Abstract
Depressive illness beginning early in life can have serious developmental and functional consequences. Therefore, understanding its etiology and pathophysiology during this developmental stage is critical for developing effective prevention and intervention strategies. There is considerable evidence of sleep alterations in adult major depressive disorder. However, studies in children and adolescents have not found consistent changes in sleep architecture paralleling adult depression. This review article summarizes sleep polysomnography research in early-onset depression, highlighting the factors associated with variable findings across studies. In addition, potential avenues for future research will be suggested in order to develop more comprehensive theoretical models and interventions for pediatric depression.
Keywords: child, adolescent, depression, sleep, polysomnography, EEG
1. Introduction
Depression is a leading cause of morbidity and mortality in youngsters. Major depressive disorder, the most severe form of depression, occurs approximately in 2% of children up to 8% of adolescents (Kessler et al., 2001; Lewinsohn and Essau, 2002), and it is associated with significant problems in multiple social domains (Birmaher et al., 1996). Elevated risk for the disorder begins in the early teens and continues to rise in a linear fashion throughout adolescence, with lifetime rates estimated to range from 15% to 25% by late adolescence (Giaconia et al., 1994; Hankin et al., 1998; Kessler et al., 2001; Weissman et al., 1997). Numerous studies also have documented that early depressive episodes persist or recur into adult life along with ongoing psychosocial difficulties (Birmaher et al., 1996; Rao and Chen, 2009). These difficulties include, but are not limited to, disruption in interpersonal relationships, early pregnancy, low educational attainment, poor occupational functioning and unemployment, as well as increased risk for suicidal behavior, resulting in substantial socioeconomic burden (Birmaher et al., 1996; Rao and Chen, 2009). A better understanding of the etiology and pathophysiology of early-onset depression will be helpful in the development and implementation of more effective primary and secondary preventive strategies, thereby allowing such youth to achieve their full potential as adults.
The pathogenesis of early-onset depressive disorder involves interactions among a range of predisposing and precipitating factors, which in combination lead to alterations in psychological and biological processes (Birmaher et al., 1996; Rao and Chen, 2009). The focus of this report will be limited to sleep disturbances associated with juvenile depression. In order to better understand the sleep changes associated with juvenile depression, a summary of the literature on adult depression will be provided; in contrast to the huge wealth of information available in adult populations, empirical data in youngsters are limited by relatively modest sample sizes in very few studies.
2. Association between Sleep Regulation and Depression
There has been considerable interest in the relationship between sleep disturbances and depression, with over 2,000 publications since the 1960s. There are a number of reasons to consider the regulation of sleep as an essential component for understanding the pathophysiology and treatment of depression. There is a significant overlap in the control of sleep and mood regulation (Adrien, 2002). Sleep complaints are commonly associated with depression and form an essential criterion of the diagnosis (American Psychiatric Association, 1994).
Developmental influence(s) on the rates of depression and maturational changes in sleep regulation also imply a close connection between depressive disorders and sleep regulation. As described above, mood disorders are relatively rare prior to puberty but increase dramatically during adolescence (Giaconia et al., 1994; Hankin et al., 1998; Kessler et al., 2001; Weissman et al., 1997). There is evidence that sleep regulation at younger ages is relatively "protected” against disruptions. Specifically, pre-school and early-school-aged children demonstrate the greatest levels of deepest (Stage IV) sleep (Feinberg, 1974); (Williams et al., 1974). A more detailed description of sleep stages is described below. Prepubertal children are highly resistant to being awakened from deep sleep (Busby and Pivik, 1985). Children also demonstrate remarkable daytime alertness on objective measures of sleep (Carskadon et al., 1983). By mid-to-late puberty, however, profound changes occur in sleep regulation. In particular, there is a large drop in slow-wave sleep (Carskadon et al., 1983; Coble et al., 1987; Dahl et al., 1990), decrease in the threshold of arousal to disrupt sleep (Busby et al., 1994), and a dramatic increase in objectively measured daytime sleepiness (Carskadon et al., 1983). There is also evidence for a shift in the circadian pattern, with a preference for late-night schedules in association with puberty (Carskadon et al., 1983).
Objective sleep changes typically associated with adult major depressive disorder are rarely seen in prepubertal depression, gradually emerge after puberty, and appear as consistent biological findings in later adolescence (Kaufman et al., 2001). More details regarding these objective sleep changes are described below. Increased risk for depression during adolescent development, greater vulnerability to perturbation of the sleep system during adolescence, and relatively more robust depression-related sleep changes in older adolescents suggest a link between sleep dysregulation and increased liability to depression.
In this review, sleep disturbances associated with adult and juvenile depression will be described. Potential influential factors on sleep parameters will be discussed in the context of understanding developmental continuities and discontinuities in sleep patterns associated with depressive disorder. Additionally, an overview of the theoretical models that have contributed to understanding the pathophysiology of depression will be provided. Finally, potential areas of future research will be suggested in order to develop more comprehensive theoretical models and interventions for pediatric depression.
3. Subjective Sleep Measures and Depression
Subjective sleep complaints can be assessed either through standardized self-report scales or clinical interviews. The information normally includes sleep/wake habits, and the duration, frequency and pattern of sleep disturbances.
3.1. Subjective sleep disturbances in adult depression
Sleep disturbance is a characteristic symptom of depressive disorders (American Psychiatric Association, 1994; Zimmerman et al., 2006), with subjective sleep complaints in over 80% of depressed patients (McCall et al., 2000; Reynolds and Kupfer, 1987). Typically, depressed patients suffer from difficulties in falling asleep, frequent nocturnal awakenings, and early morning awakening. While delayed sleep-onset and frequent awakenings accompany almost any kind of insomnia, early morning awakening was considered to be specific for endogenous depression but this hypothesis was not confirmed (Reynolds and Kupfer, 1987). Although insomnia is the most frequent complaint, hypersomnia also has been observed (Garvey et al., 1984; Hawkins et al., 1985), particularly in individuals with bipolar depression (Parker et al., 2006; Thase et al., 1989).
In a relatively recent study, insomnia was measured simultaneously by clinician ratings (Hamilton Depression Rating Scale; HRSD) and self-report (Beck Depression Inventory; BDI) in a sample of inpatients with major depressive disorder. A high proportion of patients reported insomnia on both measures; 93% and 97%, respectively (McCall et al., 2000). However, there was only a modest correlation in the severity of insomnia between the two measures. Also, increasing severity of insomnia on the HDRS was associated with better quality of life, while increasing severity of insomnia on the BDI was associated with worse quality of life. These data suggest that these two measures tap into different components of the insomnia severity in depressed patients.
In addition to cross-sectional evidence on the association between subjective sleep disturbances and depression, prospective studies demonstrated that sleep disturbances increase the risk for depressive disorders (Franzen and Buysse, 2008; Riemann and Voderholzer, 2003). Persistent insomnia also has been linked to increased risk of relapse and suicide (Agargun et al., 2007; Breslau et al., 1996; Wingard and Berkman, 1983).
3.2. Subjective sleep disturbances in pediatric depression
Few studies have assessed the prevalence and nature of subjective sleep complaints in children and adolescents with depression (Ivanenko et al., 2005; Lofthouse et al., 2009). In a study of prepubertal children with major depressive disorder, approximately two-thirds reported sleep-onset and sleep-maintenance insomnia, whereas almost 50% experienced terminal insomnia (Puig-Antich et al., 1982). Subsequent studies, including both children and adolescents with major depression, found that almost 75% manifested sleep disturbances, with over 50% experiencing insomnia only, approximately 10% with hypersomnia alone and 10% with both insomnia and hypersomnia (Liu et al., 2007; Yorbik et al., 2004). In an epidemiological sample of adolescents, almost 90% of those who met criteria for major depression indicated sleep disturbances, and approximately 75% of adolescents who initially reported sleep disturbances subsequently developed a depressive episode (Roberts et al., 1995). In a controlled investigation of children and younger adolescents with major depression, subjective ratings of sleep were assessed during a laboratory sleep study (Bertocci et al., 2005). Compared with controls matched on age, gender and pubertal status, participants with depression reported poor sleep quality, increased number of awakenings, longer wake time and difficulty in waking in the morning. Even youngsters with dysthymic disorder experience sleep disturbances (Masi et al., 2003).
Sleep problems seem to be associated with greater severity of depression as well as more protracted and recurrent episodes, particularly in those who manifest both insomnia and hypersomnia (Liu et al., 2007). Additionally, sleep disturbances increase the risk for suicidal behavior in depressed youngsters (Barbe et al., 2005; Goldstein et al., 2008; Lofthouse et al., 2009; Roane and Taylor, 2008). Comorbid anxiety disorders also might be more common in depressed youth with sleep difficulties, specifically those with insomnia (Liu et al., 2007). Longitudinal studies revealed that sleep problems increase vulnerability to depressive disorders in children and adolescents (Gregory et al., 2009; Ong et al., 2006; Roane and Taylor, 2008; Roberts et al., 2002).
Taken together, subjective sleep complaints are highly prevalent in both youngsters and adults suffering from depression. Persistent sleep problems also might be associated with increased vulnerability to depression and poor clinical course.
4. Objective Measures of Sleep
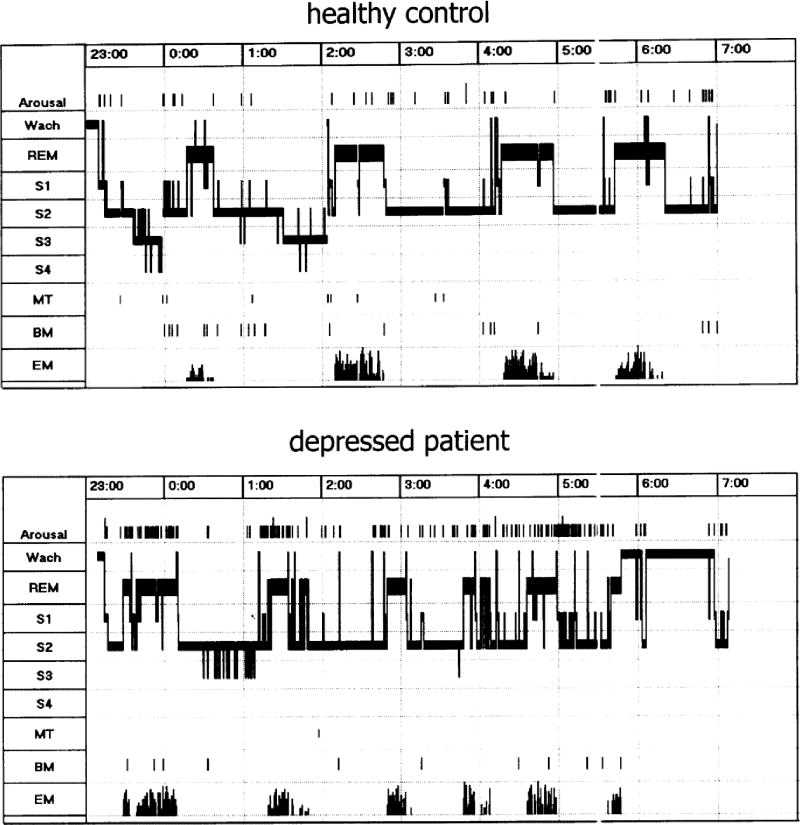
Laboratory-based sleep studies examine the physiological characteristics of sleep through electroencephalographic (EEG) sleep measures or polysomnography. The traditional method of reporting EEG sleep parameters is macroarchitecture, and it refers to the visual method of scoring sleep stages; for example, proportion and time spent in rapid eye movement (REM) sleep and the four stages of non-rapid eye movement (NREM) sleep (see Figure 1). The time between sleep-onset and the appearance of the first REM sleep episode is known as REM latency. REM activity and REM density denote the number of eye movements during REM sleep. Delta or slow-wave sleep refers to stages 3 and 4 of NREM sleep. Sleep microarchitecture refers to the measures derived from all-night computerized, quantitative EEG analysis including frequency, amplitude and power in five standard EEG bands: alpha, beta, delta, sigma and theta.
Figure 1.
Sleep profile of a medication-free depressed female patient and a healthy female control. Compared to the healthy subject, the sleep profile of this patient shows many of the typical features of sleep in depression — impaired sleep continuity, disinhibition of REM sleep and reduction of slow-wave sleep. W, Wake; REM, rapid eye movement sleep; S1–4, sleep stages 1–4; MT, Movement time; BM, body movements; EM, rapid eye movements (reprinted from Riemann et al., Biological Psychology, 2001;57:67–103).
In healthy subjects, the onset of sleep occurs about 10–15 minutes after switching off the lights, followed shortly thereafter by the progression of deeper stages of NREM sleep. The first REM period occurs approximately 90 minutes after sleep onset. NREM and REM sleep alternate throughout the night, with each sleep cycle lasting about 90–120 minutes. Short periods of intermittent awakenings occur throughout the night. The first REM episode is short in duration (1–5 minutes) but lengthens progressively across the night, whereas slow-wave sleep is concentrated in the early part of the night (see Figure 1).
4.1. Objective sleep disturbances associated with adult depression
Starting in the 1970s, numerous controlled studies have been conducted in adult patients with depression. Although no single EEG sleep marker is specifically associated with depressive disorders, a constellation of sleep changes has been observed consistently in patients suffering from major depressive disorder (Armitage, 2007; Benca et al., 1992; Riemann et al., 2001; Tsuno et al., 2005). The most reliable sleep macroarchitectural changes associated with major depression include sleep continuity disturbances (e.g., delayed sleep onset, and decreased sleep efficiency), shorter REM latency, increased REM activity and REM density, increased amount of REM sleep, and diminished slow-wave sleep (see Figure 1).
Sleep microarchitectural changes also have been described in relation to depression. Increased alpha and fast-frequency β activity were found both during NREM and REM sleep, suggesting hyperarousal and sleep fragmentation in individuals with depression (Armitage, 2007; Armitage et al., 1992b; Liscombe et al., 2002). Other studies reported reduced slow-wave activity (Borbely et al., 1981), particularly during the first NREM period (Kupfer et al., 1990). Also, lower temporal coherence of EEG sleep recorded from left and right hemispheres, and decreased synchronization of fast frequency activity have been observed in association with depression (Armitage, 2007; Armitage et al., 1999).
4.2. Objective sleep disturbances associated with pediatric depression
In contrast to the high frequency of subjective sleep complaints, EEG sleep studies in children and adolescents with depression have often failed to find objective evidence of sleep dysregulation (Ivanenko et al., 2005; Lofthouse et al., 2009). In fact, in the above-described study in which subjective sleep complaints were recorded in the laboratory, depressed youth with the most severe sleep quality ratings manifested significantly better sleep with respect to the number of awakenings and other objective measures of EEG sleep (Bertocci et al., 2005). These findings suggest that the subjective perception of sleep may differ from objectively measured sleep.
Among studies of sleep macroarchitecture (see Table 1), shorter REM latency, the most frequently observed marker of depression in youngsters, was observed only in 3/7 child samples(Arana-Lechuga et al., 2008; Dahl et al., 1990; Emslie et al., 1990), 8/13 adolescent samples (Dahl et al., 1990, 1996; Emslie et al., 1994; Kutcher et al., 1992; Lahmeyer et al., 1983; Rao and Poland, 2008; Rao et al., unpublished data; Riemann et al., 1995), and 0/3 studies that included both children and adolescents. Other observed EEG sleep changes in depressed youngsters included prolonged sleep latency (Arana-Lechuga et al., 2008; Armitage et al., 2000; Dahl et al., 1990; Dahl et al., 1996; Emslie et al., 1994; Goetz et al., 1987; Kutcher et al., 1992), decreased sleep efficiency (Appelboom-Fondu et al., 1988; Emslie et al., 1994; Goetz et al., 1987), and increased REM density (Cashman et al., 1986; Dahl et al., 1990; Emslie et al., 1994; Lahmeyer et al., 1983; McCracken et al., 1997; Rao and Poland, 2008; Rao et al., unpublished data). With respect to slow-wave sleep deficits, only one study revealed overall group differences (Rao et al., unpublished data) although changes were observed in certain subgroups of patients. In an investigation of prepubertal children, only a subset of the children who had more severe depression manifested reduced stage 4 sleep (Dahl et al., 1994). In a separate study that included both children and adolescents, reduced slow-wave sleep, particularly in the first NREM period, was observed only in adolescent males with depression (Robert et al., 2006).
Table 1.
EEG Sleep Studies Children and Adolescents
| Citation | Sample | Sleep latency | Sleep efficiency | REM latency | REM density | Delta sleep |
|---|---|---|---|---|---|---|
| Studies Conducted with Children | ||||||
| 21 High CDI | ||||||
| Arana-Lechuga et al. (2008) | 7 Low CDI | ↑ | = | ↓ | = | = |
| 36 MDD | ||||||
| Dahl et al. (1991) | 18 NC | = | = | =a | = | =a |
| 33 MDD | ||||||
| Dahl et al. (1994) | 15 NC | = | = | =b | = | = |
| 25 MDD | ||||||
| Emslie et al. (1990) | 20 NC | ↑ | = | ↓ | = | = |
| 39 MDD | ||||||
| Goetz et al. (1985) | 8 NC | = | = | = | = | = |
| 54 MDD | ||||||
| Puig-Antich et al. (1982) | 11 NC | = | = | = | = | = |
| 12 MDD | ||||||
| Young et al. (1982) | 12 NC | = | = | = | = | = |
| Studies Conducted with Adolescents | ||||||
| 9 MDD | ||||||
| Appelboom-Fondu et al. (1988) | 12 NC | = | ↓ | = | = | = |
| 8 MDD | ||||||
| Armitage et al. (2001) | 8 NC | = | = | = | = | = |
| 15 MDD | ||||||
| Cashman et al. (1986) | 15 NC | - | - | = | ↑ | = |
| 27 MDD | ||||||
| Dahl et al. (1990) | 30 NC | ↑ | = | ↓c | ↑c | = |
| 16 MDD | ||||||
| Dahl et al. (1996) | 21 NC | ↑ | = | ↓ | = | = |
| 31 MDD | ||||||
| Emslie et al. (1994) | 17 NC | ↑ | ↓ | ↓ | ↑ | = |
| 49 MDD | ||||||
| Goetz et al. (1987) | 40 NC | ↑ | ↓ | = | = | = |
| 23 MDD | = | |||||
| Kutcher et al. (1992) | 28 NC | ↑ | = | ↓ | = | |
| 20 MDD | ||||||
| McCracken et al. (1997) | 13 NC | = | = | = | ↑ | = |
| 13 MDD | ||||||
| Lahmeyer et al. (1983) | 13 NC | = | = | ↓ | ↑ | = |
| 16 MDD | ||||||
| Rao and Poland (2008) | 16 NC | = | = | ↓d | ↑d | = |
| 55 MDD | ||||||
| Rao et al (unpublished data) | 48 NC | = | = | ↓ | ↑ | ↓ |
| 10 MDD | ||||||
| Riemann et al. (1995) | 10 NC | = | = | ↓ | = | - |
| Studies Conducted with both Children and Adolescents | ||||||
| 50 MDD | ||||||
| Armitage et al (2000) | 15 NC | ↑ | = | = | = | = |
| 51 MDD | ||||||
| Bertocci et al (2005) | 42 NC | = | - | - | - | - |
| 128 MDD | ||||||
| Forbes et al (2008) | 101 NC | = | = | = | = | = |
| 97 MDD | ||||||
| Robert et al (2006) | 76 NC | = | = | = | = | =e |
REM = Rapid eye movement; CDI = Children’s Depression Inventory; MDD = major depressive disorder; NC = Normal Controls
= means no change; ↑ = increase; ↓ = decrease; - = no data (symbols represent data for MDD vs. NC)
MDD subgroup with increased depression severity had reduced REM latency and stage 4 sleep
Infusion of arecoline (0.5mg) during the first non-REM sleep period revealed ↓ REM Latency in MDD group
Differences were reported only for MDD subgroup with suicidal and/or inpatient status vs. NC
Sleep changes in the MDD group persisted during sustained remission
Adolescents with MDD had the least amount of delta sleep in the first sleep period
Even fewer studies examined sleep microarchitectural changes in depressed youth. In one investigation, depressed youngsters exhibited lower intra-and inter-hemispheric coherence than controls (Armitage et al., 2000). In a subsequent investigation, lower delta amplitude and power was observed in adolescent females with depression (Armitage et al., 2001).
In summary, EEG sleep changes have been observed quite consistently in association with adult depression. In contrast to this, there is significant heterogeneity in EEG sleep findings in studies investigating pediatric depression. Potential factors that might contribute to these discrepancies will be described below.
4.3. Factors influencing sleep abnormalities in depression
Chronological age seems to have a significant influence on EEG sleep parameters. Even among healthy adults, increased number of nocturnal awakenings, early morning awakening, reduced slow-wave sleep and shortened REM latency are more predominant in older individuals (Bliwise, 1993; Miles and Dement, 1980; Williams et al., 1974). Sleep continuity disturbances, shortened REM latency and diminished slow-wave sleep seem to be more robust in older patients with depression (Benca et al., 1992; Knowles and MacLean, 1990; Lauer et al., 1991), although one research group reported more robust changes in slow-wave activity among younger adults than older subjects (Armitage et al., 2000). Age does not appear to influence REM density (Lauer et al., 1991). Among pediatric samples, both macro- and microarchitectural changes are more prevalent in adolescents (Armitage, 2007; Armitage et al., 2006; Ivanenko et al., 2005; Robert et al., 2006).
Some studies examined the impact of gender on sleep. Healthy males have less slow-wave sleep than females (Williams et al., 1974). Among adults, both macro-and microarchitecture analyses indicated that slow-wave sleep deficits are more prevalent in depressed males than females (Armitage et al., 2000; Reynolds et al., 1990). Among youngsters, age, gender and depression diagnosis interacted, with depressed adolescent males exhibiting most severe sleep problems including highest proportion of stage 1 sleep, shortest REM latency and lowest percentage of slow-wave sleep (Robert et al., 2006). However, adolescent females had the lowest temporal coherence (Armitage et al., 2006). Summarizing the data on gender differences, Armitage (2007) has hypothesized that low slow-wave activity and impaired sleep homeostasis might be a primary biological risk factor for depression in males, whereas low temporal coherence serves as a vulnerability marker specifically in females.
Ethnicity/race also plays a role in sleep regulation. Evidence suggests that healthy adult African-Americans have more frequent sleep continuity disturbances and less proportion of slow-wave sleep compared with Hispanics or Non-Hispanic Whites (Mezick et al., 2008; Profant et al., 2002; Rao et al., 1999a; Redline et al., 2004; Stepnowsky et al., 2003). In contrast to the ethnic differences in sleep continuity disturbances and NREM sleep, few studies reported variations in REM sleep. In one investigation, Hispanics had increased phasic REM sleep compared to African-Americans and Non-Hispanic Whites (Rao et al., 1999a). These cross-ethnic differences in NREM and REM sleep also were replicated in a group of healthy adolescents (Rao et al., 2009a). Similar patterns of cross-ethnic differences in sleep profiles were observed in adult patients with depression. African-American patients with depression had less efficient sleep and NREM sleep changes, whereas Hispanic and Non-Hispanic White patients manifested predominantly REM sleep changes, although the ethnic groups were comparable on clinical symptoms and severity of depression (Giles et al., 1998b; Poland et al., 1999).
Depression severity and symptom patterns (e.g., depression subtype) also might affect sleep profiles. Among adults, some studies demonstrated that greater depression severity is associated with more impaired sleep including sleep continuity disturbances (Kerkhofs et al., 1988; Thase et al., 1986), reduced slow-wave sleep (Armitage, 2007; Thase et al., 1986), shortened REM latency (Akiskal et al., 1982; Cartwright, 1983; Thase et al., 1986), and increased REM density (Cartwright, 1983; Thase et al., 1986). In a pediatric study, a subgroup that exhibited shorter REM latency, more REM time and less stage 4 sleep had more severe depression (Dahl et al., 1994). In a separate investigation, although depression severity itself did not affect EEG sleep measures, delayed sleep onset, reduced REM latency and higher REM density was observed only in a subgroup of depressed adolescents with inpatient and suicidal status (Dahl et al., 1990).
Several investigators examined the relationship between different subtypes of depression and EEG sleep changes. Although majority of the studies failed to show significant associations (Riemann et al., 2001; (Tsuno et al., 2005), some studies reported shorter REM latency in adult patients with endogenous depression than in those with non-endogenous depression (Giles et al., 1986a; Kerkhofs et al., 1988; Rush et al., 1982). It is important to note that the endogenous groups of patients in these studies had greater depression severity than the non-endogenous groups. Reduced REM latency also was observed in adolescents with endogenous depression (Kutcher et al., 1992). Some investigations described more pronounced abnormalities in REM sleep in adolescent and adult patients with psychotic depression (Kupfer and Foster, 1972; Kupfer et al., 1986; Naylor et al., 1990), whereas other studies did not detect such differences (Ivanenko et al., 2005; Kerkhofs et al., 1988; Riemann et al., 2001). Several studies examined EEG sleep profiles in adult patients with seasonal affective disorder, and none of them found the typical sleep patterns observed in major depression (Anderson et al., 1994; (Brunner et al., 1993, 1996; Partonen et al., 1993; Rosenthal et al., 1989).
In conclusion, there is substantial evidence for developmental differences in sleep regulation. Gender and ethnicity/race also have an impact on sleep. There is little evidence that depression severity and sub-types of depression have a significant influence on EEG sleep parameters.
4.4. Stability of EEG sleep measures
An important question is whether the sleep “abnormalities” observed during the acute episode of depression normalize when the symptoms remit (“state” marker), or if they persist even during clinical remission (“scar” marker). From various adult samples with depression, including cross-sectional comparison of remitted patients with healthy controls, single episode cases versus those with recurrent illness, and prospective follow-up of individual patients through recovery, there is emerging consensus that EEG sleep disruptions associated with major depressive illness are remarkably stable from episode to recovery (for a review, see (Rao and Poland, 2008; Riemann et al., 2001; Tsuno et al., 2005). A few investigations, however, demonstrated normalization of certain EEG sleep measures during remission, particularly sleep continuity disturbances (Buysse et al., 1997; Cartwright, 1983; Riemann et al., 2001). Also, it appears that some EEG sleep changes during remission might be too subtle to be detected by visual scoring methods (Buysse et al., 1992a).
The discrepant findings among adult depressed patients on the stability of EEG sleep measures from episode to recovery suggest potential differences in the risk for relapse. Sleep measures might normalize in depressed patients with a low risk for relapse, whereas those prone to relapse tend to exhibit sleep abnormalities even during remission (Riemann et al., 2001; Thase et al., 1998). For instance, persistence of shortened REM latency during remission was associated with increased risk for relapse (Giles et al., 1987). Also, depressed patients with lower slow-wave sleep intensity during the first NREM period than the second one (“low delta ratio”) were five times more likely to develop a recurrent episode over the 2-year follow-up period than those with higher delta ratio (Kupfer et al., 1990).
To the best of my knowledge, there are only two reports of repeated EEG sleep assessments performed during the depressive episode and remission in youngsters (Rao and Poland, 2008; Rao et al., 1997). Both studies demonstrated persistent sleep abnormalities during remission in depressed adolescents.
4.5. EEG Sleep measures as vulnerability markers for depression
It is also important to know whether depression-related EEG sleep changes are already present before the clinical manifestation of the disorder (i.e., “trait” or “vulnerability” marker). A higher concordance in sleep macro- and micro-architecture has been observed in monozygotic twins compared to dizygotic twins (Ambrosius et al., 2008; Kimura and Winkelmann, 2007). There is also evidence that shortened REM latency and related sleep characteristics are familial and might be associated with increased risk for depression, beyond the risk conferred by depressive illness in relatives (Giles et al., 1992, 1998a). Specific depression-related EEG sleep markers were observed in healthy adolescents and adults who were at high familial risk for depression (Friess et al., 2008; Fulton et al., 2000; Giles et al., 1998a; Lauer et al., 1995; Morehouse et al., 2002; Rao et al., 2009b; Schreiber et al., 1992; Sitaram et al., 1987). These EEG sleep markers predicted the subsequent onset of depression (Giles and Kupfer, 1994; Lauer et al., 2004; Modell et al., 2005; Morehouse et al., 2002; Rao et al., 2009b). In addition to identifying highly vulnerable persons, familial aggregation of specific EEG sleep abnormalities might delineate a valid subtype of the depressive illness. For instance, familial aggregation of short REM latency was associated with similar clinical features and psychological profiles of depression among relatives (Giles et al., 1988, 1990).
These results confirm that EEG sleep measures can serve as vulnerability markers for identifying individuals who are at significant risk for developing depressive disorder in order to target them for primary prevention. They also might serve as suitable endophenotype measures for identifying more homogeneous subgroups of depressed patients as well as detecting the mode of inheritance, thereby aiding in developing more specific and effective interventions for the different subgroups (Gottesman and Gould, 2003).
4.6. EEG sleep measures as predictors of clinical course of depression
Among adults, certain EEG sleep measures, including reduced REM latency and diminished slow-wave sleep, have been shown to predict early relapse following the successful treatment of depressive episodes (Giles et al., 1987; Grunhaus et al., 1994; Kupfer et al., 1990; Reynolds et al., 1989).
Although EEG sleep measures did not discriminate depressed youngsters from controls in some cross-sectional studies, these same variables were helpful in predicting differential clinical course over time. For instance, adolescent healthy controls that manifested reduced REM latency and higher REM density at baseline were more likely to develop a depressive episode subsequently (Rao et al., 1996). In the same study, depressed adolescents who had a normal REM sleep profile but a tendency for reduced slow-wave sleep developed bipolar disorder (Rao et al., 2002). Although the depressed adolescents, as a group, did not exhibit EEG sleep changes at baseline (Dahl et al., 1990), after separating these latent depressive and bipolar groups from their respective cohorts, the sleep profile of the depressed youth with unipolar course was similar to the pattern seen in adult depression (Rao et al., 2002). Also, depressed adolescents who subsequently developed substance use disorders had relatively normal EEG sleep patterns compared to those who did not develop the disorder (Rao et al., 1999b).
In a separate investigation, longer sleep latency and decreased sleep efficiency predicted recurrent depression (Emslie et al., 2001). In a subset of this cohort, depressed youth who exhibited lower hemispheric coherence, particularly boys, were less likely to recover from the index depressive episode or were at increased risk for a recurrent episode after recovery (Armitage et al., 2002). Another study identified longer sleep latency and sleep period time as predictors of lifetime depression at follow-up in adulthood, whereas the combination of reduced REM latency and diminished slow-wave sleep predicted suicidality (Goetz et al., 2001).
The observed variability in EEG sleep changes in depressed youngsters may reflect, at least in part, heterogeneity in the longitudinal clinical course of these disorders. For example, sleep data in adults suggest distinct biological substrates in unipolar and bipolar mood disorders. REM latency changes were observed less frequently in bipolar depression (Giles et al., 1986b; Rao et al., 2002; Thase et al., 1989). Sleep loss can effectively trigger the onset of mania in patients with bipolar illness (Barbini et al., 1996; Wehr et al., 1987), but it has minimal euphorigenic effect in unipolar depression. Therapeutic sleep deprivation also appears to have different clinical effects in unipolar and bipolar patients (Barbini et al., 1998). A substantial minority of youngsters initially identified as having unipolar depression subsequently develop bipolar disorder, and those with early-onset illness in particular (Geller et al., 2001). Among pediatric samples, studies that excluded depressed patients with a family history of bipolar disorder were more likely to demonstrate EEG sleep changes compared with controls (Armitage et al., 2000; Emslie et al., 1990; Rao and Poland, 2008; Rao et al., unpublshed data).
These findings together with the observation that EEG sleep markers are evident prior to the clinical manifestation of depressive illness emphasize the need for careful selection of experimental and control groups based on both family and personal history.
5. Antidepressant Treatments and Sleep
5.1. Sleep deprivation therapy
One of the most striking links between depression and sleep regulation is the observation that depressive symptoms are alleviated by acute sleep deprivation for a night and that the initial symptoms reemerge after recovery sleep the following night (Pflug and Tolle, 1971; Svestka, 2008). A meta-analysis of sleep deprivation studies in adults concluded that approximately 50% to 60% of depressed patients show a transient improvement in mood after total sleep deprivation (Wu and Bunney, 1990). This is the only known intervention that has proven anti-depressive benefits within 24 hours. Because majority of the un-medicated patients (up to 80%) relapse after the next night of sleep, the clinical utility of this intervention is limited. However, from a research perspective, sleep deprivation offers a unique opportunity to relate rapidly occurring changes in mood to simultaneous changes of neurobiological measures (Benedetti and Smeraldi, 2009; Gillin et al., 2001; Wirz-Justice and Van den Hoofdakker, 1999).
Functional neuroimaging studies have revealed that responders to sleep deprivation have elevated glucose metabolism in the ventral portion of the cingulate cortex at baseline, which normalizes after total sleep deprivation (Gillin et al., 2001). Evidence suggests that signal transduction in the cingulate gyrus is dominated by cholinergic neurotransmission, which is involved in REM sleep regulation (McCarley, 2007; Nofzinger, 2005). Additionally, single photon emission computed tomography (SPECT) studies using a radioactively labeled dopamine (D2) receptor antagonist suggest that the antidepressant benefits of sleep deprivation are correlated with endogenous release of dopamine (Gillin et al., 2001; Nofzinger, 2005). Another model focuses on the role of the neuromodulator adenosine, which is now known to be involved in sleep regulation (McCarley, 2007).
Variations of total sleep deprivation have been developed for therapeutic intervention in depression. Because of the changing direction in circadian rhythm of several bodily functions, it has been proposed that staying awake in the early morning should be the central target for maximizing the therapeutic efficacy of total sleep deprivation (Schilgen et al., 1976). Although an early study reported that late partial sleep deprivation was as effective as total sleep deprivation (Schilgen et al., 1976), recent investigations concluded that total sleep deprivation was indeed more effective than partial sleep deprivation (Giedke et al., 2003; Svestka, 2008).
Almost all antidepressant drugs inhibit REM sleep, although the magnitude of effect varies between compounds within antidepressant classes (Mayers and Baldwin, 2005; Sandor and Shapiro, 1994). In order to examine whether the underlying mechanism of action of antidepressant drugs occurs via REM sleep suppression, some investigators utilized the selective REM sleep deprivation strategy (Svestka, 2008; Vogel, 1983). In a controlled study, although selective REM sleep deprivation improved mood, the NREM sleep deprivation group exhibited an even stronger antidepressant effect (Grozinger et al., 2002). Both experimental conditions increased the duration of NREM sleep cycles and, therefore, it was postulated that this might be the underlying mechanism of action.
Several techniques have been used to try to reduce the relapse of depressive symptoms following sleep deprivation. Although antidepressant drugs have little influence on the rate of response to single-night sleep deprivation, they might increase the response to multiple nights of sleep deprivation (Wirz-Justice and Van den Hoofdakker, 1999). Several investigators examined the effects of adjunctive pharmacotherapy or bright light therapy with multiple days of sleep deprivation, and these strategies resulted in more sustained improvement in depressive symptoms (Colombo et al., 2000; Giedke and Schwarzler, 2002; Smeraldi et al., 1999; Wehr et al., 1985; Wu et al., 2009).
In pediatric depression, only three studies examined the effect of sleep deprivation. The first study described the case of a 12-year-old boy who received combined partial sleep deprivation and antidepressant agent, which resulted in significantly improved mood for 1–2 days (King et al., 1987). A subsequent investigation examined the effect of sleep deprivation in four adolescents with major depression and attention-deficit hyperactivity disorder, and it reported improved mood and psychomotor activity for 3 days following treatment (Detrinis et al., 1990). The final study employed sleep deprivation for 36 hours in 17 patients (Naylor et al., 1993). Severely depressed adolescents showed a decrease in depression severity, whereas remitted depressed patients and psychiatric controls showed a worsening of symptoms after sleep deprivation.
Taken together, these findings suggest that sleep deprivation can have therapeutic utility in depression, particularly in conjunction with chronobiological or pharmacological treatment. Moreover, sleep deprivation is a useful tool for understanding the pathophysiology of mood disorders.
5.2. Pharmacological Interventions
Almost all antidepressant drugs have been shown to impact sleep architecture, notably delayed onset of REM sleep, reduced amount of REM sleep and increased slow-wave sleep (Mayers and Baldwin, 2005; Winokur et al., 2001). A large body of evidence indicates robust suppression of REM sleep immediately after antidepressant administration (Mayers and Baldwin, 2005; Winokur et al., 2001). Exceptions to this rule are trimipramine (Dunleavy et al., 1972; Wiegand et al., 1986) and trazodone (Ware and Pittard, 1990), where no REM sleep suppression occurs. Nefazodone and bupropion, both atypical antidepressants, actually enhance REM sleep (Nofzinger et al., 1995; Sharpley et al., 1992). Also, REM sleep suppression is less pronounced with the selective and reversible monoamine oxidase inhibitor (MAOI), meclobemide (Steiger et al., 1994). The effect of antidepressants on NREM sleep is less evident and less consistent. In general, tricyclic agents and antidepressants having significant 5-HT2A/2C receptor antagonist properties (e.g., trazodone, mianserin) increase slow-wave sleep, whereas other drugs, such as SSRIs or MAOIs, either lower slow-wave sleep or produce no change (Sharpley and Cowen, 1995). Antidepressants with sedating properties, such as certain tricyclic agents, trazodone and mianserin, improve sleep continuity variables. Some non-sedating drugs (e.g., ritanserin and nefazodone) also improve sleep continuity measures, possibly through 5-HT2A/2C receptor blockade (Sharpley and Cowen, 1995).
In contrast to the relatively strong influence of antidepressant drugs on REM sleep, mood stabilizers exhibit only minimal effects on REM sleep but enhance slow-wave sleep (Alfaro-Rodriguez et al., 2002; Friston et al., 1989; Harding et al., 1985; Yang et al., 1989). Preliminary data on lamotrigine and gabapentin suggest that they, in fact, increase REM sleep and reduce slow-wave sleep (Placidi et al., 2000).
A temporal discordance between REM sleep suppression and clinical response to antidepressants has been reported. For instance, clomipramine produces immediate suppression of REM sleep but clinical response is seen approximately 10 days later (Goldenberg, 1994). In contrast to this, although suppression of REM sleep in response to MAOIs is significantly delayed (about 10 days), this coincides temporally with clinical improvement (Kupfer et al., 1972). It is also not clear how long REM sleep suppression persists during long-term treatment with antidepressants. Some studies reported an attenuation of REM sleep suppression within 3–5 weeks of treatment (Berger et al., 1986); (Riemann et al., 1990), whereas another investigation demonstrated a persistent effect of antidepressants on REM sleep that persisted for up to 3 years (Kupfer et al., 1994).
Some investigators indicated that EEG sleep measures might be helpful in predicting clinical response to antidepressant therapy. Baseline REM latency (prior to treatment initiation) predicted response to antidepressant treatment (Akiskal et al., 1980); (Coble et al., 1979); (Rush et al., 1989); (Svendsen and Christensen, 1981), although some studies failed to replicate this finding (Berger et al., 1986); (Riemann et al., 2001). Additionally, the magnitude of REM sleep suppression during the early stages of antidepressant treatment predicted clinical response to antidepressant drugs (Gillin et al., 1978; Hochli et al., 1986; Kupfer et al., 1981; Ott et al., 2002; Reynolds et al., 1991; Vogel et al., 1990).
Compared with the rich data source examining the effects of pharmacological treatments on depression-related sleep problems in adults, only few studies examined this issue in pediatric samples. The first report involved the effect of a 3-week course of imipramine in 12 hospitalized children with depressive symptoms (Kupfer et al., 1979). REM sleep suppression was most pronounced in those whose depression improved significantly. Imipramine also increased wakefulness and stage 2 sleep but decreased sleep efficiency and slow-wave sleep. In a subsequent study, robust REM sleep suppression occurred in response to acute administration of imipramine in 10 hospitalized adolescents with unipolar depression (Shain et al., 1990). Consistent with the effects in adults, fluoxetine treatment was associated with poor sleep quality in both subjective and objective sleep measures in 6 youngsters, and the drug had minimal effect on REM latency (Armitage et al., 1997).
5.3. Somatic treatments
Electroconvulsive therapy (ECT) affects many EEG sleep parameters, most notably REM sleep suppression (Coffey et al., 1988; Grunhaus et al., 1988). Persistent short REM latency following ECT predicted poor clinical response to ECT as well as increased vulnerability to relapse in adults (Bourgon and Kellner, 2000; Grunhaus et al., 1994, 1997). Repetitive transcranial magnetic stimulation (rTMS) also was shown to suppress REM sleep (Cohrs et al., 1998).
5.4. Psychotherapy
Baseline EEG sleep measures, such as sleep continuity measures and reduced REM latency, predicted clinical response to cognitive-behavior therapy (CBT) and interpersonal therapy (IPT) in adult patients with depression (Buysse et al., 1992b; Jarrett et al., 1990b). However, no significant changes in EEG sleep macroarchitecture occurred in response to IPT although modest changes occurred in automated measures of delta sleep activity and REM sleep activity (Buysse et al., 1992a). Also, subsequent quantitative analysis indicated that increased number of REM counts was a robust predictor of non-response to IPT (Buysse et al., 2001). In a separate investigation, a group of depressed patients were categorized based on sleep profiles (including sleep efficiency, REM latency and REM density), and clinical response to IPT was examined. Patients with an “abnormal” sleep profile responded poorly to IPT compared to patients with a “normal” sleep profile (Thase et al., 1997). Furthermore, a substantial proportion of the poor responders to psychotherapy responded well to subsequent pharmacotherapy, suggesting that an abnormal sleep profile reflects a more marked disturbance of the central nervous system (CNS) arousal and warrants pharmacotherapy (Thase et al., 1997).
In summary, the literature on the impact of antidepressant treatment on REM sleep suggests that the majority of the successful treatment modalities suppress REM sleep. It is, however, not clear whether the EEG sleep changes associated with a given treatment are just epiphenomena of the normalization of psychopathological process or reflect a real effect on relevant underlying mechanisms. Also, some successful treatment strategies do not suppress REM sleep, thereby challenging the notion that REM sleep suppression is a necessary prerequisite for the antidepressant properties of an effective intervention.
It has been hypothesized that differential effects of antidepressants on sleep may reflect differences in receptor pharmacology, and thereby signal different pathways to treatment response (Reynolds, 1998). One pathway might involve REM sleep suppression, whereas the alternate pathway might involve the augmentation of slow-wave activity in the first sleep cycle. Both types of EEG sleep changes might reflect the amelioration of increased CNS arousal associated with depression. Consistent with this notion, greater beta power during NREM sleep was related to increased glucose metabolism in the ventromedial prefrontal cortex in depressed patients (Nofzinger et al., 2000).
6. The Functional Neuroanatomy of Sleep
In the past decade, a variety of studies have advanced our understanding of the functional neuroanatomy of the two primary sleep states, REM and NREM sleep (Nofzinger, 2005). Positron emission tomography (PET) studies, using regional cerebral flow as an index of neuronal activity, revealed that the intense and widespread cortical activation observed during sleep was not uniform (Nofzinger, 2005); (Braun et al., 1997); (Maquet et al., 1990). Several studies in healthy participants demonstrated that there is increased metabolic activity during REM sleep, particularly in the pontine tegmentum, thalamus, limbic regions and temporo-cortical areas (Buchsbaum et al., 2001); (Maquet et al., 1996); (Meyer et al., 1981); (Nofzinger et al., 1997). In contrast, the dorsolateral prefrontal cortex and parietal cortex, as well as the precuneus and posterior cingulate cortex, are least active during this sleep phase.
Globally, NREM sleep is functionally less active than either waking or REM sleep (Braun et al., 1997; Maquet et al., 1990). Several investigations demonstrated that, during the transition from waking to NREM sleep, there are regional reductions in heteromodal association cortex in the frontal, parietal and temporal lobes as well as the thalamus (Nofzinger, 2005); (Braun et al., 1997; Maquet et al., 1990). These findings are consistent with disfacilitation and active inhibition of the thalamocortical relay neurons in association with delta and spindle wave generation (Andersson et al., 1998; Braun et al., 1997; Hofle et al., 1997; Maquet et al., 1997).
Functional neuroimaging studies also have been helpful in clarifying some basic functions of sleep, such as sensory processing between waking and NREM sleep (Born et al., 2002), consolidation of memory during REM sleep (Laureys et al., 2001; Maquet et al., 2000), alertness and attention (Paus et al., 1998; Thomas et al., 2000), and the effects of sleep deprivation on cognitive performance (Thomas et al., 2000; Wu et al., 1991).
Utilizing [18F] FDG PET method, investigators have measured cerebral metabolism in 10 patients with depression and 10 controls during the first NREM period (Ho et al., 1996). They detected increased whole-brain metabolism in depressed patients, but most notably in the posterior cingulate, the amygdala, hippocampus, occipital and temporal cortex, and the pons. In contrast, depressed patients exhibited hypometabolism in the medial orbital prefrontal cortex, anterior cingulate, caudate and medial thalamus compared with controls. They concluded that this hypofrontality pattern supports the hyperarousal hypothesis of depression.
In order to further clarify the neurobiology of dysfunctional arousal in depression, Nofzinger et al. (2000) examined the relationship between β EEG power and regional cerebral glucose metabolism during NREM sleep. In both healthy and depressed participants, β power negatively correlated with subjective sleep quality. Also, significant correlations were seen between β power and metabolism in the ventromedial prefrontal cortex. At baseline, depressed patients demonstrated a trend toward greater beta power than controls. Within the depressed cohort, there was a trend for beta power to correlate with an indirect measure of absolute whole brain metabolism during NREM sleep. Given the increased electrophysiological arousal in some depressed patients and the known anatomical relations between the ventromedial prefrontal cortex and brain activating structures, they suggested that these findings raise the possibility that the ventromedial prefrontal cortex plays a significant role in mediating one aspect of dysfunctional arousal found in more severely aroused depressed patients.
As described above, the notion of hyperarousal in paralimbic structures in depression has received further support from the extensive literature describing the functional neuroanatomical correlates of the antidepressant response to sleep deprivation in depressed patients (Gillin et al., 2001).
It has been demonstrated that, while both healthy and depressed subjects showed activation in the limbic and anterior paralimbic regions during the transition from waking to REM sleep, the spatial extent of this activation was greater in depressed patients (Nofzinger et al., 2004). Additionally, depressed patients showed relatively greater activation in bilateral dorsolateral prefrontal, primary sensorimotor, left premotor and left parietal cortices, as well as in the midbrain reticular formation. The findings indicated that the altered function of limbic/anterior paralimbic and prefrontal circuits in depression may be accentuated during the REM sleep state and that this is characteristic of the observed REM sleep dysregulation in EEG sleep studies (Benca et al., 1992; Nofzinger et al., 2004; Reynolds and Kupfer, 1987). This group of authors also reported that REM density correlated positively with cerebral metabolic rate in the striatum, the posterior parietal cortices and medial and ventromedial prefrontal cortices in patients with depression (Germain et al., 2004). In contrast, REM density correlated negatively with metabolism in areas corresponding bilaterally to the lateral occipital cortex, cuneus, temporal cortex and parahippocampal gyrus. The areas where REM density was positively correlated with glucose metabolism appear to constitute a diffuse cortical system involved in the regulation of emotion-induced arousal, and that the observed pattern might be a marker of hypofrontality during REM sleep in depressed patients (Germain et al., 2004).
Taken together, these findings suggest that the neuronal processes underlying sleep differ between brain regions and depression is associated with hyperarousal. However, it is important to determine the extent to which the observed activation of brain regions is specific to depression or characteristic of psychiatric disorders in general.
7. Theoretical Models of Sleep Abnormalities in Depression
Current theories regarding the mechanisms underlying sleep disturbances in depression suggest that there is a reciprocal relationship between REM sleep and slow-wave sleep, such that a shorter latency to the first REM period results in reduced slow-wave sleep time in the first NREM period. It is, however, not clear whether the primary disturbance in depression is REM or slow-wave sleep regulation.
7.1. Two-process model of sleep regulation
Borbely (1082) proposed a model of sleep regulation based on the theoretical assumption that sleep is dependent on two processes: a homeostatic, sleep-inducing process (process “S”), and a circadian process (process “C”) (Borbely, 1982). According to this model, the interaction between process S and process C determines sleep propensity. Process S increases gradually during waking, resulting in an elevated initial level of slow-wave activity, which then decreases exponentially during sleep (Daan et al., 1984). Process C modulates the threshold of awakening and that of falling asleep. When process S declines to the level of process C, sleep is terminated. In accordance with this model, experimental studies demonstrated that the time course of slow-wave sleep activity is dependent on prior wakefulness (Dijk et al., 1990, 1992). Furthermore, slow-wave sleep activity is not influenced by the circadian phase, nor is its time correlated with that of core body temperature (Dijk et al., 1991).
According to the two process model, process S is deficient in depression, which is reflected by a reduction in delta-wave activity and slow-wave sleep (Borbely and Wirz-Justice, 1982). Studies utilizing frequency analysis of EEG sleep demonstrated reduced delta sleep in depression (Borbely et al., 1984;(Kupfer et al., 1984). As a consequence of reduced slow-wave sleep (particularly in the first NREM period), REM sleep occurs earlier (Kupfer and Ehlers, 1989). This model accounts for the anti-depressive effect of sleep deprivation in the sense that prolonging wakefulness increases process S and slow-wave sleep, resulting in improvement in depressed mood. However, several studies failed to show significant differences in the proportion or activity of slow-wave sleep in the first NREM period, or over the entire night, between depressed patients and controls (Armitage et al., 1992a; Knowles and MacLean, 1990).
7.2. The reciprocal interaction model of REM and NREM sleep
It has been postulated that the regulation of REM sleep depends on the balance between cholinergic (REM “on” neurons) and aminergic (REM “off” neurons) systems (Hobson et al., 1975). Thus, the neurotransmitter systems involved in REM sleep control are reciprocal and are responsible, in part, for subsequent REM/NREM sleep cycle oscillations. An early onset of REM sleep in depression reflects an imbalance in the normal cholinergic/aminergic neurotransmission that produces disinhibition of REM sleep (McCarley, 1982). In support of this theory, administration of cholinergic agonists triggers an earlier onset of REM sleep (Riemann and Berger, 1992; Riemann et al., 1994b). Several studies have shown an enhanced shortening of REM latency in response to cholinergic challenge in depressed patients compared to healthy controls (Riemann et al., 1994a, 1994b). One investigation in children also demonstrated greater shortening of REM latency in depressed youth than in controls (Dahl et al., 1994).
7.3. Abnormalities in the circadian rhythm
The periodic nature of depression, with a tendency for relapse and remission, indicates that mood changes might be regulated by an endogenous biological clock (Mendlewicz, 2009; Monteleone and Maj, 2008; Soria and Urretavizcaya, 2009). Recent advances in molecular genetics have implicated some “clock” genes in the regulation of circadian and seasonal rhythms in humans (Mendlewicz, 2009; Monteleone and Maj, 2008; Sangoram et al., 1998; van der Horst et al., 1999). In addition, mutations in clock genes have been related to disruptions in circadian cycles (Jones et al., 1999; Katzenberg et al., 1998; Mendlewicz, 2009). Some depressed patients manifest circadian abnormalities in mood, sleep, temperature and neuroendocrine secretion (Bunney and Bunney, 2000; Mendlewicz, 2009; Monteleone and Maj, 2008; Soria and Urretavizcaya, 2009). Abnormalities in clock-gene function are speculated to be associated with the circadian abnormalities of depression (Bunney and Bunney, 2000; Monteleone and Maj, 2008; Serretti et al., 2003).
7.4. Sleep-neuroendocrine relationships
In healthy humans, the first hours of sleep are characterized by peaks of slow-wave sleep and growth hormone along with a nadir in cortisol output. Ehler and Kupfer (1987) postulated that a disturbance in the interaction of two hypothalamic peptides [growth hormone-releasing factor (GRF) and corticotropin-releasing factor (CRF)] occurs in depression. They suggested that reduced GRF secretion and an increased output of CRF are involved in depression. Consistent with this hypothesis, increased nocturnal secretion of cortisol and adrenocorticotropic hormone (ACTH) has been observed consistently in depression (Steiger, 2002). Some studies also reported reduced growth hormone secretion in individuals with depression (Jarrett et al., 1990a; Steiger, 2003). However, it is not clear whether the sleep abnormalities and neuroendocrine disturbances are causally linked or related through a third factor (e.g., circadian rhythm disturbances).
In summary, various theories have been proposed to explain the sleep abnormalities in depression. Although each of these theories is supported by empirical data, there is still no convincing model capable of explaining all the typical EEG sleep changes associated with depression.
8. Summary and Future Directions in Sleep Research
Pediatric depression is of great public health significance, with serious morbidity and mortality, thereby emphasizing the need for early identification and effective treatment strategies. In the past three decades, considerable advances have been made regarding our knowledge on the phenomenology and natural course of juvenile depression. However, additional research is needed in understanding the pathogenesis of early-onset illness. In particular, studies aimed at elucidating mechanisms and interrelationships among the different domains of risk factors are important. Such knowledge will be beneficial in developing more effective preventive and treatment strategies. Towards this end, sleep research might provide some useful insights.
Sleep disturbance is a characteristic symptom of depressive disorders in both youngsters and adults. Developmental influences on the rates of depression and maturational changes in sleep regulation also imply a close connection between depressive disorders and sleep regulation. Although a clear causal relationship between sleep disturbance and depression has not been established yet, further research in this area might play an important role in optimizing prevention and treatment. Sleep research in adult depression has provided an extensive database and fruitful theoretical considerations concerning its etiology and pathophysiology, as well as the vulnerability for developing depressive episodes. Further studies linking the different areas of research are needed to validate such theories, also including an emphasis on developmental influences.
It is suggested that research on REM sleep may be more closely connected with the work on NREM sleep, especially slow-wave sleep, to better understand these two interdependent sleep states. Further attention is warranted on sleep-neuroendocrine interactions. Until now, the different approaches relating chronobiological, neuroendocrine and pharmacological aspects of depression have rarely been studied simultaneously. Neuroimaging studies of sleep have provided glimpses into how functional changes in the various brain regions are related to sleep abnormalities in depression. Further work is needed to clarify the reliability and specificity of these brain changes in relation to depression, as well as their association with clinical outcomes. Finally, a deeper insight into the relationship between sleep and depression might come from molecular genetic studies. Preliminary evidence suggests that sleep alterations in at-risk populations are vulnerability markers for depression. Examination of the circadian clock and circadian rhythm research in depression suggests that circadian abnormalities in depression may be related to alterations of clock genes.
Acknowledgments
This work was supported, in part, by grants DA017805, MH068391, RR003032 and R026140 from the National Institutes of Health, and by the Endowed Chair in Brain and Behavior Research at Meharry Medical College. However, these funding agencies had no further role in the planning or content of this article.
Footnotes
The author solely managed the literature searches and draft of the manuscript.
The author has no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adrien J. Neurobiological bases for the relation between sleep and depression. Sleep Med Rev. 2002;6:341–351. [PubMed] [Google Scholar]
- Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, Selvi Y. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. Journal of Affective Disorders. 2007;98:267–270. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Lemmi H, Yerevanian B, King D, Belluomini J. The utility of the REM latency test in psychiatric diagnosis: a study of 81 depressed outpatients. Psychiatry Res. 1982;7:101–110. doi: 10.1016/0165-1781(82)90058-0. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Rosenthal TL, Haykal RF, Lemmi H, Rosenthal RH, Scott-Strauss A. Characterological depressions. Clinical and sleep EEG findings separating ‘subaffective dysthymias’ from ‘character spectrum disorders’. Arch Gen Psychiatry. 1980;37:777–783. doi: 10.1001/archpsyc.1980.01780200055006. [DOI] [PubMed] [Google Scholar]
- Alfaro-Rodriguez A, Labra-Ruiz N, Carrasco-Portugal M, Gonzalez-Maciel A, Perez-Guille B, Soriano-Rosales R, Villegas F, Gonzalez-Pina R, Espinoza-Villanueva G, Ayala-Guerrero F. Effect of carbamazepine on sleep patterns disturbed by epilepsy. Proc West Pharmacol Soc. 2002;45:62–64. [PubMed] [Google Scholar]
- Ambrosius U, Lietzenmaier S, Wehrle R, Wichniak A, Kalus S, Winkelmann J, Bettecken T, Holsboer F, Yassouridis A, Friess E. Heritability of sleep electroencephalogram. Biol Psychiatry. 2008;64:344–348. doi: 10.1016/j.biopsych.2008.03.002. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: 1994. [Google Scholar]
- Anderson JL, Rosen LN, Mendelson WB, Jacobsen FM, Skwerer RG, Joseph-Vanderpool JR, Duncan CC, Wehr TA, Rosenthal NE. Sleep in fall/winter seasonal affective disorder: effects of light and changing seasons. J Psychosom Res. 1994;38:323–337. doi: 10.1016/0022-3999(94)90037-x. [DOI] [PubMed] [Google Scholar]
- Andersson JL, Onoe H, Hetta J, Lidstrom K, Valind S, Lilja A, Sundin A, Fasth KJ, Westerberg G, Broman JE, Watanabe Y, Langstrom B. Brain networks affected by synchronized sleep visualized by positron emission tomography. J Cereb Blood Flow Metab. 1998;18:701–715. doi: 10.1097/00004647-199807000-00001. [DOI] [PubMed] [Google Scholar]
- Appelboom-Fondu J, Kerkhofs M, Mendlewicz J. Depression in adolescents and young adults--polysomnographic and neuroendocrine aspects. J Affect Disord. 1988;14:35–40. doi: 10.1016/0165-0327(88)90069-9. [DOI] [PubMed] [Google Scholar]
- Arana-Lechuga Y, Nunez-Ortiz R, Teran-Perez G, Castillo-Montoya C, Jimenez-Anguiano A, Gonzalez-Robles RO, Castro-Roman R, Velazquez-Moctezuma J. Sleep-EEG patterns of school children suffering from symptoms of depression compared to healthy controls. World J Biol Psychiatry. 2008;9:115–120. doi: 10.1080/15622970701216665. [DOI] [PubMed] [Google Scholar]
- Armitage R. Sleep and circadian rhythms in mood disorders. Acta Psychiatr Scand Suppl. 2007:104–115. doi: 10.1111/j.1600-0447.2007.00968.x. [DOI] [PubMed] [Google Scholar]
- Armitage R, Calhoun JS, Rush AJ, Roffwarg HP. Comparison of the delta EEG in the first and second non-REM periods in depressed adults and normal controls. Psychiatry Res. 1992a;41:65–72. doi: 10.1016/0165-1781(92)90019-y. [DOI] [PubMed] [Google Scholar]
- Armitage R, Emslie G, Rintelmann J. The effect of fluoxetine on sleep EEG in childhood depression: a preliminary report. Neuropsychopharmacology. 1997;17:241–245. doi: 10.1016/S0893-133X(97)00048-1. [DOI] [PubMed] [Google Scholar]
- Armitage R, Emslie GJ, Hoffmann RF, Rintelmann J, Rush AJ. Delta sleep EEG in depressed adolescent females and healthy controls. J Affect Disord. 2001;63:139–148. doi: 10.1016/s0165-0327(00)00194-4. [DOI] [PubMed] [Google Scholar]
- Armitage R, Hoffmann R, Emslie G, Rintelmann J, Robert J. Sleep microarchitecture in childhood and adolescent depression: temporal coherence. Clin EEG Neurosci. 2006;37:1–9. doi: 10.1177/155005940603700103. [DOI] [PubMed] [Google Scholar]
- Armitage R, Hoffmann R, Trivedi M, Rush AJ. Slow-wave activity in NREM sleep: sex and age effects in depressed outpatients and healthy controls. Psychiatry Res. 2000;95:201–213. doi: 10.1016/s0165-1781(00)00178-5. [DOI] [PubMed] [Google Scholar]
- Armitage R, Hoffmann RF, Emslie GJ, Weinberg WA, Mayes TL, Rush AJ. Sleep microarchitecture as a predictor of recurrence in children and adolescents with depression. Int J Neuropsychopharmacol. 2002;5:217–228. doi: 10.1017/S1461145702002948. [DOI] [PubMed] [Google Scholar]
- Armitage R, Hoffmann RF, Rush AJ. Biological rhythm disturbance in depression: temporal coherence of ultradian sleep EEG rhythms. Psychol Med. 1999;29:1435–1448. doi: 10.1017/s0033291799001300. [DOI] [PubMed] [Google Scholar]
- Armitage R, Roffwarg HP, Rush AJ, Calhoun JS, Purdy DG, Giles DE. Digital period analysis of sleep EEG in depression. Biol Psychiatry. 1992b;31:52–68. doi: 10.1016/0006-3223(92)90006-l. [DOI] [PubMed] [Google Scholar]
- Barbe RP, Williamson DE, Bridge JA, Birmaher B, Dahl RE, Axelson DA, Ryan ND. Clinical differences between suicidal and nonsuicidal depressed children and adolescents. J Clin Psychiatry. 2005;66:492–498. doi: 10.4088/jcp.v66n0412. [DOI] [PubMed] [Google Scholar]
- Barbini B, Bertelli S, Colombo C, Smeraldi E. Sleep loss, a possible factor in augmenting manic episode. Psychiatry Res. 1996;65:121–125. doi: 10.1016/s0165-1781(96)02909-5. [DOI] [PubMed] [Google Scholar]
- Barbini B, Colombo C, Benedetti F, Campori E, Bellodi L, Smeraldi E. The unipolar-bipolar dichotomy and the response to sleep deprivation. Psychiatry Res. 1998;79:43–50. doi: 10.1016/s0165-1781(98)00020-1. [DOI] [PubMed] [Google Scholar]
- Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiatry. 1992;49:651–668. doi: 10.1001/archpsyc.1992.01820080059010. discussion 669–670. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Smeraldi E. Neuroimaging and genetics of antidepressant response to sleep deprivation: implications for drug development. Curr Pharm Des. 2009;15:2637–2649. doi: 10.2174/138161209788957447. [DOI] [PubMed] [Google Scholar]
- Berger M, Emrich H, Lund R, Riemann D, Lauer CJ, von Zerssen D. Sleep-EEG variables as course criteria and predictors of antidepressant therapy with fluvoxamine/oxaprotiline. In: Stille G, WWWH, editors. Adv Pharmacother. 1986. pp. 110–120. [Google Scholar]
- Bertocci MA, Dahl RE, Williamson DE, Iosif AM, Birmaher B, Axelson D, Ryan ND. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry. 2005;44:1158–1166. doi: 10.1097/01.chi.0000179057.54419.17. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Perel J, Nelson B. Childhood and adolescent depression: a review of the past 10 years. Part I. J Am Acad Child Adolesc Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Bliwise DL. Sleep in normal aging and dementia. Sleep. 1993;16:40–81. doi: 10.1093/sleep/16.1.40. [DOI] [PubMed] [Google Scholar]
- Borbely AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1:195–204. [PubMed] [Google Scholar]
- Borbely AA, Baumann F, Brandeis D, Strauch I, Lehmann D. Sleep deprivation: effect on sleep stages and EEG power density in man. Electroencephalogr Clin Neurophysiol. 1981;51:483–495. doi: 10.1016/0013-4694(81)90225-x. [DOI] [PubMed] [Google Scholar]
- Borbely AA, Tobler I, Loepfe M, Kupfer DJ, Ulrich RF, Grochocinski V, Doman J, Matthews G. All-night spectral analysis of the sleep EEG in untreated depressives and normal controls. Psychiatry Res. 1984;12:27–33. doi: 10.1016/0165-1781(84)90135-5. [DOI] [PubMed] [Google Scholar]
- Borbely AA, Wirz-Justice A. Sleep, sleep deprivation and depression. A hypothesis derived from a model of sleep regulation. Hum Neurobiol. 1982;1:205–210. [PubMed] [Google Scholar]
- Born AP, Law I, Lund TE, Rostrup E, Hanson LG, Wildschiodtz G, Lou HC, Paulson OB. Cortical deactivation induced by visual stimulation in human slow-wave sleep. Neuroimage. 2002;17:1325–1335. doi: 10.1006/nimg.2002.1249. [DOI] [PubMed] [Google Scholar]
- Bourgon LN, Kellner CH. Relapse of depression after ECT: a review. J ECT. 2000;16:19–31. doi: 10.1097/00124509-200003000-00003. [DOI] [PubMed] [Google Scholar]
- Braun AR, Balkin TJ, Wesenten NJ, Carson RE, Varga M, Baldwin P, Selbie S, Belenky G, Herscovitch P. Regional cerebral blood flow throughout the sleep-wake cycle. An H2(15)O PET study. Brain. 1997;120 (Pt 7):1173–1197. doi: 10.1093/brain/120.7.1173. [DOI] [PubMed] [Google Scholar]
- Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- Brunner DP, Krauchi K, Dijk DJ, Leonhardt G, Haug HJ, Wirz-Justice A. Sleep electroencephalogram in seasonal affective disorder and in control women: effects of midday light treatment and sleep deprivation. Biol Psychiatry. 1996;40:485–496. doi: 10.1016/0006-3223(95)00656-7. [DOI] [PubMed] [Google Scholar]
- Brunner DP, Kräuchi K, Leonhardt G, Graw P, Wirz-Justice A. Sleep parameters in SAD: effects of midday light, season, and sleep deprivation. Sleep Res. 1993;22:396. [Google Scholar]
- Buchsbaum MS, Hazlett EA, Wu J, Bunney WE., Jr Positron emission tomography with deoxyglucose-F18 imaging of sleep. Neuropsychopharmacology. 2001;25:S50–56. doi: 10.1016/S0893-133X(01)00339-6. [DOI] [PubMed] [Google Scholar]
- Bunney WE, Bunney BG. Molecular clock genes in man and lower animals: possible implications for circadian abnormalities in depression. Neuropsychopharmacology. 2000;22:335–345. doi: 10.1016/S0893-133X(99)00145-1. [DOI] [PubMed] [Google Scholar]
- Busby K, Pivik RT. Auditory arousal thresholds during sleep in hyperkinetic children. Sleep. 1985;8:332–341. doi: 10.1093/sleep/8.4.332. [DOI] [PubMed] [Google Scholar]
- Busby KA, Mercier L, Pivik RT. Ontogenetic variations in auditory arousal threshold during sleep. Psychophysiology. 1994;31:182–188. doi: 10.1111/j.1469-8986.1994.tb01038.x. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Frank E, Lowe KK, Cherry CR, Kupfer DJ. Electroencephalographic sleep correlates of episode and vulnerability to recurrence in depression. Biol Psychiatry. 1997;41:406–418. doi: 10.1016/S0006-3223(96)00041-8. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Hall M, Begley A, Cherry CR, Houck PR, Land S, Ombao H, Kupfer DJ, Frank E. Sleep and treatment response in depression: new findings using power spectral analysis. Psychiatry Res. 2001;103:51–67. doi: 10.1016/s0165-1781(01)00270-0. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Kupfer DJ, Frank E, Monk TH, Ritenour A. Electroencephalographic sleep studies in depressed outpatients treated with interpersonal psychotherapy: II. Longitudinal studies at baseline and recovery. Psychiatry Res. 1992a;42:27–40. doi: 10.1016/0165-1781(92)90036-3. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Kupfer DJ, Frank E, Monk TH, Ritenour A, Ehlers CL. Electroencephalographic sleep studies in depressed outpatients treated with interpersonal psychotherapy: I. Baseline studies in responders and nonresponders. Psychiatry Res. 1992b;42:13–26. doi: 10.1016/0165-1781(92)90035-2. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Orav EJ, Dement WC. Evolution of sleep and daytime sleepiness in adolescents. In: Lugaresi CGaE., editor. Sleep/Wake Disorders: Natural History, Epidemiology, and Long-Term Evolution. Raven Press; New York: 1983. pp. 201–216. [Google Scholar]
- Cartwright RD. Rapid eye movement sleep characteristics during and after mood-disturbing events. Arch Gen Psychiatry. 1983;40:197–201. doi: 10.1001/archpsyc.1983.01790020095009. [DOI] [PubMed] [Google Scholar]
- Cashman MA, Coble P, McCann S, Taska L, Reynolds CFKDJ. Sleep markers for major depressive disorder in adolescent patients. Vol. 15. 1986. p. 91. [Google Scholar]
- Coble PA, Kupfer DJ, Spiker DG, Neil JF, McPartland RJ. EEG sleep in primary depression. A longitudinal placebo study. J Affect Disord. 1979;1:131–138. doi: 10.1016/0165-0327(79)90032-6. [DOI] [PubMed] [Google Scholar]
- Coble PA, Reynolds CF, 3rd, Kupfer DJ, Houck P. Electroencephalographic sleep of healthy children. Part II: Findings using automated delta and REM sleep measurement methods. Sleep. 1987;10:551–562. [PubMed] [Google Scholar]
- Coffey CE, McCall WV, Hoelscher TJ, Carroll BJ, Hinkle PE, Saunders WB, Erwin CW, Marsh GR, Weiner RD. Effects of ECT on Polysomnographic Sleep: A Prospective Investigation. Convuls Ther. 1988;4:269–279. [PubMed] [Google Scholar]
- Cohrs S, Tergau F, Riech S, Kastner S, Paulus W, Ziemann U, Ruther E, Hajak G. High-frequency repetitive transcranial magnetic stimulation delays rapid eye movement sleep. Neuroreport. 1998;9:3439–3443. doi: 10.1097/00001756-199810260-00019. [DOI] [PubMed] [Google Scholar]
- Colombo C, Lucca A, Benedetti F, Barbini B, Campori E, Smeraldi E. Total sleep deprivation combined with lithium and light therapy in the treatment of bipolar depression: replication of main effects and interaction. Psychiatry Res. 2000;95:43–53. doi: 10.1016/s0165-1781(00)00164-5. [DOI] [PubMed] [Google Scholar]
- Daan S, Beersma DG, Borbely AA. Timing of human sleep: recovery process gated by a circadian pacemaker. Am J Physiol. 1984;246:R161–183. doi: 10.1152/ajpregu.1984.246.2.R161. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Holttum J, Trubnick L. A clinical picture of child and adolescent narcolepsy. J Am Acad Child Adolesc Psychiatry. 1994;33:834–841. doi: 10.1097/00004583-199407000-00009. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Puig-Antich J. Sleep disturbances in child and adolescent psychiatric disorders. Pediatrician. 1990;17:32–37. [PubMed] [Google Scholar]
- Dahl RE, Puig-Antich J, Ryan ND, Nelson B, Dachille S, Cunningham SL, Trubnick L, Klepper TP. EEG sleep in adolescents with major depression: the role of suicidality and inpatient status. J Affect Disord. 1990;19:63–75. doi: 10.1016/0165-0327(90)90010-6. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Ryan ND, Matty MK, Birmaher B, al-Shabbout M, Williamson DE, Kupfer DJ. Sleep onset abnormalities in depressed adolescents. Biol Psychiatry. 1996;39:400–410. doi: 10.1016/0006-3223(95)00190-5. [DOI] [PubMed] [Google Scholar]
- Detrinis R, Harris J, Allen R. Effects of partial sleep deprivation in children with major depression and attention deficit hyperactivity disorder (ADHD) Sleep Res. 1990:19. [Google Scholar]
- Dijk DJ, Brunner DP, Beersma DG, Borbely AA. Electroencephalogram power density and slow wave sleep as a function of prior waking and circadian phase. Sleep. 1990;13:430–440. doi: 10.1093/sleep/13.5.430. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Cajochen C, Tobler I, Borbely AA. Sleep extension in humans: sleep stages, EEG power spectra and body temperature. Sleep. 1991;14:294–306. doi: 10.1093/sleep/14.4.294. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF, Czeisler CA. Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance. J Sleep Res. 1992;1:112–117. doi: 10.1111/j.1365-2869.1992.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Dunleavy DL, Brezinova V, Oswald I, Maclean AW, Tinker M. Changes during weeks in effects of tricyclic drugs on the human sleeping brain. Br J Psychiatry. 1972;120:663–672. doi: 10.1192/bjp.120.559.663. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Kupfer DJ. Hypothalamic peptide modulation of EEG sleep in depression: a further application of the S-process hypothesis. Biol Psychiatry. 1987;22:513–517. doi: 10.1016/0006-3223(87)90173-9. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Armitage R, Weinberg WA, Rush AJ, Mayes TL, Hoffmann RF. Sleep polysomnography as a predictor of recurrence in children and adolescents with major depressive disorder. Int J Neuropsychopharmacol. 2001;4:159–168. doi: 10.1017/S1461145701002383. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Rush AJ, Weinberg WA, Rintelmann JW, Roffwarg HP. Children with major depression show reduced rapid eye movement latencies. Arch Gen Psychiatry. 1990;47:119–124. doi: 10.1001/archpsyc.1990.01810140019003. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Rush AJ, Weinberg WA, Rintelmann JW, Roffwarg HP. Sleep EEG features of adolescents with major depression. Biol Psychiatry. 1994;36:573–581. doi: 10.1016/0006-3223(94)90067-1. [DOI] [PubMed] [Google Scholar]
- Feinberg I. Changes in sleep cycle patterns with age. J Psychiatr Res. 1974;10:283–306. doi: 10.1016/0022-3956(74)90011-9. [DOI] [PubMed] [Google Scholar]
- Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10:473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friess E, Modell S, Brunner H, Tagaya H, Lauer CJ, Holsboer F, Ising M. The Munich vulnerability study on affective disorders: microstructure of sleep in high-risk subjects. Eur Arch Psychiatry Clin Neurosci. 2008;258:285–291. doi: 10.1007/s00406-007-0795-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston KJ, Sharpley AL, Solomon RA, Cowen PJ. Lithium increases slow wave sleep: possible mediation by brain 5-HT2 receptors? Psychopharmacology (Berl) 1989;98:139–140. doi: 10.1007/BF00442020. [DOI] [PubMed] [Google Scholar]
- Fulton MK, Armitage R, Rush AJ. Sleep electroencephalographic coherence abnormalities in individuals at high risk for depression: a pilot study. Biol Psychiatry. 2000;47:618–625. doi: 10.1016/s0006-3223(99)00163-8. [DOI] [PubMed] [Google Scholar]
- Garvey MJ, Mungas D, Tollefson GD. Hypersomnia in major depressive disorders. J Affect Disord. 1984;6:283–286. doi: 10.1016/s0165-0327(84)80006-3. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125–127. doi: 10.1176/appi.ajp.158.1.125. [DOI] [PubMed] [Google Scholar]
- Germain A, Buysse DJ, Wood A, Nofzinger E. Functional neuroanatomical correlates of eye movements during rapid eye movement sleep in depressed patients. Psychiatry Res. 2004;130:259–268. doi: 10.1016/j.pscychresns.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Ages of onset of psychiatric disorders in a community population of older adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33:706–717. doi: 10.1097/00004583-199406000-00012. [DOI] [PubMed] [Google Scholar]
- Giedke H, Klingberg S, Schwarzler F, Schweinsberg M. Direct comparison of total sleep deprivation and late partial sleep deprivation in the treatment of major depression. J Affect Disord. 2003;76:85–93. doi: 10.1016/s0165-0327(02)00071-x. [DOI] [PubMed] [Google Scholar]
- Giedke H, Schwarzler F. Therapeutic use of sleep deprivation in depression. Sleep Med Rev. 2002;6:361–377. [PubMed] [Google Scholar]
- Giles DE, Biggs MM, Rush AJ, Roffwarg HP. Risk factors in families of unipolar depression. I. Psychiatric illness and reduced REM latency. J Affect Disord. 1988;14:51–59. doi: 10.1016/0165-0327(88)90071-7. [DOI] [PubMed] [Google Scholar]
- Giles DE, Etzel BA, Biggs MM. Risk factors in unipolar depression: II. Relation between proband REM latency and cognitions of relatives. Psychiatry Res. 1990;33:39–49. doi: 10.1016/0165-1781(90)90147-w. [DOI] [PubMed] [Google Scholar]
- Giles DE, Jarrett RB, Roffwarg HP, Rush AJ. Reduced rapid eye movement latency. A predictor of recurrence in depression. Neuropsychopharmacology. 1987;1:33–39. doi: 10.1016/0893-133x(87)90007-8. [DOI] [PubMed] [Google Scholar]
- Giles DE, Kupfer DJ. Reduced REM latency: risk factor for first episode of depression. Sleep Res. 1994;23:197. [Google Scholar]
- Giles DE, Kupfer DJ, Rush AJ, Roffwarg HP. Controlled comparison of electrophysiological sleep in families of probands with unipolar depression. Am J Psychiatry. 1998a;155:192–199. doi: 10.1176/ajp.155.2.192. [DOI] [PubMed] [Google Scholar]
- Giles DE, Perlis ML, Reynolds CF, 3rd, Kupfer DJ. EEG sleep in African-American patients with major depression: a historical case control study. Depress Anxiety. 1998b;8:58–64. [PubMed] [Google Scholar]
- Giles DE, Roffwarg HP, Dahl RE, Kupfer DJ. Electroencephalographic sleep abnormalities in depressed children: a hypothesis. Psychiatry Res. 1992;41:53–63. doi: 10.1016/0165-1781(92)90018-x. [DOI] [PubMed] [Google Scholar]
- Giles DE, Roffwarg HP, Schlesser MA, Rush AJ. Which endogenous depressive symptoms relate to REM latency reduction? Biol Psychiatry. 1986a;21:473–482. doi: 10.1016/0006-3223(86)90189-7. [DOI] [PubMed] [Google Scholar]
- Giles DE, Rush AJ, Roffwarg HP. Sleep parameters in bipolar I, bipolar II, and unipolar depressions. Biol Psychiatry. 1986b;21:1340–1343. doi: 10.1016/0006-3223(86)90319-7. [DOI] [PubMed] [Google Scholar]
- Gillin JC, Buchsbaum M, Wu J, Clark C, Bunney W., Jr Sleep deprivation as a model experimental antidepressant treatment: findings from functional brain imaging. Depress Anxiety. 2001;14:37–49. doi: 10.1002/da.1045. [DOI] [PubMed] [Google Scholar]
- Gillin JC, Wyatt RJ, Fram D, Snyder F. The relationship between changes in REM sleep and clinical improvement in depressed patients treated with amitriptyline. Psychopharmacology (Berl) 1978;59:267–272. doi: 10.1007/BF00426633. [DOI] [PubMed] [Google Scholar]
- Goetz RR, Puig-Antich J, Ryan N, Rabinovich H, Ambrosini PJ, Nelson B, Krawiec V. Electroencephalographic sleep of adolescents with major depression and normal controls. Arch Gen Psychiatry. 1987;44:61–68. doi: 10.1001/archpsyc.1987.01800130069009. [DOI] [PubMed] [Google Scholar]
- Goetz RR, Wolk SI, Coplan JD, Ryan ND, Weissman MM. Premorbid polysomnographic signs in depressed adolescents: a reanalysis of EEG sleep after longitudinal follow-up in adulthood. Biol Psychiatry. 2001;49:930–942. doi: 10.1016/s0006-3223(00)01092-1. [DOI] [PubMed] [Google Scholar]
- Goldenberg F. Other medications used for insomnia. In: MB, editor. Le sommeil normal et pathologique. Masson, Paris: 1994. pp. 269–281. [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–645. doi: 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Rijsdijk FV, Lau JY, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32:189–199. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grozinger M, Kogel P, Roschke J. Effects of REM sleep awakenings and related wakening paradigms on the ultradian sleep cycle and the symptoms in depression. J Psychiatr Res. 2002;36:299–308. doi: 10.1016/s0022-3956(02)00022-5. [DOI] [PubMed] [Google Scholar]
- Grunhaus L, Shipley JE, Eiser A, Pande AC, Tandon R, Krahn DD, Demitrack MA, Remen A, Hirschmann S, Greden JF. Sleep-onset rapid eye movement after electroconvulsive therapy is more frequent in patients who respond less well to electroconvulsive therapy. Biol Psychiatry. 1997;42:191–200. doi: 10.1016/S0006-3223(96)00333-2. [DOI] [PubMed] [Google Scholar]
- Grunhaus L, Shipley JE, Eiser A, Pande AC, Tandon R, Remen A, Greden JF. Shortened REM latency PostECT is associated with rapid recurrence of depressive symptomatology. Biol Psychiatry. 1994;36:214–222. doi: 10.1016/0006-3223(94)90602-5. [DOI] [PubMed] [Google Scholar]
- Grunhaus L, Tiongco D, Pande A, Eiser A, Haskett RF, Greden JF, Shipley JE. Monitoring of antidepressant response to ECT with polysomnographic recordings and the dexamethasone suppression test. Psychiatry Res. 1988;24:177–185. doi: 10.1016/0165-1781(88)90060-1. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Harding GF, Alford CA, Powell TE. The effect of sodium valproate on sleep, reaction times, and visual evoked potential in normal subjects. Epilepsia. 1985;26:597–601. doi: 10.1111/j.1528-1157.1985.tb05698.x. [DOI] [PubMed] [Google Scholar]
- Hawkins DR, Taub JM, Van de Castle RL. Extended sleep (hypersomnia) in young depressed patients. Am J Psychiatry. 1985;142:905–910. doi: 10.1176/ajp.142.8.905. [DOI] [PubMed] [Google Scholar]
- Ho AP, Gillin JC, Buchsbaum MS, Wu JC, Abel L, Bunney WE., Jr Brain glucose metabolism during non-rapid eye movement sleep in major depression. A positron emission tomography study. Arch Gen Psychiatry. 1996;53:645–652. doi: 10.1001/archpsyc.1996.01830070095014. [DOI] [PubMed] [Google Scholar]
- Hobson JA, McCarley RW, Wyzinski PW. Sleep cycle oscillation: reciprocal discharge by two brainstem neuronal groups. Science. 1975;189:55–58. doi: 10.1126/science.1094539. [DOI] [PubMed] [Google Scholar]
- Hochli D, Riemann D, Zulley J, Berger M. Initial REM sleep suppression by clomipramine: a prognostic tool for treatment response in patients with a major depressive disorder. Biol Psychiatry. 1986;21:1217–1220. doi: 10.1016/0006-3223(86)90227-1. [DOI] [PubMed] [Google Scholar]
- Hofle N, Paus T, Reutens D, Fiset P, Gotman J, Evans AC, Jones BE. Regional cerebral blood flow changes as a function of delta and spindle activity during slow wave sleep in humans. J Neurosci. 1997;17:4800–4808. doi: 10.1523/JNEUROSCI.17-12-04800.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanenko A, Crabtree VM, Gozal D. Sleep and depression in children and adolescents. Sleep Med Rev. 2005;9:115–129. doi: 10.1016/j.smrv.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Jarrett DB, Miewald JM, Kupfer DJ. Recurrent depression is associated with a persistent reduction in sleep-related growth hormone secretion. Arch Gen Psychiatry. 1990a;47:113–118. doi: 10.1001/archpsyc.1990.01810140013002. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Rush AJ, Khatami M, Roffwarg HP. Does the pretreatment polysomnogram predict response to cognitive therapy in depressed outpatients? A preliminary report. Psychiatry Res. 1990b;33:285–299. doi: 10.1016/0165-1781(90)90045-7. [DOI] [PubMed] [Google Scholar]
- Jones CR, Campbell SS, Zone SE, Cooper F, DeSano A, Murphy PJ, Jones B, Czajkowski L, Ptacek LJ. Familial advanced sleep-phase syndrome: A short-period circadian rhythm variant in humans. Nat Med. 1999;5:1062–1065. doi: 10.1038/12502. [DOI] [PubMed] [Google Scholar]
- Katzenberg D, Young T, Finn L, Lin L, King DP, Takahashi JS, Mignot E. A CLOCK polymorphism associated with human diurnal preference. Sleep. 1998;21:569–576. doi: 10.1093/sleep/21.6.569. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Martin A, King RA, Charney D. Are child-, adolescent-, and adult-onset depression one and the same disorder? Biol Psychiatry. 2001;49:980–1001. doi: 10.1016/s0006-3223(01)01127-1. [DOI] [PubMed] [Google Scholar]
- Kerkhofs M, Kempenaers C, Linkowski P, de Maertelaer V, Mendlewicz J. Multivariate study of sleep EEG in depression. Acta Psychiatr Scand. 1988;77:463–468. doi: 10.1111/j.1600-0447.1988.tb05152.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Andrade L, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Merikangas KR, Molnar BE, Vega WA, Walters EE, Wittchen HU, Ustun TB. Mental-substance comorbidities in the ICPE surveys. Psychiatria Fennica. 2001;32 (suppl 2):62–80. [Google Scholar]
- Kimura M, Winkelmann J. Genetics of sleep and sleep disorders. Cell Mol Life Sci. 2007;64:1216–1226. doi: 10.1007/s00018-007-6532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BH, Baxter LR, Jr, Stuber M, Fish B. Therapeutic sleep deprivation for depression in children. J Am Acad Child Adolesc Psychiatry. 1987;26:928–931. doi: 10.1097/00004583-198726060-00020. [DOI] [PubMed] [Google Scholar]
- Knowles JB, MacLean AW. Age-related changes in sleep in depressed and healthy subjects. A meta-analysis. Neuropsychopharmacology. 1990;3:251–259. [PubMed] [Google Scholar]
- Kupfer DJ, Coble P, Kane J, Petti T, Conners CK. Imipramine and EEG sleep in children with depressive symptoms. Psychopharmacology (Berl) 1979;60:117–123. doi: 10.1007/BF00432281. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Ehlers CL. Two roads to rapid eye movement latency. Arch Gen Psychiatry. 1989;46:945–948. doi: 10.1001/archpsyc.1989.01810100087016. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Ehlers CL, Frank E, Grochocinski VJ, McEachran AB, Buhari A. Persistent effects of antidepressants: EEG sleep studies in depressed patients during maintenance treatment. Biol Psychiatry. 1994;35:781–793. doi: 10.1016/0006-3223(94)91140-1. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Foster FG. Interval between onset of sleep and rapid-eye-movement sleep as an indicator of depression. Lancet. 1972;2:684–686. doi: 10.1016/s0140-6736(72)92090-9. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, McEachran AB, Grochocinski VJ. Delta sleep ratio. A biological correlate of early recurrence in unipolar affective disorder. Arch Gen Psychiatry. 1990;47:1100–1105. doi: 10.1001/archpsyc.1990.01810240020004. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Himmelhoch JM, Swartzburg M, Anderson C, Byck R, Detre TP. Hypersomnia in manic-depressive disease (a preliminary report) Dis Nerv Syst. 1972;33:720–724. [PubMed] [Google Scholar]
- Kupfer DJ, Reynolds CF, 3rd, Grochocinski VJ, Ulrich RF, McEachran A. Aspects of short REM latency in affective states: a revisit. Psychiatry Res. 1986;17:49–59. doi: 10.1016/0165-1781(86)90041-7. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry. 1981;138:429–434. doi: 10.1176/ajp.138.4.429. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Ulrich RF, Coble PA, Jarrett DB, Grochocinski V, Doman J, Matthews G, Borbely AA. Application of automated REM and slow wave sleep analysis: II. Testing the assumptions of the two-process model of sleep regulation in normal and depressed subjects. Psychiatry Res. 1984;13:335–343. doi: 10.1016/0165-1781(84)90081-7. [DOI] [PubMed] [Google Scholar]
- Kutcher S, Williamson P, Marton P, Szalai J. REM latency in endogenously depressed adolescents. Br J Psychiatry. 1992;161:399–402. doi: 10.1192/bjp.161.3.399. [DOI] [PubMed] [Google Scholar]
- Lahmeyer HW, Poznanski EO, Bellur SN. EEG sleep in depressed adolescents. Am J Psychiatry. 1983;140:1150–1153. doi: 10.1176/ajp.140.9.1150. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Modell S, Schreiber W, Krieg JC, Holsboer F. Prediction of the development of a first major depressive episode with a rapid eye movement sleep induction test using the cholinergic agonist RS 86. J Clin Psychopharmacol. 2004;24:356–357. doi: 10.1097/01.jcp.0000125744.22031.3a. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Riemann D, Wiegand M, Berger M. From early to late adulthood. Changes in EEG sleep of depressed patients and healthy volunteers. Biol Psychiatry. 1991;29:979–993. doi: 10.1016/0006-3223(91)90355-p. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Schreiber W, Holsboer F, Krieg JC. In quest of identifying vulnerability markers for psychiatric disorders by all-night polysomnography. Arch Gen Psychiatry. 1995;52:145–153. doi: 10.1001/archpsyc.1995.03950140063009. [DOI] [PubMed] [Google Scholar]
- Laureys S, Peigneux P, Phillips C, Fuchs S, Degueldre C, Aerts J, Del Fiore G, Petiau C, Luxen A, van der Linden M, Cleeremans A, Smith C, Maquet P. Experience-dependent changes in cerebral functional connectivity during human rapid eye movement sleep. Neuroscience. 2001;105:521–525. doi: 10.1016/s0306-4522(01)00269-x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Essau CA. Depression in adolescents. In: Gotlib IH, Hammen CL, editors. Handbook of depression. Guilford Press; New York: 2002. pp. 541–559. [Google Scholar]
- Liscombe MP, Hoffmann RF, Trivedi MH, Parker MK, Rush AJ, Armitage R. Quantitative EEG amplitude across REM sleep periods in depression: preliminary report. J Psychiatry Neurosci. 2002;27:40–46. [PMC free article] [PubMed] [Google Scholar]
- Liu X, Buysse DJ, Gentzler AL, Kiss E, Mayer L, Kapornai K, Vetro A, Kovacs M. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep. 2007;30:83–90. doi: 10.1093/sleep/30.1.83. [DOI] [PubMed] [Google Scholar]
- Lofthouse N, Gilchrist R, Splaingard M. Mood-related Sleep Problems in Children and Adolescents. Child and Adolescent Psychiatric Clinics of North America. 2009;18:893–916. doi: 10.1016/j.chc.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Maquet P, Degueldre C, Delfiore G, Aerts J, Peters JM, Luxen A, Franck G. Functional neuroanatomy of human slow wave sleep. J Neurosci. 1997;17:2807–2812. doi: 10.1523/JNEUROSCI.17-08-02807.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maquet P, Dive D, Salmon E, Sadzot B, Franco G, Poirrier R, von Frenckell R, Franck G. Cerebral glucose utilization during sleep-wake cycle in man determined by positron emission tomography and [18F]2-fluoro-2-deoxy-D-glucose method. Brain Res. 1990;513:136–143. doi: 10.1016/0006-8993(90)91099-3. [DOI] [PubMed] [Google Scholar]
- Maquet P, Laureys S, Peigneux P, Fuchs S, Petiau C, Phillips C, Aerts J, Del Fiore G, Degueldre C, Meulemans T, Luxen A, Franck G, Van Der Linden M, Smith C, Cleeremans A. Experience-dependent changes in cerebral activation during human REM sleep. Nat Neurosci. 2000;3:831–836. doi: 10.1038/77744. [DOI] [PubMed] [Google Scholar]
- Maquet P, Peters J, Aerts J, Delfiore G, Degueldre C, Luxen A, Franck G. Functional neuroanatomy of human rapid-eye-movement sleep and dreaming. Nature. 1996;383:163–166. doi: 10.1038/383163a0. [DOI] [PubMed] [Google Scholar]
- Masi G, Millepiedi S, Mucci M, Pascale RR, Perugi G, Akiskal HS. Phenomenology and comorbidity of dysthymic disorder in 100 consecutively referred children and adolescents: beyond DSM-IV. Can J Psychiatry. 2003;48:99–105. doi: 10.1177/070674370304800206. [DOI] [PubMed] [Google Scholar]
- Mayers AG, Baldwin DS. Antidepressants and their effect on sleep. Hum Psychopharmacol. 2005;20:533–559. doi: 10.1002/hup.726. [DOI] [PubMed] [Google Scholar]
- McCall WV, Reboussin BA, Cohen W. Subjective measurement of insomnia and quality of life in depressed inpatients. J Sleep Res. 2000;9:43–48. doi: 10.1046/j.1365-2869.2000.00186.x. [DOI] [PubMed] [Google Scholar]
- McCarley RW. REM sleep and depression: common neurobiological control mechanisms. Am J Psychiatry. 1982;139:565–570. doi: 10.1176/ajp.139.5.565. [DOI] [PubMed] [Google Scholar]
- McCarley RW. Neurobiology of REM and NREM sleep. Sleep Med. 2007;8:302–330. doi: 10.1016/j.sleep.2007.03.005. [DOI] [PubMed] [Google Scholar]
- McCracken JT, Poland RE, Lutchmansingh P, Edwards C. Sleep electroencephalographic abnormalities in adolescent depressives: effects of scopolamine. Biol Psychiatry. 1997;42:577–584. doi: 10.1016/S0006-3223(96)00431-3. [DOI] [PubMed] [Google Scholar]
- Mendlewicz J. Disruption of the circadian timing systems: molecular mechanisms in mood disorders. CNS Drugs. 2009;23(Suppl 2):15–26. doi: 10.2165/11318630-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Meyer JS, Hayman LA, Amano T, Nakajima S, Shaw T, Lauzon P, Derman S, Karacan I, Harati Y. Mapping local blood flow of human brain by CT scanning during stable xenon inhalation. Stroke. 1981;12:426–436. doi: 10.1161/01.str.12.4.426. [DOI] [PubMed] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Strollo PJ, Jr, Buysse DJ, Kamarck TW, Owens JF, Reis SE. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008;70:410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles LE, Dement WC. Sleep and aging. Sleep. 1980;3:1–220. [PubMed] [Google Scholar]
- Modell S, Ising M, Holsboer F, Lauer CJ. The Munich vulnerability study on affective disorders: premorbid polysomnographic profile of affected high-risk probands. Biol Psychiatry. 2005;58:694–699. doi: 10.1016/j.biopsych.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Monteleone P, Maj M. The circadian basis of mood disorders: recent developments and treatment implications. Eur Neuropsychopharmacol. 2008;18:701–711. doi: 10.1016/j.euroneuro.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Morehouse RL, Kusumakar V, Kutcher SP, LeBlanc J, Armitage R. Temporal coherence in ultradian sleep EEG rhythms in a never-depressed, high-risk cohort of female adolescents. Biol Psychiatry. 2002;51:446–456. doi: 10.1016/s0006-3223(01)01297-5. [DOI] [PubMed] [Google Scholar]
- Naylor MW, King CA, Lindsay KA, Evans T, Armelagos J, Shain BN, Greden JF. Sleep deprivation in depressed adolescents and psychiatric controls. J Am Acad Child Adolesc Psychiatry. 1993;32:753–759. doi: 10.1097/00004583-199307000-00008. [DOI] [PubMed] [Google Scholar]
- Naylor MW, Shain BN, Shipley JE. REM latency in psychotically depressed adolescents. Biol Psychiatry. 1990;28:161–164. doi: 10.1016/0006-3223(90)90633-d. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA. Functional neuroimaging of sleep. Semin Neurol. 2005;25:9–18. doi: 10.1055/s-2005-867070. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA, Buysse DJ, Germain A, Carter C, Luna B, Price JC, Meltzer CC, Miewald JM, Reynolds CF, 3rd, Kupfer DJ. Increased activation of anterior paralimbic and executive cortex from waking to rapid eye movement sleep in depression. Arch Gen Psychiatry. 2004;61:695–702. doi: 10.1001/archpsyc.61.7.695. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA, Mintun MA, Wiseman M, Kupfer DJ, Moore RY. Forebrain activation in REM sleep: an FDG PET study. Brain Res. 1997;770:192–201. doi: 10.1016/s0006-8993(97)00807-x. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA, Price JC, Meltzer CC, Buysse DJ, Villemagne VL, Miewald JM, Sembrat RC, Steppe DA, Kupfer DJ. Towards a neurobiology of dysfunctional arousal in depression: the relationship between beta EEG power and regional cerebral glucose metabolism during NREM sleep. Psychiatry Res. 2000;98:71–91. doi: 10.1016/s0925-4927(00)00045-7. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA, Reynolds CF, 3rd, Thase ME, Frank E, Jennings JR, Fasiczka AL, Sullivan LR, Kupfer DJ. REM sleep enhancement by bupropion in depressed men. Am J Psychiatry. 1995;152:274–276. doi: 10.1176/ajp.152.2.274. [DOI] [PubMed] [Google Scholar]
- Ong SH, Wickramaratne P, Tang M, Weissman MM. Early childhood sleep and eating problems as predictors of adolescent and adult mood and anxiety disorders. J Affect Disord. 2006;96:1–8. doi: 10.1016/j.jad.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Ott GE, Rao U, Nuccio I, Lin KM, Poland RE. Effect of bupropion-SR on REM sleep: relationship to antidepressant response. Psychopharmacology (Berl) 2002;165:29–36. doi: 10.1007/s00213-002-1165-4. [DOI] [PubMed] [Google Scholar]
- Parker G, Malhi G, Hadzi-Pavlovic D, Parker K. Sleeping in? The impact of age and depressive sub-type on hypersomnia. J Affect Disord. 2006;90:73–76. doi: 10.1016/j.jad.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Partonen T, Appelberg B, Partinen M. Effects of light treatment on sleep structure in seasonal affective disorder. Eur Arch Psychiatry Clin Neurosci. 1993;242:310–313. doi: 10.1007/BF02190391. [DOI] [PubMed] [Google Scholar]
- Paus T, Koski L, Caramanos Z, Westbury C. Regional differences in the effects of task difficulty and motor output on blood flow response in the human anterior cingulate cortex: a review of 107 PET activation studies. Neuroreport. 1998;9:R37–47. doi: 10.1097/00001756-199806220-00001. [DOI] [PubMed] [Google Scholar]
- Pflug B, Tolle R. Therapy of endogenous depressions using sleep deprivation. Practical and theoretical consequences. Nervenarzt. 1971;42:117–124. [PubMed] [Google Scholar]
- Placidi F, Diomedi M, Scalise A, Marciani MG, Romigi A, Gigli GL. Effect of anticonvulsants on nocturnal sleep in epilepsy. Neurology. 2000;54:S25–32. [PubMed] [Google Scholar]
- Poland RE, Rao U, Lutchmansingh P, McCracken JT, Lesser IM, Edwards C, Ott GE, Lin KM. REM sleep in depression is influenced by ethnicity. Psychiatry Res. 1999;88:95–105. doi: 10.1016/s0165-1781(99)00080-3. [DOI] [PubMed] [Google Scholar]
- Profant J, Ancoli-Israel S, Dimsdale JE. Are there ethnic differences in sleep architecture? Am J Hum Biol. 2002;14:321–326. doi: 10.1002/ajhb.10032. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Goetz R, Hanlon C, Davies M, Thompson J, Chambers WJ, Tabrizi MA, Weitzman ED. Sleep architecture and REM sleep measures in prepubertal children with major depression: a controlled study. Arch Gen Psychiatry. 1982;39:932–939. doi: 10.1001/archpsyc.1982.04290080046007. [DOI] [PubMed] [Google Scholar]
- Rao U, Chen LA. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin Neurosci. 2009;11:45–62. doi: 10.31887/DCNS.2009.11.1/urao. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Dahl RE, Ryan ND, Birmaher B, Williamson DE, Giles DE, Rao R, Kaufman J, Nelson B. The relationship between longitudinal clinical course and sleep and cortisol changes in adolescent depression. Biol Psychiatry. 1996;40:474–484. doi: 10.1016/0006-3223(95)00481-5. [DOI] [PubMed] [Google Scholar]
- Rao U, Dahl RE, Ryan ND, Birmaher B, Williamson DE, Rao R, Kaufman J. Heterogeneity in EEG sleep findings in adolescent depression: unipolar versus bipolar clinical course. J Affect Disord. 2002;70:273–280. doi: 10.1016/s0165-0327(01)00396-2. [DOI] [PubMed] [Google Scholar]
- Rao U, Hammen CL, Poland RE. Ethnic differences in electroencephalographic sleep patterns in adolescents. Asian J Psychiatry. 2009a;2:17–24. doi: 10.1016/j.ajp.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Hammen CL, Poland RE. Risk markers for depression in adolescents: sleep and HPA measures. Neuropsychopharmacology. 2009b;34:1936–1945. doi: 10.1038/npp.2009.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, McCracken JT, Lutchmansingh P, Edwards C, Poland RE. Electroencephalographic sleep and urinary free cortisol in adolescent depression: a preliminary report of changes from episode to recovery. Biol Psychiatry. 1997;41:369–373. doi: 10.1016/s0006-3223(96)00430-1. [DOI] [PubMed] [Google Scholar]
- Rao U, Poland RE. EEG sleep and HPA changes from episode to recovery in depressed adolescents. Journal of Child and Adolescent Psychopharmacology. 2008;18:607–613. doi: 10.1089/cap.2008.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Poland RE, Lutchmansingh P, Ott GE, McCracken JT, Lin KM. Relationship between ethnicity and sleep patterns in normal controls: implications for psychopathology and treatment. J Psychiatr Res. 1999a;33:419–426. doi: 10.1016/s0022-3956(99)00019-9. [DOI] [PubMed] [Google Scholar]
- Rao U, Ryan ND, Dahl RE, Birmaher B, Rao R, Williamson DE, Perel JM. Factors associated with the development of substance use disorder in depressed adolescents. J Am Acad Child Adolesc Psychiatry. 1999b;38:1109–1117. doi: 10.1097/00004583-199909000-00014. [DOI] [PubMed] [Google Scholar]
- Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–418. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- Reynolds CF., 3rd What do antidepressant effects on sleep tell us about pathways to treatment response? Biol Psychiatry. 1998;44:1–2. doi: 10.1016/s0006-3223(98)00129-2. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Hoch CC, Buysse DJ, George CJ, Houck PR, Mazumdar S, Miller M, Pollock BG, Rifai H, Frank E, et al. Sleep in late-life recurrent depression. Changes during early continuation therapy with nortriptyline. Neuropsychopharmacology. 1991;5:85–96. [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Kupfer DJ. Sleep research in affective illness: state of the art circa 1987. Sleep. 1987;10:199–215. doi: 10.1093/sleep/10.3.199. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Kupfer DJ, Thase ME, Frank E, Jarrett DB, Coble PA, Hoch CC, Buysse DJ, Simons AD, Houck PR. Sleep, gender, and depression: an analysis of gender effects on the electroencephalographic sleep of 302 depressed outpatients. Biol Psychiatry. 1990;28:673–684. doi: 10.1016/0006-3223(90)90454-a. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Perel JM, Frank E, Imber S, Kupfer DJ. Open-trial maintenance nortriptyline in geriatric depression: survival analysis and preliminary data on the use of REM latency as a predictor of recurrence. Psychopharmacol Bull. 1989;25:129–132. [PubMed] [Google Scholar]
- Riemann D, Berger M. Sleep, age, depression and the cholinergic REM induction test with RS 86. Prog Neuropsychopharmacol Biol Psychiatry. 1992;16:311–316. doi: 10.1016/0278-5846(92)90082-p. [DOI] [PubMed] [Google Scholar]
- Riemann D, Berger M, Voderholzer U. Sleep and depression--results from psychobiological studies: an overview. Biol Psychol. 2001;57:67–103. doi: 10.1016/s0301-0511(01)00090-4. [DOI] [PubMed] [Google Scholar]
- Riemann D, Gann H, Dressing H, Muller WE, Aldenhoff JB. Influence of the cholinesterase inhibitor galanthamine hydrobromide on normal sleep. Psychiatry Res. 1994a;51:253–267. doi: 10.1016/0165-1781(94)90013-2. [DOI] [PubMed] [Google Scholar]
- Riemann D, Hohagen F, Bahro M, Berger M. Sleep in depression: the influence of age, gender and diagnostic subtype on baseline sleep and the cholinergic REM induction test with RS 86. Eur Arch Psychiatry Clin Neurosci. 1994b;243:279–290. doi: 10.1007/BF02191586. [DOI] [PubMed] [Google Scholar]
- Riemann D, Kammerer J, Low H, Schmidt MH. Sleep in adolescents with primary major depression and schizophrenia: a pilot study. J Child Psychol Psychiatry. 1995;36:313–326. doi: 10.1111/j.1469-7610.1995.tb01827.x. [DOI] [PubMed] [Google Scholar]
- Riemann D, Velthaus S, Laubenthal S, Muller WE, Berger M. REM-suppressing effects of amitriptyline and amitriptyline-N-oxide after acute medication in healthy volunteers: results of two uncontrolled pilot trials. Pharmacopsychiatry. 1990;23:253–258. doi: 10.1055/s-2007-1014515. [DOI] [PubMed] [Google Scholar]
- Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord. 2003;76:255–259. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–1356. [PMC free article] [PubMed] [Google Scholar]
- Robert JJ, Hoffmann RF, Emslie GJ, Hughes C, Rintelmann J, Moore J, Armitage R. Sex and age differences in sleep macroarchitecture in childhood and adolescent depression. Sleep. 2006;29:351–358. doi: 10.1093/sleep/29.3.351. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Symptoms of DSM-III-R major depression in adolescence: evidence from an epidemiological survey. J Am Acad Child Adolesc Psychiatry. 1995;34:1608–1617. doi: 10.1097/00004583-199512000-00011. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Ramsay Roberts C, Ger Chen I. Impact of insomnia on future functioning of adolescents. Journal of Psychosomatic Research. 2002;53:561–569. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Skwerer RG, Levendosky BA, Joseph-Vanderpool JR, Jacobsen FM, Duncan CC, Gaist PA, Wehr TA. Sleep architecture in seasonal affective disorder: the effects of light therapy and changing seasons. Sleep Res. 1989:18. [Google Scholar]
- Rush AJ, Giles DE, Jarrett RB, Feldman-Koffler F, Debus JR, Weissenburger J, Orsulak PJ, Roffwarg HP. Reduced REM latency predicts response to tricyclic medication in depressed outpatients. Biol Psychiatry. 1989;26:61–72. doi: 10.1016/0006-3223(89)90008-5. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Giles DE, Roffwarg HP, Parker CR. Sleep EEG and dexamethasone suppression test findings in outpatients with unipolar major depressive disorders. Biol Psychiatry. 1982;17:327–341. [PubMed] [Google Scholar]
- Sandor P, Shapiro CM. Sleep patterns in depression and anxiety: theory and pharmacological effects. J Psychosom Res. 1994;38(Suppl 1):125–139. doi: 10.1016/0022-3999(94)90143-0. [DOI] [PubMed] [Google Scholar]
- Sangoram AM, Saez L, Antoch MP, Gekakis N, Staknis D, Whiteley A, Fruechte EM, Vitaterna MH, Shimomura K, King DP, Young MW, Weitz CJ, Takahashi JS. Mammalian circadian autoregulatory loop: a timeless ortholog and mPer1 interact and negatively regulate CLOCK-BMAL1-induced transcription. Neuron. 1998;21:1101–1113. doi: 10.1016/s0896-6273(00)80627-3. [DOI] [PubMed] [Google Scholar]
- Schilgen B, Bischofs W, Blaszkiewicz F, Bremer W, Rudolf GA, Tolle R. Total and partial sleep deprivation in the treatment of depression: preliminary communication. Arzneimittelforschung. 1976;26:1171–1173. [PubMed] [Google Scholar]
- Schreiber W, Lauer CJ, Krumrey K, Holsboer F, Krieg JC. Cholinergic REM sleep induction test in subjects at high risk for psychiatric disorders. Biol Psychiatry. 1992;32:79–90. doi: 10.1016/0006-3223(92)90144-o. [DOI] [PubMed] [Google Scholar]
- Serretti A, Benedetti F, Mandelli L, Lorenzi C, Pirovano A, Colombo C, Smeraldi E. Genetic dissection of psychopathological symptoms: insomnia in mood disorders and CLOCK gene polymorphism. Am J Med Genet B Neuropsychiatr Genet. 2003;121B:35–38. doi: 10.1002/ajmg.b.20053. [DOI] [PubMed] [Google Scholar]
- Shain BN, Naylor M, Shipley JE, Alessi N. Imipramine effects on sleep in depressed adolescents: a preliminary report. Biol Psychiatry. 1990;28:459–462. doi: 10.1016/0006-3223(90)90414-w. [DOI] [PubMed] [Google Scholar]
- Sharpley AL, Cowen PJ. Effect of pharmacologic treatments on the sleep of depressed patients. Biol Psychiatry. 1995;37:85–98. doi: 10.1016/0006-3223(94)00135-P. [DOI] [PubMed] [Google Scholar]
- Sharpley AL, Walsh AE, Cowen PJ. Nefazodone--a novel antidepressant--may increase REM sleep. Biol Psychiatry. 1992;31:1070–1073. doi: 10.1016/0006-3223(92)90101-5. [DOI] [PubMed] [Google Scholar]
- Sitaram N, Dube S, Keshavan M, Davies A, Reynal P. The association of supersensitive cholinergic REM-induction and affective illness within pedigrees. J Psychiatr Res. 1987;21:487–497. doi: 10.1016/0022-3956(87)90097-5. [DOI] [PubMed] [Google Scholar]
- Smeraldi E, Benedetti F, Barbini B, Campori E, Colombo C. Sustained antidepressant effect of sleep deprivation combined with pindolol in bipolar depression. A placebo-controlled trial. Neuropsychopharmacology. 1999;20:380–385. doi: 10.1016/S0893-133X(98)00129-8. [DOI] [PubMed] [Google Scholar]
- Soria V, Urretavizcaya M. Circadian rhythms and depression. Actas Esp Psiquiatr. 2009;37:222–232. [PubMed] [Google Scholar]
- Steiger A. Sleep and the hypothalamo-pituitary-adrenocortical system. Sleep Med Rev. 2002;6:125–138. doi: 10.1053/smrv.2001.0159. [DOI] [PubMed] [Google Scholar]
- Steiger A. Sleep and endocrine regulation. Front Biosci. 2003;8:s358–376. doi: 10.2741/1055. [DOI] [PubMed] [Google Scholar]
- Steiger A, Benkert O, Holsboer F. Effects of long-term treatment with the MAO-A inhibitor moclobemide on sleep EEG and nocturnal hormonal secretion in normal men. Neuropsychobiology. 1994;30:101–105. doi: 10.1159/000119145. [DOI] [PubMed] [Google Scholar]
- Stepnowsky CJ, Jr, Moore PJ, Dimsdale JE. Effect of ethnicity on sleep: complexities for epidemiologic research. Sleep. 2003;26:329–332. doi: 10.1093/sleep/26.3.329. [DOI] [PubMed] [Google Scholar]
- Svendsen K, Christensen PG. Duration of REM sleep latency as predictor of effect of antidepressant therapy. A preliminary report. Acta Psychiatr Scand. 1981;64:238–243. doi: 10.1111/j.1600-0447.1981.tb00779.x. [DOI] [PubMed] [Google Scholar]
- Svestka J. Sleep deprivation therapy. Neuro Endocrinol Lett. 2008;29(Suppl 1):65–92. [PubMed] [Google Scholar]
- Thase ME, Buysse DJ, Frank E, Cherry CR, Cornes CL, Mallinger AG, Kupfer DJ. Which depressed patients will respond to interpersonal psychotherapy? The role of abnormal EEG sleep profiles. Am J Psychiatry. 1997;154:502–509. doi: 10.1176/ajp.154.4.502. [DOI] [PubMed] [Google Scholar]
- Thase ME, Fasiczka AL, Berman SR, Simons AD, Reynolds CF., 3rd Electroencephalographic sleep profiles before and after cognitive behavior therapy of depression. Arch Gen Psychiatry. 1998;55:138–144. doi: 10.1001/archpsyc.55.2.138. [DOI] [PubMed] [Google Scholar]
- Thase ME, Himmelhoch JM, Mallinger AG, Jarrett DB, Kupfer DJ. Sleep EEG and DST findings in anergic bipolar depression. Am J Psychiatry. 1989;146:329–333. doi: 10.1176/ajp.146.3.329. [DOI] [PubMed] [Google Scholar]
- Thase ME, Kupfer DJ, Ulrich RF. Electroencephalographic sleep in psychotic depression. A valid subtype? Arch Gen Psychiatry. 1986;43:886–893. doi: 10.1001/archpsyc.1986.01800090076010. [DOI] [PubMed] [Google Scholar]
- Thomas M, Sing H, Belenky G, Holcomb H, Mayberg H, Dannals R, Wagner H, Thorne D, Popp K, Rowland L, Welsh A, Balwinski S, Redmond D. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9:335–352. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–1269. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- van der Horst GT, Muijtjens M, Kobayashi K, Takano R, Kanno S, Takao M, de Wit J, Verkerk A, Eker AP, van Leenen D, Buijs R, Bootsma D, Hoeijmakers JH, Yasui A. Mammalian Cry1 and Cry2 are essential for maintenance of circadian rhythms. Nature. 1999;398:627–630. doi: 10.1038/19323. [DOI] [PubMed] [Google Scholar]
- Vogel GW. Evidence for REM sleep deprivation as the mechanism of action of antidepressant drugs. Prog Neuropsychopharmacol Biol Psychiatry. 1983;7:343–349. doi: 10.1016/0278-5846(83)90122-7. [DOI] [PubMed] [Google Scholar]
- Vogel GW, Buffenstein A, Minter K, Hennessey A. Drug effects on REM sleep and on endogenous depression. Neurosci Biobehav Rev. 1990;14:49–63. doi: 10.1016/s0149-7634(05)80159-9. [DOI] [PubMed] [Google Scholar]
- Ware JC, Pittard JT. Increased deep sleep after trazodone use: a double-blind placebo-controlled study in healthy young adults. J Clin Psychiatry. 1990;51(Suppl):18–22. [PubMed] [Google Scholar]
- Wehr TA, Rosenthal NE, Sack DA, Gillin JC. Antidepressant effects of sleep deprivation in bright and dim light. Acta Psychiatr Scand. 1985;72:161–165. doi: 10.1111/j.1600-0447.1985.tb02589.x. [DOI] [PubMed] [Google Scholar]
- Wehr TA, Sack DA, Rosenthal NE. Sleep reduction as a final common pathway in the genesis of mania. Am J Psychiatry. 1987;144:201–204. doi: 10.1176/ajp.144.2.201. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents. 10 Years later. Arch Gen Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Wiegand M, Berger M, Zulley J, Vonzerssen D. The Effect of Trimipramine on Sleep in Patients with Major Depressive Disorder. Pharmacopsychiatry. 1986;19:198–199. [Google Scholar]
- Williams HL, Karacan J, Harsch CJ. Electroencephalography (EEG) of Human Sleep. John Wiley & Sons; 1974. [Google Scholar]
- Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–107. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- Winokur A, Gary KA, Rodner S, Rae-Red C, Fernando AT, Szuba MP. Depression, sleep physiology, and antidepressant drugs. Depress Anxiety. 2001;14:19–28. doi: 10.1002/da.1043. [DOI] [PubMed] [Google Scholar]
- Wirz-Justice A, Van den Hoofdakker RH. Sleep deprivation in depression: what do we know, where do we go? Biol Psychiatry. 1999;46:445–453. doi: 10.1016/s0006-3223(99)00125-0. [DOI] [PubMed] [Google Scholar]
- Wu JC, Bunney WE. The biological basis of an antidepressant response to sleep deprivation and relapse: review and hypothesis. Am J Psychiatry. 1990;147:14–21. doi: 10.1176/ajp.147.1.14. [DOI] [PubMed] [Google Scholar]
- Wu JC, Gillin JC, Buchsbaum MS, Hershey T, Hazlett E, Sicotte N, Bunney WE., Jr The effect of sleep deprivation on cerebral glucose metabolic rate in normal humans assessed with positron emission tomography. Sleep. 1991;14:155–162. [PubMed] [Google Scholar]
- Wu JC, Kelsoe JR, Schachat C, Bunney BG, DeModena A, Golshan S, Gillin JC, Potkin SG, Bunney WE. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009;66:298–301. doi: 10.1016/j.biopsych.2009.02.018. [DOI] [PubMed] [Google Scholar]
- Yang JD, Elphick M, Sharpley AL, Cowen PJ. Effects of carbamazepine on sleep in healthy volunteers. Biol Psychiatry. 1989;26:324–328. doi: 10.1016/0006-3223(89)90046-2. [DOI] [PubMed] [Google Scholar]
- Yorbik O, Birmaher B, Axelson D, Williamson DE, Ryan ND. Clinical characteristics of depressive symptoms in children and adolescents with major depressive disorder. J Clin Psychiatry. 2004;65:1654–1659. doi: 10.4088/jcp.v65n1210. quiz 1760–1651. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, McGlinchey JB, Young D. Diagnosing major depressive disorder X: can the utility of the DSM-IV symptom criteria be improved? J Nerv Ment Dis. 2006;194:893–897. doi: 10.1097/01.nmd.0000248970.50265.34. [DOI] [PubMed] [Google Scholar]