Abstract
Purpose
The purpose of this study was to describe a free-hand pedicle screw insertion technique and to evaluate the accuracy of pedicle screw placement and validity of pedicle screw fixation in patients with subaxial cervical spine injuries.
Methods
We retrospectively reviewed 32 consecutive patients with subaxial cervical spine injuries who underwent posterior cervical fixation using our cervical pedicle screw (CPS) insertion technique. We also assessed the clinical and radiological outcomes and the accuracy of pedicle screw placement.
Results
The mean preoperative kyphosis was 4.0°, which was corrected to −5.2° after the operation, and the mean kyphosis angle was −4.4° at the final follow-up. The mean preoperative disc height ratio was 81.9%, and it improved to 105.4% after the operation, which was maintained until the final follow-up measurement of 103.4%. Bony union was achieved, and there were no instrumentation failures in any patient. Overall, 127 pedicle screws were inserted, of which 112 (88.1%) were classified as grade 1 (exact intrapedicular screw positioning), 10 (7.8%) as grade 2 (perforation <50% of the screw diameter), and 5 (3.9%) as grade 3 (perforation more than 50% of the screw diameter).
Conclusion
In our technique, a gutter is created using a high-speed burr at the transitional area between the lateral mass and lamina similar to the procedure in double-door laminoplasty to identify an entry point for CPS insertion. It is easy for general spine surgeons to identify a CPS insertion entry point using our technique.
Keywords: Accuracy, Cervical spine, Entry point, Pedicle screw
Introduction
The use of the pedicle screw system has become increasingly popular for treating an unstable cervical spine resulting from traumatic, degenerative, inflammatory, and neoplastic conditions. Because a cervical pedicle screw (CPS) has superior biomechanical stability as the lateral mass screw or transarticular screw [1, 2], pedicle screws allow for shorter instrumentation with improved spinal alignment. However, CPS insertion is technically demanding because of the anatomical variations in cervical pedicle size, lack of anatomical landmarks, small pedicle diameter, and the large transverse angle of cervical pedicles [3–5]. The potential risk of injury to neurovascular structures, such as the vertebral artery, spinal cord, or nerve roots, caused by CPS remains a great concern. Therefore, accurate and safe CPS insertion techniques are necessary.
Although a number of studies have evaluated the morphometry of cervical pedicles to support accurate placement of pedicle screws [3, 5], the results are inconclusive. Therefore, several techniques and computer-assisted navigation systems for CPS insertion have been advocated. Determining an appropriate entry point for screw insertion as well as a proper trajectory angle of the screw on the axial plane is important for successful pedicle screw placement. Here, we present our method of a simple free-hand pedicle screw insertion technique and evaluate the accuracy of pedicle screw placement and validity of pedicle screw fixation in patients with subaxial cervical spine injuries treated using our method.
Materials and methods
Patient population
We retrospectively reviewed 32 consecutive patients with subaxial cervical spine injuries who underwent posterior cervical fixation using our CPS insertion technique at Imakiire General Hospital. Screw diameter was 3.5 mm. There were 28 male and 4 female patients with an average age of 66 years (range 18–89 years). Seventeen patients had fallen from heights, 11 patients were involved in traffic accidents, and 4 patients were involved in other accidents. The mean follow-up period was 27.6 months (range 12–47 months). Application of Allen’s classification [6] to the injuries in these patients revealed that, 22 patients had distractive flexion (DF) injuries, 3 had compressive flexion (CF) injuries, 4 had compressive extension (CE) injuries, and 3 had distractive extension (DE) injuries. Neurological deficits were classified according to Frankel grading. Application of Frankel grading revealed that 9 patients had grade A deficit, 2 had grade B deficit, 12 had grade C deficit, 4 had grade D deficit, and 5 had grade E deficit. The injury site was C2/3 in 1 patient, C3/4 in 5 patients, C4/5 in 9 patients, C5/6 in 4 patients, and C6/7 in 13 patients.
Surgical procedure
Patients were placed in the prone position with the head fixed using a Mayfield clamp. A standard midline incision was made and paravertebral muscles were dissected and retracted laterally to expose injured facets joints. A gutter was created to identify the pedicle entrance using a high-speed burr at the transitional area between the lateral mass and lamina; this procedure is also used in double-door laminoplasty. The pedicle screw insertion point is indicated by a cancellous bone at the pedicle entrance, which is commonly observed to be reddish because of a bloody cancellous bone. After direct observation of the screw insertion point, the articular mass lateral to the pedicle entrance was scraped off using a high-speed burr for insertion of the pedicle screw at the appropriate angle (Fig. 1). On the basis of the measurements obtained from a preoperative computed tomography (CT) scan, we determined the aimed gutter depth in the transitional area between the lateral mass and lamina and the transverse angle of the pedicle probe and screw (Fig. 2). The direction in the sagittal plane of the pedicle probe and screw was intraoperatively determined using lateral fluoroscopic imaging. Because a distinct characteristic of the human cervical pedicle is that the medial wall of the pedicle is significantly thicker than the lateral wall [3, 5, 7], the medial pedicle cortex was used as a guide into the vertebral body. Through separate stab incisions, 3.5-mm diameter pedicle screws were inserted after tapping (Figs. 3, 4). Laminoplasty or laminectomy was conducted for posterior decompression. Local bone harvested from the decompression site was grafted in the lateral mass bone defect. After plate application, connections between screws and plates were tightened.
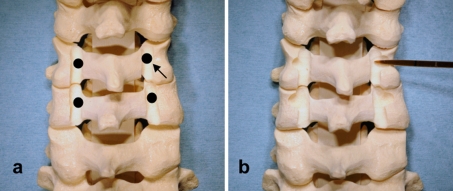
Fig. 1.
Until the cancellous bone of the pedicle entrance (arrow) becomes directly visible, creation of a gutter at the transitional area between the lateral mass and the lamina must precede identification of a screw-insertion point (a). The articular mass lateral to the pedicle entrance was scraped off to conduct probing, tapping, and insertion of the pedicle screw at an appropriate angle (b)
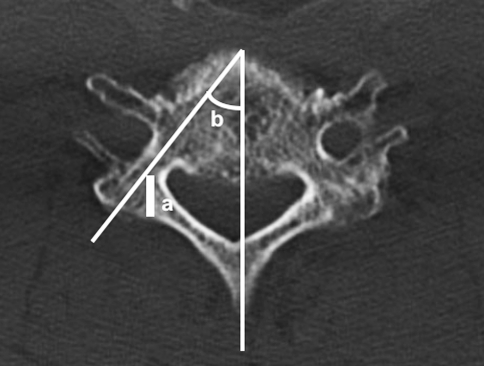
Fig. 2.
Using a preoperative axial computed tomography scan to determine the target gutter depth (a) and pedicle transverse angle (b) is mandatory
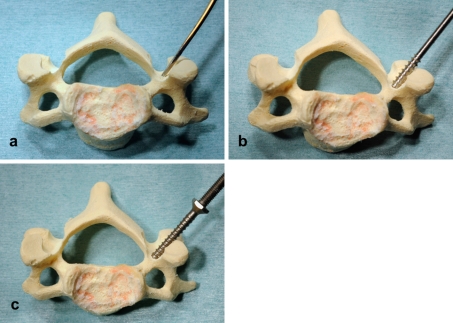
Fig. 3.
Probing (a), tapping (b), and screwing (c)
Fig. 4.
Pedicle screws were inserted after probing and tapping over separate stab incisions
Clinical and radiological outcomes
We investigated the clinical records and radiographs of all patients. Clinical assessment included neurological status, operation time, blood loss, and complications. Follow-up radiographs were assessed for the degree of kyphosis, disc height ratio, bony fusion, and instrumentation failure, such as breakage, dislodgement, and loosening. Kyphosis degree is defined as the angle between the posterior margins of vertebral bodies of the injured segment according to a lateral radiograph. Disc height ratio is defined as the percentage of vertical height of the injured disc at the intervertebral overlap midpoint divided by the vertical height of the normal disc above the injury [8]. Fusion was defined as stability observed on dynamic radiographs obtained at final follow-up. The paired Student’s t test was used to detect the difference in kyphosis degree and disc height ratio between the postoperative group and the final follow-up group, with P < 0.05 considered to be statistically significant.
Postoperative assessment of pedicle screw placement
Medial and lateral screw deviation was evaluated using an axial CT scan. Superior and inferior screw deviation was examined using oblique radiographs. CPS position was classified into three grades: grade 1, correct screw placement without pedicle perforation; grade 2, partial perforation, defined as deviation of the screws from the pedicles by <50% of the screw diameter; and grade 3, complete perforation, defined as deviation of the screws from the pedicles by more than 50% of the screw diameter. We considered grade 3 to indicate a potential injury risk to neurovascular structures. In addition, the diameter (medial–lateral outer cortical width of the pedicle) of each pedicle was measured to assess the relationship between CPS placement classification and pedicle diameter size. The diameters of non-perforated pedicles (grade 1) and perforated pedicles (grade 2 and grade 3) were compared using the Student t test, with P < 0.05 considered to be statistically significant.
Results
Clinical assessments
The mean operation time was 173.4 min (range 80–230 min) and mean blood loss was 322.6 g (range 50–1080 g). None of the patients showed neurological deterioration after the operation. Thirteen (48.1%) of 27 patients with initial neurological deficits improved by at least one Frankel grade: nine improved by one grade and four improved by two grades. There were no serious complications such as surgical site infection.
Radiographic results
The mean preoperative kyphosis was 4.0° (range −14° to 21°), which was postoperatively corrected to −5.2° (range −14° to 15°). At the final follow-up, the mean kyphosis angle was −4.4° (range −14° to 15°). There was no significant difference between postoperative kyphosis angle and the final follow-up kyphosis angle (P = 0.0705). Loss of correction (>10°) was not observed in any patient. The mean preoperative disc height ratio was 81.9% (range 15.1–133.3%), which postoperatively improved to 105.4% (range 61.5–136.8%); this value was maintained until final follow-up (103.4%; range 62.8–145.0%). There was no significant difference between the postoperative disc height ratio and final follow-up disc height ratio (P = 0.3909). Bony union was achieved and there were no instrumentation failures in any patients at final follow-up.
Accuracy of pedicle screw placement
Overall, 127 pedicle screws were inserted, of which 112 (88.1%) were classified as grade 1 (exact intrapedicular screw positioning), 10 (7.8%) as grade 2 (partial perforation), and 5 (3.9%) as grade 3 (complete perforation). There were no complications directly attributable to pedicle screw insertion, such as arterial bleeding from vertebral artery and injuries to the spinal cord or nerve roots. In 15 screws classified as grade 2 or 3, 4 perforated the pedicle medial wall and 11 perforated the lateral wall. Superior and inferior screw malpositioning was not observed in any case. Perforation occurred at C3 in two cases, C4 in five cases, C5 in one case, C6 in six cases, and C7 in one case. Mean pedicle diameter was 4.8 ± 0.8 mm and 5.7 ± 0.8 mm in perforated pedicles (grades 2 and 3) and non-perforated pedicles (grade 1), respectively. A significant difference was observed between the two groups (P = 0.0004).
Discussion
Although broad guidelines for CPS entry point localization on the lateral mass have been advocated in several clinical reports [7, 9–11], reports of unsuccessful screw placement account for up to 87.5% of the anatomical studies [12]. Recently, an anatomical study of subaxial cervical pedicles and lateral masses using CT scans of adult volunteers provided entry points and trajectories for subaxial CPSs [13]. Zheng et al. [14] reported a high success rate using subaxial CPS placement, with an overall accuracy of 83.3%, including a non-critical breach of 13.3% and a critical breach of 3.3%. This success can be achieved using the recently proposed guidelines and the oblique views obtained through fluoroscopy. However, the pedicle entrance location is unique to each level, and even at the same level, large variations are observed within the same individual [4, 11]; thus, landmarks to the cervical pedicle entrance alone are insufficient for achieving accurate CPS placement.
Several insertion techniques using direct pedicle exposure have been advocated in clinical or cadaver studies [9, 12, 15, 16]. Abumi et al. [9] described a technique in which the cortex at the insertion point is penetrated using a high-speed burr, resulting in direct observation of the pedicle introitus. They also reported a pedicle-perforation rate of 6.7% in another clinical report [17]. In their cadaver study, Karaikovic et al. [15] used the funnel technique, in which the entrance into the pedicle and vertebral body was identified by removing the outer cortex. They used the medial cervical pedicle cortex as a guide into the vertebral body through the pedicle isthmus. This study reported a screw perforation rate of 16.8%, including non-critical perforations of 9.7% and critical perforations of 7.1%, using the funnel technique. Miller et al. [16] used partial laminectomy and a tapping technique in their cadaver study, in which the entrance point for screw insertion and angulations for screw placement were guided by direct determination of the superior, medial, and inferior borders of the pedicle through the laminar window opening. Ludwig et al. [12] inserted a CPS after a laminoforaminotomy, which provides supplemental visual and tactile cues regarding orientation of the medial, superior, and inferior pedicle walls, in their cadaver study.
There have been several reports of successful CPS-insertion techniques using computer-assisted navigation systems [12, 18–20]. Several authors have reported that computer-assisted navigation systems have lower pedicle screw perforation than free-hand techniques [18, 20, 21]. Kotani et al. [18] reported that the screw misplacement rate was significantly lower in a computer-assisted group (1.2%) than in a free-hand group (6.7%). Richter et al. [20] reported that the rate of pedicle perforations was 3.0% in the computer-assisted group and 8.6% in the conventional free-hand group when using cannulated screws and separate stab incisions. Increasing use of three-dimensional fluoroscopy-based computer-assisted navigation systems has recently been reported [21, 22]. Three-dimensional fluoroscopy is superior to conventional CT-based image guidance because anatomical registration is not required and real-time updates of the spine position can be obtained intraoperatively. Ito et al. [22] reported that the rate of pedicle perforations was 2.8% in the absence of clinically significant perforation when a three-dimensional fluoroscopy-based navigation system was used. Ishikawa et al. [21] reported that the prevalence of pedicle perforation was 18.7% in a three-dimensional fluoroscopy-based navigation group and 27% in a conventional free-hand group. Although computer-assisted navigation systems can improve the accuracy of CPS insertion, there are also some disadvantages, such as the requirement of cumbersome formalities and very expensive system costs. Moreover, surgeons should possess excellent surgical skills and experience and should not rely only on the computer-assisted navigation systems.
Several pedicle screw insertion techniques that do not require navigation systems have been reported with successful clinical results. In a clinical study, Yukawa et al. [23] reported that a fluoroscopic imaging technique using the pedicle axis view used for determining the CPS entry point improved the accuracy and safety of CPS placement. They reported successful results, with 13% screw malpositions, including 9.2% screw exposure and 3.9% pedicle perforation. Miyamoto et al. [24] described a CT cutout technique, showing promise as a safe pedicle insertion method, for the cervical spine with a critical breach rate of 3.8%. Our technique presented here shows a pedicle-perforation rate of 11.8%, including partial perforation of 7.8% and complete perforation of 3.9%, which is comparable to the perforation rates obtained by insertion techniques that do not involve navigation systems.
Accurate determination of an entry point for CPS insertion is the first step in proper pedicle screw placement. In our technique, a gutter is created using a high-speed burr at the transitional area between the lateral mass and lamina, similar to the procedure of double-door laminoplasty, to identify the CPS insertion entry point. Finding the entry point using this technique is not difficult for general spine surgeons because of their familiarity with laminoplasty. In addition, because the entry point for CPS insertion is the pedicle entrance, the permitted range of the screw insertion angle is larger in our technique than in other methods. While preoperative planning is indispensable for any technique, special preoperative preparation or an intraoperative environment is not required for this procedure. Because our technique requires removal of the bone in the lateral mass, similar to the Abumi [9] and funnel [15] techniques, the expected outcome includes a significant reduction of screw fixation strength. However, Kowalski et al. [25] reported no significant difference in the biomechanical pullout strength of CPS when the lateral mass cancellous bone is removed. In addition, this study showed no significant difference between the postoperative kyphosis angle and the final follow-up kyphosis angle as well as good maintenance of the postoperative disc height ratio.
In conclusion, this study shows that good screw position placement and strong screw fixation stability can be achieved using our technique. For general spine surgeons familiar with laminoplasty, it is not difficult to identify the CPS insertion entry point using our technique. However, less-experienced spine surgeons should perform CPS insertion with the assistance of experienced surgeons.
Conflict of interest
None.
References
- 1.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 3.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ. Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res. 1999;359:77–88. doi: 10.1097/00003086-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Panjabi MM, Shin EK, Chen NC, Wang JL. Internal morphology of human cervical pedicles. Spine. 2000;25:1197–1205. doi: 10.1097/00007632-200005150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Allen BL, Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7:1–27. doi: 10.1097/00007632-198200710-00001. [DOI] [PubMed] [Google Scholar]
- 7.Jeanneret B, Gebhard JS, Magerl F. Transpedicular screw fixation of articular mass fracture-separation: results of an anatomical study and operative technique. J Spinal Disord. 1994;7:222–229. doi: 10.1097/00002517-199407030-00004. [DOI] [PubMed] [Google Scholar]
- 8.Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br. 1992;74:224–227. doi: 10.1302/0301-620X.74B2.1544957. [DOI] [PubMed] [Google Scholar]
- 9.Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22:1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 11.Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW., Jr Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord. 2000;13:63–72. doi: 10.1097/00002517-200002000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine. 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Rao RD, Marawar SV, Stemper BD, Yoganandan N, Shender BS. Computerized tomographic morphometric analysis of subaxial cervical spine pedicles in young asymptomatic volunteers. J Bone Joint Surg Am. 2008;90:1914–1921. doi: 10.2106/JBJS.G.01166. [DOI] [PubMed] [Google Scholar]
- 14.Zheng X, Chaudhari R, Wu C, Mehbod AA, Transfeldt EE. Subaxial cervical pedicle screw insertion with newly defined entry point and trajectory: accuracy evaluation in cadavers. Eur Spine J. 2010;19:105–112. doi: 10.1007/s00586-009-1213-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karaikovic EE, Yingsakmongkol W, Gaines RW., Jr Accuracy of cervical pedicle screw placement using the funnel technique. Spine. 2001;26:2456–2462. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpedicular screw placement in the cervical spine. An analysis of two approaches. Spine. 1996;21:2317–2322. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 17.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 18.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(Suppl 3):257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 19.Richter M, Mattes T, Cakir B. Computer-assisted posterior instrumentation of the cervical and cervico-thoracic spine. Eur Spine J. 2004;13:50–59. doi: 10.1007/s00586-003-0604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine. 2005;30:2280–2287. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S. Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine. 2010;13:606–611. doi: 10.3171/2010.5.SPINE09993. [DOI] [PubMed] [Google Scholar]
- 22.Ito Y, Sugimoto Y, Tomioka M, Hasegawa Y, Nakago K, Yagata Y. Clinical accuracy of 3D fluoroscopy-assisted cervical pedicle screw insertion. J Neurosurg Spine. 2008;9:450–453. doi: 10.3171/SPI.2008.9.11.450. [DOI] [PubMed] [Google Scholar]
- 23.Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H, Machino M. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009;18:1293–1299. doi: 10.1007/s00586-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miyamoto H, Uno K. Cervical pedicle screw insertion using a computed tomography cutout technique. J Neurosurg Spine. 2009;11:681–687. doi: 10.3171/2009.6.SPINE09352. [DOI] [PubMed] [Google Scholar]
- 25.Kowalski JM, Ludwig SC, Hutton WC, Heller JG. Cervical spine pedicle screws: a biomechanical comparison of two insertion techniques. Spine. 2000;25:2865–2867. doi: 10.1097/00007632-200011150-00005. [DOI] [PubMed] [Google Scholar]