Abstract
Introduction
In general, bony injuries heal well with immobilization when the fractured segments are well apposed in the cases of stable atlas fracture. Osseous nonunion of the displaced anterior arch fracture of the atlas has been reported in the literature. However, there have been no reports published on the treatment of nonunion of the atlas fractures.
Objective
The objective of this study is to describe a new technique for direct repair of the displaced anterior arch fracture of the atlas in a minimally invasive manner.
Methods
Seven patients with the atlas fracture were treated by a minimally invasive approach. Reduction of anterior arch fractures was not performed by skull traction and the displacement of fractures was more than 5 mm. Direct autograft was performed under microendoscope to improve union of the anterior arch fractures. Radiographic and CT evaluation of the atlas fractures were performed at 3, 6 and 12 months postoperatively.
Results
Seven cases of the atlas fractures (one old and six new fractures) underwent the surgical procedure smoothly without major complications. Total average displacement of the anterior arch fracture was 5.7 mm (range 5–8 mm) before surgery. Of the seven patients, bony union of the fracture developed in six. At latest follow-up, two patients had neck pain associated with movement and limited range of rotational motion.
Conclusion
Direct repair under microendoscope is a new technique that improves bony union of displaced anterior arch of the atlas fractures.
Keywords: Atlas fracture, Repair, Microendoscope, Minimally invasive spine surgery
Introduction
In various adult series, atlas fractures have accounted for 25% of craniocervical injuries, 3–13% of cervical spine injuries, and 1.3–2% of all spinal injuries [1–4]. Although there is still controversy over the management of atlas fractures, treatment principle is based on the integrity of the transverse ligament and/or on whether fractures occur in combination with other spinal injuries. Segal et al. [5] reported 18 patients of the atlas fractures treated with external immobilization. Of the five patients with isolated C1 fractures, nonunion of the fracture and poor clinical results occurred in three. Srinivas et al. [6] found that isolated fractures of the anterior arch of the atlas could result in osseous nonunion. Our indications for surgery were a displacement of anterior arch fracture of greater than 5 mm after continuous traction of ≥3 weeks or bone nonunion of anterior arch fracture with clinical presentation. To our knowledge, however, there have no report on the treatment of the displaced anterior arch fractures of the atlas. The purpose of this study is to describe a new technique by which direct repair of the C1 anterior arch fractures is performed.
Materials and methods
Clinical data
Our study was a retrospective analysis of seven consecutively treated patients for the period from March 2007 to August 2009. Seven patients, five males and two females with an average age of 47.3 (38–61) were evaluated. All the patients received radiologic evaluation via plain cervical spine radiographs, computerized tomography (CT), and magnetic resonance imaging (MRI) examination. The patients had a displacement of the anterior arch of more than 5 mm (mean 5.7 mm; range 5–8 mm) and an intact transverse ligament. Of the seven patients with displaced anterior arch fractures, falls occurred in four, motor vehicle accident in three. Of the three displaced anterior arch fractures with associated injuries, one fracture occurred in combination with cervical congenital deformity, one with type I Hangman’s fracture and one with type III odontoid fracture. According to Landells and Van Peteghem’s classification system [4], the cases included two type I, three type II and two type III atlas fractures. The neurologic motor examinations were normal in seven patients, while two patients complained of upper extremity numbness in 1 upper limb. All patients complained of neck pain and six patients had limited range of motion. All patients with new atlas fractures underwent skull traction within 5 days after accident. Poor reduction established obvious displacement of the anterior arch fractures of the atlas after continuous traction of ≥3 weeks. The operation was performed within 1 month after the accident in six cases and delayed for 4 months in one case. The incidence of bone nonunion in the atlas posterior ring is exceedingly rare. We encountered no cases of osseous nonunion of posterior arch fracture of the atlas. The demographic characteristic of the patients, clinical characteristics of injuries, and mode of presentation are presented in Table 1.
Table 1.
Patient demographic data and clinical characteristic
| Case no. | Age (years) | Sex | Mechanism of injury | Classification of atlas F | Associated injuries | Neurological findings | Op at days after trauma |
|---|---|---|---|---|---|---|---|
| 1 | 42 | M | MVA | Type III | None | None | 23 |
| 2 | 45 | M | Fall | Type II | Hangman’s F | 1 limb numb | 27 |
| 3 | 61 | M | Fall | Type I | Deformity | None | 25 |
| 4 | 50 | F | MVA | Type III | None | None | 27 |
| 5 | 53 | F | Fall | Type II | Odontoid F | 1 limb numb | 28 |
| 6 | 42 | M | Fall | Type II | None | None | 26 |
| 7 | 38 | M | MVA | Type I | None | None | 129 |
MVA Motor-vehicle accident, F fracture, Op operation
Surgical techniques
After induction of general endotracheal anesthesia, patients were positioned supine on a radiolucent frame. A radiolucent bite block was placed in the patient’s mouth to improve radiographic transoral visualization of the C1. The patient’s head was secured using Gardner-Wells tongs with 2 kg of traction weight. A 1.4 cm unilateral horizontal incision was made along the medial border of the right sternocleidomastoid muscle at approximately the C3–4 level. The platysma and the fascia of the sternocleidomastoid were divided by mosquito forceps. Using a guide tube with a blunt tip, blunt dissection was performed to arrive at the anterior surface of the vertebral body at the midcervical level by opening the natural tissue planes medial to the carotid artery sheath and lateral to the trachea and esophagus. The guide tube continued upward along the anterior margin of the vertebral body and was placed straight below the anterior arch of the C1 under fluoroscopic control. After the set of serial dilators were inserted through the guide tube, the 14-mm METRx tubular retractor was passed over the final dilator. Finally, the rigid microendoscope (Medtronic Sofamor Danek, USA) was then inserted into the tubular retractor.
Using microendoscopic illumination and vision, the fractures of the anterior arch of the C1 was identified and exposed after removing soft tissue including the anterior longitudinal ligament between the bony fragments. Burr was used to prepare bone graft bed especially in the patient of old fracture. Sufficient autologous bone graft obtained from the iliac was packed in the fracture space. A representative case is showed in Figs. 1, 2 and 3. The patient was allowed to walk 1 day after the surgery and immobilized in a soft cervical collar for 4–6 weeks.
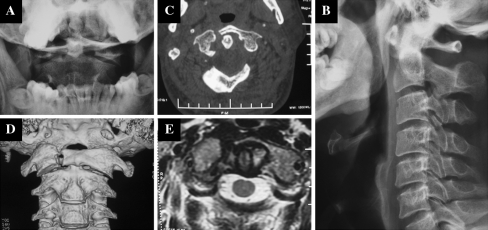
Fig. 1.
The open mouth and lateral radiographs of a 38-year-old male 4 months after accident (a, b). The distance between the dens and atlas is 3 mm. The preoperative CT reconstruction (c, d) showed displaced fracture of more than 5 mm at the anterior arch of the C1. The preoperative MRI (e) revealed nonunion of the anterior arch of the atlas and intact transverse ligament. The bony union of lateral mass fracture restored the integrity of transverse ligament
Fig. 2.
The removal of soft tissue and preparation of bone graft bed (a, b) and autologous bone graft (c) under microendoscope
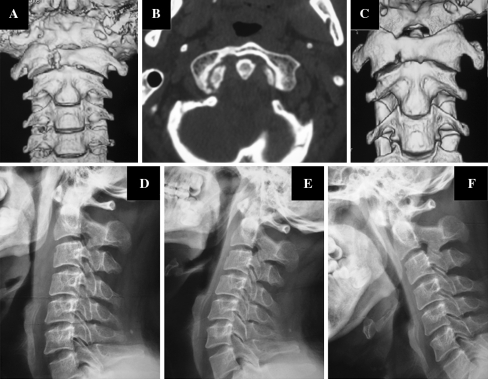
Fig. 3.
The postoperative CT reconstruction at the third day (a) and 6 months (b, c) after surgery showed a good bony union of the fracture. The neutral (d), extension (e) and flexion (f) of the cervical vertebra showed atlantoaxial stability 6 months after surgery
Clinical and radiological evaluation
The data collected retrospectively for analysis included operating time between open and closure of the skin incision, clinical and radiographic results, and complication. Lateral, open mouth and flexion–extension lateral radiographs of the upper cervical level were obtained at 3, 6 and 12 months postoperatively to assess union and alignment of the C1–C2. 1 mm thin-slice computed tomographic scans and construction were necessary to assess bone healing. Definitive fusion was identified by formation of bony bridges through fracture. The rotational capacity at the C1–2 joints was measured by functional CT-scans in supine position as described by Koller et al. [7].
Results
The average follow-up was 23.6 months with a range of 13–30 months. The mean operating time was 56.3 min (range 45–75 min). Two patients with upper extremity numbness in one upper limb made a recovery without neurologic sequelae. Two patients (one having nonunion of the fracture) complained of neck pain and limitation of cervical rotational motion without further surgical therapy. Bony fusion of displaced anterior arch fractures of the atlas was observed in six patients. Atlantoaxial stability was confirmed by flexion–extension X-rays in all cases.
No serious morbidities, such as esophageal perforation, carotid artery laceration, neurological deterioration and airway obstruction occurred in all patients. Two cases of transient dysphagia occurred after surgery. This complication had resolved gradually within 3 or 5 days without special therapy. The details of clinical and radiographic data are illustrated in Table 2.
Table 2.
Clinical and radiographic results at latest follow-up
| Case no. | Operative time (min) | Clinical presentation | Rotation of C1–C2 (°) | Bony fusion of atlas F | Complication |
|---|---|---|---|---|---|
| 1 | 65 | None | 66 | Yes | Dysphagia |
| 2 | 60 | Neck pain | 39 | No | None |
| 3 | 52 | None | 67 | Yes | None |
| 4 | 47 | None | 72 | Yes | None |
| 5 | 50 | None | 65 | Yes | None |
| 6 | 45 | None | 70 | Yes | None |
| 7 | 75 | Neck pain | 35 | Yes | Dysphagia |
Discussion
The first cervical vertebra (C1), also known as the atlas, is an integral and crucial part of the craniocervical junction or the upper cervical spine and acts as a transitional structure between the occiput and cervical spine. Its unique ring shape and design allows the most range of motion and flexibility compared with any other level of the spinal column [8]. Burst fractures of the atlas were first described by Sir Geoffrey Jefferson in 1920 [9]. There is no single uniformly accepted classification system of atlas fractures. Several classification methods such as Gehweiler [10] or Landells and Van Peteghem’s classification system are commonly used. However, no single classification system accommodates all the types of atlas fractures seen in clinical situations.
Treatment of atlas fractures depends on whether they occur in isolation or in conjunction with other cervical spine fractures. Isolated atlas fractures can usually be treated by external immobilization of the craniocervical junction typically for 8–12 weeks [11, 12]. There are no established standards for the treatment of combined C1–C2 fractures. Treatment is primarily based on the nature of the C2 fracture and on the integrity of the transverse ligament. Although no guidelines have been established for the treatment of isolated or combined injuries, atlantoaxial instability and disruption of transverse ligament are accepted as an important surgical indication for an occiput–C2 fusion or a C1–C2 fusion.
Radiographic outcomes of treatment of isolated atlas fractures, with or without closed traction reduction, seem highly successful [13]. Cases of nonunion or instability have been rare. However, the clinical outcomes of these patients are not well addressed. Neck pain is present in 20–80% of patients after external immobilization [5, 13]. Segal et al. [5] reported 18 patients of the atlas fractures treated with external immobilization. Of the five patients with isolated C1 fractures, nonunion of the fracture and poor clinical results occurred in three. Srinivas et al. [6] reported one case of isolated vertical fracture of the anterior arch of the atlas. Despite adequate immobilization, the fracture had established bony nonunion. However, the patient has no residual symptoms of neck pain or any neurological deficit. The authors concluded that isolated fractures of the anterior arch of the atlas could result in osseous nonunion. In the case reported by Strano et al. [14], the patient was a delayed presentation with existing non-union and had persistent headache. The incidence of bone nonunion in the atlas posterior ring is very rare. No cases of osseous nonunion of posterior arch fracture of the atlas were observed and reported. Nonunion of isolated fractures of the atlas may be associated with transverse ligament disruption, inadequate fracture reduction and absence of adequate cervical immobilization.
The indications for surgery by microendoscopic bone graft were a displacement of anterior arch fracture of more than 5 mm after continuous traction of ≥3 weeks or nonunion of anterior arch fracture with clinical presentation. In our study on seven patients of displaced anterior arch fractures of the atlas with the integrity of transverse ligament, a new minimally invasive method is confirmed to be safe and efficacious. Direct repair of the atlas fractures under microendoscope facilitates bony union of displaced fractures and decreases risk of injury to the C1 and neural elements by improving the integrity of atlantoaxial structure. A small incision definitely lead to a smaller scar, which is the most obvious result of surgery for the patient. For the surgeon, a smaller approach implies the possibility of a lower infection rate. Other potential benefits include less invasiveness and blood loss. Only complication is transient dysphagia occurring in two patients which has relation to unfamiliar manipulation and long operative time. There is one case of nonunion of the atlas fracture after surgery because of displacement of bone chips. The patient refused further treatment because of no obvious complaints of neck pain. Two patients have limitation of atlantoaxial rotational motion and neck pain. Further clinical trials would be warranted to elucidate the relationship among nonunion of displaced anterior arch of the atlas, atlantoaxial movement and neck pain. To our knowledge, this is the first study on direct repair of displaced anterior arch of the atlas by minimally invasive technique but it has some drawbacks and limitations. A challenging learning curve and potential risk must be stressed to surgeon without experiences on cervical minimally invasive surgery. Furthermore, more cases and longer follow-up should be necessary for further investigation.
The clinical study proposal was approved by the medical ethical committee of the authors’ institution. The written informed consents were obtained from all patients at study entry.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest None of the authors has any potential conflict of interest.
References
- 1.Hadley MN, Dickman CA, Browner CM, et al. Acute traumatic atlas fractures: management and long term outcome. Neurosurgery. 1988;23:31–35. doi: 10.1227/00006123-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Levine AM, Edwards CC. Fractures of the atlas. J Bone Joint Surg Am. 1991;73:680–691. [PubMed] [Google Scholar]
- 3.Sherk HH, Nicholson JT. Fractures of the atlas. J Bone Joint Surg Am. 1970;52:1017–1024. [PubMed] [Google Scholar]
- 4.Landells CD, Peteghem PK. Fractures of the atlas: classification, treatment and morbidity. Spine (Phila Pa 1976) 1988;13:450–452. doi: 10.1097/00007632-198805000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Segal LS, Grimm JO, Stauffer ES. Non-union of fractures of the atlas. J Bone Joint Surg Am. 1987;69:1423–1434. [PubMed] [Google Scholar]
- 6.Srinivas S, Harshavardhana N, Bayley E, et al. Isolated vertical fracture of the anterior arch of the atlas—Case report. Injury Extra. 2009;40:152–154. doi: 10.1016/j.injury.2009.03.018. [DOI] [Google Scholar]
- 7.Koller H, Acosta F, Forstner R, et al. C2-fractures: part II. A morphometrical analysis of computerized atlantoaxial motion, anatomical alignment and related clinical outcomes. Eur Spine J. 2009;18:1135–1153. doi: 10.1007/s00586-009-0901-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kakarla UK, Chang SW, Theodore N, et al. Atlas fractures. Neurosurgery. 2010;66(Suppl):60–67. doi: 10.1227/01.NEU.0000366108.02499.8F. [DOI] [PubMed] [Google Scholar]
- 9.Jefferson G. Fractures of the atlas vertebra: report of four cases, and a review of those previously recorded. Br J Surg. 1920;7:407–422. doi: 10.1002/bjs.1800072713. [DOI] [Google Scholar]
- 10.Gehweiler J, Duff D, Salutario M, et al. Fractures of the atlas vertebra. Skeletal Radiol. 1976;23:97–102. doi: 10.1007/BF00347414. [DOI] [Google Scholar]
- 11.Kesterson L, Benzel E, Orrison W, et al. Evaluation and treatment of atlas burst fractures (Jefferson fractures) J Neurosurg. 1991;75:213–220. doi: 10.3171/jns.1991.75.2.0213. [DOI] [PubMed] [Google Scholar]
- 12.Fowler JL, Sandhu A, Fraser RD. A review of fractures of the atlas vertebra. J Spinal Disord. 1990;3:19–24. doi: 10.1097/00002517-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Levine AM, Edwards CC. Fractures of the atlas. J Bone Joint Surg Am. 1991;73:680–691. [PubMed] [Google Scholar]
- 14.Strano SD, Marais AD. Cervical spine fracture in a boxer—a rare but important sporting injury. A case report. S Afr Med J. 1983;63:328–330. [PubMed] [Google Scholar]