Abstract
Purpose
The term “segmental instability” of the lumbar spine is not clearly defined, especially as it relates to degenerative spondylolisthesis (DS) and rotational translation (RT). We investigated whether facet joint effusion on conventional supine MRI indicated increased abnormal motion in DS and RT.
Methods
160 patients (119 female, 41 male, mean age 68.8 years, range 38.8–89.3 years) who had undergone decompression only or decompression with instrumented fusion for degenerative spondylolisthesis with different degrees of narrowing of the spinal canal were identified retrospectively from our spine surgery database. All had preoperative upright X-rays in AP and lateral views as well as supine MRI. The imaging studies were assessed for the following parameters: percent of slippage, absolute value of facet joint effusion, facet angles, degree of facet degeneration and spinal canal central narrowing, disc height, presence of facet cysts and the presence of rotational translation in the AP X-ray.
Results
40/160 patients showed no facet joint effusion, and in these the difference in the values for the % slip on upright X-ray and % slip on supine MRI was ≤3%. A further 12 patients also showed a difference ≤3%, but had some fluid in the joints (0.44 ± 0.38 mm). In 108 patients, the difference in the % slip measured on X-ray and on MRI was >3% (mean 10.6%, range 4–29%) and was associated with a mean facet effusion size of 2.15 ± 0.85 mm. The extent of effusion correlated significantly with the relative slippage difference between standing and supine positions (r = 0.64, p < 0.001), and the extent of the left/right difference in effusion was associated with the presence of rotational translation (RT 1.31 ± 0.8 mm vs. no-RT 0.23 ± 0.17 mm, p < 0.0001).
Conclusions
Facet joint effusion is clearly correlated with spontaneous reduction of the extent of slippage in the supine position compared to the upright position. Also, the greater the difference in right and left facet effusion, the higher the likelihood of having a RT. Future studies should assess whether analysis of facet joint effusion measured on routine MRI can help in decision-making regarding the optimal surgical treatment to be applied (decompression alone or combined with fusion).
Keywords: Lumbar spine, Facet joint effusion, Magnetic resonance imaging, Degenerative spondylolisthesis, Rotational translation
Introduction
“Instability conditions” such as degenerative spondylolisthesis (DS) and rotational translation (RT) in segments of the lumbar spine are common reasons for surgical treatment. These alterations are often associated with spinal stenosis, facet joint cysts and osteoarthritis of the facets. Patients mainly suffer from low back pain and radicular or spinal claudication. There is ongoing discussion as to whether additional fusion is really superior to decompression alone in the surgical treatment of these patients [1].
The presence of a higher grade of segmental instability than the surgeon is aware of upon examination of the preoperative MRI could lead to less satisfactory results if spondylolisthesis is treated with decompression alone (i.e., no additional fusion). Recently, Chaput et al. [2] highlighted the possibility that DS could be completely overlooked in the MRI, if this was the only imaging used for evaluation, because of spontaneous segmental repositioning of the DS in the supine position. Furthermore, he observed a distension of the facet joints on MRI in some patients and a correlation between this facet joint effusion and the presence of DS. This provided the impetus for carrying out the present investigation, in which we analysed standard standing X-rays and supine MRIs of the lumbar spine in patients with DS (with and without RT) with the aim of testing the following hypotheses:
Not every patient with DS shows facet joint effusion in the supine MRI.
The extent of facet joint effusion is directly correlated with the difference in slip distance between standing (X-ray) and supine lying positions (MRI).
Unilateral facet joint effusion or a notable difference in the degree of effusion between the right and left joints is associated with RT.
It was anticipated that, if found to be a valid means of assessing instability, the facet joint effusion sign recorded on MRI (a routinely acquired imaging sequence) could be further evaluated for its contribution to decision-making regarding the use of decompression alone versus decompression with additional fusion in the surgical treatment of DS.
Patients and methods
Patients
All patients who had undergone decompression alone or decompression with instrumented fusion for lumbar DS with or without RT between January 2005 and May 2008, were identified retrospectively from our local Quality Management system, part of the Spine Society of Europe Spine Tango registry. DS was defined as an anterior sliding of the upper vertebra over the lower one with an intact vertebral arch caused by segmental degenerative changes, measured as a misalignment of the posterior borders on standing X-ray [3]. Analogously, RT was defined as a misalignment of the lateral borders of adjacent vertebra in the AP-view on the standing X-ray (Fig. 1). Only patients with preoperative standing X-rays of the lumbar spine in the lateral and AP-views and a lumbar MRI in the supine position were included. All radiographs and MRI images were captured digitally in the image database JiveX [rv] Diagnostic Client (VISUS Technology Transfer GmbH, Bochum, Germany). For measurements, the digital panel measuring tools included in the software were used. Patients with more than two affected levels and patients with previous lumbar spinal fusion were excluded, as were patients with spondylolysis, neoplasm and inflammatory arthritis. In patients with DS at two levels, the more severe level was taken into account.
Fig. 1.
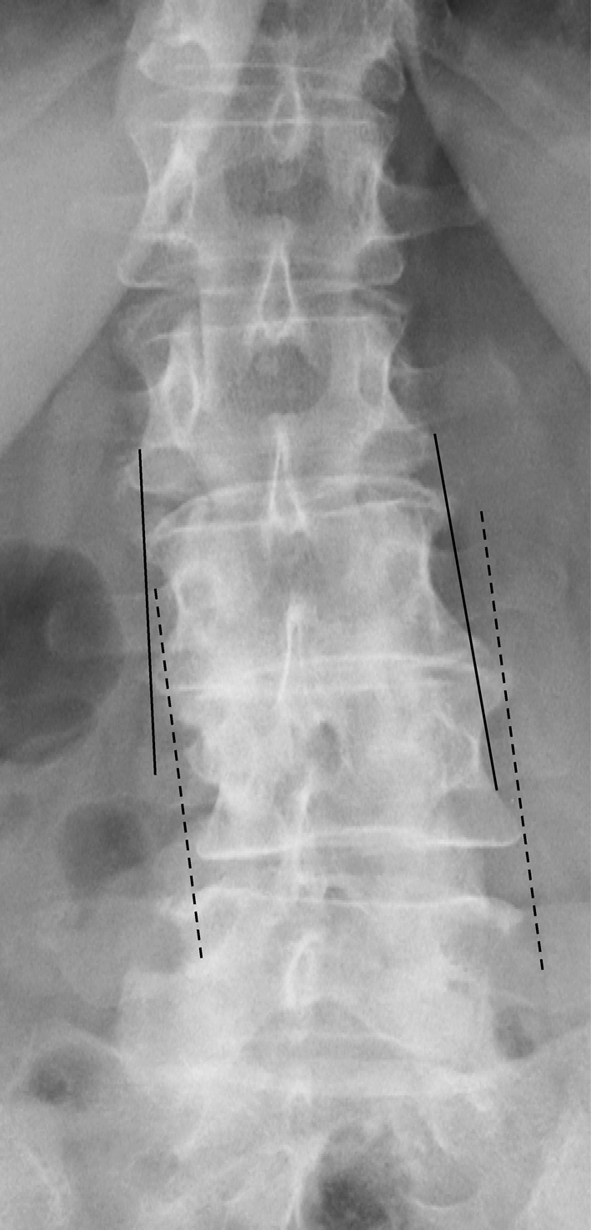
If the lateral edges of the upper and lower end plate of the vertebra next to each other are connected with lines, these lines will run parallel or cross outside of the height of the disc level in degenerative RT, whereas they will intersect at the level of the disc in, e.g., an idiopathic scoliotic segment
A total of 160 patients fulfilled the study admission criteria (n = 63 with decompression only and n = 97 with decompression and fusion). There were 119 (74.4%) females [mean (SD) age, 68.8 (9.4) years] and 41 males [mean (SD) age, 72.7 (8.3) years]. The affected level was most frequently L4/5 [123 (76.9%) patients], followed by L3/4 [28 (17.5%) patients], L5/S1 [8 (5.0%) patients] and L2/3 [1 (0.6%) patient].
Radiographic assessment
Pre-operative standing AP and lateral radiographs and supine MRIs were assessed for the following radiographic parameters: percent of slip [4]; facet joint effusion, determined as the largest distance between the apparent articular surfaces (Fig. 2), on left and right sides separately [2]; facet angle on both sides measured as the angle between the midsagittal line and each facet joint tangent line [4]; and grade (0–3) of facet joint osteoarthritis [5].
Fig. 2.
Spontaneous partial reduction of DS in the supine position in the MRI compared to the standing position in the X-ray lateral view leads to distension of the facet joints with effusion, measured perpendicular to the joint line of the inferior articular process
Additional features such as intraspinal facet joint cysts in the MRI [6], translatory gaps in the affected segment in the X-ray AP-view (Fig. 1), the degree of central narrowing of the spinal canal (0 = normal width, 1 = relative stenosis of the spinal canal, 2 = absolute stenosis = sagittal canal dimension of 10 mm or less, or no cerebral fluid) [7–9] and the disc height were registered. The intervertebral distance was measured as the perpendicular distance from the midpoint of the lower endplate of the slipped vertebra to the upper endplate of the lowermost vertebra in millimetres, taken from the lateral X-ray view [10].
Statistical analysis
The difference in % slip with the two imaging modalities (“MRI–X-ray slip difference”) was calculated by deducting the % slip in MRI from the % slip on X-ray. A cut-off value of >3% was arbitrarily chosen to represent the threshold for a “real” difference, allowing for a certain measurement error in making the measures. Descriptive data are presented as means ± standard deviations (SD) or frequencies (%). The significance of differences in mean values between groups (>3% MRI–X-ray slip difference vs. ≤3%) for continuous, normally distributed data was analysed using unpaired Students t tests. Chi-square contingency analyses and the Fisher’s exact test were used to analyse group differences in the distribution of nominal (categorical) variables.
Linear regression analysis was used to describe the relationship between the MRI–X-ray slip difference and the extent of facet joint effusion.
Statistical significance was accepted at the p < 0.05 level.
Results
A total of 108/160 (67.5%) patients showed a difference in slip on MRI and X-ray of more than 3% (Fig. 2); the mean difference was 10.4 (SD 4.6)% (range 4–29%). In these 108 patients, the mean (SD) effusion of the facet was 1.78 (SD 1.00) mm on the right side, 1.77 (SD 1.03) mm on the left side and 2.15 (SD 0.85) mm for the maximum value on either side. In this sub-group of 108 patients, 41 had been treated with decompression alone and 67 with decompression and additional instrumented fusion.
In 52/160 (32.5%) patients the difference between the % slip in MRI and the % slip in X-ray was ≤3%; 40 of these had no facet effusion at all while in 12 patients, fluid in one facet joint (6 patients) or both joints (6 patients) was observed. The mean joint effusion for these 12 patients was 0.44 (SD 0.38) mm (range 0–2.2 mm). In this sub-group of 52 patients, 22 had been treated with decompression alone, whereas 30 had undergone decompression and instrumented fusion.
Considering all patients, both mean and maximum facet joint effusion were significantly greater (p = 0.0001) in the group with >3% MRI–X-ray slip difference than in the ≤3% group (Table 1).
Table 1.
Comparison between groups of patients with a difference in % slip (MRI vs. lateral X-ray view) of ≤3 and >3%
| Difference % slip MRI–X-ray ≤3% | Difference % slip MRI–X-ray >3% | p value | |
|---|---|---|---|
| Number patients | 52 | 108 | – |
| Age (years), mean (SD) | 72.0 (7.4) | 68.7 (9.9) | 0.04 |
| Gender m:f, number (%) | 15:37 (29%:71%) | 26:82 (24%:76%) | 0.52 |
| Difference % slip MRI–X-ray, mean (SD) | 1.6 (1.2) | 10.4 (4.6) | <0.0001 |
| % slip in X-ray, mean (SD) | 20.2 (7.1) | 20.6 (6.7) | 0.70 |
| Maximum (R or L) facet effusion (mm), mean (SD) | 0.15 (0.38) | 2.15 (0.85) | 0.0001 |
| Mean facet effusion (mm), mean (SD) | 0.10 (0.26) | 1.77 (0.86) | 0.0001 |
| Difference (R vs. L) facet effusion (mm), mean (SD) | 0.10 (0.29) | 0.75 (0.77) | 0.0001 |
| Intervertebral distance, mean (SD) (mm) | 6.9 (2.8) | 7.6 (2.0) | 0.08 |
| Average (right and left) facet joint angle (°), mean (SD) | 40.2 (9.6) | 44.2 (12.0) | 0.04 |
| Facet joint cysts (number, %) | 9/52 (17.3%) | 35/108 (32.4%) | 0.045 |
| Facet degeneration (number, %) | |||
| Grade 1 | 4/52 (7.7%) | 15/108 (13.9%) | 0.0001 |
| Grade 2 | 7/52 (13.5%) | 47/108 (43.5%) | |
| Grade 3 | 41/52 (78.8%) | 46/108 (42.6%) | |
| Stenosis (number, %) | |||
| Grade 0 | 7/52 (13.5%) | 20/108 (18.5%) | 0.24 |
| Grade 1 | 23/52 (25.0%) | 37/108 (34.3%) | |
| Grade 2 | 22/52 (61.5%) | 51/108 (47.2%) | |
| Presence of rotatory translation in axial X-ray (number, %) | 11/52 (21.2%) | 52/108 (48.2%) | 0.001 |
The two groups (≤3 and >3% MRI–X-ray slip difference) showed no significant difference for the % slip on X-ray, intervertebral distance, or grade of stenosis (Table 1). However, the degree of facet joint osteoarthritis was significantly greater in the group with a slip difference ≤3% compared with the >3% group (Table 1).
There was also a slightly but significantly lower proportion of facet joint cysts (p = 0.045) and a lower mean facet joint angle (p = 0.04) in the group with ≤3% MRI–X-ray slip difference compared with the group with >3% slip difference.
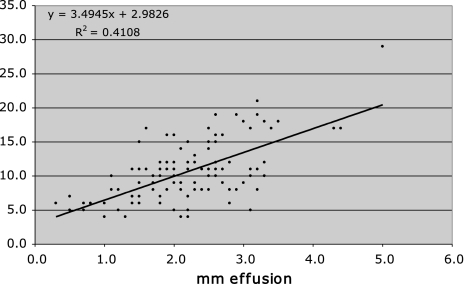
The correlation between the MRI–X-ray slip difference and facet effusion for the 108 patients with >3% slip difference was r = 0.64 (p < 0.001) (Fig. 3).
Fig. 3.
Correlation between facet effusion (mm) and % difference in slippage between MRI and X-ray (%) in the 108 patients with degenerative spondylolisthesis and % slip difference >3% between MRI and X-ray
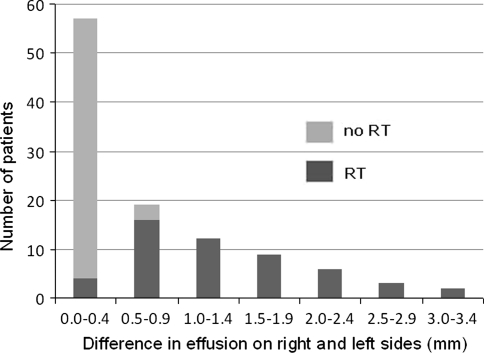
52 of the 108 patients with >3% MRI–X-ray slip difference showed a RT at the affected level on AP X-ray. These patients had a significantly higher mean value for the difference in effusion between the right and left facet joints than did those with no-RT (1.31 ± 0.8 vs. 0.23 ± 0.17 mm, respectively; p < 0.0001) (see also Fig. 4).
Fig. 4.
Distribution of patients with (n = 52, dark grey) and without (n = 56, light grey) rotatory translation in relation to the facet joint effusion difference between right and left sides (in mm) in the group with more than 3% difference in slippage (n = 108). All 32 patients with a facet joint effusion difference ≥1 mm showed a shift of the lateral borders of the two corresponding vertebrae indicating RT in the X-ray AP-view
Discussion
The current results lead us to conclude that not every case of DS (defined as described in “Patients and methods”) necessarily constitutes an unstable condition. Nearly one-third of the 160 patients with DS showed no relevant change of slippage between the standing and supine lying positions, even though the absolute extent of anterior translation in standing was as high as in the group with notable differences in standing versus supine slippage. In the patients with a “stable” DS, the extent of facet joint effusion was significantly lower than in the patients with a difference in the % slip of more than 3% between the two postures, and there were significantly more patients with severe facet degeneration than in the “unstable” group. This finding supports the theory of Kirkaldy-Willis and Farfan [11] that advancing segmental degeneration follows a course from stable to dysfunctional, unstable to re-stabilised. According to our findings, the most important factor for re-stabilisation seems to be not so much the reduction in intervertebral distance (“disc height”) (which was similar in both groups; Table 1), but rather the formation of hook-shaped osteophytes of the facet joints, associated with severe osteoarthritis (Grade 3), which leads to an interlocking between the vertebrae.
The significant correlation between the extent of effusion of the facet joints on MRI and the difference in the degree of slippage between the standing and lying positions in patients with DS supports the results of Chaput et al. [2]. These authors compared lateral flexion–extension X-rays with supine MRI and showed that an increasing effusion size increased the probability of having DS. In the current study, 12/52 (23%) patients had facet effusions but no significant change in the degree of spondylolisthesis between standing and lying positions. Possibly flexion–extension radiographs would have revealed a greater degree of instability than could be shown in going from just standing to lying. Despite this, we can state that the combination of plain X-rays in the standing position and supine MRI is valuable in detecting abnormal (or unphysiological) mobility in DS. To assess solely a supine MRI with regard to the position of the vertebral bodies could lead one to completely overlook an “unstable” DS [2]; on the other hand, the pure existence of facet effusion could lead to overestimation of the degree of instability. Ben-Galim and Reitman [10] reported on six patients in whom spinal stenosis was diagnosed with dynamic myelography, whereas the supine MRI showed unimpressive stenosis. If facet joint effusion is present, it could be anticipated that a mild central and/or lateral spinal stenosis could develop into a severe stenosis in the standing position, or that a small facet joint cyst could develop into a larger one that compresses the nerve root. Dynamic MRI might be a helpful tool to examine these hypotheses in future studies, as indicated by the report of two such cases by Jakakumar et al. [14].
Rotatory motion is another form of slip between vertebrae that is caused by degenerative changes. Accurate measurement of the reduction in RT in MRI compared with the AP X-ray in standing is not possible, but our results show that as the difference in the extent of effusion between the two facet joints of a given segment increases, so too does the probability of identifying a RT in the X-ray. In all but one of the 32 patients with a difference ≥1 mm a shift of the lateral borders of the two corresponding vertebrae indicating RT (Fig. 1) was found in the X-ray (AP-view).
This study is not without its limitations. Firstly, measuring the segmental sliding distance between the standing position and the supine position mainly reflects a movement along the transverse plane. Whether patients with so called “stable DS” might show an increased translation-rotation movement in standing lateral flexion–extension X-rays was not investigated in this study. Secondly, inaccuracies in the measurement of the facet joint distance would have occurred if the MRI plane was not absolutely perpendicular to the facet joint.
Conclusion
Based on the results of this study and previous studies [2, 12, 13], we propose the existence of both stable and unstable DS and RT. We believe that, in DS, the presence of facet joint effusion in the MRI and spontaneous repositioning between the standing and lying positions should be evaluated and documented by the radiologist and surgeon. Our follow-on studies will assess whether analysis of facet joint effusion on routine MRI can help in decision-making regarding the optimal surgical treatment to be applied i.e., whether decompression combined with fusion yields better outcomes than decompression alone in patients with a positive effusion sign.
Acknowledgments
We would like to thank Gordana Balaban, Dave O’Riordan, Julian Amacker, Kirsten Clift, and Sara Preziosa for their help with the Spine Tango Registry documentation.
Conflict of interest No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Martin CR, Gruszczynski AT, Braunsfurth HA, et al. The surgical management of degenerative lumbar spondylolisthesis. Spine. 2007;32(16):1791–1798. doi: 10.1097/BRS.0b013e3180bc219e. [DOI] [PubMed] [Google Scholar]
- 2.Chaput C, Padon D, Rush J, et al. The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine. 2007;32(17):1883–1887. doi: 10.1097/BRS.0b013e318113271a. [DOI] [PubMed] [Google Scholar]
- 3.Herkowitz HN. Spine update. Degenerative lumbar spondylolisthesis. Spine. 1995;20(9):1084–1090. doi: 10.1097/00007632-199505000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Kanayama M, Hashimoto T, Shigenobu K, et al. Intraoperative biomechanical assessment of lumbar spinal instability: Validation of radiographic parameters indicating anterior column support in lumbar spinal fusion. Spine. 2003;28(20):2368–2372. doi: 10.1097/01.BRS.0000085357.24025.27. [DOI] [PubMed] [Google Scholar]
- 5.Weishaupt D, Zanetti M, Hodler J, et al. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 6.Apostolaki E, Davies AM, Evans N, et al. MR imaging of lumbar facet joint synovial cysts. Eur Radiol. 2000;10:615–623. doi: 10.1007/s003300050973. [DOI] [PubMed] [Google Scholar]
- 7.Saifuddin A. The imaging of lumbar spinal stenosis. Clin Radiol. 2000;55(8):581–594. doi: 10.1053/crad.2000.0223. [DOI] [PubMed] [Google Scholar]
- 8.Verbiest H. Results of surgical treatment of idiopathic developmental stenosis of the lumbar vertebral canal. A review of twenty-seven years’ experience. J Bone Joint Surg (Br) 1977;59(2):181–188. doi: 10.1302/0301-620X.59B2.141452. [DOI] [PubMed] [Google Scholar]
- 9.Postacchini F, Amatruda A, Morace GB, Perugia D. Magnetic resonance imaging in the diagnosis of lumbar spinal canal stenosis. Ital J Orthop Traumatol. 1991;17(3):327–337. [PubMed] [Google Scholar]
- 10.Ha KY, Na KH, Shin JH, et al (2008) Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech 21(4):229–234 [DOI] [PubMed]
- 11.Kirkadly-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;165:110–123. [PubMed] [Google Scholar]
- 12.Bendo JA, Ong B. Importance of correlating static and dynamic imaging studies in diagnosing degenerative lumbar spondylolisthesis. Am J Orthop. 2001;30:247–250. [PubMed] [Google Scholar]
- 13.Ben-Galim P, Reitman CA. The distended facet sign: an indicator of position-depending spinal stenosis and degenerative spondylolisthesis. Spine J. 2007;7:245–248. doi: 10.1016/j.spinee.2006.06.379. [DOI] [PubMed] [Google Scholar]
- 14.Jayakumar P, Nnadi C, Saifuddin A, et al. Dynamic degenerative lumbar spondylolisthesis: diagnosis with axial loaded magnetic resonance imaging. Spine. 2006;31(10):E298–E301. doi: 10.1097/01.brs.0000216602.98524.07. [DOI] [PubMed] [Google Scholar]