpreting these results. The cross-sectional design and reliance on retrospective reports of care and conflict at the end-of-life are important limitations. Current affective states may affect retrospective appraisals of subjective measures. Prospective studies are necessary to evaluate the direction of relationships and capture experiences as they occur, but do present ethical and methodological challenges of their own (Casarett, Knebel, & Helmers, 2003). Although the interaction between hospice utilization and patient fear of death was interpretable, it may be a chance finding given the multiple exploratory tests used to evaluate possible interaction effects. Other studies are needed to test for replication. Some of our measures are limited such as the clinical care needs of the patient that measured the number of symptoms rather than symptom severity that may underestimate the relationship between symptoms and complicated grief. In addition, we did not collect any data on the end-of-life care treatment preferences that were expressed by patients or the extent to which they were carried out, which seriously limits our ability to interpret the unanticipated positive correlation between care preferences specified and grief symptoms. It is possible that the patient’s expressed end-of-life care wishes were not fulfilled or were a source of disagreement among family members. Finally, the nonrepresentative nature of the sample, seriously limits the generalizability of study findings. Although the ACCESS study sought a representative statewide sample and over sampled by race, less than half of the eligible families completed the survey, and the sample was primarily older White female spouses. In addition, the hospice utilization rate of our sample is higher than that of lung cancer Medicare beneficiaries (i.e., 68% compared to 27%; McCarthy et al., 2003), and the overall rates of family conflict were fairly modest (Kramer et al., 2009).
Despite its limitations, this study was guided by a theoretical framework to provide a more comprehensive understanding of the complex determinants of the bereavement process with attention to domains not previously considered in research. Results provide substantial support documenting a relationship between family conflict, intrapsychic strains and complicated grief, and a moderating influence of hospice utilization. Risk assessment tools used to identify persons at risk for complicated grief (Melliar-Smith, 2002) could be expanded to include assessment of patient symptoms, intrapsychic strains, prior and end-of-life conflict, and caregiver education. Future research to replicate these findings and to illuminate understanding of the primary and secondary stressors and resources that might influence the bereavement process, as well as development and testing of interventions to address these are warranted.
Acknowledgments
The authors gratefully acknowledge the bereaved family members for their participation in this study, and the contributions of our colleagues who participated in the design of the ACCESS survey.
Footnotes
This study used data from the Assessment of Cancer CarE and SatiSfaction (ACCESS), survey, a project of the Wisconsin Comprehensive Cancer Control Program. Funding for the WI CCC Program is provided by The Centers for Disease Control & Prevention, The Wisconsin Department of Health Services, The Wisconsin Partnership Fund for a Healthy Future, and the UW-Paul P. Carbone Comprehensive Cancer Center. This article was prepared with support from the National Institute of Mental Health (T32 MH65185 to Jan. Greenberg).
References
- American Cancer Society. Cancer facts and figures 2009. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. New York: Academic Press; 1995. [Google Scholar]
- Barr P, Cacciatore JE. Personal fear of death and grief in bereaved mothers. Death Studies. 2008;32:445–460. doi: 10.1080/07481180801974752. [DOI] [PubMed] [Google Scholar]
- Bass DM, Bowman K, Noelker LS. The influence of caregiving and bereavement support on adjusting to an older relative’s death. The Gerontologist. 1991;31:32–42. doi: 10.1093/geront/31.1.32. [DOI] [PubMed] [Google Scholar]
- Beckwith BE, Beckwith SK, Gray TL, Micsko MM. Identification of spouses at high risk during bereavement: A preliminary assessment of Parkes and Weiss’ Risk Index. Hospice Journal. 1990;6(3):35–46. doi: 10.1080/0742-969x.1990.11882676. [DOI] [PubMed] [Google Scholar]
- Bernard LL, Guarnaccia CA. Two models of caregiver strain and bereavement adjustment: A comparison of husband and daughter caregivers of breast cancer hospice patients. The Gerontologist. 2003;43:808–816. doi: 10.1093/geront/43.6.808. [DOI] [PubMed] [Google Scholar]
- Burton AM, Haley WE, Small BJ, Finley MR, Dillinger-Vasille M, Schonwetter R. Predictors of well-being in bereaved former hospice care-givers: The role of caregiving stressors, appraisals, and social resources. Palliative and Supportive Care. 2008;6:149–158. doi: 10.1017/S1478951508000230. [DOI] [PubMed] [Google Scholar]
- Cameron J, Franche R, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- Carr M, Merriman MP. Comparison of death attitudes among hospice workers and health care professionals in other settings. Omega. 1995–1996;32:287–301. [Google Scholar]
- Casarett D, Knebel A, Helmers K. Ethical challenges of palliative care research. Journal of Pain and Symptom Management. 2003;25(4):S3–S5. doi: 10.1016/s0885-3924(03)00058-7. [DOI] [PubMed] [Google Scholar]
- Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. British Medical Journal. 2004;328(7454):1470–1474. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ. The health impact of health care on families: A matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Social Science & Medicine. 2003;57:465–475. doi: 10.1016/s0277-9536(02)00370-2. [DOI] [PubMed] [Google Scholar]
- Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: A randomised controlled trial. British Medical Journal. 2010;340 doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey RG, King C. Missing data in Likert ratings: A comparison of replacement methods. Journal of General Psychology. 1998;125:175–191. doi: 10.1080/00221309809595542. [DOI] [PubMed] [Google Scholar]
- Godkin MA, Krant MJ, Doster NJ. The impact of hospice care on families. International Journal of Psychiatry in Medicine. 1983–84;13(2):153–165. doi: 10.2190/g526-4w46-vp27-tjb6. [DOI] [PubMed] [Google Scholar]
- Grande GE, Farquhar MC, Barclay SIG. Caregiver bereavement outcome: Relationship with hospice at home, satisfaction with care, and home death. Journal of Palliative Care. 2004;20(2):69–77. [PubMed] [Google Scholar]
- Griffin JP, Koch KA, Ackerman TF, Cole FH., Jr End-of-life care in patients with lung cancer. CHEST: Supplement. 2003;123:312S–331S. doi: 10.1378/chest.123.1_suppl.312s. [DOI] [PubMed] [Google Scholar]
- Griffin JP, Koch KA, Nelson JE, Cooley ME. Palliative care consultation, quality-of-life measurements, and bereavement for end-of-life care in patients with lung cancer. CHEST: Supplement. 2007;132:404S–422S. doi: 10.1378/chest.07-1392. [DOI] [PubMed] [Google Scholar]
- Gustavson K, Dal Santo TS. Caregiver service use: A complex story of care at the end of life. Journal of Social Work in End-of-Life & Palliative Care. 2008;4:286–311. [Google Scholar]
- Hammes BJ, Rooney BL. Death and end-of-life planning in one midwestern community. Archives of Internal Medicine. 1998;158:383–390. doi: 10.1001/archinte.158.4.383. [DOI] [PubMed] [Google Scholar]
- Hawthorne G, Elliott P. Imputing cross-sectional missing data: Comparison of common techniques. Australian and New Zealand Journal of Psychiatry. 2005;39:583–590. doi: 10.1080/j.1440-1614.2005.01630.x. [DOI] [PubMed] [Google Scholar]
- Hultman T, Keene Reder EA, Dahlin CM. Improving psychological and psychiatric aspects of palliative care: The national consensus project and the national quality forum preferred practices for palliative and hospice care. Omega. 2008;57:323–339. doi: 10.2190/OM.57.4.a. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Turrisi R, Wan CK. Interaction effects in multiple regression. Newbury Park, CA: Sage; 1990. [DOI] [PubMed] [Google Scholar]
- Jordan JR, Neimeyer RA. Does grief counseling work? Death Studies. 2003;27:765–786. doi: 10.1080/713842360. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Bloch S. Family focused grief therapy: A model of family-centered care during palliative care and bereavement. Philadelphia, PA: Open University Press; 2002. [Google Scholar]
- Kissane DW, Bloch S, Miach P, Smith GC, Seddon A, Keks N. Cognitive-existential group therapy for patients with primary breast cancer—Techniques and themes. Psycho-Oncology. 1997;6:25–33. doi: 10.1002/(SICI)1099-1611(199703)6:1<25::AID-PON240>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Kissane DW, McKenzie M, Bloch S, Moskowitz C, McKenzie DP, O’Neill J. Family focused grief therapy: A randomized, controlled trial in palliative care and bereavement. American Journal of Psychiatry. 2006;163(7):1208–1218. doi: 10.1176/ajp.2006.163.7.1208. [DOI] [PubMed] [Google Scholar]
- Kramer BJ, Boelk A, Auer C. Family conflict at the end-of-life: Lessons learned in a model program for vulnerable older adults. Journal of Palliative Medicine. 2006;9:791–801. doi: 10.1089/jpm.2006.9.791. [DOI] [PubMed] [Google Scholar]
- Kramer BJ, Kavanaugh M, Trentham-Dietz A, Walsh M, Yonker JA. Predictors of family conflict at the end of life: The experience of spouses and adult children of persons with lung cancer. The Gerontologist. 2009 doi: 10.1093/geront/gnp 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer BJ, Vitaliano PP. Coping: A review of the theoretical frameworks and the measures used among caregivers of individuals with dementia. Journal of Gerontological Social Work. 1994;23(1/2):151–174. [Google Scholar]
- Krishnasamy M, Wilkie E, Haviland J. Lung cancer health care needs assessment: Patients’ and informal carers’ responses to a national mail questionnaire survey. Palliative Medicine. 2001;15:213–227. doi: 10.1191/026921601678576202. [DOI] [PubMed] [Google Scholar]
- Latham AE, Prigerson HG. Suicidality and bereavement: Complicated grief as psychiatric disorder presenting greatest risk for suicidality. Suicide and Life-Threatening Behavior. 2004;34:350–362. doi: 10.1521/suli.34.4.350.53737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenthal WG, Nilsson M, Zhang B, Trice ED, Kissane DW, Prigerson HG. Do rates of mental disorders and existential distress among advanced stage cancer patients increase as death approaches. Psycho-Oncology. 2009;18:50–61. doi: 10.1002/pon.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy EP, Burns RB, Davis RB, Phillips RS. Barriers to hospice care among older patients dying with lung and colorectal cancer. Journal of Clinical Oncology. 2003;21:728–735. doi: 10.1200/JCO.2003.06.142. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ. Using the COPE intervention for family caregivers to improve symptoms of hospice homecare patients: A clinical trial. Oncology Nursing Forum. 2007;34:313–321. doi: 10.1188/07.ONF.313-321. [DOI] [PubMed] [Google Scholar]
- Melliar-Smith C. The risk assessment of bereavement in a palliative care setting. International Journal of Palliative Nursing. 2002;8:281–287. doi: 10.12968/ijpn.2002.8.6.10498. [DOI] [PubMed] [Google Scholar]
- Morita T, Akechi T, Ikenaga M, Inoue S, Kohara H, Matsubara T, et al. Terminal decline: Recommendations from bereaved families’ experiences. Journal of Pain and Symptom Management. 2007;34:579–589. doi: 10.1016/j.jpainsymman.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Mullan JT. The bereaved caregiver: A prospective study of changes in well-being. The Gerontologist. 1992;32:673–683. doi: 10.1093/geront/32.5.673. [DOI] [PubMed] [Google Scholar]
- Neimeyer RA, Wittkowski J, Moser RP. Psychological research on death attitudes: An overview and evaluation. Death Studies. 2004;28:309–340. doi: 10.1080/07481180490432324. [DOI] [PubMed] [Google Scholar]
- Pearlin L, Mullan J, Semple M, Skaff M. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Persson C, Östlund U, Wennman-Larsen A, Wengström Y, Gustavsson P. Health-related quality of life in significant others of patients dying from lung cancer. Palliative Medicine. 2008;22:239–247. doi: 10.1177/0269216307085339. [DOI] [PubMed] [Google Scholar]
- Portenoy R, Payne D, Jacobson P. Breakthrough pain: Characteristics and impacts in patients with cancer pain. Pain. 1999;81:129–134. doi: 10.1016/s0304-3959(99)00006-8. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Jacobs SC. Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In: Stroebe MS, Hansson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping and care. Washington, DC: American Psychological Association; 2001. pp. 613–637. [Google Scholar]
- Prigerson HG, Maciejewski PK. A call for sound empirical testing and evaluation of criteria for complicated grief proposed for DSM-V. Omega. 2005;52:9. [Google Scholar]
- Prigerson HG, Maciejewski PK. Grief and acceptance as opposite sides of the same coin: Setting a research agenda to study peaceful acceptance of loss. British Journal of Psychiatry. 2008;193:435–437. doi: 10.1192/bjp.bp.108.053157. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Maciejewski PK, Reynolds CF, Bierhals AJ, Newsom JT, Fasiczka A, et al. Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research. 1995;59:65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- Ryan RP, Howell V, Jones J, Hardy EJ. Lung cancer, caring for the caregivers. A qualitative study of providing pro-active social support targeted to the carers of patients with lung cancer. Palliative Medicine. 2008;22:233–238. doi: 10.1177/0269216307087145. [DOI] [PubMed] [Google Scholar]
- Schulz R, Boerner K, Shear K, Zhang S, Gitlin LN. Predictors of complicated grief among dementia caregivers: A prospective study of bereavement. American Journal of Geriatric Psychiatry. 2006;14:650–656. doi: 10.1097/01.JGP.0000203178.44894.db. [DOI] [PubMed] [Google Scholar]
- Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin in patients who die in the intensive care unit. Critical Care Medicine. 2008;36:1722–1728. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- Steele LL. The death surround: Factors influencing the grief experience of survivors. Oncology Nursing Forum. 1990;17:235–241. [PubMed] [Google Scholar]
- Stuifbergen A, Becker H, Blozis S, Beal C. Conceptualization and development of the acceptance of chronic health conditions scale. Issues in Mental Health Nursing. 2008;29:101–114. doi: 10.1080/01612840701792548. [DOI] [PubMed] [Google Scholar]
- Teno JM. TIME: Toolkit of instruments to measure end of life care. 2004 Retrieved August 1, 2000 from http://www.chcr.brown.edu/pcoc/linkstoinstrumhtm.htm.
- Tilden VP, Tolle SW, Garland MJ, Nelson CA. Decisions about life-sustaining treatments. Archives of Internal Medicine. 1995;155:633–638. [PubMed] [Google Scholar]
- Tolstikova K, Fleming S, Chartier B. Grief, complicated grief, and trauma: The role of the search for meaning, impaired self-reference, and death anxiety. Illness, Crisis & Loss. 2005;18:293–313. [Google Scholar]
- Trentham-Dietz A, Walsh MC. Summary of results. Madison, WI: University of Wisconsin Paul P. Carbone Comprehensive Cancer Center; 2008. ACCESS: Assessment of Cancer CarE and SatiSfaction. [Google Scholar]
- Wolff JL, Dy SM, Frick KD, Kasper JD. End-of-life care: Findings from a national survey of informal caregivers. Annals of Internal Medicine. 2007;167:40–46. doi: 10.1001/archinte.167.1.40. [DOI] [PubMed] [Google Scholar]
- Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Journal of the American Medical Association. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey D, Greger HA, Coburn P. Determinants of grief resolution in cancer death. Journal of Palliative Care. 1990;6(4):24–31. [PubMed] [Google Scholar]
- Zhang A, El-Jawahri A, Prigerson HG. Update on bereavement research: Evidence-based guidelines for the diagnosis and treatment of complicated bereavement. Journal of Palliative Medicine. 2006;9:1188–1203. doi: 10.1089/jpm.2006.9.1188. [DOI] [PubMed] [Google Scholar]