Abstract
Purpose
Lumbar flexion–extension radiographs in standing position (SFE) are the most commonly used imaging method to evaluate segmental mobility. Many surgeons use SFE to disclose abnormal vertebral motion and base their decision for surgical fusion on its results. We tested the hypothesis that imaging in standing and recumbent position (SRP) reveals a higher sagittal translation (ST) and sagittal rotation (SR) in symptomatic patients than with SFE.
Materials and methods
We analysed images of 100 symptomatic patients with a low-grade spondylolisthesis that underwent surgical fusion. To determine the ST and SR in SRP, we compared the images taken in the recumbent position in the CT with images taken in the standing position during the routine plain radiography.
Results
The measurement of ST revealed an absolute value of 2.3 ± 1.5 mm in SFE and 4.0 ± 2.0 mm in SRP and differed significantly (p = 0.001). The analysis of the relative value showed an ST of 5.9 ± 3.9% in SFE and 7.8 ± 5.4% in SRP (p = 0.008). The assessment of ST in flexion and in a recumbent position (FRP) revealed the highest ST (4.6 ± 2.5 mm or 9.2 ± 5.7%). Comparison of SR showed the highest rotation in SFE (6.1° ± 3.8°), however, compared to SRP (5.4° ± 3.3°), it missed the level of significance (p = 0.051).
Conclusions
For evaluation of ST in symptomatic patients with spondylolisthesis SRP appears to be more suitable than SFE, while a pathological SR is better revealed in SFE. The analysis of SRP might offer a complementary method to detect or exclude pathological mobility in more cases.
Keywords: Lumbar surgery, Back pain, Radiography
Introduction
Lumbar flexion–extension radiographs taken in a standing position (SFE) are the most commonly used imaging method to detect abnormal segmental mobility. Many surgeons use SFE to detect abnormal vertebral motion or to base their decision for surgical fusion on its results [1–4]. The range of lumbar segmental mobility is wide, but a sagittal translation (ST) of ≥4 mm or ≥8% and sagittal rotation (SR) of ≥10° in L1-5 and ≥2° in L5-S1, respectively, are commonly accepted as a radiologic sign of pathologic mobility and seem to have a strong clinical impact [3, 5–7].
Nonetheless, the use of SFE to determine pathologic lumbar mobility has been questioned due to its lack of routine reference standard, inaccurate reproducibility and non-standardized techniques. The optimal choice of patient’s position to reveal the maximal ST has been critically discussed as well. While many authors claim that the measurements taken in a sitting position demonstrate the overall best performance and the least interference by concomitant motions [5, 8], other authors prefer the lateral decubitus position, traction or compression to maximize the degree of slip [9, 10].
However, due to the fact that the standing position evokes a greater slip than the recumbent position [9, 11, 12], and due to its simple usage and low cost SFE is routinely applied in most spinal centres.
A low-grade spondylolisthesis with an ST of less than 5 mm, compared with SFE no longer seems to represent a criterion for fusion surgery [13, 14]. Therefore, many patients with a “stable” spondylolisthesis undergo spinal decompression surgery without instrumentation [13, 14], however in symptomatic patients pain may prevent an adequate bending of the trunk and lead to an underestimation of the intervertebral motion. Furthermore, even small differences in measurements shown by the various methods could reveal a substantial vertebral slip especially in low-grade spondylolisthesis. A substantial vertebral slip would be an important criterion to base the decision for or against fusion surgery.
There are no recent comparative studies about radiography of low-grade spondylolisthesis [15, 16]. The multitude of possible positions for functional radiography and complicated manoeuvres that might cause the maximal ST makes it difficult to choose the proper diagnostic modality. Yet, plain and flexion–extension radiographs taken in a standing position and CT or MRI-scans taken in a recumbent supine position are available for almost every patient undergoing spinal surgery.
We tested the hypothesis, that imaging in standing and recumbent position (SRP) that is done as part of the routine diagnostics with CT and radiography reveals a higher ST- and SR-value than SFE in symptomatic patients.
Materials and methods
Patients
We compared and analysed the plain anterior–posterior and lateral radiographs (APL), SFE-radiographs and CT scans of 100 symptomatic patients with a low-grade spondylolisthesis that have undergone surgical fusion in our department.
Radiographs
Preoperative APL and SFE as well as CT scans were available in all cases. We only analysed images of patients who received the radiographs in our hospital to ensure a constant distance between the patient and the X-ray source. The distance between the X-ray source and the patient during plain and functional radiography was 1.15 m. These images were available as part of the preoperative routine diagnostics. No extra radiography was performed to avoid unnecessary radiation exposure. All radiographs were digitally available in our hospital archives.
ST and SR were analyzed according to Dupuis et al. [3] (Fig. 1). The determination of translational displacement was measured in absolute values and percentage of the upper vertebral body width.
Fig. 1.
Sagittal CTreconstruction of the lumbar spine to demonstrate the measurement technique of Dupuis et al. [3]: The ST was defined as the perpendicular distance between parallel lines L and R. The intersection line I is drawn along the endplate of the superior vertebral body to determine the exact intersection between R and U. To obviate inaccuracies due to magnification, ST was also assessed as percentage of the upper vertebral body width (W). SR was measured as the angle between the posterior body lines L and U
To validate the assessed data the measurement was performed independently by two examiners.
Data analysis
SR and ST were measured on the dynamic radiographs by subtraction from flexion to extension (SFE), on the plain radiographs (standing position) and on the CT (recumbent supine position) by subtraction from plain standing position and supine recumbent position (SRP), respectively.
We preferred to use the scout view in the CT to determine vertebral angulation and sagittal motion, however due to the lower resolution, we additionally validated the measurement with the aid of the sagittal CT reconstruction. The SFE radiographs were performed in a standing position (Fig. 2).
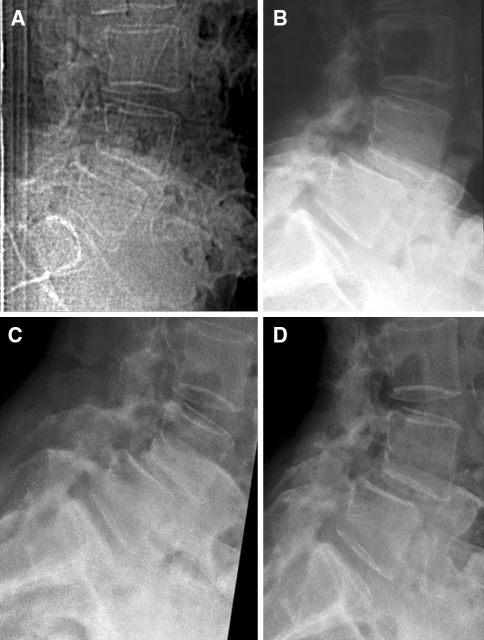
Fig. 2.
Radiographs of a female patient in recumbent supine position in CT scout view (a) and plain standing position (b). The sagittal vertebral slip increases in standing position (b) compared to recumbent supine position (a), while it does not substantially change when comparing standing flexion (c) and extension (d) radiographs
The measurement was performed with the aid of the Osirix Imaging Software (Pixmeo Sarl, Switzerland). The values were expressed as mean with standard deviation. The statistical analysis was performed using the Wilcoxon test for dependent, non-parametric values, Pearson’s Chi square test and t test for dependent values.
Besides comparison of absolute and relative values we analysed the abiliy of the various positions in SFE and SRP to detect a pathologic ST and SR as defined by previous studies (i.e. ST of ≥4 mm or ≥8% at L1-5 and ≥6% at L5-S1; and SR of ≥10° at L1-5 and ≥2° at L5-S1) [7, 17].
Results
100 patients were included (65 females and 35 males). The patients’ age ranged from 24 to 85 years (mean age 62.1 years) at time of surgery. Spondylolisthesis was present in all cases and it involved grade I in 72 cases and grade II in 28 cases. Most patients (n = 83) had a degenerative spondylolisthesis and suffered from a claudicatio spinalis, back pain and sciatica. 17 patients presented an isthmic spondylolisthesis and suffered from back pain only.
The patients with a degenerative spondylolisthesis were significantly older than the patients with an isthmic spondylolisthesis (70.1 ± 5.7 and 39.5 ± 8.1 years, respectively, p = 0.001). The majority of patients had a level L4-5 spondylolisthesis (Table 1).
Table 1.
Type, level and grade of spondylolisthesis
| N | |
|---|---|
| Type of spondylolisthesis | |
| Degenerative | 83 |
| Isthmic | 17 |
| Level of interest | |
| L1-2 | 1 |
| L2-3 | 5 |
| L3-4 | 15 |
| L4-5 | 58 |
| L5-S1 | 21 |
| Grade of spondylolisthesis | |
| Grade I | 72 |
| Grade II | 28 |
Presentation of type, level and grade of spondylolisthesis
The average spondylolisthesis was 25.2 ± 8.5% in the standing position.
Sagittal translation (ST)
The measurement of ST revealed an absolute value of 2.3 ± 1.5 mm in SFE and 4.0 ± 2.0 mm in SRP and differed significantly (p = 0.001) (Table 2A).
Table 2.
Sagittal translation values Sagittal translation presented with mean and standard deviation in absolute (A) and relative values (B) and subdivided into absolute and relative values defined as pathologic [7, 17] (C)
| (A) | |||
| SFE (mm) | 2.3 ± 1.5 | ||
| SRP (mm) | 4.0 ± 2.0** | ||
| FRP (mm) | 4.6 ± 2.5** | ||
| (B) | |||
| SFE (%) | 5.9 ± 3.9 | ||
| SRP (%) | 7.8 ± 5.4* | ||
| FRP (%) | 9.2 ± 5.7* | ||
| ≥4 mm in L1-S1 (n = 100) | ≥8% in L1-5 (n = 79) | ≥6% in L5-S1 (n = 21) | |
|---|---|---|---|
| (C) | |||
| SFE (n) | 12 | 19 | 12 |
| SRP (n) | 47** | 42* | 11 |
| FRP (n) | 60** | 44* | 13 |
The statistical analysis was performed using the Wilcoxon test for dependent, non-parametric values, Pearson’s Chi-square test and t test for dependent values
SFE Flexion–Extension radiography in standing position, SRP radiography in standing and recumbent position, FRP radiography in flexion and recumbent supine position
** p = 0.001, * p = 0.01–0.049, only statistical comparison of SRP and FRP with SFE indicated
The analysis of the relative value showed an ST of 5.9 ± 3.9% in SFE and 7.8 ± 5.4% in SRP and differed significantly (p = 0.008) as well (Table 2B). The vertebral anterior translation was highest during flexion and lowest during recumbent supine position (FRP). The measurement of ST in FRP showed an absolute value of 4.6 ± 2.5 mm and differed significantly from ST in SFE (p = 0.001) and SRP (p = 0.045).
The analysis of the relative value showed an ST of 9.2 ± 5.7% in FRP (Table 2). This differed significantly from SFE (p = 0.0062), but did not reach the level of significance when comparing the relative values with SRP (p = 0.062).
An ST at levels L1-5 of ≥4 mm and ≥8% could be detected significantly more often in SRP and FRP than in SFE (p < 0.001 and p < 0.03, respectively) (Table 2C). However, it is important to note that in 11 of these patients, SFE revealed a pathologic ST of ≥8% (in L1-5), while SRP did not. FRP revealed a pathologic ST in only 6 of these 11 cases and missed 5 of them being pathologic as well. The interobserver error was 1.4 mm assessing ST and did not affect statistical analysis.
Sagittal rotation (SR)
The measurement of SR revealed no significant differences between SFE, SRP and FRP (Table 3), however there was at least a trend that SFE evokes a greater SR than SRP (p = 0.051). In 51 cases a higher SR could be assessed in SFE compared to SRP. SR in SFE revealed the most cases with a pathological segmental mobility (21%) (Table 3D). Only 13 of these 21 cases showed a pathological ST of ≥8% in SFE.
Table 3.
Sagittal rotation presented with mean and standard deviation for L1-S1 (A), L1-5 (B) and L5-S1 (C) and subdivided into values defined as pathologic[7, 17] (D)
| (A) | |
| SFE (L1-S1) | 6.1° ± 3.8° |
| SRP (L1-S1) | 5.4° ± 3.3° |
| FRP (L1-S1) | 6.0° ± 3.5° |
| (B) | |
| SFE (L1-5) | 7.7° ± 2.9° |
| SRP (L1-5) | 7.2° ± 2.6° |
| FRP (L1-5) | 7.5° ± 2.7° |
| (C) | |
| SFE (L5-S1) | 4.2° ± 3.1° |
| SRP (L5-S1) | 3.6° ± 2.5° |
| FRP (L5-S1) | 3.4° ± 2.7° |
| ≥10° in L1-5 (n = 79) | ≥2° in L5-S1 (n = 21) | |
| (D) | ||
| SFE (n) | 15 | 6 |
| SRP (n) | 9 | 5 |
| FRP (n) | 10 | 6 |
The statistical analysis was performed using the Wilcoxon test for dependent, non-parametric values, Pearson’s Chi square test and t test for dependent values
SFE flexion–extension radiography in standing position, SRP radiography in standing and recumbent position, FRP radiography in flexion and recumbent supine position
Regarding a rotation of ≥10° at L1-5 and ≥2° at L5-S1 as a sign of pathologic mobility, SFE, SRP and FRP did not differ either (p > 0.86). The interobserver error was 2.6° assessing SR and did not influence the statistical results.
Discussion
The study of 100 symptomatic patients with a low-grade spondylolisthesis showed that the radiography in SRP evokes a greater ST than the standard SFE in most of the patients. SR might be better achieved with SFE than with SRP. Nevertheless, SFE revealed a pathologic ST in 11% of cases that had not been apparent in SRP.
The number of comparative studies analysing different positions and movements to reveal maximal slip of the vertebral body is limited, and recent studies are rare [16]. The abnormal translation appears to be increased in standing position compared to recumbent position [9, 11, 12, 18–20]. Thus, dynamic flexion extension radiographs became the standard imaging technique to reveal maximal segmental motion [1, 2, 21]. Our study confirms the finding that the vertebral sagittal slip is higher in standing position than in recumbent supine position in most of our patients [10]. This may be related to axial compressing forces.
While static radiographs seem to show the greatest slip in standing position, in cases of hypermobile spondylolisthesis the lateral decubitus position may reveal an even higher abnormal translation, because the stiffness of the splinting muscles is reduced as shown by Wood et al. [9]. Nevertheless, the study of Wood et al. [9] involved only 50 subjects and 6 of them were asymptomatic. Four of the patients (8%) patients did not reveal any abnormal motion in decubitus position. Furthermore, the majority of the patients (52%) had an isthmic spondylolisthesis and were younger than 40 years, which may result in a better physical condition and lumbar mobility [22].
Pain leads to decreased intervertebral motion in symptomatic patients with spondylolisthesis [23]. Adequate functional radiographs depend on the patient’s effort and cooperation, on the examiner’s proper control and motivation, and can lead to different results from test to test [24]. Imaging in a recumbent supine position with a relatively relaxed state of muscles and in a standing position with activation of the muscles excludes this bias as far as possible and still reveals a vertebral motion. Nevertheless, SFE identified 11% of patients with a pathologic segmental mobility that had not been apparent in SRP. These patients might have been better motivated by the examiner or adapted to pain, but it also shows the value of SFE. While studies exist that reveal the maximum slip of the vertebral bodies in various positions, they lack considerable patient numbers and symptomatic subjects with substantial pain and demand special manoeuvres and tools that complicate practical clinical application [10].
Greater values of SR could be assessed in SFE, however it was a comparably poor method to reveal pathological values in any position. Interestingly, increased SR did not accompany pathological ST in all cases. This could be explained by degenerative changes of the intervertebral space and the facet joint that may hinder an adequate angular motion. An abnormal ST was the most common sign of pathologic segmental mobility. A pathological SR in SFE was only detected in 21% of cases. This is consistent with other studies that showed a high variation and limited clinical value of sagittal rotation [9, 19, 25]. The comparatively high SR at level L5-S1 in our series can probably be explained by the high share of young patients with an isthmic spondylolisthesis who have a better physical condition than the older patients with a protracted degeneration [22]. The pathogenesis of an isthmic and a degenerative spondylolisthesis is different, as are often age, physical condition and symptoms of the patients. Therefore, the mixture of both patient groups presents a potential bias in such a study. We have previously emphasized such a bias in the study of Wood et al. [9]. While the difference between standing and recumbent position affected both entities in a similar way in our collective, the differences between the two groups must be carefully considered.
While the assessment of absolute ST in FRP reached the level of statistical significance compared to SFE and SRP, it did not do so when comparing with the relative values. This might be related to measurement inaccuracies resulting from different magnification, although the distance between patients and X-ray source was constant. The measurement of structures without a visible calibration represents a substantial source of error. Vertebral bodies of irregular shapes that might be seen in degenerative spinal diseases can complicate a precise comparison as well [25]. Nevertheless, the measurement method of Dupuis et al. is accepted as a valid technique to determine translational and angular displacement and similar to techniques used by other authors [7, 10]. The measurement of the percentage of vertebral body width avoids inaccuracies resulting from magnification [21]. Our interobserver error is comparable with other studies and it did not affect the statistical result [9, 18].
CT and MRI are considered as the gold standard to assess the level of stenosis, but it must be considered that clinical symptoms of a stenosis impair in standing position when compared to a recumbent position. Our study could show that the vertebral slip significantly increases from supine to standing position. Thus, the presence of at least standing X-ray images represent a necessity in spinal degenerative pathology as the availability of standing MRI or CT images are technically challenging and, from a financial point of view, probably not useful.
Taking a ST of 4 mm or 8% or more in SFE as a sole criterion for pathologic segmental mobility would have meant that only a minority of our patients would have been properly selected for fusion surgery, at least according to recent studies [13, 14]. The overestimate of ST in radiographs can lead to fusion surgery as well, however, deciding for surgery and choosing a specific surgical procedure depends on many factors that involve the patient’s history, the clinical symptoms and the radiologic findings. Based on these criterions, we decided to perform fusion surgery in all of these 100 symptomatic patients with low-grade spondylolisthesis.
Nevertheless, considering the value of 4 mm and 8% ST in SFE would have meant that the majority of our patients with a degenerative spondylolisthesis could have undergone surgery without instrumentation, although a pathologic condition could be revealed regarding ST in SRP or FRP. This could have caused later problems in these patients due to secondary hypermobility. Thus, SFE alone is not sufficient to disclose pathologic segmental motion. Fusion surgery was recommended as two important conditions could be observed in our study collective: the presence of pain and of a spinal pathology, spondylolisthesis. It is debatable whether the patients with a pathological ST of more than 4 mm or 8% in SRP would have found benefit for a longer period, if decompression alone had been performed.
Conclusions
SFE represents a common and proper method to reveal pathologic segmental mobility, however it shows a lower ST than SRP in most patients. Adequate functional radiographs depend on the patient’s pain status, effort and cooperation and can lead to different results from test to test. The imaging in a recumbent supine position with a relatively relaxed state of the muscles and in a standing position with an activation of the muscles acting as a splinter against gravity excludes this bias as far as possible.
Therefore, to disclose a pathologic segmental mobility SFE alone is not sufficient and should be complemented by the analysis of radiographs in SRP that are commonly available in most patients before surgery.
As CT scans and plain and functional radiographs are commonly available in symptomatic patients and are often performed routinely in most of the spine centres, the evaluation of ST in SRP might offer an easily available complementary diagnostic modality.
Acknowledgment
We thank Mrs. Leah Hecker for editing the manuscript.
Conflict of interest None.
References
- 1.Pitkanen MT, Manninen HI, Lindgren KA, Sihvonen TA, Airaksinen O, Soimakallio S. Segmental lumbar spine instability at flexion-extension radiography can be predicted by conventional radiography. Clin Radiol. 2002;57(7):632–639. doi: 10.1053/crad.2001.0899. [DOI] [PubMed] [Google Scholar]
- 2.Guyer RD, McAfee PC, Banco RJ, Bitan FD, Cappuccino A, Geisler FH, Hochschuler SH, Holt RT, Jenis LG, Majd ME, Regan JJ, Tromanhauser SG, Wong DC, Blumenthal SL. Prospective, randomized, multicenter food and drug administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow-up. Spine J. 2009;9(5):374–386. doi: 10.1016/j.spinee.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine. 1985;10(3):262–276. doi: 10.1097/00007632-198504000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;165:110–123. [PubMed] [Google Scholar]
- 5.Morgan FP, King T. Primary instability of lumbar vertebrae as a common cause of low back pain. J Bone Joint Surg Br. 1957;39(1):6–22. doi: 10.1302/0301-620X.39B1.6. [DOI] [PubMed] [Google Scholar]
- 6.Kanemura A, Doita M, Kasahara K, Sumi M, Kurosaka M, Iguchi T. The influence of sagittal instability factors on clinical lumbar spinal symptoms. J Spinal Disord Tech. 2009;22(7):479–485. doi: 10.1097/BSD.0b013e31818d1b18. [DOI] [PubMed] [Google Scholar]
- 7.Posner I, White AA, Edwards WT, Hayes WC. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982;7(4):374–389. doi: 10.1097/00007632-198207000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Shaffer WO, Spratt KF, Weinstein J, Lehmann TR, Goel V. Volvo Award in clinical sciences. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment. An experimental model. Spine (Phila Pa 1976) 1990;15(8):741–750. [PubMed] [Google Scholar]
- 9.Wood KB, Popp CA, Transfeldt EE, Geissele AE. Radiographic evaluation of instability in spondylolisthesis. Spine. 1994;19(15):1697–1703. doi: 10.1097/00007632-199408000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Luk KD, Chow DH, Holmes A. Vertical instability in spondylolisthesis: a traction radiographic assessment technique and the principle of management. Spine. 2003;28(8):819–827. doi: 10.1097/00007632-200304150-00016. [DOI] [PubMed] [Google Scholar]
- 11.Lowe RW, Hayes TD, Kaye J, Bagg RJ, Luekens CA. Standing roentgenograms in spondylolisthesis. Clin Orthop Relat Res. 1976;117:80–84. [PubMed] [Google Scholar]
- 12.Penning L, Blickman JR. Instability in lumbar spondylolisthesis: a radiologic study of several concepts. Am J Roentgenol. 1980;134(2):293–301. doi: 10.2214/ajr.134.2.293. [DOI] [PubMed] [Google Scholar]
- 13.Thome C, Zevgaridis D, Leheta O, Bazner H, Pockler-Schoniger C, Wohrle J, Schmiedek P. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3(2):129–141. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 14.Epstein NE. Decompression in the surgical management of degenerative spondylolisthesis: advantages of a conservative approach in 290 patients. J Spinal Disord. 1998;11(2):116–122. doi: 10.1097/00002517-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245(1):62–77. doi: 10.1148/radiol.2451051359. [DOI] [PubMed] [Google Scholar]
- 16.Leone A, Cassar-Pullicino VN, Guglielmi G, Bonomo L. Degenerative lumbar intervertebral instability: what is it and how does imaging contribute? Skeletal Radiol. 2009;38(6):529–533. doi: 10.1007/s00256-009-0646-5. [DOI] [PubMed] [Google Scholar]
- 17.Nachemson AL, Schultz AB, Berkson MH. Mechanical properties of human lumbar spine motion segments. Influence of age, sex, disc level, and degeneration. Spine. 1979;4(1):1–8. doi: 10.1097/00007632-197901000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Friberg O. Lumbar instability: a dynamic approach by traction-compression radiography. Spine. 1987;12(2):119–129. doi: 10.1097/00007632-198703000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion extension in asymptomatic individuals. Spine. 1989;14(3):327–331. doi: 10.1097/00007632-198903000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Pennal GF, Conn GS, McDonald G, Dale G, Garside H. Motion studies of the lumbar spine: a preliminary report. J Bone Joint Surg Br. 1972;54(3):442–452. [PubMed] [Google Scholar]
- 21.Wiltse LL, Hutchinson RH. Surgical treatment of spondylolisthesis. Clin Orthop Relat Res. 1964;35:116–135. [PubMed] [Google Scholar]
- 22.McGregor AH, McCarthy ID, Hughes SP. Motion characteristics of the lumbar spine in the normal population. Spine. 1995;20(22):2421–2428. doi: 10.1097/00007632-199511001-00009. [DOI] [PubMed] [Google Scholar]
- 23.Pearcy M, Portek I, Shepherd J. The effect of low-back pain on lumbar spinal movements measured by three-dimensional X-ray analysis. Spine. 1985;10(2):150–153. doi: 10.1097/00007632-198503000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Quinnell RC, Stockdale HR. Flexion and extension radiography of the lumbar spine: a comparison with lumbar discography. Clin Radiol. 1983;34(4):405–411. doi: 10.1016/S0009-9260(83)80224-4. [DOI] [PubMed] [Google Scholar]
- 25.Panjabi M, White AA., 3rd A mathematical approach for three-dimensional analysis of the mechanics of the spine. J Biomech. 1971;4(3):203–211. doi: 10.1016/0021-9290(71)90005-4. [DOI] [PubMed] [Google Scholar]