Abstracts
Introduction
The purpose of this study was to measure the structures of the ventral of lateral masses using cadaver specimens and to quantitatively compare the safety zone for the two major techniques used on each vertebral level from C3 to C6.
Methods
This study is based on 52 cervical vertebrae of 13 cadavers. The anatomical measurements focused on the anterior surface of the lateral mass. We investigated the safety width, heights, and the height of nerve roots.
Results
The mean values of the safety width of the Magerl technique from C3 to C6 were 6.1, 7.3, 6.4 and 4.3 mm, respectively. The mean values of the safety width of the Roy-Camille technique were 6.7, 6.6, 5.8 and 5.4 mm, respectively. The mean values of the safety height of the Magerl technique were 5.0, 5.4, 5.8 and 5.2 mm, respectively. The mean values of the safety height of the Roy-Camille technique were 4.9, 4.0, 1.0 and −1.2 mm, respectively. The mean values of the nerve root height were 3.9, 4.9, 5.9 and 6.9 mm, respectively.
Conclusion
The safety width of the Magerl technique was shorter at C6 because the vertebral artery runs more laterally at C6. The height for the Magerl technique was not significantly different from C3 to C6, however, the safety height for the Roy-Camille technique was significantly shorter at C5 and C6. Our findings suggest that it is important to ensure that the screw(s) penetrate through the cranial side of the ventral aspect of a lateral mass when performing the Magerl technique at all vertebral levels, and to carefully select the screw length when using the Roy-Camille technique, especially at C5 and C6, in order to avoid nerve root injury.
Keywords: Anatomy, Cervical foramen, Lateral mass screw
Introduction
Posterior lateral mass screw fixation is one the most commonly used techniques for an unstable cervical spine resulting from trauma, neoplasms, degenerative conditions, or failed anterior fusion. Several techniques of lateral mass screw fixation are available, including the Roy-Camille [15], Magerl [12], Anderson [2], and An techniques [1], especially, the two most popular techniques for lateral mass screws are the Roy-Camille and the Magerl techniques. Roy-Camille et al. [15] advocated that the starting point should be located at the tip of the articular mass hill, precisely in its middle, and that the drill should be oriented perpendicular to the posterior aspect of the cervical spine and 10° lateral. The Magerl group [13] recommended starting the drill hole 2–3 mm medial and superior to the apex of the lateral mass and angled 30° upward and 25° outward. The spinal nerve roots and vertebral arteries (VA) lie in the close proximity to the lateral masses and are at risk of injury during lateral mass screw insertion.
Sekhon [17] reported that after evaluating the placement of a lateral mass screw in 143 patients, no screw-related injuries to the vertebral artery or nerve roots occurred. However, there are several potential complications associated with screw fixation which include injury of the vertebral artery and nerve root, as well as violation of the facet joints. In fact, there have been numerous reports describing the potential complications of the lateral mass screws. Heller et al. [11] suggested the incidence of nerve root injury to be higher with the Magerl technique than with the Roy-Camille technique. However, there have been conflicting results regarding each technique. It is thus not apparent which technique is safer, and under what conditions. It is therefore important to quantitatively understand the anatomic structure of the ventral lateral mass, which is the exit of the lateral mass screw, in order to avoid these complications, and to select the best surgical technique. However, few studies have been performed that have quantitatively measured the safety zone of the cervical lateral mass where the screws are applied.
The purpose of this study was to measure the structures of the ventral of lateral masses using cadaver specimens, and to quantitatively compare the safety zones of the two techniques at each vertebral level from C3 to C6.
Materials and methods
This study details the quantitative surface anatomy of the middle and lower cervical foramens. This information is based on a study of 52 cervical vertebrae of 13 cadavers (7 males and 6 females). A total of 13 cervical spines from C3 to C6 were directly evaluated using digital calipers for this study. Anatomic evaluation included the dimension of the vertebral artery foramens and anterior aspect of the vertebral artery of the lateral mass. Cadaveric specimens ranged from 64 to 85 years of age at time of death (mean age: 78 years) and had no gross deformities such as scoliosis and kyphosis. The cervical spines were harvested from the cadavers. The anterolateral aspect of the cervical spine was dissected carefully to expose the lateral mass. The anatomical measurements focused on the anterior surface of the lateral mass. Paired structures were measured bilaterally. The linear measurements using digital calipers were accurate to 0.01 mm.
The parameters included all of the measurements below:
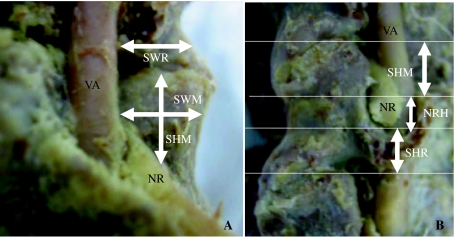
The distance between the lateral border of the VA and the lateral edge of the lateral mass above the root (SWM: The safety width for the Magerl technique) or below the root (SWR: The safety width for the Roy-Camille technique) (Fig. 1a).
The distance between the upper edge of the facet joint and the upper border of the nerve root at the midline of the lateral mass (SHM: The safety height for the Magerl technique). The distance of the nerve height at the middle of the lateral mass (NRH: Nerve root height). The distance between the root and the lower edge of the facet joint (SHR: The safety height for the Roy-Camille technique) (Fig. 1b).
Fig. 1.
a Safety width for the Magerl (SWM) technique. b Safety width for the Roy-Camille (SWR) technique. c Safety height for the Magerl (SHM) technique. d Safety height for the Roy-Camille (SHR) technique. e Nerve root height (NRH). VA vertebral artery, NR nerve root
The mean value and standard deviation for each these parameters were calculated. Normal distributions were evaluated using analysis of variance (ANOVA). Intralevel differences were determined using Scheffe’s F test. Significant differences were considered to exist at a P value of <0.05.
Results
The results of various parameters from C3 to C6 are shown in Table 1.
Table 1.
Measurements of the Dimensions of the Ventral Lateral Mass from C3 to C6
| Cervical level | C3 | C4 | C5 | C6 |
|---|---|---|---|---|
| SWM | 6.1 ± 1.7 | 7.3 ± 1.1 | 6.4 ± 1.5 | 4.4 ± 1.0 |
| SWR | 6.7 ± 1.2 | 6.6 ± 0.9 | 5.8 ± 0.6 | 5.3 ± 1.0 |
| SHM | 5.0 ± 1.3 | 5.4 ± 1.0 | 5.7 ± 1.1 | 5.2 ± 0.6 |
| SHR | 4.9 ± 1.1 | 4.0 ± 0.7 | 1.2 ± 1.6 | −1.0 ± 1.1 |
| NRH | 3.9 ± 0.4 | 4.6 ± 0.2 | 5.8 ± 0.3 | 6.8 ± 0.4 |
Values are the mean ± SD
The safety widths of the Magerl and Roy-Camille techniques
The mean values of the SWM from C3 to C6 were 6.1, 7.3, 6.4 and 4.3 mm, respectively. Significant differences were observed between C3 and C5, and between C4 and C5. The mean values of the SWR were 6.7, 6.6, 5.8 and 5.4 mm, respectively. Significant differences were also seen between C3 and C4, as well as C5 and C6 (Table 2).
Table 2.
Multiple comparisons for each parameter (P value)
| C3/4 | C3/5 | C3/6 | C4/5 | C4/6 | C5/6 | |
|---|---|---|---|---|---|---|
| SWM | <0.03 | >0.93 | <0.001 | >0.11 | <0.001 | <0.001 |
| SWR | >0.99 | <0.02 | <0.001 | <0.03 | <0.001 | >0.38 |
| SHM | >0.65 | >0.05 | >0.89 | >0.51 | >0.97 | >0.26 |
| SHR | >0.05 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| NRH | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
The safety height for the Magerl and Roy-Camille techniques and the height of nerve root
The mean values of the SHM were 5.0, 5.4, 5.8 and 5.2 mm, respectively. No significant difference was observed among the vertebral levels. The mean values of the SHR were 4.9, 4.0, 1.0 and −1.2 mm, respectively. There was a significant difference between C3 and C4. The distance was dramatilly shorter at C5 and C6. The mean values of the NRH were 3.9, 4.9, 5.9 and 6.9 mm, respectively. There were significant differences among each of the vertebral levels. The distance gradually increased from C3 to C6 (Table 2).
Discussion
Cervical spine fixation using lateral mass screws has equivalent or superior biomechanical stability over posterior wiring techniques, without the risk of spinal canal entry. These techniques reduce the need for halo immobilization and allow earlier neck mobilization. However, the insertion of lateral mass screws is associated with some risk of nerve root, VA, or facet joint injury by excessively long or misdirected screws. Several cadaveric studies have examined the placement of screws into the lateral mass, and their relationship to the neighboring anatomic structures [5, 8, 14, 18]. It is necessary to select appropriate screw lengths to avoid these potential complications. Few studies [5, 9, 18] have reported the screw lengths for the lateral mass screws. Each of these papers noted that the screw path length in the Magerl technique was several millimeters longer than that in the Roy-Camille technique. Muffoletto et al. [14] reported that the longer unicortical insertion of a lateral mass screw leads to equal pullout strength compared with bicortical insertion, and recommended longer unicortical screw purchase to reduce the risk of neural or arterial involvement. However, many investigators in clinical studies [2, 9, 10, 16] have recommended the use of bicortical screw purchase in the lateral mass, because it is biomechanically superior to unicortical purchase. Moreover, it is very difficult to control the screw length within a few millimeters. However, bicortical screws have a potential risk of nerve root and vertebral artery injury, and violation of the facet joint. To avoid these complications, it is important to understand the anatomic characteristics of the ventral lateral mass, which is the exit of lateral mass screws.
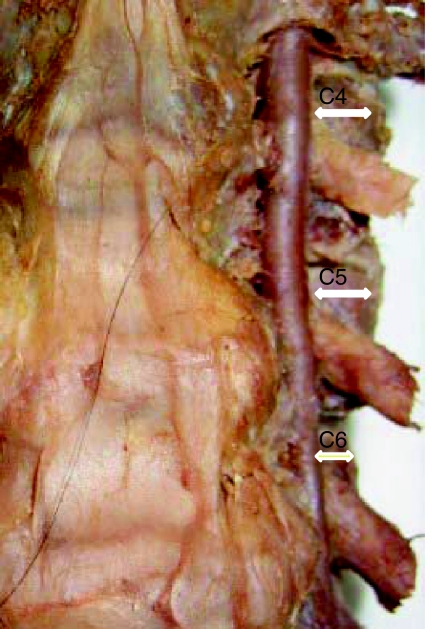
With regard to the safety width, the potential risk of vertebral artery injury by lateral mass screwing is considered to be relatively low compared to the use of pedicle screws. However, Cho et al. [4] reported a case whose vertebral artery injury and brain stem infarction were due to poor surgical technique of lateral mass plating in the cervical spine. Few authors have reported anatomic studies regarding the risk of vertebral artery injury. Ebraheim et al. [7] reported the vertebral artery foramens to be located anteromedial to the posterior midpoint of the lateral mass at C3–C5, and directly in front of the posterior midpoint of the lateral mass at C6. In our current study, safety width for Magerl technique were significantly shorter at C6 than at other vertebral levels in this value, since the vertebral artery runs more laterally at C6 (Fig. 2). Consequently, it is necessary to pay special attention to inserting a lateral mass screw at C6 to avoid vertebral artery injury. The safety width of the Roy-Camille technique was shorter at lower vertebral levels (C5 and C6) than upper vertebral levels (C3 and C4). However, the biggest difference among these values was only about 1 mm, which is therefore unlikely to be a significant difference in the clinical setting.
Fig. 2.
The location of the vertebral artery
With regard to the safety height, lateral mass screwing seems to pose considered potential for injuring the nerve root or for facet violation. Injury of the nerve root by lateral mass screwing was a major concern because it occurs more frequently than vertebral artery injury. Many authors [6, 10, 13] have studied the radicular symptoms after posterior lateral mass screw placement (4–8.3%). Cedric et al. [3] studied nerve root injuries by comparing the Magerl and Roy-Camille techniques, and measured the sagittal safety angle (SSA) for both techniques, and also performed a morphometry study of the lateral masses. They reported that for the Magerl technique, the SSA is nearly constant from C3 to C6 (around 18°–20°) whereas it decreased considerably for the Roy-Camille technique at the lower part of the cervical spine. In this anatomic study, the safety height for the Magerl technique was not significantly different from C3 to C6, however, the safety height for the Roy-Camille technique showed a significantly smaller value at C5 and C6. The exit of the lateral mass screw for the Roy-Camille technique was almost covered by the nerve root at C5 and C6. This was due to the anatomic characteristic of the spine by which the nerve height increases gradually from C3 to C6 only toward the caudal side.
However, in a previous study, the risk of the nerve root injury for the Magerl technique was higher than that for the Roy-Camille technique. Heller et al. [11] reported that nerve root injury occurred in 10.3% of patients who were treated using the Magerl technique and 3.6% for those who received the Roy-Camille technique, and they concluded that the Magerl screws had a greater risk of violation of the nerve root when compared with the Roy-Camille technique. We suspected that the distance from the nerve root to the exit of the screw might thus have demonstrated a greater distance, because the exit of the Roy-Camille technique was the ventral cortex outside of the transverse process. Therefore, we suggest that it was important to avoid nerve root injury that arises due to penetration through the cranial side of ventral aspect of lateral mass when using the Magerl technique at all vertebral levels. It is also important to ensure that the screw length used during the Roy-Camille technique, especially at C5 and C6, is appropriate.
Conclusion
We measured the structures of the ventral of lateral masses using cadaver specimens, and quantitatively compared the safety zones of the Magerl and the Roy-Camille techniques at each vertebral level from C3 to C6. The safety width of the Magerl technique was shorter at C6 because the vertebral artery runs more laterally at C6. The safety height for the Magerl technique was not significantly different from C3 to C6, whereas the safety height for the Roy-Camille technique was significantly shorter at C5 and C6. We suggest that it is important to penetrate through the cranial side of the ventral aspect of a lateral mass when using the Magerl technique at all vertebral levels, whereas special care should be taken in selecting the screw length for the Roy-Camille technique, especially at C5 and C6 in order to avoid nerve root injury.
Conflict of interest
None.
References
- 1.An HS, Gordin R, Renner K. Anatomic consideration for plate-screw fixation of the cervical spine. Spine. 1991;16(Suppl):S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 2.Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR. Posterior cervical arthrodesis with AO reconstruction plate and bone graft. Spine. 1991;16(Suppl):S72–S79. doi: 10.1097/00007632-199103001-00012. [DOI] [PubMed] [Google Scholar]
- 3.Barrey C, Mertens P, Jund J, et al. Quantitative anatomic evaluation of cervical lateral mass fixation with a comparison of the Roy-Camille and the Magerl screw techniques. Spine. 2005;30:E140–E147. doi: 10.1097/01.brs.0000155416.35234.a3. [DOI] [PubMed] [Google Scholar]
- 4.Cho KH, Shin YS, Yoon SH, et al. Poor surgical technique in cervical plating leading to vertebral artery injury and brain stem infarction—Case report. Surg Neurol. 2005;64:221–225. doi: 10.1016/j.surneu.2004.09.042. [DOI] [PubMed] [Google Scholar]
- 5.Choueka J, Spivak JM, Kummer FJ, Steger T. Fixation failure of posterior cervical lateral mass screws. Spine. 1996;21:462–468. doi: 10.1097/00007632-199602150-00010. [DOI] [PubMed] [Google Scholar]
- 6.Deen HG, Nottmeier EW, Reimer R (2006) Early complications of posterior rod-screw fixation of the cervical and upper thoracic spine. Neurosurgery 59:1062–1067 (discussion 7–8) [DOI] [PubMed]
- 7.Ebraheim NA, Xu R, Yeasting RA. The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine. 1996;21:1291–1295. doi: 10.1097/00007632-199606010-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Klausner T, Xu R, et al. Safe lateral mass screw lengths in the Roy-Camille and Magerl technique Anatomic study. Spine. 1998;23:1739–1742. doi: 10.1097/00007632-199808150-00006. [DOI] [PubMed] [Google Scholar]
- 9.Gill K, Paschal S, Corin J, Asham R, Bucholz R. Posterior plating of the cervical spine: a biomechanical comparison of different posterior fusion techniques. Spine. 1988;13:813–816. doi: 10.1097/00007632-198807000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Graham AW, Swank ML, Kinard RE, Lowery GL, Dials BE. Posterior cervical arthrodesis and stabilization with a lateral mass plate: clinical and computed tomography evaluation of lateral mass screw placement and associated complications. Spine. 1996;21:323–329. doi: 10.1097/00007632-199602010-00014. [DOI] [PubMed] [Google Scholar]
- 11.Heller JG, Garlson GD, Abitbol J, Garfin SR. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement. Spine. 1991;16(suppl):S552–S557. doi: 10.1097/00007632-199110001-00020. [DOI] [PubMed] [Google Scholar]
- 12.Jeanneret B, Magerl F, Ward EH, Ward J. Posterior stabilization of the cervical spine with hook plates. Spine. 1991;16(suppl):S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 13.Levine AM, Mazel C, Roy-Camille R. Management fracture separations of the articular mass using posterior cervical plating. Spine. 1992;17:S447–S454. doi: 10.1097/00007632-199210001-00018. [DOI] [PubMed] [Google Scholar]
- 14.Muffoletto AJ, Yang J, Vadhva M, et al. Cervical stability with lateral mass plating: unicortical versus bicortical screw purchase. Spine. 2003;28:778–781. [PubMed] [Google Scholar]
- 15.Roy-Camille R, Saillant G, Lavile C, Mazel C (1989) Internal fixation of lower cervical spine by a posterior osteosynthesis with plates and screws. In: Cervical Spine Research Society (ed) The cervical spine, 2nd edn. JB Lippicott, Philadelphia, pp 390–430
- 16.Roy-Camille R, Saillant G, Berteaux D, Serge MA. Treatment of lower cervical spinal injuries-C3 to C7. Spine. 1992;17(Suppl):S442–S446. doi: 10.1097/00007632-199210001-00017. [DOI] [PubMed] [Google Scholar]
- 17.Sekhon LH. Posterior cervical lateral mass screw fixation, analysis of 1026 consecutive screws in 143 patients. J Spinal Disord Tech. 2005;18:297–303. doi: 10.1097/01.bsd.0000166640.23448.09. [DOI] [PubMed] [Google Scholar]
- 18.Stemper BD, Marawar SV, et al. Quantitative anatomy of subaxial cervical lateral mass. An analysis of safe screw lengths for Roy-camille and Magerl techniques. J Spinal Disord Tech. 2004;17:102–107. doi: 10.1097/00024720-200404000-00004. [DOI] [PubMed] [Google Scholar]