Abstract
Purpose
The aim of this study was to determine whether the recent refinement and downsizing of the implants for posterior cervical fusion increase the occurrence of implant failure.
Methods
One hundred forty-two consecutive cases of cervical fusion, using either cannulated Magerl screws or a multiaxial pedicle screw–rod system, were reviewed retrospectively after an average follow-up period of more than 3 years, and the rate and characteristics of the failure of these implants were evaluated.
Results
Implant failure occurred in six (4.2%) patients: five with rheumatoid arthritis and one with athetoid cerebral palsy. Occipital plate fracture occurred in two patients, Magerl screw breakage in one patient, cervical pedicle screw fracture in two patients, and disassembly of the pedicle screw and rod in two patients (one with an occipital plate fracture). There was no rod fracture. The implant failures were asymptomatic, except in one patient. Disassembly of the pedicle screw and rod was observed immediately after another surgical procedure under general anesthesia in two patients.
Conclusions
The failure rate of 4.2% was similar to the rates reported in the literature for posterior lumbar spinal fusion, confirming the reliability of the recent cervical screw–rod system.
Keywords: Posterior cervical fusion, Rod–screw systems, Implant failure, Transarticular screw fixation
Introduction
Recent advances and refinements of spinal implants with the screw and rod system allow us to fix the cervical spine rigidly and safely, with favorable clinical outcomes. From a mechanical perspective, atlantoaxial transarticular screws (Magerl screws; MS) and cervical pedicle screws (CPS) provide excellent strength as anchors [1]. The advent of cannulated MS screws, which are inserted along a guide wire, has increased their safety and reduced the inherent risk of injury to the spinal cord or vertebral artery (VA) [2, 3]. However, cannulated screws may be mechanically inferior to solid screws. CPS were originally monoaxial and were used with a plate [4, 5], which restricted their insertion points, increasing the risk of VA injury. It was also sometimes difficult to connect multiple CPS. The development of multiaxial CPS and rod systems, which allow more freedom, has resolved these problems. However, the more complex mechanisms used in these refined systems may have mechanical weak points. In the cervical spine, the anatomical size of the bone and the course of the VA restrict the size of the implant, so much smaller screws and rods have been developed than those used in thoracic and lumbar spinal implants. The diameters of the most commonly available screws are 3.5 and 4.0 mm, and the diameters of the rods are 3.0–3.5 mm. Although the mechanical stress in the cervical spine is also less than that in the lumbar spine, the reduced size of the refined implants may increase the possibility of implant failure in the cervical spine. In this study, 142 consecutive cases of cervical fusion with either cannulated Magerl screws or the multiaxial pedicle screw–rod systems were reviewed retrospectively after an average follow-up period of more than 3 years, and the rate and characteristics of the failure of these implants were determined.
Materials and methods
One hundred forty-two patients (41 men and 101 women, age range 16–84 years) underwent posterior cervical fusion at our institute with screws and/or rods during a 12-year period from January 1998 to December 2009. Patients who had undergone occipitocervical (O–C) fusion or cervicothoracic (C–T) fusion were also included if at least one screw was inserted into the cervical spine. Patients who had undergone cervical fusion with monoaxial pedicle screws or without screws were excluded. The original diagnoses were 83 atlantoaxial subluxation (AAS) with or without vertical subluxation (VS) or subaxial subluxation (SAS), 11 SAS without AAS, 15 primary or metastatic spinal tumors, ten cervical spondylotic myelopathy, nine athetotic myelopathy, five dens fractures, and nine others. Eighty patients with rheumatoid arthritis (RA) were included. The spinal ranges of fixation included 66 simple C1–2 fusions, 27 O–C fusions, 26 cervical fusions other than C1–2 fixation, 13 C–T fusions, and ten occipitocervicothoracic (O–C–T) fusions. The fusion ranges according to the numbers of vertebrae fixed were two vertebrae in 70 patients, three in 21 patients, four in three patients, five in 11 patients, six in 13 patients, seven in six patients, and eight or more in 18 patients. The fixation methods included 49 occipital plates, 158 MS, 320 CPS, five C1 lateral mass screws, eight lateral mass screws other than C1, two C2 laminar screws, and four subaxial transarticular screws. All screws were made of titanium alloy. The systems used were Oasys® (Stryker Spine) in 41 patients, UCSS® (Medtronics Sofamor Danek) in 34 patients, Reunion® (Surgical Dynamics) in 31 patients, Olerud Cervical® (Anatomica AB) in 19 patients, Mountaineer® (DePuy Spine) in five patients, Vertex® (Medtronics Sofamor Danek) in four patients, and eight others. In C1–2 fixation, a unicortical iliac bone graft strut was fixed on C1–2 supported with morselized bone chips, according to Gallie [6] using either a metal cable or polyethylene cable (Secure Strand; Surgical Dynamics, Norwalk, CT). In fixation other than C1–2, unicortical iliac bone graft struts and morselized bone chips were put on laminae, facet joints, and occipital bone after meticulous decortications and resection of the articular cartilage.
The follow-up period ranged from 1 week to 122 months, with an average follow-up of 36.4 months. Thirteen patients were confirmed to have died independently of their cervical operation, and half the patients (72 patients) saw one of the authors and underwent radiographic analysis within 1 year of the time of writing.
We defined “implant failure” as the fracture of a metal component, such as the screws or rods, or the disassembly of fixed constructs. Screw loosening or back-out was not included because our aim in this study was to analyze clinically the mechanical and fatigue strengths of the implants.
To evaluate the bone union, we set the following criteria for pseudoarthrosis. (1) No apparent bone continuity was observed between the graft bone and posterior elements such as posterior arch, lamina, and facet joints in lateral radiographs and CT scan. (2) Apparent intervertebral mobility inside the fixation range was observed in the three (extension/neutral/flexion positions) lateral functional radiographs. If both criteria were fulfilled, the fixation was defined as apparent pseudoarthrosis.
Results
The demographic and clinical data for the patients with and without implant failure are summarized in Table 1. Implant failure was observed in six (4.2%) of the 142 patients. Five of these patients had RA, and one had athetoid cerebral palsy. Occipital plate fracture occurred in two patients, MS breakage in one patient, CPS fracture in two patients, and disassembly of the pedicle screw and rod in two patients (one instance of which occurred with occipital plate fracture; Table 2). There was no rod breakage. The average duration between surgery and implant failure was 16.8 months (3 weeks to 38 months). Among the 100 patients followed more than 12 months, implant failure rate was 6.0%. Bilateral implant breakage was observed in five patients, and the contralateral breakage occurred within 1 year of the first failure at the same spinal level. Disassembly between the pedicle screw and the rod occurred in both cases immediately after another surgical procedure performed under general anesthesia.
Table 1.
Comparative summary of patients with and without implant failure
| Implant failure | No failure | Total | |
|---|---|---|---|
| Number of patients (%) | 6 (4.2) | 136 | 142 |
| Gender | |||
| Male | 3 | 38 | 41 |
| Female | 3 | 98 | 101 |
| Mean age | 61 (45–70) | 59 (16–84) | 59 (16–84) |
| Diagnosis | |||
| RA(AAS/SAS/VS) | 5 (6.3%) | 75 | 80 |
| Spinal tumor | 0 | 15 | 15 |
| Cervical spondylotic myelopathy | 0 | 10 | 10 |
| Athetotic myelopathy | 1 (11) | 8 | 9 |
| Os odontoideum | 0 | 6 | 6 |
| Dens fracture | 0 | 5 | 5 |
| Other | 0 | 17 | 17 |
| Fixation level | |||
| Cervical | |||
| C1–2 | 1 | 65 | 66 |
| C–T | 1 | 12 | 13 |
| Other | 1 | 25 | 26 |
| Occipital | |||
| O–C | 2 | 25 | 27 |
| O–C–T | 1 | 9 | 10 |
| Fixation range* | |||
| 2 | 1 | 69 | 70 |
| 3 | 1 | 20 | 21 |
| 4 | 0 | 3 | 3 |
| 5 | 0 | 11 | 11 |
| 6 | 1 | 12 | 13 |
| 7 | 0 | 6 | 6 |
| ≧8 | 3 | 15 | 18 |
* Fixation range means the number of levels of instrumentation
Table 2.
Data of the six patients with implant failures
| Case | Age/gender | Diagnosis | Type of implants | System of implants | Diameter of screw (mm) | Fixation level | Type of failure | Onset of failure (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 59/M | RA | MS | UCSS | 4.0 | C1–2 | Screw fracture (bilateral) | 33 |
| 2 | 59/F | RA | CPS | Olerud | 4.0 | C2–7 | Screw fracture | 6 |
| 3 | 45/M | Athetoid CP | CPS | OASYS | 4.0 | C2–Th2 | Screw fracture | 12 |
| Screw fracture | 24 | |||||||
| 4 | 64/M | RA | MS + CPS + | OASYS | 3.5 | O–C7 | Plate fracture | 37 |
| O-plate | Plate fracture | 42 | ||||||
| 5 | 70/M | RA | CPS + LS + | OASYS | 3.5 | O–C2 | Screw disassemble | 1 |
| O-plate | ||||||||
| 6 | 70/M | RA | CPS + O-plate | OASYS | 4.0 | O–Th2 | Screw disassemble | 6 |
| Plate fracture (bilateral) | 11 |
MS Magerl screw, CPS cervical pedicle screw, O-plate occipital plate, LS laminar screw
Apparent pseudoarthrosis without implant failure was observed in three patients (3.0%), two of whom were followed up conservatively and one of whom had dropped out of follow-up.
After the implant failures, only one patient with bilateral MS fractures required a salvage operation because of neck pain (Fig. 1). Neither de novo complaints nor instabilities requiring revision surgery were observed after the implant failures in the other five patients (Fig. 2). Three patients were followed up conservatively, one had delayed bone union, and one dropped out of follow-up.
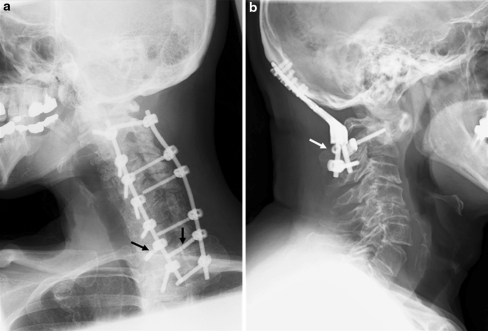
Fig. 1.
Implant failure Case 1. a Lateral X-ray 3 years after the initial C1–2 fixation showing bilateral MS breakage. b Lateral X-ray after the revision surgery with MS and Atlas claw. The distal stumps of the screws (arrow) were left alone
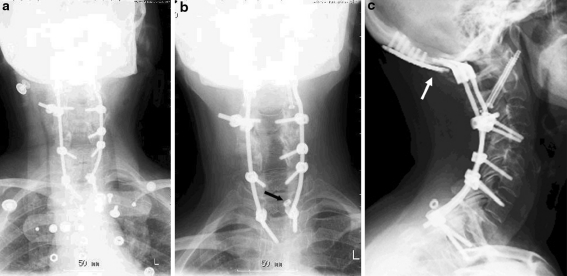
Fig. 2.
a Implant failure Case 3. Oblique X-ray 2 years after the C2–T2 fixation showing bilateral T1 PS breakage (arrows). b Implant failure Case 5. Lateral X-ray 1 month after the O–C2 fixation showing disassembly of the C2 PS and rod (arrow)
Case illustration
There was one illustrative case of disassembly of the constructs (Fig. 3). This 70-year-old woman with RA had a surgical history of atlantoaxial fixation with MS for AAS. She was treated with cervical laminoplasty and an O–C–Th2 fusion for cervical myelopathy with SAS. An allograft was used because no autograft from the iliac crest was available because she had previously undergone multiple lumbar fusions. Another surgical procedure (total elbow arthroplasty) was performed under general anesthesia 6 months after the O–C–T fusion. She had mild neck pain and a stiff shoulder immediately after her recovery from anesthesia. Disassembly between the left T2 pedicle screw and rod was identified. The patient also reported a clattery noise in her neck 5 months after the implant failure. An X-ray showed subsequent breakage of the bilateral occipital plates. Revision surgery was not required because her symptoms were mild.
Fig. 3.
a Early postoperative anteroposterior (AP) X-ray after O–C–T2 fusion. Lateral connector was used to connect right C4 pedicle screw and the rod to avoid excessive bending of the rod. b AP X-ray after total elbow arthroplasty revealing disassembly between the left T2 pedicle screw and rod (arrow). c Lateral X-ray 5 months after the initial implant failure showing bilateral occipital plate breakage (arrow)
Discussion
Although posterior cervical spinal fusion using screw–rod devices has become a popular technique for the treatment of spinal instability or deformity, few studies have discussed the mechanical implant failure of these devices. The results of the present study show an implant failure rate of 4.2% in posterior cervical spinal fusions using either cannulated MS or a multiaxial pedicle screw–rod system. When the patients were divided into two groups according to the implant used, MS group (simple atlantoaxial fixation using cannulated MS), screw–rod group (other cervical fixation using multiaxial CPS), an implant failure rate was 1.7% (1/60) in MS group and 6.1% (5/82) in screw–rod group.
Implant failure in MS
Madawi et al. [7] reported that screw breakage occurred in five (8.2%) of 61 patients treated for AAS with MS. The patients included 37 (61%) with RA, 15 with traumatic atlantoaxial instability, and 9 with other indications. Either 3.5 mm solid full-threaded cortical screws or lag screws were used. Four of the patients with screw breakage had RA. In our series, one patient with RA experienced MS breakage, and failure rate of 1.7% was lower than their report even though cannulated screws were used. They pointed out that all five broken screws were associated with one of 17 malpositioned screws that missed the lateral mass of C–1, whereas there were no malpostitioned screws in our series. That may be the reason for a lower rate of screw breakage.
Implant failure in CPS
Hirano et al. [8] reviewed 56 RA patients who had undergone O–C–T fusions with unit rods (4.75 mm in diameter) with sublaminar wiring or with multiaxial CPS and rod systems (3.2/3.5 mm rod). They reported that implant failure, including both mechanical failure of the implants and screw loosening or back-out occurred in 13 (23.2%) patients, and that the failure rate was 15.8% in the unit rod group and 38.9% in the CPS and rod group. Our implant failure rate of 6.1% in CPS is similar to, or lower than, those in the report. Unfortunately, in our knowledge, there was no large case study regarding implant failure of monoaxial cervical pedicle screw and plate systems.
Implant failure and bone union
Naturally, bone fusion is by far the most important factor in preventing implant failure. Therefore, mechanical failure rates are closely related to the bone graft technique, the patient’s medical condition and activity, and the gap to be fused, making a simple comparison between implant failure rates meaningless. All the cases of implant failure involved patients with RA or athetosis, in which the bone union rate is generally thought to be low. In Madawi’s MS series, four of the five patients with screw breakage had RA and an overall osseous fusion rate was 81% in RA patients, whereas traumatic group achieved 100% union. Ito [9] in our group reviewed 38 patients who submitted to MS fixation with posterior bone graft and reported that an osseous fusion rate was 93.1% in RA patients, whereas the fusion rate was 100% in non-RA patients.
We tried to use meticulous bone graft techniques. However, no bone graft was performed in ten of 13 patients with metastatic tumor, taking their prognosis into consideration, but no implant failure was observed in these patients after a mean follow-up period of 12.6 months (1 week–38 months). In our study, the mean postoperative period before each implant failure, excluding the disassembly of implants, was 28.7 months. These results demonstrate that the modern implants tolerate the mechanical stress imposed in daily life well for a couple of years.
Considering the parameters of the patients who experienced implant failure in the present study, we infer that basic morbidities such as RA and athetosis, fusions that include the occipital bone, and longer fusion ranges could be risk factors for implant failure, although we performed no statistical correlation analysis because the number of patients who experienced implant failure was small.
The characteristics as for cervical instrumentation failure
Several reports have highlighted the complications associated with instrumentation failure in posterior lumbar or thoracolumbar fusion with pedicle screw systems. The failure rates ranged from 0.4 to 22% [10–17]. Interestingly, some characteristics of the implant failures in this study differed from those involving lumbar or thoracolumbar fusions reported in the literature. First is the lack of rod fractures. Jutte et al. [16] reported a 0.9% incidence of rod failure in 105 lumbar or lumbosacral fusions, and in most other reports, rod fractures occurred after posterior lumbar fusion surgery. Intraoperative rod contouring and corrective procedures using reduction devices are generally thought to be risk factors for the failure of spinal constructs, particularly with pure titanium or titanium alloy implants because of their notch sensitivity [10, 18, 19]. One reason that no rod fracture was observed in our cohort may be that we tried as much as possible to avoid bending the rod, taking maximal advantage of the polyaxial screw and offset connecting device (Fig. 1). Another possible reason is that no corrective procedure that depended on the implant itself (e.g., correction of kyphosis) was performed in our series. It may be concluded that the mechanical strength of a 3.5 mm rod is sufficient as far as intraoperative rod contouring and corrective procedures are avoided.
Second, all but one of the implant failures was asymptomatic. This is consistent with the report of Deen et al. [20], who analyzed complications incurred by 100 patients treated with the cervical lateral mass screw–rod system. They reported two screw breakages, both of which were asymptomatic. This may be because the mechanical loading in the cervical spine is far less than that in the lumbar spine [21], and the residual implants maintain enough stability to allow bone fusion without de novo symptoms. Among our seven implant failures, five occurred at the end or second from the end of the construct in four patients who had undergone multilevel fusions. In multilevel fusion, the most critical site to be fused is generally located in the middle of the construct. One reason for the lack of de novo symptoms could be that the implant remained stabilized at the critical site, despite the failure at the end of the construct. Erwin et al. [22] reported breakage of the Harrington spinal instrumentation used to treat scoliosis with solid arthrodesis. Implant failure with a solid fusion occurred in 19 (2.1%) of 888 patients, but none of them experienced symptoms. The authors hypothesized that a solid fusion mass ultimately causes metal fatigue in multiple areas. Our results may support this hypothesis.
Finally, it is noteworthy that disassembly between the pedicle screw and rod was found immediately after another surgical procedure under general anesthesia in two patients. To the best of our knowledge, no cases of spinal implant failure in such a unique situation have been reported in the literature. From a biomechanical perspective, it has been reported that the nut-locking mechanisms between the tulip-shaped head of the screw and the rod are vulnerable to fatigue stress [23]. The reason for the nut disassembly remains unclear but Kim [24] speculated that nut tightening with limited torque, nut cracking, and nut-thread failure, and wear between nut and rod could cause nut loosening. Furthermore, in the tulip-type mono- or multiaxial screws, it is possible that the final tightening of the rod–screw fixation is completed before the rod is perfectly perpendicular to the tulip. With endotracheal intubation or when the patient is placed in a surgical position, an unusual load may be applied to the cervical spine. At that moment, the rod may be situated parallel to the bottom surface of the tulip, causing rod–screw loosening. This could be another possible reason. Therefore, we recommend that we should consider spinal implant disassembly when a subsequent operation is performed under general anesthesia in a patient recently treated with spinal fusion.
We believe that our results can serve as a benchmark to motivate future detailed studies of the long-term durability of the screw–rod fixation devices in the cervical spine and to clarify the risk factors that affect their longevity.
Conclusion
Overall mechanical implant failure occurred in 4.2% of patients treated with posterior cervical spine fusion using either cannulated MS or a multiaxial pedicle screw–rod system. This rate is similar to those reported in the literature for posterior cervical fusion with previous generation instruments or for posterior lumbar spinal fusion, confirming the reliability of the systems despite their small size. Although no absolute evidence can be derived from our small number of patients, three characteristics as for cervical implantation failure become apparent. First, patients who experienced implant failure all suffered comorbidities unfavorable to bone union, including RA and athetoid myelopathy. Second, the implant failures observed in this study were characterized by a lack of rod fractures or de novo symptoms. Third, we should consider the possibility of spinal implant disassembly when performing a subsequent operation under general anesthesia in a patient who has recently undergone cervical spinal fusion.
References
- 1.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. Spine (Phila Pa 1976) 1994;19(22):2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Neo M, Matsushita M, Yasuda T, Sakemoto T, Nakamura T. Use of an aiming device in posterior atlantoaxial transpedicular screw fixation. J Neurosurg Spine. 2002;97:123–127. doi: 10.3171/spi.2002.97.1.0123. [DOI] [PubMed] [Google Scholar]
- 3.Neo M, Sakamoto T, Fujibayashi S, Nakamura T. A safe screw trajectory for atlantoaxial transpedicular fixation achieved using an aiming device. Spine (Phila Pa 1976) 2005;30(9):E236–E242. doi: 10.1097/01.brs.0000160998.53282.3f. [DOI] [PubMed] [Google Scholar]
- 4.Abumi K, Ito H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7(1):19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 5.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997;22(16):1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 6.Gallie WE. Fractures and dislocations of the upper cervical spine. Am J Surg. 1939;46:495–499. doi: 10.1016/S0002-9610(39)90309-0. [DOI] [Google Scholar]
- 7.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86(6):961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 8.Hirano K, Matsuyama Y, Sakai Y, Katayama Y, Imagama S, et al. Surgical complications and management of occipitothoracic fusion for cervical destructive lesions in RA patients. J Spinal Disord Tech. 2010;23(2):121–126. doi: 10.1097/BSD.0b013e3181993315. [DOI] [PubMed] [Google Scholar]
- 9.Ito H, Neo M, Fujibayashi S, Miyata M, Yoshitomi H, Nakamura T. Atlantoaxial transarticular screw fixation with posterior wiring using polyethylene cable: facet fusion despite posterior graft resorption in rheumatoid patients. Spine (Phila Pa 1976) 2008;33(15):1655–1661. doi: 10.1097/BRS.0b013e31817b5c07. [DOI] [PubMed] [Google Scholar]
- 10.McAfee PC, Weiland DJ, Carlow JJ. Survivorship analysis of pedicle spinal instrumentation. Spine (Phila Pa 1976) 1991;16:S422–S427. doi: 10.1097/00007632-199108001-00022. [DOI] [PubMed] [Google Scholar]
- 11.Davne SH, Myers DL. Complications of lumbar spinal fusion with transpedicular instrumentation. Spine (Phila Pa 1976) 1992;17(6):S184–S189. doi: 10.1097/00007632-199206001-00021. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal S, Gill K. Complications of the Wiltse pedicle screw fixation system. Spine (Phila Pa 1976) 1993;18(13):1867–1871. doi: 10.1097/00007632-199310000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J. 1997;6:324–326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine (Phila Pa 1976) 1998;23(14):1566–1571. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 15.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Jt Surg Am. 1999;81:1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11:594–598. doi: 10.1007/s00586-002-0469-8. [DOI] [PubMed] [Google Scholar]
- 17.Peele MW, Lenke LG, Bridwell KH. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976) 2006;31:2392–2398. doi: 10.1097/01.brs.0000238973.13294.16. [DOI] [PubMed] [Google Scholar]
- 18.Dick JC, Bourgeault CA. Notch sensitivity of titanium alloy, commercially pure titanium, and stainless steel spinal implants. Spine (Phila Pa 1976) 2001;26:1668–1672. doi: 10.1097/00007632-200108010-00008. [DOI] [PubMed] [Google Scholar]
- 19.Lindsey C, Deviren V, Xu Z, Yeh RF, Puttlitz CM. The effect of rod contouring on spinal construct fatigue strength. Spine (Phila Pa 1976) 2006;31(15):1680–1687. doi: 10.1097/01.brs.0000224177.97846.00. [DOI] [PubMed] [Google Scholar]
- 20.Deen HG, Nottimeier EW, Reimer R. Early complications of posterior rod-screw fixation of the cervical and upper thoracic spine. Neurosurgery. 2006;59:1062–1068. doi: 10.1227/01.NEU.0000245592.54204.D0. [DOI] [PubMed] [Google Scholar]
- 21.Przybyla AS, Skrzypiec D, Pollintine P, Dolan P, Adams MA. Strength of the cervical spine in compression and bending. Spine (Phila Pa 1976) 2007;32(15):1612–1620. doi: 10.1097/BRS.0b013e318074c40b. [DOI] [PubMed] [Google Scholar]
- 22.Erwin WD, Dickson JH, Harrington PR. Clinical review of patients with broken Harrington rods. J Bone Jt Surg Am. 1980;62(8):1302–1307. [PubMed] [Google Scholar]
- 23.Stanford RE, Loefler AH, Stanford PM, Walsh WR. Multiaxial pedicle screw designs: static and dynamic mechanical testing. Spine (Phila Pa 1976) 2004;29(4):367–375. doi: 10.1097/01.BRS.0000092369.50397.85. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y, Kim T. Finite element analysis of the effects of pedicle screw fixation nut loosening on lumbar interbody fusion based on the elasto-plateau plasticity of bone characteristics. Spine (Phila Pa 1976) 2010;35(6):599–606. doi: 10.1097/BRS.0b013e3181b6258a. [DOI] [PubMed] [Google Scholar]