Abstract
Purpose
The purpose of this study is to investigate if lumbar disc pathology identified on MRI scans is more common in patients with acute, likely discogenic, low back pain than matched controls.
Methods
We compared rates of MRI findings between 30 cases with low back pain and 30 pain-free controls. Cases were patients presenting for care with likely discogenic low back pain (demonstrated centralisation with repeated movement testing), of moderate intensity and with minimal past history of back pain. Controls were matched for age, gender and past history of back pain. Cases and controls underwent MRI scanning which was read for the presence of a range of MRI findings by two blinded assessors.
Results
The presence of disc degeneration, modic changes and disc herniation significantly altered the odds of a participant being a case or control. For example subjects were 5.2 times more likely to be a case than a control when disc degeneration grade of ≥3 was present, and 6.0 times more likely with modic changes. The presence of a high-intensity zone or annular tear was found to significantly alter odds for one assessor but not the other assessor.
Conclusion
MRI findings including disc degeneration, modic changes and herniation are more common in selected people with current acute (likely discogenic) low back pain than in controls without current low back pain. Further investigation of the value of MRI findings as prognostic factors and as treatment effect modifiers is required to assess the potential clinical importance of these findings.
Keywords: Low back pain, Magnetic resonance imaging, Case–control study, Diagnosis, Sensitivity, Disc degeneration
Introduction
International clinical practice guidelines report that it is not possible in primary care to identify a tissue source for the majority of patients presenting with low back pain and recommend the term non-specific low back pain to convey the diagnostic uncertainty [1, 2]. It is suggested that 90–95% of patients with low back pain have non-specific low back pain [1, 2]. Despite hundreds of trials of different treatments for non-specific low back pain there has been no major breakthrough; the treatments have been shown to only have small to moderate effects [3, 4]. In most areas of medicine diagnosis is considered the cornerstone of effective management and it is possible that identifying the tissue source of low back pain may open the way for more effective therapies and so provide a breakthrough that is needed for this major health problem.
A difficulty when investigating potential pathoanatomic sources of low back pain is the lack of accepted gold standards. Recommended reference tests for the most common tissue sources of low back pain (disc, facet joint and sacroiliac joint) are controversial and involve invasive, painful and expensive diagnostic injections [5]. These reference tests are not appropriate for the majority of patients with low back pain and importantly do not aim to differentiate between different pathology of the target structure. For example discography, provides no information about what pathology of the disc (e.g. degeneration, annular tear, endplate changes etc.) may be responsible for the pain [5, 6]. MRI on the other hand has the potential, in a non-invasive manner, to identify pathology of tissues in the spine, including the disc, which may be a source of low back pain [7]. We recently published a diagnostic systematic review of clinical and radiological tests for low back pain which found that certain features on MRI scans increase the likelihood of the disc being the source of low back pain [8], based on the existing invasive reference standard of discography.
A common argument against the validity of MRI as a non-invasive tool to identify pathoanatomical sources of low back pain is that positive findings are reported on MRI in people without low back pain [9, 10]. However, few studies have compared the rate of MRI findings in people with and without low back pain. A recent large population-based study found that although disc degeneration was common; its presence was associated with low back pain [11].
There are problems with the methods and interpretation of previous studies, so it remains unclear what real value MRI findings have. Many previous studies reporting positive MRI findings in people without current LBP have not controlled for past history of LBP, so it is not clear if the MRI findings represent previous LBP episodes. The presence of MRI findings in currently asymptomatic people may represent markers of ongoing disease that is characterised by episodes of pain and disability. Previous studies typically include a proportion of older people [10, 12] in whom the likelihood of degenerative findings is increased. Most previous studies have focussed on degenerative disc findings or disc herniation and few have investigated a range of different pathologies on MRI including annular tears, and Modic (endplate) changes. An important limitation of most previous studies investigating MRI in people with low back pain is the inclusion of heterogeneous cases based on the symptom of low back pain. For example, studies investigating pathoanatomic findings of the disc include cases with low back pain with no evidence of their pain originating from the disc rather than other spinal structures. Based on previous research the best estimate would be that approximately 40% of these cases were true cases with discogenic pain [7]. Including a large proportion of people with low back pain originating from other structures will mask a potential association between disc pathology on MRI and presence of discogenic low back pain. There is currently no perfect solution to this problem as no gold standard for discogenic low back pain exists. However, several previous studies [8, 13, 14] have shown the centralisation phenomenon has high specificity for discogenic low back pain (positive discography). By recruiting patients who demonstrate centralisation, a more heterogeneous group likely to have discogenic low back pain can be assembled. Many of the patients included in previous studies had chronic low back pain. These patients are known to have higher levels of centrally generated or enhanced pain and are, therefore, a sub-optimal group to identify markers of a local pain producing pathology in the lumbar spine.
The aim of the current study was, therefore, to investigate if lumbar disc pathology identified on MRI scans can discriminate patients with current acute low back pain of likely discogenic origin from asymptomatic controls matched for low back pain history, age and gender.
Methods
The study used a case–control design. Ethical approval was gained through the University of Sydney Human Research Ethics Committee.
Participants/inclusion criteria
Cases were 30 consecutive patients with low back pain (with or without leg pain or sciatica) who presented to physiotherapy clinics in Sydney, Australia and met the inclusion criteria. Patients were required to be between 18 and 50 years of age, have at least moderate pain (measured using SF-36 question 7) of less than 6 weeks duration and no known or suspected serious spinal pathology. To increase the likelihood of cases having pain generated from one of the lumbar discs all patients needed to demonstrate centralisation (progressive retreat of referred pain towards the midline of the back in response to standardised testing of repeated movements) as assessed by an experienced clinician. Based on data from a previous systematic review [8] 84% of patients who demonstrated centralisation had positive discography. To minimise the influence of previous back pain, patients were required to have had no episodes of low back pain (lasting more than 72 h causing the patient to seek treatment or change activity) in the last 12 months and no more than two episodes during their lifetime.
Controls were 30 people matched for age (±3 years), sex, and previous history of low back pain. Previous history was matched as either no prior episodes of low back pain or 1–2 prior episodes. Controls were recruited through advertisements within our institution and through word of mouth.
Procedures
Cases and controls that met the inclusion criteria and volunteered to participate were contacted by one of the researchers through phone. Baseline data including demographic information, and details of the current episode (cases only) and any past episodes of low back pain were recorded (Table 1). Participants were then scheduled for an MRI scan as soon as possible and within 1 week. MRI scans were performed on a single 1.5-T scanner. T1 and T2 sagittal and T2 axial scans were performed with 4-mm thick slices and a 1-mm gap. All participants underwent an identical MRI protocol including T1 and T2-weighted sagittal scans and T2-weighted axial scans of the lumbar spine. Spin echo sequences were 3,425/102 for sagittal T2, 500/minimum full for sagittal T1 and 3,150/102 for axial T2. Field of view was 32 cm for sagittal T1 and T2 and 20 cm for Axial T2.
Table 1.
Participant information
| Participant characteristic | Cases | Controls |
|---|---|---|
| Male gender | 53% | 53% |
| Age (years) | 36.8 (7.4) | 36.6 (7.4) |
| Height (cm) | 172.7 | 172.3 |
| Pain | 6.5 (1.6) | 0.0 |
| Pain extends below knee | 10% | N/A |
| Duration of episode (days) | 8.9 (8.9) | N/A |
| Previous episode of low back pain (%) | 50% | 50% |
Continuous data are mean values (SD); Pain was rated on a 0–10 scale
Reporting of MRI scans
After all participants had undergone their MRI scan two reviewers reported on all scans according to the study protocol. The reviewers were a radiologist specialising in spinal conditions and a spinal neuro-surgeon. The reviewers were blinded to the participants’ status (case or control), baseline participant data and the ratings of the other reviewer. MRI features reported on included disc degeneration [15], high-intensity zone [16], Modic changes [17], annular tears [17] and disc herniation [17]. Each reviewer reported on each study MRI feature, for each lumbar disc according to the study guidelines as described in Table 2. To enhance consistency both raters were provided with detailed descriptions of the criteria for rating each feature including pictures where appropriate. Any questions regarding the criteria were discussed and the other rater was informed. Based on these ratings the presence or absence of each feature in the entire lumbar spine (L1/2 to L5/S1) was determined and used in the analyses. For disc degeneration the worst rating at any single level (1–5) was used.
Table 2.
MRI scoring options and criteria
| MRI feature | Scoring options | Scoring criteria/guidelines |
|---|---|---|
| Disc degeneration | Grade 1–5 | As per Pfirrmann et al. [15] |
| High-intensity zone | Yes or no | As per April and Bogduk [16] |
| Modic changes | No, grade 1, 2, or 3 | As per Fardon et al. [17] |
| Annular tears | Yes or no | As per Fardon et al. [17] |
| Disc herniation | Nil, bulge, protrusion, extrusiona | As per Fardon et al. [17] |
aProtrusions and extrusion were considered as herniations while bulges were considered as negative
Statistical analysis
We assessed the reliability of ratings between the two assessors for each MRI feature using Kappa for dichotomous outcomes and ICC for the single continuous outcome. For each individual MRI feature we calculated the sensitivity, specificity, positive likelihood ratio (LR+) and percent correctly classified for each assessor individually. For the variable worst disc degeneration (1–5 scale) we used area under the receiver operating curve to describe the overall predictive ability of the test when assessed across a range of threshold values. We further examined each MRI feature using logistic regression. For disc degeneration we decided a priori to investigate thresholds of ≥3 and ≥4. To assess the diagnostic value of combinations of MRI findings we performed forward multiple logistic regressions. MRI findings were considered as candidate variables for the multiple logistic regression if the p value for the univariate model was <0.2. While we investigated several threshold values for the MRI findings with worst disc degeneration, we only entered worst disc degeneration variable based on raw values (1–5 scale) into the multivariate model. We treated this as a continuous variable after testing the linearity assumption by comparing −2loglikelihood values. Separate multivariate models were generated for each assessor.
Within the cohort of controls we performed secondary analyses to investigate if past history of low back pain influenced the rate of MRI findings in controls. Linear regression was used to assess if previous low back pain was predictive of worst disc degeneration score in control participants.
Results
Baseline characteristics of the cases and controls are presented in Table 1. The mean age of participants was 37 and just over half were male (53%). Cases had moderate levels of pain, relatively short duration of symptoms and 50% had no previous LBP while 50% had 1–2 previous episodes.
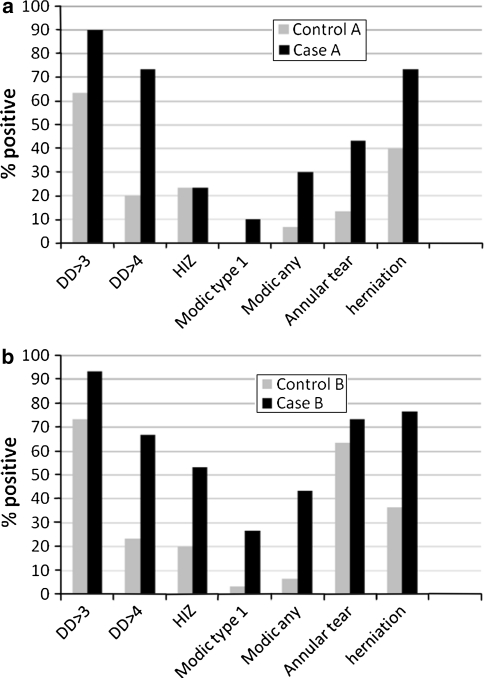
The reliability of most MRI findings was moderate to good (k = 0.46–0.81) apart from annular tear which was poor (k = 0.02) (Table 3). All MRI findings investigated were more common in cases than in controls (Fig. 1). The sensitivity, specificity and proportion correctly classified for each MRI finding are presented in Table 4. The area under the curve for worst disc degeneration (1–5 scale) was 0.79 for assessor A and 0.74 for assessor B. Based on the results of the univariate logistic regression the presence of disc degeneration (1–5), disc degeneration ≥4, modic changes type 1, any modic changes and disc herniation significantly alters the odds of a participant being a case or control for both assessors (Table 5). The presence of the MRI findings high-intensity zone or annular tear was found to significantly alter odds for one assessor but not the other assessor (Table 5). For both assessors the only variable remaining in the multivariate model was worst disc degeneration.
Table 3.
Reliability between assessors A and B
| MRI feature | Prevalencea | Kappa or ICC (95% CI) | Observed agreement |
|---|---|---|---|
| DDW (0–5) | N/A | 0.81 (0.70–0.88) (ICC) | 65% exact 100% within 1 grade |
| DD ≥ 3 | 80% | 0.69 (0.46–0.92) | 90% |
| DD ≥ 4 | 46% | 0.77 (0.60–0.93) | 88% |
| HIZ | 30% | 0.46 (0.22–0.69) | 77% |
| Modic type 1 | 10% | 0.46 (0.11–0.80) | 90% |
| Modic any | 22% | 0.80 (0.62–0.99) | 93% |
| Annular tear | 48% | 0.02 (−0.16–0.20) | 43% |
| Herniation | 57% | 0.59 (0.39–0.80) | 80% |
DDW, disc degeneration score (0–5 scale) at the worst lumbar level; DD ≥ 3, participants with a disc degeneration score ≥3 at any level (%); DD ≥ 4, participants with a disc degeneration score ≥4 at any level (%), HIZ, participants with a high-intensity zone at any level (%)
aPrevalence is based on average of the two raters, ICC was used for DDW
Fig. 1.
Proportion of positive MRI findings for cases and controls. a Represents finding for assessor A. b Represents findings for assessor B. DD ≥ 3, participants with a disc degeneration score ≥3 at any level (%); DD ≥ 4, participants with a disc degeneration score ≥4 at any level (%); HIZ, participants with a high-intensity zone at any level (%)
Table 4.
Diagnostic accuracy of each test for both assessors independently
| Sens A | Sens B | Spec A | Spec B | Correctly classified A (%) | Correctly classified B (%) | LR+ (A) | LR+ (B) | |
|---|---|---|---|---|---|---|---|---|
| DD ≥ 2 | 0.97 (0.83–1.00) | 1.0 (0.88–1.00) | 0.20 (0.08–0.39) | 0.00 (0.00–0.12) | 58 | 50 | 1.2 (1.0–1.4) | 1.0 (1.0–1.0) |
| DD ≥ 3 | 0.90 (0.73–0.98) | 0.93 (0.78–0.99) | 0.37 (0.20–0.56) | 0.27 (0.12–0.46) | 63 | 60 | 1.4 (1.1–1.9) | 1.3 (1.0–1.6) |
| DD ≥ 4 | 0.73 (0.54–0.88) | 0.67 (0.47–0.83) | 0.80 (0.61–0.92) | 0.77 (0.58–0.90) | 77 | 72 | 3.7 (1.7–7.7) | 2.9 (1.4–5.7) |
| DD ≥ 5 | 0.07 (0.00–0.22) | 0.03 (0.00–0.17) | 1.0 | 1.0 (0.88–1.0) | 53 | 52 | ∞ | ∞ |
| HIZ | 0.23 (0.10–0.42) | 0.53 (0.34–0.72) | 0.77 (0.58–0.90) | 0.80 (0.61–0.92) | 50 | 67 | 1.0 (0.40–0.25) | 2.7 (1.2–5.9) |
| Modic type 1 | 0.10 (0.02–0.27) | 0.27 (0.12–0.46) | 1.0 (0.88–1.00) | 0.97 (0.83–1.00) | 55 | 62 | ∞ | 8.0 (1.1–60.1) |
| Modic any | 0.30 (0.15–0.49) | 0.43 (0.25–0.63) | 0.93 (0.78–0.99) | 0.93 (0.78–0.99) | 62 | 68 | 4.50 (1.1–19.1) | 6.5 (1.6–26.4) |
| Annular tear | 0.43 (0.25–0.63) | 0.73 (0.54–0.88) | 0.87 (0.69–0.96) | 0.37 (0.20–0.56) | 65 | 58 | 3.3 (1.2–8.8) | 1.2 (0.8–1.6) |
| Herniation | 0.73 (0.54–0.88) | 0.77 (0.58–0.90) | 0.60 (0.41–0.77) | 0.63 (0.44–0.80) | 67 | 70 | 1.8 (1.1–3.0) | 2.1 (1.3–3.5) |
DD ≥ 2, disc degeneration score ≥2 at any single level
A reviewer A, B reviewer B, HIZ high-intensity zone
Table 5.
Logistic regression for univariate analyses
| Explanatory variable | Assessor A | Assessor B | ||
|---|---|---|---|---|
| Exp B (CI) | P value | Exp B (CI) | P value | |
| DD worst (0–5) | 3.32 (1.63–6.76) | 0.001 | 3.89 (1.67–9.057) | 0.002 |
| DD ≥ 3 | 5.21 (1.28–21.24) | 0.021 | 5.09 (0.98–26.43) | 0.053 |
| DD ≥ 4 | 11.00 (3.29–36.75) | 0.000 | 6.57 (2.11–20.48) | 0.001 |
| HIZ | 1.00 (0.30–3.31) | 1.0 | 4.57 (1.45–14.39) | 0.009 |
| Modic type 1 | Unable to calc | Unable to calc | 10.54 (1.23–90.66) | 0.032 |
| Modic any | 6.00 (1.17–30.73) | 0.032 | 10.71 (2.15–53.35) | 0.004 |
| Annular tear | 4.97 (1.39–17.82) | 0.014 | 1.59 (0.53–4.78) | 0.407 |
| Herniation | 4.13 (1.39–12.27) | 0.011 | 5.68 (1.84–17.49) | 0.003 |
DD ≥ 3, degenerative disc score ≥3 at any single level
HIZ high-intensity zone
Secondary analyses demonstrated no significant differences in rates of MRI findings between controls with 1–2 past episodes and those with no past history of low back pain. Mean worst level disc degeneration in controls with a past history of low back pain was 2.9 (SD = 1.1) (1–5 scale) compared with 2.4 (SD = 0.9) in controls with no past history of low back pain (p = 0.22). No Modic changes were reported by either rater for controls with an absence of past history of LBP, while two controls with a history of LBP had Modic changes. Herniations occurred in four cases without a past history of LBP and in seven cases with a past history of LBP. As we restricted the number of past episodes to a maximum of two, it is possible that greater differences would exist if those with no previous low back pain were compared to those with a greater number of past episodes.
Discussion
The results of this study demonstrate that several MRI findings are substantially more common in selected patients with likely discogenic low back pain than in matched controls. All MRI features investigated were present significantly more often in the cases than controls according to the ratings of at least one of the two MRI raters. Disc degeneration, Modic changes and herniation were present significantly more often in the people with back pain, based on ratings of both assessors. We did not find that a combination of MRI findings was able to more accurately differentiate between cases and controls than a single finding.
There was no one MRI finding that was clearly more important or powerful than the others. All dichotomous MRI findings had an estimated OR of greater than 4 for one of the assessors. The OR for disc degeneration, measured on a 5-point scale, was greater than 3 for both assessors. This represents the odds ratio for a single point change on the scale. Therefore, the odds of being a case (compared to control) would be approximately 9 times more likely for a participant with a disc degeneration score of 5 compared to 2. The multivariate analysis was unable to find a combination of MRI findings that was significantly better at discriminating cases and controls than single MRI findings. The results of the multivariate analysis suggest that disc degeneration may be one of the most important findings as this feature was the only feature included in the multivariate models. However, the high correlations between some of the MRI findings means these results are less robust and we suggest readers to focus primarily on the results of univariate analyses.
Previous studies have reported the presence of MRI findings (false positives) in people without low back pain. We similarly found that some MRI findings were reasonably common in controls without pain; however, the rates were lower than in those people with pain. The rate of disc degeneration in people without pain depended greatly on the threshold for disc degeneration. When a low threshold of ≥3 was used the mean rate for the two examiners was 68% (41/60, the denominator of 60 represents 30 patient MRIs read by 2 assessors). When this threshold was increased to ≥4 and ≥5, rates of degeneration in the controls reduced to 22% (13/60) and 0% (0/60), respectively. Therefore, mild levels of degeneration are common in controls but high levels are uncommon. Previous studies typically do not investigate different thresholds for disc degeneration [12]. A recent population study of 1,043 people found a significant association between the severity of disc degeneration and the presence of low back pain [11]. Together with our results this suggests the severity of disc degeneration is important to consider when evaluating the clinical significance of disc degeneration. In our study, HIZ occurred in 22% of controls and herniations were present in 38% of controls. Modic changes were rare in controls (7%), which is consistent with a recent systematic review reporting a prevalence of 6% in non-clinical populations [18]. The number of annular tears reported by our two MRI raters varied too much to provide any useful data on the prevalence of annular tears in controls.
Our controls consisted of 15 people with no history of low back pain and 15 with 1–2 previous episodes but no pain for the last year. Secondary analyses did not find significant differences in rates of MRI findings between controls with and without a history of low back pain. However, we were underpowered for this investigation and it is possible we missed a significant effect. Rates for all MRI findings, while not significantly different, were higher in controls with a past history of low back pain than in controls without previous low back pain. People with more than two previous episodes of past low back pain were not included in this study so the relationship between MRI findings and past history of low back pain might be stronger in those with many previous episodes. Future investigation is required to better understand the relationship between previous low back pain and MRI findings.
Our data and that of some previous studies demonstrates that there is an important association between the presence of MRI finding and low back pain. However, it is also clear that most MRI findings occur in people without low back pain at rates which mean the MRI findings cannot be used to confidently “diagnose” the source of most patients’ low back pain. This has led to many authors and leaders in the back pain field dismissing the value of MRI. This position, however, ignores the relatively strong association demonstrated between MRI findings and low back pain. It has long been understood that low back pain is a multifactorial biopsychosocial condition. We believe the current findings suggest that the biological component of low back pain is important for at least some patients and requires further investigation. Research is required to investigate MRI findings as predictors of the development and course of an episode of low back pain and also as effect modifiers for specific low back pain interventions.
An important difference between our study and previous research was the selection criteria for the cases. We included relatively young people, with minimal previous low back pain who demonstrated centralisation on their initial clinical examination. We included people who centralise to increase the probability that cases were true cases (likely to have discogenic low back pain). As the MRI findings we investigated were all associated with disc pathology we did not want to include cases who had low back pain from entirely different sources, e.g. facet joint or sacroiliac joint. The inclusion of these patients in previous studies may explain low sensitivity. However, the strict inclusion criteria (and case–control design) used in our trial limits the generalisability of the current findings to a clinical setting. For example our results will not necessarily generalise to people older than 50 where degenerative findings are more common. Our results may also be specific to acute low back pain and not generalise to patients with chronic low back pain where psychosocial factors or pain sensitisation may be more important. The aim of this study was not to test the diagnostic accuracy of MRI findings when used in a clinical setting. This study is explanatory and aimed to improve our understanding of MRI findings by selecting a specific group of patients in whom we believed it most likely that an association would exist. The results suggest that pathoanatomical findings identified on MRI in people with low back pain may identify a pain source in some patients. While findings do occur in people without pain they are more common in matched people with pain.
Conclusion
MRI findings including disc degeneration, modic changes and herniation are more common in selected people with current, acute (likely discogenic) low back pain than in controls without current low back pain. Further investigation of the value of MRI findings as prognostic factors and as treatment effect modifiers is required to assess the potential clinical importance of these findings.
Acknowledgments
This work was supported by Faculty of Health Sciences Grant, The University of Sydney.
Conflict of interest None.
References
- 1.Tulder M, Becker A, Bekkering T, Breen A, Real MTG, Hutchinson A, Koes B, Laerum E, Malmivaara A, Cost B13 Working Group on Guidelines for the Management of Acute Low Back Pain in Primary Care Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15(Suppl 2):S169–S191. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Australian Acute Musculoskeletal Pain Guidelines Group (2004) Evidence-based management of acute musculoskeletal pain—a guide for clinicians. Australian Academic Press, Bowen Hills
- 3.Deyo RA. Treatments for back pain: can we get past trivial effects? Ann Intern Med. 2004;141:957–958. doi: 10.7326/0003-4819-141-12-200412210-00012. [DOI] [PubMed] [Google Scholar]
- 4.Keller A, Hayden J, Bombardier C, Tulder M. Effect sizes of non-surgical treatments of non-specific low-back pain. Eur Spine J. 2007;16:1776–1788. doi: 10.1007/s00586-007-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Seattle: IASP Press; 1994. [PubMed] [Google Scholar]
- 6.Standards Committee of the International Spine Intervention Society (2004) International Spine Intervention Society practice guidelines for spinal diagnostic and treatment procedures In: Bogduk N (ed) International Spine Intervention Society
- 7.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995;20:1878–1883. doi: 10.1097/00007632-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hancock MJ, Maher CG, Latimer J, Spindler MF, McAuley JH, Laslett M, Bogduk N. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J. 2007;16:1539–1550. doi: 10.1007/s00586-007-0391-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 10.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403–408. [PubMed] [Google Scholar]
- 11.Cheung KM, Karppinen J, Chan D, Ho DW, Song YQ, Sham P, Cheah KS, Leong JC, Luk KD. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34:934–940. doi: 10.1097/BRS.0b013e3181a01b3f. [DOI] [PubMed] [Google Scholar]
- 12.Jarvik JJ, Hollingworth W, Heagerty P, Haynor DR, Deyo RA. The Longitudinal Assessment of Imaging and Disability of the Back (LAIDBack) Study: baseline data. Spine. 2001;26:1158–1166. doi: 10.1097/00007632-200105150-00014. [DOI] [PubMed] [Google Scholar]
- 13.Laslett M, Aprill CN, McDonald B, Oberg B, Laslett M, Aprill CN, McDonald B, Oberg B. Clinical predictors of lumbar provocation discography: a study of clinical predictors of lumbar provocation discography. Eur Spine J. 2006;15:1473–1484. doi: 10.1007/s00586-006-0062-7. [DOI] [PubMed] [Google Scholar]
- 14.Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine. 1997;22:1115–1122. doi: 10.1097/00007632-199705150-00011. [DOI] [PubMed] [Google Scholar]
- 15.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65:361–369. doi: 10.1259/0007-1285-65-773-361. [DOI] [PubMed] [Google Scholar]
- 17.Fardon DF, Milette PC, Combined Task Forces of the North American Spine Society ASoSR, American Society of N Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 18.Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17:1407–1422. doi: 10.1007/s00586-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]