Abstract
Objective
To evaluate the effects of cervical artificial disc replacement (ADR) and anterior discectomy and fusion (ACDF) on adjacent spinal alignments.
Methods
The cohort consisted of 33 patients who undergone single-level cervical ADR (15 patients) and ACDF (18 patients) for radiculopathy, who had not had any previous spine surgery, and who had a minimum follow-up of 2 years. Whole-spine lateral radiographs were taken at the pre-operative and follow-up consultations. Cervical lordosis, thoracic kyphosis, lumbar lordosis, and sagittal balance were measured each time. The patients filled out pre-operative and follow-up functional evaluation forms including visual analogue scale (VAS) of neck and arm. The mean follow-up durations of patients who had cervical ADR and ACDF were 28 ± 5.0 and 30 ± 5.8 months, respectively. The patients having ACDF had the higher mean age (53 ± 9.0 years) than that of patients with cervical ADR (45 ± 11.7 years).
Results
The cervical lordosis and thoracic kyphosis in cervical ADR group increased significantly more than those of the ACDF group in follow-up assessment (P = 0.011 and 0.012). There was no significant change of lumbar lordosis in intra- and inter-group analyses. The follow-up sagittal balances for the cervical ADR and ACDF groups moved towards a neutral value. Although the follow-up neck and arm VAS of the both groups improved than those of the pre-operative status, the groups did not differ significantly except for a difference in neck VAS, which improved more after ADR.
Conclusions
The remodeling of cervical and thoracic curves after cervical ADR and ACDF was coupled and complementary. Cervical ADR contributed the restorations of angulations of cervical and thoracic spines. The neck VAS improved more after cervical ADR than after ACDF.
Keywords: Spine, Thoracic, Cervical, Alignment, Artificial disc
Introduction
Anterior cervical discectomy and fusion (ACDF) has been performed on patients with cervical spondylotic radiculopathy for the past 50 years, and successful fusion rates and excellent clinical outcomes have been reported following ACDF [1–3]. However, ACDF reduces the range of neck motion and increases adjacent segment degeneration (ASD) during the long-term follow-up period [4, 5]. Therefore, cervical artificial disc replacement (ADR) has emerged as an alternative to ACDF, and it has been reported that cervical ADR is advantageous in maintaining the range of motion and preventing ASD, thus, the artificial disc can allow normal physiological curvatures [6–8]. Therefore, cervical ADR could reproduce normal kinematics after implantation and cervical fusion alters spinal biomechanics to initiate or accelerate the ASD [9, 10]. Thus, cervical ADR and ACDF could influence adjacent spinal alignment. However, there was no report about the changes of other spinal curves except cervical lordosis after cervical ADR. The purpose of this study was to evaluate the effects of cervical ADR and ACDF on the other spinal alignment using changes of sagittal balance and the curves of the thoracic and lumbar spines.
Materials and methods
Study population
Between July 2007 and December 2008, the cohort for this study consisted of 33 consecutive patients who were operated by two senior surgeons for cervical degenerative radiculopathy using cervical ADR or ACDF. The patients met the following criteria: (1) they had upper extremity radiculopathy that were refractory to conservative treatments including medication and physiotherapy for a minimum of 6 weeks, (2) they had not had any previous spine surgery and, (3) they had a minimum follow-up of 2 years. After the patients were informed of advantages and disadvantages of cervical ADR and ACDF using written informed consent, they chose one among the two kinds of surgery. The study using cervical arthroplasty was approved by the university’s Ethics Committee.
There were 15 patients in cervical ADR group of mean age 45 years (range 17–61) and 18 patients in the ACDF group of mean age 53 years (range 38–66). The number of male patients in the ADR and ACDF were 5 and 8, respectively. Mean follow-up duration of cervical ADR group was 28 ± 5.0 months (range 24–37 months), and mean duration of the ACDF group was 30 ± 5.8 months (range 24–38). Cervical discs at lower level, such as, the disc between C5 and C6 or between C6 and C7, were most common in both groups.
Surgical technique
All patients underwent a standard Smith–Robinson approach [8]. The operative techniques were same in both groups. The cartilage portion of the endplate was removed with a curette to avoid the destruction of the bony endplate, and the uncovertebral joints were left intact. The posterior longitudinal ligament was removed, and the cervical cord and roots were decompressed in all patients. The cervical ADR group underwent arthroplasty with an artificial disc (Mobi-C disc, LDR Medical, Troyes, France). The Mobi-C disc consists of three pieces (two metal base plates and one mobile core of ultrahigh-molecular-weight polyethylene). The ACDF group was undertaken fusion operation with stand alone cage (MC+, LDR Medical) filled with allograft.
Outcome assessment
Pre-operative and follow-up whole-spine radiographs in the standing position were obtained pre-operatively and at 12, 24, and the last follow-up months after surgery. The radiographic parameters, including sagittal balance, cervical lordosis (C2–C7), thoracic kyphosis (T4–T12), and lumbar lordosis (L1–S1), were measured using the C7 plumb line deviation and the Cobb method with PACS software (M-view, Marosis, Seoul, Korea). Sagittal balance was determined from the deviation of the C7 plumb line, originating at the middle of the C7 vertebral body, from the posterosuperior corner of the S1 vertebra (Fig. 1) [11]. The lordotic angle was expressed as a negative value and the kyphotic angle was expressed as a positive value. The development of new spondylotic changes in the adjacent vertebral bodies or a decrease of more than 10% in the height of the adjacent discs was considered to indicate ASD.
Fig. 1.
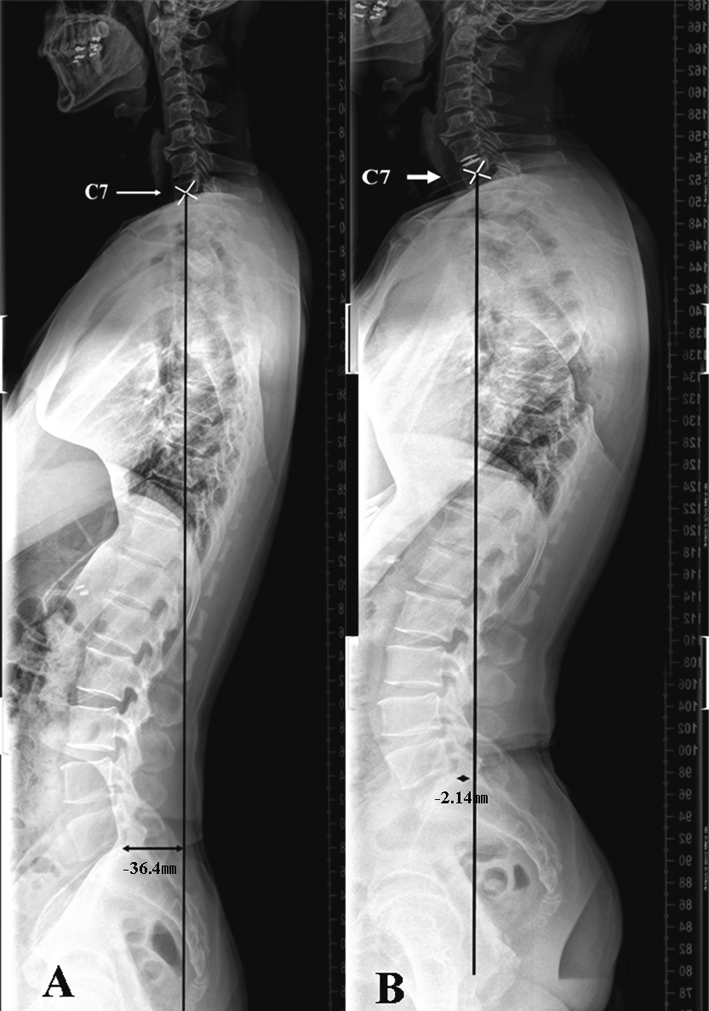
The sagittal vertical axis is the horizontal distance (arrow) from the line starting from the center of C7 and running perpendicular to the posterosuperior corner of the sacrum. a Pre-operative whole-spine lateral view shows loss of cervical lordosis and negative sagittal balance. b Post-operative whole-spine lateral view shows restoration of cervical lordosis, increased thoracic kyphosis and lumbar lordosis, and movement of sagittal balance to a neutral point
The clinical evaluation was performed using neck and arm pain intensities,which were assessed on visual analogue scale (VAS). The patients were asked to check neck and arm VAS ratings before surgery and each time of follow-up period at the surgeon’s clinic. The VAS for pain intensity ranged from 0 to 10 (0 = no pain, 10 = worst pain). Among the follow-up assessments, 1-year follow-up and the late follow-up (over 2 years) data including radiological and clinical assessments were analyzed.
Statistical analysis
The results were presented as means ± standard deviations. Mann–Whitney U test and Wilcoxon signed rank test were used to assess the statistical differences in the radiological and clinical data using SPSS software version 12.0. A value of P < 0.05 was considered significant.
Results
Spinal alignments
Although pre-operative sagittal balances in the cervical ADR and ACDF groups were positive and negative, respectively, the last follow-up balance in both groups move towards a more neutral value. There was no significant difference in pre-operative and the last follow-up values of sagittal balance between two groups (P = 0.062 and 0.489).
For the ACDF group, the cervical lordosis and thoracic kyphosis had been decreasing during follow-up period. However, cervical and thoracic curves of the cervical ADR group had been increasing post-operatively and difference of cervical Cobb angles between the pre-operative and 1 year was significant (−6.1 ± 8.71 vs. −10.1 ± 8.95, P = 0.022) and the comparison with the last follow-up was also significant (−6.1 ± 8.71 vs. −16.7 ± 6.32, P = 0.010). The difference of thoracic kyphosis between the pre-operative and the last follow-up was significant (21.6 ± 9.60 vs. 34.0 ± 9.06, P = 0.005). The differences of cervical and thoracic curves at the last follow-up between two groups were significant (P = 0.011 and 0.012). There was no significant change of lumbar lordosis in two groups in follow-up period (Table 1; Fig. 2).
Table 1.
Radiological data of cervical ADR and ACDF groups
| ACDF | ADR | P value | |
|---|---|---|---|
| Sagittal balance (SB) | |||
| Pre-operative SB | 15.6 ± 39.69 | −13.0 ± 36.45 | 0.062 |
| Post-operative SB (1 year) | 11.2 ± 32.73 | −8.6 ± 22.83 | 0.142 |
| Post-operative SB (>2 years) | 6.0 ± 19.54 | −0.9 ± 17.78 | 0.489 |
| Cervical lordosis (CL) | |||
| Pre-operative CL | −9.7 ± 9.00 | −6.1 ± 8.71 | 0.326 |
| Post-operative CL (1 year) | −7.3 ± 8.05 | −10.1 ± 8.95 | 0.439 |
| Post-operative CL (>2 years) | −6.7 ± 7.24 | −16.7 ± 6.32 | 0.011 |
| Thoracic kyphosis (TK) | |||
| Pre-operative TK | 27.6 ± 10.07 | 21.6 ± 9.60 | 0.142 |
| Post-operative TK (1 year) | 23.2 ± 10.95 | 25.0 ± 10.29 | 0.726 |
| Post-operative TK (>2 years) | 19.5 ± 11.09 | 34.0 ± 9.06 | 0.012 |
| Lumbar lordosis (LL) | |||
| Pre-operative LL | −42.1 ± 22.08 | −42.3 ± 10.32 | 0.983 |
| Post-operative LL (1 year) | −41.2 ± 8.93 | −50.5 ± 9.37 | 0.043 |
| Post-operative LL (>2 years) | −44.2 ± 10.52 | −46.7 ± 11.04 | 0.649 |
ACDF anterior cervical discectomy and fusion, ADR artificial disc replacement
Fig. 2.
The mean sagittal balance and cervical, thoracic, and lumbar curves were measured before the operation, 1 year after the operation, and at the last follow-up (more than 2 years) in the cervical ADR and ACDF groups. Both groups showed neutralization of sagittal balance post-operatively. The segmental curves in the cervical and thoracic spines increased significantly in the cervical ADR group. Lumbar lordosis did not change significantly in either group. SB sagittal balance, CL cervical lordosis, TK thoracic kyphosis, LL lumbar lordosis, A ACDF group, T cervical artificial disc replacement
The pre-operative and the last follow-up values for cervical lordosis and thoracic kyphosis were strongly inversely correlated in the total cohort (n = 33) (rs = −0575, P = 0.005 and rs = −0689, P = 0.004).
Adjacent segment degeneration (ASD) and subsidence
Eight patients (8/18, 44.4%) in the ACDF group and four patients (4/15, 26.7%) in the cervical ADR group had ASD at follow-up. There was no significant difference in incidence of ASD between the two groups (P = 0.433). There was no subsidence in cervical ADR group. However, six patients (6/18, 33.3%) in the ACDF group had subsidence at follow-up and there was significant difference of incidence of subsidence between two groups (P = 0.035).
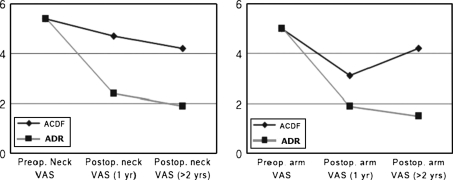
Clinical outcomes
The mean arm and axial VAS scores in two groups were improved at 1 year follow-up and the last follow-up and there was a significant difference of neck VAS at 1 year follow-up between two groups (Table 2; Fig. 3).
Table 2.
Clinical data of cervical ADR and ACDF groups
| ACDF | ADR | P value | |
|---|---|---|---|
| Neck visual analogue scale (VAS) | |||
| Pre-operative VAS | 5.4 ± 2.80 | 5.4 ± 3.67 | 0.962 |
| Post-operative. VAS (1 year) | 4.7 ± 2.71 | 2.4 ± 2.32 | 0.033 |
| Post-operative VAS (>2 years) | 4.2 ± 3.33 | 1.9 ± 2.17 | 0.084 |
| Arm VAS | |||
| Pre-operative VAS | 5.0 ± 2.86 | 5.0 ± 3.83 | 1.000 |
| Post-operative VAS (1 year) | 3.1 ± 2.85 | 1.9 ± 2.13 | 0.300 |
| Post-operative VAS (>2 years) | 3.6 ± 3.38 | 1.5 ± 1.64 | 0.150 |
ACDF anterior cervical discectomy and fusion, ADR artificial disc replacement
Fig. 3.
The neck and arm VAS scores measured before the operation, 1 year after the operation, and at the last follow-up (more than 2 years) in the cervical ADR and ACDF groups. The clinical outcomes improved post-operatively. The difference in post-operative axial VAS at 1 year was significant. VAS visual analogue scale
In intragroup analysis of cervical ADR group, difference of mean arm VAS scores between pre-operative and 1 year follow-up periods was significant (5.0 ± 3.83 vs. 1.9 ± 2.13, P = 0.003). And, mean arm VAS score at last follow-up was improved significantly than pre-operative score (5.4 ± 3.67 vs. 1.9 ± 2.17, P = 0.008). However, in ACDF group, there was only a significant difference of mean arm VAS between pre-operative and 1-year follow-up scores (5.0 ± 2.86 vs. 3.1 ± 2.85, P = 0.034).
Complications
There was no complication related to the surgical procedures or devices observed during the follow-up period. No patient underwent spine surgery due to ASD or other causes related to spine problem in the follow-up period.
Discussion
Although ACDF is a common standard procedure for the treatment of cervical spondylosis and has excellent clinical outcomes, many studies have demonstrated that the patients treated with ACDF have degenerative changes and hypermobility in the adjacent segments of the spine, including osteophyte formation, endplate sclerosis, and disc space narrowing during the long-term follow-up period [1, 9, 12]. It is clear that ACDF contributes to the biomechanical remodeling of the spine including the limitation of motion, and predicts increased intradiscal pressures at levels adjacent to the cervical fusion [9]. However, cervical ADR allows ASD to be avoided and the range of motion to be maintained [5, 13]. These advantages may be the consequences of the preservation of the normal cervical kinematics after cervical ADR. A study using Bryan cervical artificial disc (Medtronic Sofamor Danek, Memphis, TN) with mobile core was used demonstrated that the artificial disc maintained overall sagittal balance of the cervical spine during the follow-up period [13].
As the cervical spine is a mobile structure, the biomechanical changes to the cervical spine could affect the adjacent segments. Park et al. [14] reported that spine seems to rebalance itself after cervical ACDF or ADR. In the correlation analysis of this study, cervical and thoracic curves had a strongly negative correlation. In other words, a coupling change of cervical and thoracic curves happens after cervical ADR or ACDF and this change might affect sagittal vertical axis of whole-spine. Although changes of cervical and thoracic curves were found to be strongly related, thoracic curve changes and sagittal vertical axis shifts could have been influenced by pelvic parameters. Therefore, we recommend that an analysis of pelvic parameters be included in any future study.
In this study, the incidences of ASD and subsidence for cervical ADR were lower than those of ACDF. However, the difference in the incidence of ASD was not significant. This is probably attributable to the size of the difference between incidences of ASD in the two groups or the small number of patients enrolled. Had the rate of ASD in the ACDF group been three times higher than in the ADR group or the number of patients been increased, the ASD incidence difference would have been significant. The difference of incidence of subsidence can affect the cervical lordosis after surgery.
Among results of clinical assessments, the neck VAS at the last follow-up for cervical ADR group was significantly improved. These results demonstrate that cervical ADR contributes more to biomechanical changes in the cervical and thoracic spines than does ACDF.
This study has some limitations, such as non-randomisation, retrospective design and the small sample size. Further studies with a randomized prospective design and large samples are required to evaluate more precisely, the meaning of the correlation between sagittal alignment and clinical outcome following cervical ADR and ACDF.
Conclusion
The functional outcomes improved more after cervical ADR than after ACDF. The restoration of cervical lordosis after cervical ADR was more effective than that of ACDF. The change of cervical lordosis after cervical fusion or arthroplasty affected the thoracic curve.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST) (2011-0018259).
Conflict of interest None of the authors has any potential conflict of interest.
References
- 1.Bose B. Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol. 1998;49:25–31. doi: 10.1016/S0090-3019(97)00306-6. [DOI] [PubMed] [Google Scholar]
- 2.Cloward RB. Cervical diskography; technique, indications and use in diagnosis of ruptured cervical disks. Am J Roentgenol Radium Ther Nucl Med. 1958;79:563–574. [PubMed] [Google Scholar]
- 3.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Calenbergh F, Loon J. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 5.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24:670–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 6.Liu F, Cheng J, Komistek RD, Mahfouz MR, Sharma A. In vivo evaluation of dynamic characteristics of the normal, fused, and disc replacement cervical spines. Spine. 2007;32:2578–2584. doi: 10.1097/BRS.0b013e318158cdf8. [DOI] [PubMed] [Google Scholar]
- 7.Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using mobi-c(r) and anterior cervical discectomy and fusion using the solis(r)-cage. J Korean Neurosurg Soc. 2008;44:217–221. doi: 10.3340/jkns.2008.44.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3:417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 9.Kim SW, Shin JH, Arbatin JJ, Park MS, Chung YK, McAfee PC. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17:20–29. doi: 10.1007/s00586-007-0459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine. 2007;32:2933–2940. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 11.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 12.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993;18:2167–2173. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V, Calenbergh F, Loon J. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002;51:840–845. doi: 10.1227/00006123-200209000-00048. [DOI] [PubMed] [Google Scholar]
- 14.Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion. Spine. 2011;36:721–730. doi: 10.1097/BRS.0b013e3181df10fc. [DOI] [PubMed] [Google Scholar]