Abstract
Objective
The current study examined the sex- and age-specific structure and comorbidity of lifetime anxiety disorders among U.S. adolescents.
Method
The sample consisted of 2,539 adolescents (1,505 females and 1,034 males) from the National Comorbidity Survey-Adolescent Supplement who met criteria for DSM-IV lifetime anxiety disorders. Adolescents ranged in age from 13-18 years (M = 15.2 years, SE = 0.08 years) and were 39% non-White. Multiple-group latent class analysis (LCA) was conducted by adolescent sex and age to identify subgroups of adolescents with similar anxiety disorder profiles. Developmental and clinical correlates of empirically-derived classes were also examined to assess the nomological validity of identified subgroups.
Results
A seven-class solution provided the best fit to the data, with classes defined primarily by one rather than multiple anxiety disorders. Results also indicated that classes displayed similar diagnostic profiles across age, but varied by sex. Classes characterized by multiple anxiety disorders were consistently associated with a greater degree of persistence, clinical severity, impairment, and comorbidity with other DSM-IV psychiatric disorders.
Conclusions
The presentation of lifetime anxiety disorders among adolescents and the observation of unique correlates of specific classes provide initial evidence for the utility of individual DSM-IV anxiety disorder categories. Although findings of the present study should be considered preliminary, results emphasize the potential value of early intervention and gender-specific conceptualization and treatment of anxiety disorders.
Keywords: anxiety disorders, lifetime comorbidity, epidemiology, adolescents, National Comorbidity Survey Replication Adolescent Supplement (NCS-A), latent class analysis
Introduction
Although the scope, persistence, and impact of anxiety disorders in youth have been well-documented (Costello et al., 1996; Essau, Conradt, & Petermann, 2000; Merikangas et al., 2010), investigators continue to raise concerns about the classification of these disorders in contemporary diagnostic nosology. In particular, both clinical (Franco, Saavedra, & Silverman, 2007; Masi et al., 2004; Verduin & Kendall, 2003) and epidemiologic studies (Costello, Egger, & Angold, 2005; Essau et al., 2000; Ferdinand, Dieleman, Ormel, & Verhulst, 2007; Lewinsohn, Zinbarg, Seeley, Lewinsohn, & Sack, 1997) have consistently indicated that these disorders evidence a great degree of comorbidity within their diagnostic category (homotypic comorbidity; Angold, Costello, & Erkanli, 1999). Such substantial overlap among the anxiety disorders has called into question whether their classification as several distinct categories is both theoretically and empirically meaningful (Caron & Rutter, 1991; Costello et al., 2005; Saavedra & Silverman, 2002; Weems & Stickle, 2005).
Theoretical and Clinical Importance of Examining Anxiety Disorder Comorbidity
Implicit in our current diagnostic nomenclature (and future proposals for the DSM-5) is a conceptualization of anxiety in which disorders are unique from one another in focus, yet share the common underlying feature of fear, anxiety, or worry (Zinbarg & Barlow, 1996). Whereas some factor analytic studies have provided evidence for this conceptualization, yielding several discrete anxiety factors resembling the DSM-IV anxiety disorder subtypes (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000; Higa-McMillan, Smith, Chorpita, & Hayashi, 2008; Muris, Schmidt, Engelbrecht, & Perold, 2002; Spence, 1997; Wittchen, Beesdo, & Gloster, 2009), other work has found support for two- and three-factor solutions (Beesdo-Baum et al., 2009; Brown, Chorpita, & Barlow, 1998; Krueger, 1999; Watson, 2005). In view of such observed inconsistencies across studies, it is unclear whether the conceptualization of anxiety disorders inherent in the DSM-IV parallels the presentation of anxiety disorders among individuals.
Beyond its theoretical implications, accurate classification of the anxiety disorders can inform the development of clinical interventions and treatment. While there is some uniformity in the components of effective treatment across disorders (i.e., exposure, cognitive-restructuring), many empirically-supported interventions target individual anxiety disorders (e.g., Social Effectiveness Therapy for Social Phobia; Beidel, Turner, Young, & Paulson, 2005; Parent-Child Interaction Therapy for Separation Anxiety Disorder; Choate, Pincus, Eyberg, & Barlow, 2005; Adolescent Panic Control Treatment for Panic Disorder; Hoffman & Mattis, 2000). More recent treatment paradigms, on the other hand, espouse a transdiagnostic or unified approach in which shared features of disorders are addressed in treatments that may be useful for a variety of conditions (Barlow, Allen, & Choate, 2004; Ehrenreich, Goldstein, Wright, & Barlow, 2009; Lumpkin, Silverman, Weems, Markam, & Kurtines, 2002; Norton, 2008; Norton & Hope, 2005). In line with this approach, a more parsimonious diagnostic nomenclature may promote the development of innovative treatment protocols that target the features, diatheses, and etiologic factors shared by presentations of anxiety that are now understood as distinct disorders. By contrast, unique characteristics and etiologic correlates of disorders may indicate a need for interventions that are specific to individual conditions.
Methodological Approaches to Studying Comorbidity Among the Anxiety Disorders
Although a non-negligible number of youth may exhibit comorbidity for multiple anxiety disorders (Last, Strauss, & Francis, 1987; Masi et al., 2004), the majority of research on this topic has focused on pairs of disorders, limiting examination of comorbidity to bivariate analysis (e.g., Essau, Conradt, & Petermann, 1999a; Essau, Conradt, & Petermann, 1999b; Essau et al., 2000; Last, Strauss, et al., 1987; Lewinsohn et al., 1997; Masi et al., 2004; Simonoff et al., 1997; Verduin & Kendall, 2003). Of exception, factor analytic studies have enhanced empirically-based knowledge of the structure of anxiety by identifying how symptoms or conditions covary at the multivariate level. At the same time, these studies present a number of challenges that may curtail their utility in characterizing the underlying structure of anxiety disorders. First, when dichotomous variables are subjected to factor analysis, correlations among variables are often inflated due to violations of bivariate normality (Kraemer, 1997). This may result in inaccurate solutions in which only a small number of factors are extracted due to exaggerated covariation among disorders. Second, given that factor analysis is a variable-centered analytic approach, results of these studies may be less applicable to current systems of care in which treatment referral, entry, provision, and reimbursement are supplied at the individual level.
In contrast to variable-centered analytic approaches, such as factor analysis, which classify variables into a restricted number of dimensional constructs based on their covariation (Achenbach, 1985), person-centered analytic approaches, such as latent class analysis (LCA), classify individuals into mutually exclusive categories defined by similar diagnostic presentations. Moreover, LCA assigns individuals into probabilistic groups based on shared features that discriminate members of one class from members of another class (B. O. Muthén & Muthén, 2000). Because LCA offers the advantage of identifying subgroups of individuals who share common characteristics, this analytic method provides different information than variable-level strategies when attempting to identify the complexity and heterogeneity of comorbid presentations among individuals (Herman, Ostrander, Walkup, Silva, & March, 2007; Lilienfeld, Waldman, & Israel, 1994; Wittchen, Beesdo, et al., 2009). Further, there is a practical need for analytic methods that are compatible with health care policy, practice, and organization. The characterization of individuals (as opposed to variables) in LCA may be of greater use to investigators and practitioners in each of these settings. For instance, if large subgroups of individuals are characterized by two or more anxiety disorders, this may indicate a greater need for research protocols and/or empirically-based practice specifically suited to these individuals. Conversely, if individuals are more accurately characterized by single, rather than multiple anxiety disorders, existing models of investigation and treatment delivery may be ecologically valid.
Limitations of Current Studies of Anxiety Structure and Comorbidity Among Youth
Among the few studies that have used LCA to examine the structure and comorbidity of anxiety problems in youth, most have provided support for the conceptualization of anxiety as a single construct, with classes of individuals differentiated primarily by symptom severity rather than symptom type (Ferdinand, De Nijs, Van Lier, & Verhulst, 2005; Ferdinand, van Lang, Ormel, & Verhulst, 2006; Wadsworth, Hudziak, Heath, & Achenbach, 2001). However, these studies exhibit a number of limitations. First, because all prior studies have employed symptom-level instruments, in which only a small number of anxiety items were included (van Lang, Ferdinand, Ormel, & Verhulst, 2006) or a limited range of anxiety disorders were reflected by items (Ferdinand et al., 2006), results may underestimate the number of distinct anxious presentations that exist. Second, no LCA studies of anxiety to date have examined the structure of anxiety exclusively among adolescents who meet criteria for DSM-IV anxiety disorders. Because the majority of youth in previous LCA studies do not meet diagnostic criteria for anxiety, the degree of variability in clinical levels of anxiety remains unclear. Third, although some studies suggest that the structure of anxiety disorders may differ by youth sex and age (Beesdo-Baum et al., 2009; Marmorstein, 2006; Wittchen, Beesdo-Baum, et al., 2009), most work has not examined how anxiety disorders may aggregate differently across these demographic groups, or instead has treated them as covariates in analyses (Ferdinand et al., 2006; Muris et al., 2002; van Lang et al., 2006). Finally, most studies that have examined the degree of overlap among the anxiety disorders have acquired information using relatively narrow assessment periods (e.g., 2 weeks, 1-month, 12-months) rather than a lifetime assessment approach. Although such work is valuable in better understanding the overlap and covariation of different anxiety disorders within a limited time interval, these studies cannot provide data on the presence of anxious conditions during the early life course. In consideration of work that suggests the anxiety disorders follow a clear developmental sequence (Beesdo, Knappe, & Pine, 2009; Costello et al., 2005), studies that investigate comorbidity using narrow assessment periods may fail to detect early manifestations of anxiety that reflect a distinct syndrome, illness course, or prognosis (Jensen, 2003).
Goals and Hypotheses of Present Study
The goal of the present study was to inform current understanding of anxiety disorder comorbidity and nosology by: (1) examining the sex and age-specific structure and comorbidity of lifetime anxiety disorders among adolescents using LCA; and (2) characterizing empirically-derived classes of anxiety disorders in terms of age of onset, developmental sequence, indices of severity and impairment, and comorbidity with other DSM-IV psychiatric disorders. Because prior research concerning the structure of anxiety has been inconclusive and no previous work has examined the covariation of DSM-IV anxiety disorders using LCA methodology, no specific predictions concerning the nature or number of classes were introduced. However, in consideration of work that has found higher levels of impairment and comorbidity among adolescents with multiple relative to single anxiety disorders (Essau, Conradt, & Petermann, 2002; Woodward & Fergusson, 2001), we expected to observe the greatest severity, impairment, and additional psychiatric comorbidity in youth assigned to classes defined by more than one anxiety disorder.
Method
Participants and Procedure
The National Comorbidity Survey-Adolescent Supplement (NCS-A) is a nationally-representative face-to-face survey of 10,148 adolescents ages 13-18 years in the continental United States (Merikangas, Avenevoli, Costello, Koretz, & Kessler, 2009). Aspects of the sampling strategy, participation rates, and instruments in the NCS-A are described in greater detail elsewhere (Kessler et al., 2009; Merikangas et al., 2010). Briefly, the NCS-A was carried out in a dual-frame sample that included a household subsample (n = 904) and a school subsample (n = 9,217) (Kessler et al., 2009; Merikangas et al., 2009). A self-administered questionnaire (SAQ) regarding the adolescent’s mental health was completed by 6,491 parents. Recruitment and consent procedures were approved by the Human Subjects Committees of both Harvard Medical School and the University of Michigan.
The present study focused on a subsample (n=2,539) of the larger NCS-A sample of adolescents who met criteria for lifetime anxiety disorders including separation anxiety disorder (SAD), panic disorder (PD), agoraphobia (Ago), specific phobia (SP), social phobia (SoP), and/or generalized anxiety disorder (GAD). While all anxiety disorders may vary in their etiology and conceptualization, post-traumatic stress disorder was not included in the present study due to implicit assumptions concerning its etiology and timing that are unique to this disorder (i.e., condition must follow exposure to a traumatic event; Rosen & Lilienfeld, 2008).1 In addition, obsessive-compulsive disorder could not be considered since the criteria for this disorder were not assessed.
Of the 2,539 adolescents with lifetime anxiety disorders, there were 1,505 females (56.3%, SE = 1.4%) and 1,034 males (43.7%, SE = 1.4%) between the ages of 13-18 years (M = 15.2 years, SE = 0.08 years). Participants were distributed relatively evenly across younger (13-15 years; n = 1,411) and older (16-18 years; n = 1,136) adolescent age groups. Youth were predominantly non-Hispanic white (60.1%, SE = 2.0%), followed by non-Hispanic black (18.3%, SE = 1.6%), Hispanic (15.8%, 1.3%), and other racial or ethnic groups (4.9%, SE = 0.7%). Approximately 82.8% (SE = 1.5%) of adolescents had parents who had completed at least high school. There were no statistically significant differences in sociodemographic characteristics such as race/ethnicity, parental education, poverty level, or marital status between male versus female adolescents and between younger versus older adolescents (all Wald χ2 ps > .05).
The majority of adolescents met criteria for only one anxiety disorder (72%), while 28% of adolescents met criteria for two or more anxiety disorders in their lifetime (21% had two; 6% had three; and 2% had four or more). Wald chi-square tests indicated that there were no differences in the likelihood of single vs. comorbid disorders between adolescent groups defined by sex and age (all ps > .05).
Measures
Diagnostic Assessment
Adolescents were administered a modified version of the World Health Organization (WHO) Composite International Diagnostic Interview Version 3.0 (CIDI), a fully structured interview administered by trained lay interviewers to generate DSM-IV diagnoses (Kessler & Ustun, 2004). Lifetime disorders assessed by the CIDI included anxiety disorders (SAD, SP, SoP, Ago, PD, GAD), mood disorders (major depressive disorder [MDD], dysthymic disorder), behavior disorders (oppositional defiant disorder [ODD], conduct disorder [CD], attention deficit/hyperactivity disorder [ADHD]), and substance use disorders (alcohol abuse/dependence, drug abuse/ dependence). Adolescent reports from the CIDI were used to assess diagnostic criteria for anxiety disorders, mood disorders, and substance use disorders, whereas information from both the parent and adolescent were combined and classified as positive if either informant endorsed the diagnostic criteria for behavior disorders (Cantwell, Lewinsohn, Rohde, & Seeley, 1997; Grills & Ollendick, 2002). In order to provide a direct estimate of the degree of overlap between the anxiety disorders and other DSM-IV disorders, no hierarchy rules were applied in diagnostic algorithms. For example, the hierarchical rule that prohibits assigning a diagnosis of GAD exclusively during the course of a mood disorder was not applied. In the present study, class indicators included DSM-IV lifetime disorders of SAD, SP, SoP, Ago, PD, and GAD, whereas mood, behavior, and substance use disorders were examined as possible validators of classes.
Class Characteristics and Validation
Age of Onset
Age-of-onset (AOO) information was obtained from adolescents using an assessment procedure created to enhance retrospective recall. For every disorder, respondents were asked whether they could remember their “exact age the very first time” they experienced symptoms of the disorder. Adolescents who declined were further probed by progressing up the age range in a step-wise fashion using developmental milestones as steps (e.g., “Can you remember what grade you were in at school?”). Experimental research has demonstrated that the emphasis on recall of an exact age coupled with step-wise probing significantly and meaningfully improves the accuracy of AOO data (Knauper, Cannell, Schwarz, Bruce, & Kessler, 1999). When respondents displayed multiple anxiety disorders, the median age of onset for each class was derived from the median estimate among all disorders defining the class.
Past Year Anxiety
The CIDI also collected information from the adolescent on the diagnostic criteria of DSM-IV disorders for the previous 12-month period. A past year anxiety variable was created by positively scoring cases who met criteria for any anxiety disorder of interest during the past 12 months (n = 1,863; 73.4%).
Lifetime Anxiety Treatment Contact
Within each anxiety disorder section of the CIDI, respondents were asked whether they had ever discussed their anxiety with a professional (e.g., “Did you ever in your life talk to a medical doctor or other professional about your [anxiety]?”). Types of professionals included psychologists, counselors, spiritual advisors, herbalists, acupuncturists, and other healing professionals. A dichotomous index of anxiety treatment contact was generated by positively scoring cases who endorsed seeking treatment for any anxiety disorder in their lifetime.
Past Year Impairment and Days Out of Role
Adolescents who met 12-month criteria for an anxiety disorder were also asked to rate the degree of impairment and disability they experienced during the worst month of the previous year in the areas of household chores, school or work, family relations, and social life (Sheehan Disability Scales; Leon, Olfson, Portera, Farber, & Sheehan, 1997). The response scale ranged from 0-10 and included verbal anchors of none (0), mild (1-3), moderate (4-6), severe (7-9), and very severe (10). The maximum value endorsed by respondents across each of the four areas was used. An additional item required respondents to estimate the number of days in the previous year that they were totally unable to carry out their normal activities because of their specific disorder. When respondents were assigned to classes characterized by more than one anxiety disorder, the highest impairment value or number of days out of role associated with a specific anxiety disorder was used.
Analytic Procedure
The primary objective of LCA is to explain the relationship between several categorical manifest variables (indicators) by one or more underlying latent categories (classes). The parameters in LCA include the class probabilities and the conditional probabilities. Whereas the class probabilities represent the number and relative size of estimated classes, the conditional probabilities reflect the probability that an individual will score in a particular direction for each indicator given class membership (McCutcheon, 1987). To illustrate, a final LCA model yielding two classes, labeled class A and class B, indicates that individuals in the population under investigation may be best characterized by two groups. If class A displays a class probability of 0.75 and class B displays a class probability of 0.25, then one can expect 75% of the population to be represented by class A and 25% of the population to be represented by class B. Further, if class A displays conditional probabilities of 0.8 for GAD, 0.2 for SoPh, and approximately zero for all other anxiety disorders, then an adolescent in class A is likely to have an 80% chance of meeting criteria for GAD, a 20% chance of meeting criteria for SoPh, and almost no chance of meeting criteria for any other anxiety disorder. Thus, the conditional probabilities of a class reflect its diagnostic profile.
Models are estimated sequentially, increasing the number of specified classes in each model until an optimal solution is reached. Based on individual diagnostic profiles, the most probable class membership is calculated for each individual such that the relationship between sets of anxiety disorders are explained by class membership (McCutcheon, 1987). Applied in this case, affected youth are assigned to classes based on common patterns of anxiety disorder presentation and comorbidity.
Multiple-group LCA, an extension of the LCA procedure, simultaneously estimates the conditional probabilities of classes for pre-existing groups of interest (e.g., males and females) in a single model. This approach also enables empirical examination of the equivalence of class diagnostic profiles across groups using nested model comparison (McCutcheon, 1987).
Given observed variations in comorbidity across youth sex and age (Beesdo-Baum et al., 2009; Marmorstein, 2006; Wittchen, Beesdo-Baum, et al., 2009), multiple-group LCA was employed by estimating a series of models with the Mplus Version 6.1 software package (L. K. Muthén & Muthén, 2010). Analysis adhered to recommended procedures for comparing latent structures across groups and proceeded in a number of steps (McCutcheon, 1987). First, we conducted separate exploratory LCAs in subpopulations defined by sex (n = 1,037 males vs. n = 1,510 females) and age (n = 1,411 younger adolescents vs. n = 1,136 older adolescents) to account for possible variations in the most favorable number of classes across these demographic groups.
In each step, specified classes were increased monotonically until an optimal solution was reached. A number of information criteria were used to evaluate model fit, including the Akaike information criterion (AIC; Akaike, 1974), the Bayesian information criterion (BIC; Schwartz, 1978), and the sample-size-adjusted Bayesian information criterion (BICssa; Sclove, 1987), with lower values indicating a better model fit. As additional indices of model fit, we also examined the adjusted Vuong-Lo-Mendell-Rubin Likelihood Difference Test (VLMR), with a significant p-value indicating that the estimated model provides a better fit than does the former model with one less class (Lo, Mendell, & Rubin, 2001), and entropy, with values closer to 1 indicating more precision and accuracy in classification. Although all evaluative criteria were considered, the BICssa was given primary weight due to simulation studies that have found this criterion to be one of the most robust indicators of model fit when attempting to determine the optimal number of classes (e.g., Nylund, Asparouhov, & Muthén, 2007). The most favorable class solution for each demographic group was used to guide model specification in the multiple-group analysis.
Within the multiple-group framework, all observations were combined and analyzed together using the KNOWNCLASS option in Mplus. We examined differences between sex and age groups by considering one demographic factor at a time (i.e., first, sex was specified as the grouping variable; then, age was specified as the grouping variable). For each demographic factor, an omnibus nested model comparison was conducted. This was performed by comparing a model in which the conditional probabilities of each class were allowed to vary across groups (e.g., Sex [or Age] Unrestricted Model) to a nested model in which these parameters were constrained to be equal across groups (e.g., Sex [or Age] Restricted Model). The Unrestricted Model hypothesizes that the diagnostic profiles of classes differ across demographic groups, whereas the Restricted Model hypothesizes that these parameters are invariant across groups.
When results of omnibus nested model comparisons indicated significant differences in these parameters across demographic groups, we identified which classes differed by constraining the conditional probabilities of each class in isolation, and comparing this restricted model to the Unrestricted Model. In the final multiple-group latent class model, all parameters were constrained that did not result in a significant difference when compared to the Unrestricted Model.
Nested models were compared using the log-likelihood difference formula recommended by Muthén and Muthén (2010) under cluster sampling. This formula multiplies the log-likelihood difference of the more restrictive and the less restrictive models (i.e., H0-H1) by negative two, and divides this value by a scaling correction factor (i.e., cd) in order to adjust for the fact that these values are not chi-square distributed under cluster sampling. Significant changes in fit demonstrate that the more restrictive model provides a worse fit to the data than the less restrictive model, indicating that class diagnostic profiles are significantly different across groups.
Once the final model was estimated, individuals were assigned to classes based on their most probable class membership. SUDAAN (version 10; Research Triangle Institute, 2005) and SAS (version 9.2; SAS Institute Inc., 2008) statistical software were used to examine the descriptive characteristics of classes and to perform class comparisons. For dichotomous dependent variables, logistic regression analyses tested whether individuals in each class differed in indices of persistence (past year anxiety), severity (lifetime anxiety treatment contact), and comorbidity with other psychiatric disorders, using the class of the largest size as the reference group. For continuous outcome variables (past year impairment, days out of role in the past 12 months), one-way analyses of variance and post-hoc comparisons using the Duncan procedure were conducted to examine differences across classes. Logistic regressions and ANOVAs accounted for the complex sampling design using the Taylor series linearization method applied in SUDAAN. These analyses were also weighted to adjust for differential probabilities of selection, non-response, and post-stratification (see Kessler et al., 2009, for a description).
Results
Latent Class Analyses of Anxiety Disorders by Adolescent Sex and Age
Table 1 displays the model fit for the one-through nine-class solutions of latent class models estimated separately by adolescent sex. Although the AIC suggested that an eight-class solution was optimal among females and the BIC suggested that a six-class solution was optimal among males, evaluation of the BICssa supported selection of a seven-class solution for both groups. Optimal class solutions also varied across information criteria when LCAs were conducted separately by younger (13-15 year olds) and older (16-18 year olds) adolescent age groups. Yet, similar to LCAs conducted by sex, seven-class solutions provided the best fit to the data based on evaluation of the BICssa (class solutions by adolescent age are available upon request). Inspection of alternative, competing class solutions for each subpopulation indicated that the main diagnostic profiles of derived classes were similar to the seven-class solutions. However, the greatest agreement across model information criteria was observed for the seven-class solutions.2
Table 1.
Model Fit Indices for One- to Nine-Class Solutions of DSM-IV Anxiety Disorders By Adolescent Sex
| Females (n = 1505) |
Males (n = 1034) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Classes | AIC | BIC | BICssa | VLMR value |
VLMR p-value |
Entropy | AIC | BIC | BICssa | VLMR value |
VLMR p-value |
Entropy |
| 1 | 8801.24 | 8833.14 | 8814.08 | — | — | — | 5545.78 | 5575.43 | 5556.37 | — | — | — |
| 2 | 8474.68 | 8543.80 | 8502.50 | 49897.01 | 0.00 | 0.65 | 5307.54 | 5371.78 | 5330.49 | 48149.08 | 0.01 | 0.64 |
| 3 | 8312.47 | 8418.80 | 8355.27 | 47814.79 | 0.00 | 0.75 | 5184.72 | 5283.55 | 5220.03 | 45852.03 | 0.00 | 0.85 |
| 4 | 8231.56 | 8375.11 | 8289.34 | 46741.10 | 0.00 | 0.80 | 5099.20 | 5232.61 | 5146.86 | 44631.04 | 0.09 | 0.95 |
| 5 | 8114.77 | 8295.54 | 8187.53 | 46241.26 | 0.00 | 1.00 | 5008.98 | 5176.98 | 5069.00 | 43774.11 | 0.00 | 0.96 |
| 6 | 7972.42 | 8190.40 | 8060.15 | 45528.92 | 0.00 | 0.99 | 4963.33 | 5165.92 | 5035.70 | 42817.43 | 0.00 | 0.99 |
| 7 | 7908.31 | 8163.51 | 8011.03 | 44570.08 | 0.00 | 0.98 | 4945.06 | 5182.23 | 5029.78 | 42285.11 | 0.00 | 0.96 |
| 8 | 7900.58 | 8192.99 | 8018.27 | 44074.20 | 0.00 | 0.95 | 4953.12 | 5224.89 | 5050.20 | 41979.54 | 0.00 | 0.95 |
| 9 | 7903.87 | 8233.50 | 8036.54 | 43940.84 | 0.00 | 0.89 | 4959.96 | 5266.31 | 5069.40 | 41929.30 | 0.00 | 0.96 |
Note. AIC = Akaike information criterion; BIC = Bayesian information criterion; BICssa = sample size adjusted Bayesion information criterion; VLMR value = adjusted Vuong-Lo-Mendell-Rubin likelihood difference test. Optimal solutions are denoted in bold.
Multiple-Group Latent Class Analysis
Results of stratified analyses were incorporated into the multiple-group LCA models in which seven classes were specified across demographic groups defined by sex and age. Omnibus nested model comparisons by sex indicated that the Sex Unrestricted Model, in which the conditional probabilities of classes were free to vary across male and female adolescent groups, was significantly different from the Sex Restricted Model, in which these parameters were constrained to be equal across sex (χ2(42) = 58.37, p < .05). By contrast, the Age Unrestricted Model, in which the conditional probabilities of classes were free to vary across younger and older adolescent age groups, was not significantly different from the Age Restricted Model, in which these probabilities were constrained to be equal across age (χ2(42) = 41.10, p > .05). On a global level, these results suggest that while the diagnostic profiles of classes significantly differ for male and female adolescents, these profiles are similar for younger and older adolescents. Therefore, sex was retained as the grouping variable in our multiple-group LCA model, allowing the diagnostic profiles of classes to vary across sex, while remaining equal across age.
Nested model comparisons of individual classes across sex indicated significant differences among four of the seven classes identified (all ps < 0.05). Therefore, in the final multiple-group model, the conditional probabilities of the three classes displaying similar diagnostic profiles were constrained, while the four remaining classes were allowed to vary across sex.3 Given observed differences in class structure across sex, class characteristics and comorbidity were examined separately by sex in remaining analyses.
Class Proportions and Diagnostic Profiles
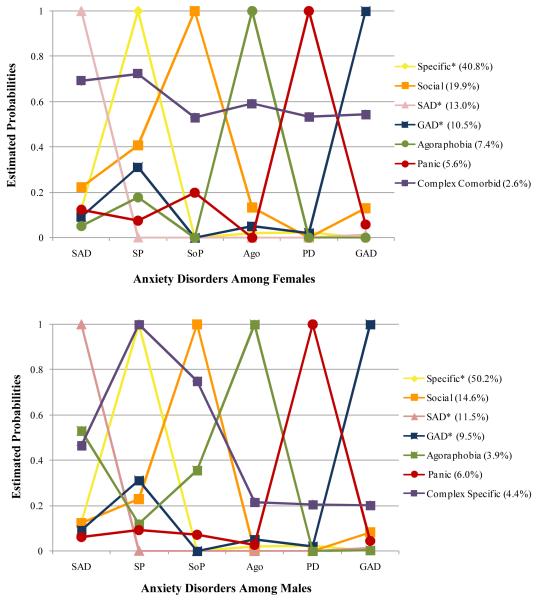
Class proportions and diagnostic profiles of the seven identified classes are shown by adolescent sex in Figure 1. Class labels were adopted to provide a clear and descriptive summary of the diagnostic presentation characterizing each class. All disorders that evidenced a probability ≥ 0.15 were considered in the class profile. A rule was implemented whereby classes were labeled according to the highest probable diagnosis. When more than one diagnosis was estimated as highly probable (i.e., defined as ≥ 0.60 probability), class labels included the additional descriptive specifier of Complex.
Figure 1.
Seven-Class Solutions of DSM-IV Anxiety Disorders Among Females and Males. Class proportions are presented in parentheses; *, denotes classes of the same name were constrained to be equal; SAD = separation anxiety disorder, SP = specific phobia, SoP = social phobia, Ago = agoraphobia, PD = panic disorder, GAD = generalized anxiety disorder.
The three classes that evidenced similar diagnostic profiles across sex were labeled Specific, SAD, and GAD. The Specific class was the most prevalent, representing 44.9% of all youth (40.8% of females, 50.2% of males) and characterized by a definite diagnosis of SP (p = 1.00) and a low probability of all other anxiety disorders. The second most prevalent among the sex-equivalent classes, the SAD class, consisted of 12.3% of youth (13% of females, 11.5% of males) and evidenced a definite diagnosis only of SAD (p = 1.00) and negligible probabilities of other anxiety disorders. Finally, comprising 10.1% of youth (10.5% of females, 9.5% of males), the GAD class was characterized by a definite diagnosis of GAD (p = 1.00) and a lower probability of SP (0.31).
The four classes that displayed sex-specific diagnostic profiles had predominant diagnoses of SoP, PD, Ago, or were characterized by a high probability of multiple anxiety disorders. While the Social class among females (19.9%) demonstrated a definite diagnosis of SoP (p = 1.00) and low to moderate probabilities of multiple anxiety disorders (SAD: p = 0.22, SP: p = 0.41), the Social class among males (14.6%) displayed a definite diagnosis of SoP (p =1.00) and a low probability only of SP (p = 0.23). Likewise, although the Panic class among females (5.6% of females) was characterized by PD (p = 1.00) and to a lesser degree SoP (p = 0.20), the Panic class among males (6.0%) was defined only by PD (p = 1.00). Similarly but conversely, the Agoraphobia class among females (7.4%) showed a definite diagnosis of Ago (p = 1.00) and a low probability of SP (p = 0.18), yet the same class among males (3.9%) displayed a definite diagnosis of Ago (p = 1.00), and low to moderate probabilities of two other anxiety disorders (SoP: p = 0.36; SAD: p = 0.53). Lastly, classes labeled with the Complex specifier were among the least prevalent of the sex-specific classes. Although no anxiety disorder clearly predominated in the Complex Comorbid class among females (2.6%), these youth showed a moderate to high probability of meeting criteria for all six anxiety disorders: SAD (p = 0.69), SP (p = 0.72), SoP (p = 0.53), Ago (p = 0.59), PD (p = 0.53), and GAD (p = 0.54). However, the Complex Specific class among males (4.4%) displayed a definite diagnosis of SP (p = 1.00) and low to high probabilities for the other anxiety disorders (SAD: p = 0.47; SoP: p = 0.75; Ago: p = 0.21; PD: p = 0.21; GAD: p = 0.20).
Thus, although there were no differences in the overall rate of comorbid vs. single anxiety disorders by adolescent sex, differences in diagnostic profiles were present by sex, and varied by class. In addition to differences in the nature of comorbid disorders, females tended to display a greater likelihood of comorbidity than males in the Social and Panic classes, whereas males appeared to display a greater likelihood of comorbidity than females in the Agoraphobia class. While the Complex Comorbid and Complex Specific classes shared a high probability for multiple anxiety disorders, the probability estimates for diagnoses differed considerably across sex.
Developmental Characteristics of Anxiety Disorder Classes by Adolescent Sex
The median age of anxiety disorder onset and the developmental sequence among the anxiety diagnoses characterizing each class are shown by adolescent sex in Table 2. As is shown, among both sexes, classes characterized by SP had the earliest onset (females: 4.9 years, males: 5.0 years), followed by classes characterized by SAD. Classes with predominant diagnoses of Ago, SoP, and the Complex Comorbid and Complex Specific classes had median ages of onset during middle childhood, whereas classes characterized primarily by PD (females: 11.5 years, males: 8.8 years) and GAD (females: 10.8 years, males: 9.8 years) had the latest ages of onset. In addition, there was a trend for SP to precede onset of other anxiety disorders in classes with comorbid profiles.
Table 2.
Developmental Characteristics of Anxiety Disorder Classes By Adolescent Sex.
| Females (n = 1505) |
Males (n = 1034) |
||||
|---|---|---|---|---|---|
| Class Label | Age of Onseta | Order of Onsetb | Class Label | Age of Onseta | Order of Onsetb |
| Specific | 4.9 | N/A | Specific | 5.0 | N/A |
| Social | 8.1 | SP (4.1) < SAD (8.1) < SoP (9.3) | Social | 8.6 | SP (6.0) < SoP (8.7) |
| SAD | 7.3 | N/A | SAD | 5.9 | N/A |
| GAD | 10.8 | SP (5.1) < GAD (12.3) | GAD | 9.8 | SP (4.0) < GAD (10.6) |
| Agoraphobia | 7.9 | SP (4.5) < Ago (8.4) | Agoraphobia | 8.7 | SoP (4.9) < Ago (6.1) < SAD (6.5) |
| Panic | 11.5 | SoP (9.5) < PD (11.6) | Panic | 8.8 | N/A |
| Complex Comorbid | 9.2 | SP (6.3) < SAD (6.4) < SoP (7.0) < Ago (9.0) < PD (10.9) < GAD (12.0) |
Complex Specific | 7.0 | SP (4.4) < GAD (7.0) < SAD (7.5) < SoP (9.2) < PD (9.5) < Ago (9.6) |
Note. SAD = separation anxiety disorder, SP = specific phobia, SoP = social phobia, Ago = agoraphobia, PD = panic disorder, GAD, generalized anxiety disorder, N/A = not applicable; age is presented in years
age of onset value is median value among all anxiety disorders defining the class; the median age of onset value was used for individuals with multiple anxiety disorders
age of onset value for each diagnosis is median value; only disorders evidencing a probability ≥ .15 in each anxiety class are considered in the Order of Onset column
Clinical Correlates of Anxiety Disorder Classes by Adolescent Sex
The proportion of individuals in each class and class comparisons are displayed for indices of persistence, severity, and impairment by adolescent sex in Table 3. Among females, logistic regression analyses indicated that there were significant differences across classes in past year anxiety (Wald χ2[6] = 30.80, p < .001) and lifetime anxiety treatment contact (Wald χ2[6] = 4.56, p < .01). One way ANOVAs and post-hoc comparisons also demonstrated significant differences across classes in the degree of past year impairment experienced by female adolescents (Wald F [6, 42] = 19.94, p < .001) and the number of days out of role in the previous year (Wald F [6, 42] = 5.72, p < .001). Across almost all domains, females in the Complex Comorbid class demonstrated the greatest problems, including a high proportion of females who had past year anxiety disorders (93.3%) and the greatest proportion who spoke to a professional about their anxiety (56.7%). Females in this class also displayed the most severe past year impairment, and had the greatest number of days out of role in the previous 12-month period. Likewise, but with some variations, a great degree of severity and impairment was also observed among females in the Social, GAD, and Panic classes. By contrast, females in the Specific and SAD classes tended to display the lowest levels of severity and impairment in terms of lifetime anxiety treatment contact, past year impairment, and total number of days out of role. Though females in the Specific class displayed relatively low levels of severity and impairment, a high proportion of these females had past year anxiety (85.7%).
Table 3.
Clinical Correlates of Anxiety Disorder Classes By Adolescent Sex.
| Females (n = 1505) |
Males (n = 1034) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Class Label |
Past Year Anxiety* (%) |
Treatment Contact* (%) |
Past Year Impairment1* M (SE) |
Days Out of Role* M (SE) |
Class Label |
Past Year Anxiety* (%) |
Treatment Contact* (%) |
Past Year Impairment1* M (SE) |
Days Out of Role* M (SE) |
| Specific | 85.7 | 13.8 | 2.97 (0.17)a | 1.09 (0.44)a | Specific | 71.5 | 10.2 | 2.73 (0.23)a | 1.11 (0.29)a |
| Social | 96.3 | 20.5 | 5.58 (0.32)b | 6.58 (1.98)a,b | Social | 87.1 | 23.2 | 4.85 (0.37)b | 2.88 (1.03)a |
| SAD | 22.0 | 19.7 | 2.49 (0.55)a | 1.77 (0.84)a | SAD | 7.9 | 8.9 | 5.40 (1.18)b | 1.17 (0.90)a |
| GAD | 61.5 | 40.1 | 5.17 (0.43)b | 5.88 (1.66)a,b | GAD | 57.2 | 35.4 | 5.23 (0.61)b | 2.67 (1.07)a |
| Agoraphobia | 81.1 | 20.0 | 3.24 (0.39)a | 0.96 (0.47)a | Agoraphobia | 61.0 | 18.0 | 5.86 (1.01)b,c | 1.04 (0.50)a |
| Panic | 92.1 | 46.2 | 5.39 (0.46)b | 6.93 (1.76)a,b | Panic | 78.6 | 17.6 | 2.75 (0.64)a | 3.04 (1.85)a |
| Complex Comorbid |
93.3 | 56.7 | 6.96 (0.67)c | 8.45 (2.34)b | Complex Specific |
100 | 38.6 | 7.16 (0.53)c | 10.81 (3.14)b |
Note. Past year impairment and days out of role was assessed among adolescents with past year anxiety disorders (n = 1,863)
value displayed is maximum of functional domains (household chores, school/work, family relations, social life); only disorders evidencing a probability ≥ .15 in each class were considered in past year impairment and days out of role
overall Wald χ2 or Wald F value is significant, indicating differences in variable across classes
different superscript letters within the same column indicate that estimated means are significantly different.
different superscript letters within the same column indicate that estimated means are significantly different.
different superscript letters within the same column indicate that estimated means are significantly different.
Similar to females, logistic regression analyses among males also indicated significant differences across classes in past year anxiety (Wald χ2[6] = 17.07, p < .001) and lifetime anxiety treatment contact (Wald χ2[6] = 3.55, p < .01). In addition, there were significant differences across classes in the level of past year impairment experienced by male youth (Wald F [6, 42] = 17.21, p < .001) and the number of days out of role in the previous year (Wald F [6, 42] = 2.69, p < .05). As is shown, the Complex Specific class showed the greatest degree of severity and impairment across domains, with all males in this class meeting criteria for past year anxiety and the highest proportion speaking to a professional about their anxiety. Similarly, these males demonstrated severe past year impairment, and the greatest number of days out of role in the previous 12-month period. A high level of severity and impairment was also observed among males in the Social, GAD, and Agoraphobia class, though to a somewhat lesser degree. Conversely, and consistent with female classes characterized by the same disorders, males in the Specific and SAD classes evidenced fairly low levels of severity and impairment.
Class Comorbidity with other DSM-IV Lifetime Disorders
The proportion of individuals in each class with other lifetime DSM-IV disorders and the estimated odds of exhibiting these disorders relative to the Specific class are displayed by adolescent sex in Table 4. As is displayed, females in the Complex Comorbid class had the greatest amount of comorbidity with other DSM-IV disorders, including mood disorders and substance use disorders. For remaining classes, the most consistent associations with other DSM-IV disorders emerged for females in the Social, GAD, and Panic classes. By contrast, females in the Specific, SAD, and Agoraphobia classes appeared to display the lowest rates of other DSM-IV disorders.
Table 4.
Lifetime Comorbidity of Anxiety Disorder Classes By Adolescent Sex.
| Mood Disorders |
Females (n = 1505) Behavior Disorders |
Substance Use Disorders |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class Label |
MDD | Dys | ODD | CD | ADHD | Alcohol | Drug | |||||||
| (%) | MDD OR 95% CI |
(%) | Dys OR 95% CI |
(%) | ODD OR 95% CI |
(%) | CD OR 95% CI |
(%) | ADHD OR 95% CI |
(%) | Alcohol OR 95% CI |
(%) | Drug OR 95% CI |
|
| Specific | 24.2 | 1.00 | 8.0 | 1.00 | 9.3 | 1.00 | 11.7 | 1.00 | 6.7 | 1.00 | 6.2 | 1.00 | 7.5 | 1.00 |
| Social | 38.0 | 1.92* | 11.3 | 1.46 | 28.5 | 3.86* | 24.5 | 2.45 | 8.2 | 1.24 | 11.7 | 2.01 | 19.6 | 3.01* |
| 1.25-2.96 | 0.74-2.90 | 1.43-10.43 | 0.84-7.14 | 0.63-2.47 | 0.93-4.33 | 1.38-6.56 | ||||||||
| SAD | 26.3 | 1.12 | 6.3 | 0.78 | 6.9 | 0.71 | 9.2 | 0.76 | 8.8 | 1.34 | 3.1 | 0.48 | 4.1 | 0.53 |
| 0.69-1.82 | 0.26-2.32 | 0.22-2.36 | 0.29-1.98 | 0.48-3.78 | 0.21-1.13 | 0.23-1.20 | ||||||||
| GAD | 56.0 | 3.99* | 25.5 | 3.93* | 26.1 | 3.42* | 21.6 | 2.07 | 13.6 | 2.18 | 10.8 | 1.84 | 12.4 | 1.75 |
| 2.68-5.94 | 1.76-8.74 | 1.21-9.68 | 0.63-6.80 | 0.75-6.29 | 0.62-5.48 | 0.74-4.14 | ||||||||
| Ago | 19.2 | 0.75 | 4 .9 | 0.59 | 6 .2 | 0.64 | 8 . 0 | 0.66 | 2 . 4 | 0.34 | 1.5 | 0.23* | 2.1 | 0.26* |
| 0.46-1.21 | 0.33-1.05 | 0.16-2.62 | 0.18-2.44 | 0.09-1.25 | 0.06-0.91 | 0.08-0.89 | ||||||||
| Panic | 36.8 | 1.83* | 12.9 | 1.69 | 11.3 | 1.23 | 13.3 | 1.16 | 9.5 | 1.46 | 16.9 | 3.09* | 32.0 | 5.78* |
| 1.00-3.33 | 0.73-3.92 | 0.34-4.49 | 0.32-4.19 | 0.38-5.62 | 1.15-8.27 | 2.60-12.86 | ||||||||
| Complex | 61.3 | 4.96* | 34.9 | 6.16* | 10.6 | 1.15 | 39.3 | 4.88* | 23.6 | 4.30* | 18.7 | 3.48* | 19.5 | 2.97* |
| Comorbid | 1.66-14.83 | 1.74-21.82 | 0.30-4.43 | 1.22-19.43 | 1.54-12.00 | 1.28-9.45 | 1.07-8.28 | |||||||
| Specific | 13.2 | 1.00 | 2.4 | 1.00 | 13.6 | 1.00 | 17.6 | 1.00 | 16.6 | 1.00 | 6.0 | 1.00 | 10.3 | 1.00 |
| Social | 33.6 | 3.32* | 4.2 | 1.76 | 11.8 | 0.86 | 2 0.4 | 1.20 | 2 3 .1 | 1.51 | 2 0.0 | 3.90* | 2 5 .0 | 2.92 |
| 1.72-6.39 | 0.53-5.85 | 0.40-1.83 | 0.47-3.06 | 0.91-2.50 | 1.71-8.90 | 1.33-6.40 | ||||||||
| SAD | 19.2 | 1.56 | 8 .3* | 3.69* | 2 2.9 | 1.90 | 1 9.2 | 1.11 | 16.8 | 1.01 | 4 .3 | 0.70 | 1 3.7 | 1.38 |
| 0.96-2.54 | 1.64-8.30 | 0.67-5.35 | 0.36-3.48 | 0.38-2.73 | 0.27-1.82 | 0.46-4.16 | ||||||||
| GAD | 38.3 | 4.07* | 1 8 . 9 | 9.49* | 29.6 | 2.69 | 22.6 | 1.37 | 21.7 | 1.39 | 1 9 .1 | 3.68* | 2 4.6 | 2.85 |
| 2.22-7.48 | 3.62-24.89 | 0.76-9.45 | 0.29-6.45 | 0.64-3.05 | 1.54-8.79 | 0.80-10.14 | ||||||||
| Ago | 26.7 | 2.38 | 0.3 | 0.12 | 3.9 | 0.26 | 5.2 | 0.26 | 18.3 | 1.12 | 11.7 | 2.08 | 2 0 .6 | 2.27 |
| 0.66-8.68 | 0.01-1.09 | 0.07-1.02 | 0.06-1.14 | 0.28-4.45 | 0.35-12.51 | 0.60-8.57 | ||||||||
| Panic | 20.2 | 1.65 | 2 . 1 | 0.87 | 3.1 | 0.21 | 5.5 | 0.28 | 9 .0 | 0.50 | 15.9 | 2.95 | 1 3.7 | 1.39 |
| 0.71-3.84 | 0.18-4.29 | 0.07-0.62 | 0.06-1.23 | 0.16-1.50 | 0.81-10.76 | 0.36-5.32 | ||||||||
| Complex | 27.9 | 2.53* | 5 .4 | 2.32 | 4 7.3 | 5.73* | 3 5 .4 | 2.57 | 28.0 | 1.95 | 1 6.7 | 3.13 | 1 3.7 | 1.38 |
| Specific | 1.11-5.79 | 0.60-8.94 | 1.67-19.69 | 0.85-7.80 | 0.60-6.36 | 0.81-12.17 | 0.54-3.54 | |||||||
Note. OR = odds ratio, CI = confidence interval, Ago = Agoraphobia, MDD = major depressive disorder, Dys = dysthymia, ODD = oppositional defiant disorder, CD = conduct disorder, ADHD = attention/deficit hyperactivity disorder, Alcohol = alcohol abuse or dependence, Drug = drug abuse or dependence
odds ratio is significant using the Specific class as the reference group.
Among males, individuals in the GAD class showed the greatest comorbidity with other DSM-IV disorders. Males in this class demonstrated high rates of MDD, Dysthymia, and Alcohol Use Disorders. Elevated rates of psychiatric disorders, particularly MDD and ODD, were also observed among males in the Complex Specific class. In addition, males in the Social class showed elevated rates of MDD and Alcohol Use Disorders. However, with minor variations, males in the Specific, SAD, and Panic classes showed among the lowest rates of comorbidity with other DSM-IV psychiatric disorders.
Discussion
The present study sought to inform current diagnostic nomenclature by examining the underlying structure and comorbidity of lifetime anxiety disorders among adolescents with these conditions in the general population. To achieve this goal, LCA was employed to identify classes of adolescents who displayed similar anxiety disorder profiles across the early life course. Developmental and clinical correlates of these classes were also examined to determine whether subgroups of adolescents with anxiety disorders could be differentiated by developmental features, clinical indices, and comorbidity with other DSM-IV disorders.
In contrast to previous LCA studies of anxiety in youth (Ferdinand et al., 2005; Ferdinand et al., 2006; van Lang et al., 2006; Wadsworth et al., 2001), our results revealed that classes were better characterized by the nature rather than the degree or number of anxiety disorders. Although comorbidity was possible among several classes predominantly defined by one disorder, probability estimates for additional disorders in these classes were low. Indeed, only a small number of classes (and individuals) demonstrated high rates of cross-anxiety characterization. However, it is important to note that prior LCA studies of anxiety in youth did not assess a broad range of anxiety problems and most examined this research question in general population samples in which individuals with clinical diagnoses were in the minority. Because anxiety problems in these studies were likely narrowly represented both in terms of measurement and sampling, the detection of variations in clinical levels of anxiety may have been obscured. In support of this notion, one LCA study of anxiety symptoms involving a referred sample of youth did find evidence of a class defined by symptoms of GAD (Ferdinand et al., 2005). Our results are also in accord with several factor analytic studies of anxiety symptoms (Chorpita et al., 2000; Muris et al., 2002; Spence, 1997) and disorders (Wittchen, Beesdo, et al., 2009) as well as longitudinal studies of anxiety (Ferdinand et al., 2007) that have offered support for differentiating among anxiety disorder subtypes.
Similar to the findings of a number of previous studies of youth (Franco et al., 2007; Verduin & Kendall, 2003), analyses also demonstrated that the rate of anxiety disorder comorbidity was invariant across sex. However, these findings counter one large, general population study of adults in which a higher rate of anxiety disorder comorbidity was found among females relative to males (McLean, Asnaani, Litz, & Hofmann, 2011). Such discrepant results are likely a function of differences in the sample characteristics and/or methodology across studies. For instance, differences in rates of comorbidity across sex may become more evident as youth enter adulthood due to incident cases of anxiety during this developmental period (Costello, Copeland, & Angold, 2011). It is also possible that the previous study of adults found a higher rate of anxiety disorder comorbidity among females because of its consideration of PTSD in estimates of comorbidity, particularly given that the largest sex discrepancy in prevalence rates was observed for this diagnosis.
Despite no differences in the rate of comorbidity across adolescent sex, several classes displayed differences in the quality of anxiety disorder comorbidity across sex, consistent with earlier work (Marmorstein, 2006). In general, whereas the Social and Panic classes among females showed a greater likelihood of comorbidity than did these classes among males, the reverse pattern was revealed for the Agoraphobia class. Although the reasons underlying such differences may involve both biological (Altemus & Epstein, 2008) and sociocultural mechanisms (Shear, Feske, & Greeno, 2000), results suggest that future classification, assessment, and treatment of anxiety disorders may do well to consider gender-specific presentations.
Approximating previous studies that have demonstrated distinctions in anxiety disorder onset across developmental time (Beesdo et al., 2009; Costello et al., 2005; Kessler et al., 2005), the age of onset patterns observed in this study support the validity of derived classes from a developmental perspective. Consistent with others, we found classes of SP and SAD to exhibit ages of onset in early childhood, classes characterized by SoP to onset in middle childhood, and classes defined by PD and GAD to have the latest ages of onset, in late childhood and adolescence. Although our finding of the emergence of Ago in middle childhood differs from prior studies yielding estimates in late childhood or adolescence (Beesdo et al., 2009; Wittchen, Lieb, & Schuster, 1999), such differences may be due to variations in the level of dysfunction characterizing onset (e.g., subclinical vs. clinical; Wittchen et al., 1999). Additional research that examines differences in age of onset by diagnostic level may be useful in better understanding the developmental progression of a condition from initial symptoms to clinical disorder.
Perhaps most intriguing was the observation that, with little variation, SP predated onset of other anxiety disorders in classes exhibiting any likelihood of comorbidity. Because of its high prevalence (Essau et al., 2000; Merikangas et al., 2010) and relatively low degree of impairment (Simonoff et al., 1997; Strauss & Last, 1993), SP is often considered an innocuous condition (Becker et al., 2007). However, these findings raise the possibility that the presence of SP in early childhood may serve as an initial marker for subsequent comorbidity, clinical severity, and/or poor clinical prognosis. Despite its implications, future longitudinal research is needed to support this finding and identify factors that may distinguish between youth whose fear remains circumscribed and those whose fear generalizes to other content areas over time, leading to a more serious clinical course.
Class validation by clinical correlates and psychiatric comorbidity also demonstrate the empirical and clinical value of the classes of anxiety identified in this study. Resembling previous studies that have documented the cumulative negative impact of multiple vs. single anxiety disorders in youth (Essau et al., 2000; Woodward & Fergusson, 2001), almost invariably, youth in classes with the greatest number of lifetime anxiety disorders evidenced the highest levels of persistence, severity, impairment, and comorbidity. Likewise, youth in classes defined primarily by individual anxiety disorder subtypes displayed characteristic patterns of course and risk that have been identified by prior work. For example, classes defined primarily by SP and SoP displayed among the highest degrees of persistence (Bittner et al., 2007; Merikangas, Avenevoli, Acharyya, Zhang, & Angst, 2002; Wittchen, Lieb, & Pfister, 2000) and elevated rates of impairment, professional help-seeking, and mood disorders were observed among youth with GAD and SoP relative to other anxiety disorders (Essau et al., 2000; Shaffer et al., 1996; Wittchen, Nelson, & Lachner, 1998). Taken together, differentiation of classes by clinical indicators and patterns of comorbidity provide support for retaining distinctions among the anxiety disorder subtypes.
However, several limitations of the current investigation introduce additional empirical questions, highlighting the need for future work on this topic. First, although we examined comorbidity among anxiety disorders using a lifetime assessment framework, it is important to note that these data are cross-sectional in nature. Thus, retrospective reports of the timing of anxiety disorders among youth should be considered preliminary. The importance of longitudinal research in providing further support for our findings cannot be overstated. Second, while the majority of adolescents with lifetime anxiety disorders also met criteria for an anxiety disorder in the previous 12 months (i.e., 73%), past year functioning data were not available for youth who failed to meet criteria during this time period. Thus, findings may not generalize to all youth who present with anxiety disorders in their lifetime.
In addition, because we were interested in examining the degree of overlap among DSM-IV anxiety disorders in youth, it was necessary to use disorders as indicators and to focus analysis on those youth affected with these problems. While this approach allowed us to directly examine variations in the presentation of anxiety disorders at the clinical level, other approaches to instrumentation or sampling may generate a different pattern of results. For example, different findings may be observed with other sets of anxiety disorders, and results may not extend to clinically-referred and/or adult samples in which rates of comorbidity are often greater (Brown & Barlow, 1992; Last, Hersen, Kazdin, Finkelstein, & Strauss, 1987). Further, although the current analysis classified individuals based upon a series of characteristics, these characteristics are not independent from the system of assessment employed. As such, our results should be viewed within the constraints of the DSM-IV. Future work that investigates the aggregation of symptoms with other features (e.g., etiologic, neurobiological, physiological) will likely advance our conceptualization of anxiety disorders beyond typologies that are purely descriptive.
With these caveats in mind, results of the present study generate a number of important diagnostic and clinical implications. Most notably, findings indicate that the DSM-IV anxiety disorder categories closely resemble how these conditions manifest in youth at the individual level. Although alternative systems of diagnosis and classification have increasingly been proposed, this study provides some evidence for the performance and utility of the system currently in use. At the same time, the presence of classes characterized by high levels of comorbidity draws attention to its inherent limitations. However, rather than abandoning the current system of classification entirely, results suggest that it may be best understood as a work in progress and may serve as a suitable foundation for future research, practice, and additional revision.
Related, the finding that the majority of youth in the general population were affected with only one type of anxiety supports the continued investigation and development of disorder-specific approaches to treatment. Additionally, the observation of unique developmental and clinical correlates of classes suggests that existing disorder-focused interventions may be further refined to address risk profiles specific to individual anxiety disorders. It is important to recognize, however, that only comparative treatment studies can provide information on the relative value of disorder-specific versus transdiagnostic or unified approaches to treatment. Given that some data suggest that unified treatment provides the greatest benefit to youth with the most diagnostic complexity (Ehrenreich et al., 2009), future comparative research is needed to improve our understanding of the merits of each of these treatment paradigms for youth with different diagnostic presentations.
Further, the identification of sex-specific classes suggests fundamental differences in the nature and expression of anxiety disorders for male and female youth. While most models of clinical assessment and intervention are uniformly applied across sex (Bekker & Mens-Verhulst, 2007; Mackinaw-Koons & Vasey, 2000), these results highlight the potential need for strategies of clinical assessment and practice that more carefully consider this demographic characteristic. For example, the higher probability of SAD among females vs. males who present with SoP most directly recommends a broader assessment approach among these youth, but also introduces additional pathways of intervention and prevention.
As well, the age of onset patterns observed in this study point to the possible value of staging models of intervention (Beesdo et al., 2009), and appear to signify the importance of addressing anxiety very early in the developmental course. With few exceptions (e.g., Rapee, Kennedy, Ingram, Edwards, & Sweeney, 2005; Roth & Dadds, 2004), nearly all universal and selective anxiety prevention programs target youth in middle childhood or adolescence (see Neil & Christensen, 2009, for a review). Yet, our work suggests that clinical-level anxiety may present at appreciably younger ages, often in the form of specific fears. Therefore, prevention programs that screen and address these problems earlier in development may more effectively delay or halt progression to additional disorder and/or further stages of illness (McGorry et al., 2007).
In sum, while the efficacy of many psychosocial treatments (Ollendick & King, 2010) and preventive interventions for anxiety disorders have been established (Dadds, Spence, Holland, Barrett, & Laurens, 1997; Ginsburg, 2009), few treatments prescribe the optimal timing and intensity of interventions. As revealed in the current study, anxiety may often be the starting point of a maladaptive developmental trajectory. Clarifying knowledge of the developmental course and clinical severity associated with presentations of anxiety among youth can provide information on when and how aggressively to intervene. Such data may be an important foundation for establishing interventions designed to offset a pernicious developmental cascade.
Acknowledgments
The National Comorbidity Survey-Adolescent Supplement (NCS-A) is supported by the National Institute of Mental Health (U01-MH60220) and the National Institute of Drug Abuse (R01DA016558) with supplemental support from the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; 044708), and the John W. Alden Trust. The NCS-A was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. This work was supported by the Intramural Research Program of the National Institute of Mental Health, with additional support to Femke Lamers from a Rubicon Fellowship awarded by the Netherlands Organisation for Scientific Research (NWO). The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. government.
Footnotes
Results were stable when PTSD was included in model estimation.
Parallel analyses of the entire study sample (n = 2,539) also indicated that a seven-class solution was optimal according to the greatest number of information criteria.
All standardized bivariate residuals of the final estimated model were non-significant, indicating that the model did not violate the assumption of local independence.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp.
Contributor Information
Marcy Burstein, National Institute of Mental Health.
Katholiki Georgiades, McMaster University.
Femke Lamers, National Institute of Mental Health.
Sonja A. Swanson, Harvard School of Public Health
Lihong Cui, National Institute of Mental Health.
Jian-Ping He, National Institute of Mental Health.
Shelli Avenevoli, National Institute of Mental Health.
Kathleen R. Merikangas, National Institute of Mental Health
References
- Achenbach TM. Assessment and taxonomy of child and adolescent psychopathology. Sage; Newbury Park: 1985. [Google Scholar]
- Akaike H. A new look a the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- Altemus M, Epstein L. Sex differences in anxiety disorders. In: Becker JB, Berkley KJ, Geary N, Hampson E, Herman JP, Young EA, editors. Sex Differences in the Brain: From Genes to Behavior. Oxford University Press; New York, NY: 2008. pp. 397–402. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Becker ES, Rinck M, Turke V, Kause P, Goodwin R, Neumer S, Margraf J. Epidemiology of specific phobia subtypes: findings from the Dresden Mental Health Study. Eur Psychiatry. 2007;22(2):69–74. doi: 10.1016/j.eurpsy.2006.09.006. doi: S0924-9338(06)00158-1 10.1016/j.eurpsy.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Beesdo-Baum K, Hofler M, Gloster AT, Klotsche J, Lieb R, Beauducel A, Wittchen HU. The structure of common mental disorders: a replication study in a community sample of adolescents and young adults. Int J Methods Psychiatr Res. 2009;18(4):204–220. doi: 10.1002/mpr.293. doi: 10.1002/mpr.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. doi: S0193-953X(09)00056-210.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Young B, Paulson A. Social effectiveness therapy for children: three-year follow-up. J Consult Clin Psychol. 2005;73(4):721–725. doi: 10.1037/0022-006X.73.4.721. doi: 2005-11147-01510.1037/0022-006X.73.4.721. [DOI] [PubMed] [Google Scholar]
- Bekker MH, Mens-Verhulst J. Anxiety disorders: Sex differences in prevalence, degree, and background, but gender-neutral treatment. Gender Medicine. 2007;4(Supplement B):178–193. doi: 10.1016/s1550-8579(07)80057-x. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? J Child Psychol Psychiatry. 2007;48(12):1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. doi: JCPP181210.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Comorbidity among anxiety disorders: implications for treatment and DSM-IV. J Consult Clin Psychol. 1992;60(6):835–844. doi: 10.1037//0022-006x.60.6.835. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol. 1998;107(2):179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Cantwell DP, Lewinsohn M, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(5):610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: concepts, issues and research strategies. J Child Psychol Psychiatry. 1991;32(7):1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Choate ML, Pincus DB, Eyberg SM, Barlow DH. Parent-Child Interaction Therapy for Treatment of Separation Anxiety Disorder in Young Children: A Pilot Study. Cognitive and Behavioral Practice. 2005;12:126–135. [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53(12):1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry. 2011 doi: 10.1111/j.1469-7610.2011.02446.x. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005;14(4):631–648. vii. doi: 10.1016/j.chc.2005.06.003. doi: S1056-4993(05)00061-110.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Spence SH, Holland DE, Barrett PM, Laurens KR. Prevention and Early Intervention for Anxiety Disorders: A Controlled Trial. Journal of Consulting and Clinical Psychology. 1997;65(4):627–635. doi: 10.1037//0022-006x.65.4.627. [DOI] [PubMed] [Google Scholar]
- Ehrenreich JT, Goldstein CM, Wright LR, Barlow DH. Development of a Unified Protocol for the Treatment of Emotional Disorders in Youth. Child Fam Behav Ther. 2009;31(1):20–37. doi: 10.1080/07317100802701228. doi: 10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency and comorbidity of social phobia and social fears in adolescents. Behav Res Ther. 1999a;37(9):831–843. doi: 10.1016/s0005-7967(98)00179-x. doi: S0005-7967(98)00179-X. [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency of panic attacks and panic disorder in adolescents. Depress Anxiety. 1999b;9(1):19–26. doi: 10.1002/(SICI)1520-6394(1999)9:1<19::AID-DA3>3.0.CO;2-#. [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. J Anxiety Disord. 2000;14(3):263–279. doi: 10.1016/s0887-6185(99)00039-0. doi: S0887618599000390. [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Course and outcome of anxiety disorders in adolescents. J Anxiety Disord. 2002;16(1):67–81. doi: 10.1016/s0887-6185(01)00091-3. [DOI] [PubMed] [Google Scholar]
- Ferdinand RF, De Nijs PFA, Van Lier P, Verhulst FC. Latent class analysis of anxiety and depressive symptoms in referred adolescents. Journal of Affective Disorders. 2005;88:299–306. doi: 10.1016/j.jad.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Ferdinand RF, Dieleman G, Ormel J, Verhulst FC. Homotypic versus heterotypic continuity of anxiety symptoms in young adolescents: evidence for distinctions between DSM-IV subtypes. J Abnorm Child Psychol. 2007;35(3):325–333. doi: 10.1007/s10802-006-9093-0. doi: 10.1007/s10802-006-9093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand RF, van Lang ND, Ormel J, Verhulst FC. No distinctions between different types of anxiety symptoms in pre-adolescents from the general population. J Anxiety Disord. 2006;20(2):207–221. doi: 10.1016/j.janxdis.2004.12.003. doi: S0887-6185(05)00021-6 10.1016/j.janxdis.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Franco X, Saavedra LM, Silverman WK. External validation of comorbid patterns of anxiety disorders in children and adolescents. Journal of Anxiety Disorders. 2007;21:717–729. doi: 10.1016/j.janxdis.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS. The Child Anxiety Prevention Study: Intervention Model and Primary Outcome. Journal of Consulting and Clinical Psychology. 2009;77(3):580–587. doi: 10.1037/a0014486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews/ Clinical Child and Family Psychology Review. 2002;5(1):57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- Herman KC, Ostrander R, Walkup JT, Silva SG, March JS. Empirically derived subtypes of adolescent depression: latent profile analysis of co-occurring symptoms in the Treatment for Adolescents with Depression Study (TADS) J Consult Clin Psychol. 2007;75(5):716–728. doi: 10.1037/0022-006X.75.5.716. doi: 2007-13640-00510.1037/0022-006X.75.5.716. [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Smith RL, Chorpita BF, Hayashi K. Common and unique factors associated with DSM-IV-TR internalizing disorders in children. J Abnorm Child Psychol. 2008;36(8):1279–1288. doi: 10.1007/s10802-008-9250-8. doi: 10.1007/s10802-008-9250-8. [DOI] [PubMed] [Google Scholar]
- Hoffman EC, Mattis SG. A developmental adaptation of panic control treatment for panic disorder in adolescence. Cognitive and Behavioral Practice. 2000;7:253–261. [Google Scholar]
- Jensen PS. Comorbidity and child psychopathology: recommendations for the next decade. J Abnorm Child Psychol. 2003;31(3):293–300. doi: 10.1023/a:1023281513936. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Zaslavsky AM. Design and Field Procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) International Journal of Methods in Psychiatric Research. 2009;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–768. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knauper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC. Improving the accuracy of major depression age of onset reports in the US National Comorbidity Survey. Int J Methods Psychiatr Res. 1999;8:39–48. [Google Scholar]
- Kraemer HC. What is the ‘right’ statistical measure of twin concordance (or diagnostic reliability and validity)? Archives of General Psychiatry. 1997;54:1121–1124. doi: 10.1001/archpsyc.1997.01830240081011. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Last CG, Hersen M, Kazdin AE, Finkelstein R, Strauss CC. Comparison of DSM-III separation anxiety and overanxious disorders: demographic characteristics and patterns of comorbidity. J Am Acad Child Adolesc Psychiatry. 1987;26(4):527–531. doi: 10.1097/00004583-198707000-00011. doi: S0890-8567(09)65731-210.1097/00004583-198707000-00011. [DOI] [PubMed] [Google Scholar]
- Last CG, Strauss CC, Francis G. Comorbidity among childhood anxiety disorders. J Nerv Ment Dis. 1987;175(12):726–730. doi: 10.1097/00005053-198712000-00004. [DOI] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry in Medicine. 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, Sack WH. Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. J Anxiety Disord. 1997;11(4):377–394. doi: 10.1016/s0887-6185(97)00017-0. doi: S0887-6185(97)00017-0. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Waldman ID, Israel AC. A Critical Examination of the Use of the Term and Concept of Comorbidity in Psychopathology Research. Clinical Psychology: Science and Practice. 1994;1(1):71–83. [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. [Google Scholar]
- Lumpkin PW, Silverman WK, Weems CF, Markam MR, Kurtines WM. Treating a heterogeneous set of anxiety disorders in youth with group cognitive-behavioral therapy: A partially nonconcurrent multiple-baseline evaluation. Behavior Therapy. 2002;33:163–177. [Google Scholar]
- Mackinaw-Koons B, Vasey MW. Considering sex differences in anxiety and its disorders across the life span: A construct validation approach. Applied & Preventive Psychology. 2000;9(191-201) [Google Scholar]
- Marmorstein NR. Generalized versus performance-focused social phobia: patterns of comorbidity among youth. J Anxiety Disord. 2006;20(6):778–793. doi: 10.1016/j.janxdis.2005.08.004. doi: S0887-6185(05)00088-510.1016/j.janxdis.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Masi G, Millepiedi S, Mucci M, Poli P, Bertini N, Milantoni L. Generalized anxiety disorder in referred children and adolescents. J Am Acad Child Adolesc Psychiatry. 2004;43(6):752–760. doi: 10.1097/01.chi.0000121065.29744.d3. doi: S0890-8567(09)61325-3 10.1097/01.chi.0000121065.29744.d3. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent class analysis. Sage Publications; Beverly Hills: 1987. [Google Scholar]
- McGorry PD, Purcell R, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging: a heuristic model for psychiatry and youth mental health. Med J Aust. 2007;187(7 Suppl):S40–42. doi: 10.5694/j.1326-5377.2007.tb01335.x. doi: mcg10315_fm. [DOI] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. doi: S0022-3956(11)00045-810.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S, Acharyya S, Zhang H, Angst J. The spectrum of social phobia in the Zurich cohort study of young adults. Biol Psychiatry. 2002;51(1):81–91. doi: 10.1016/s0006-3223(01)01309-9. doi: S0006322301013099. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(4):367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. doi: S0890-8567(10)00476-410.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Schmidt H, Engelbrecht P, Perold M. DSM-IV-defined anxiety disorder symptoms in South African children. J Am Acad Child Adolesc Psychiatry. 2002;41(11):1360–1368. doi: 10.1097/00004583-200211000-00018. doi: S0890-8567(09)60642-010.1097/00004583-200211000-00018. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24(6):882–891. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6 ed. Muthén & Muthén; Los Angeles, CA: 2010. [Google Scholar]
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev. 2009;29(3):208–215. doi: 10.1016/j.cpr.2009.01.002. doi: S0272-7358(09)00003-810.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Norton PJ. An open trial of a transdiagnostic cognitive-behavioral group therapy for anxiety disorder. Behav Ther. 2008;39(3):242–250. doi: 10.1016/j.beth.2007.08.002. doi: S0005-7894(08)00005-1 10.1016/j.beth.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Norton PJ, Hope DA. Preliminary evaluation of the broad-spectrum cognitive-behavioral group therapy for anxiety. Journal of Behavior Therapy and Experimental Psychiatry. 2005;36:79–97. doi: 10.1016/j.jbtep.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén B. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling:A Monte Carlo Simulation Study. Structural Equation Modeling. 2007;14(4):535–569. [Google Scholar]
- Ollendick TH, King NJ. Empirically supported treatments for children with phobic and anxiety disorders: Current status. Journal of Clinical Child & Adolescent Psychology. 2010;27(2):156–167. doi: 10.1207/s15374424jccp2702_3. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy S, Ingram M, Edwards S, Sweeney L. Prevention and early intervention of anxiety disorders in inhibited preschool children. J Consult Clin Psychol. 2005;73(3):488–497. doi: 10.1037/0022-006X.73.3.488. doi: 2005-06517-01110.1037/0022-006X.73.3.488. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute . SUDAAN: Professional software for survey data analysis. 10 ed. Research Triangle Institute; Research Triangle Park, NC: 2005. [Google Scholar]
- Rosen GM, Lilienfeld SO. Posttraumatic stress disorder: an empirical evaluation of core assumptions. Clin Psychol Rev. 2008;28(5):837–868. doi: 10.1016/j.cpr.2007.12.002. doi: S0272-7358(07)00204-8 10.1016/j.cpr.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Roth JH, Dadds MR. Prevention of internalizing problems in early childhood:Results of a universal trial. 2004. Manuscript submitted for publication. [Google Scholar]
- Saavedra JM, Silverman WK. Classification of anxiety disorders in children: what a difference two decades make. International Review of Psychiatry. 2002;14:87–101. [Google Scholar]
- SAS Institute Inc. SAS/STAT® user’s guide. 9.2 ed. SAS Institute; Cary, NC: 2008. [Google Scholar]
- Schwartz G. Estimating the dimensions of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sclove LS. Application of a model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, Regier DA. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Shear MK, Feske U, Greeno C. Gender differences in anxiety disorders. In: Frank E, editor. Gender and Its Effects on Psychopathology. American Psychiatric Press, Inc.; Washington, D.C.: 2000. pp. 151–165. [Google Scholar]
- Simonoff E, Pickles A, Meyer JM, Silberg JL, Maes HH, Loeber R, Eaves LJ. The Virginia Twin Study of Adolescent Behavioral Development. Influences of age, sex, and impairment on rates of disorder. Arch Gen Psychiatry. 1997;54(9):801–808. doi: 10.1001/archpsyc.1997.01830210039004. [DOI] [PubMed] [Google Scholar]
- Spence SH. Structure of anxiety symptoms among children: a confirmatory factor-analytic study. J Abnorm Psychol. 1997;106(2):280–297. doi: 10.1037//0021-843x.106.2.280. [DOI] [PubMed] [Google Scholar]
- Strauss CC, Last CG. Social and simple phobias in children. Journal of Anxiety Disorders. 1993;7:141–152. [Google Scholar]
- van Lang ND, Ferdinand RF, Ormel J, Verhulst FC. Latent class analysis of anxiety and depressive symptoms of the Youth Self-Report in a general population sample of young adolescents. Behav Res Ther. 2006;44(6):849–860. doi: 10.1016/j.brat.2005.06.004. doi: S0005-7967(05)00146-410.1016/j.brat.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Verduin TL, Kendall PC. Differential occurrence of comorbidity within childhood anxiety disorders. J Clin Child Adolesc Psychol. 2003;32(2):290–295. doi: 10.1207/S15374424JCCP3202_15. [DOI] [PubMed] [Google Scholar]
- Wadsworth ME, Hudziak JJ, Heath AC, Achenbach TM. Latent class analysis of child behavior checklist anxiety/depression in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(1):106–114. doi: 10.1097/00004583-200101000-00023. doi: S0890-8567(09)60822-4 10.1097/00004583-200101000-00023. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the Mood and Anxiety Disorders: A Quantitative Hierarchical Model for DSM-V. Journal of Abnormal Psychology. 2005;114(522-536) doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Weems CF, Stickle TR. Anxiety disorders in childhood: casting a nomological net. Clin Child Fam Psychol Rev. 2005;8(2):107–134. doi: 10.1007/s10567-005-4751-2. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Beesdo-Baum K, Gloster AT, Hofler M, Klotsche J, Lieb R, Kessler RC. The structure of mental disorders re-examined: is it developmentally stable and robust against additions? Int J Methods Psychiatr Res. 2009;18(4):189–203. doi: 10.1002/mpr.298. doi: 10.1002/mpr.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Beesdo K, Gloster AT. The position of anxiety disorders in structural models of mental disorders. Psychiatr Clin North Am. 2009;32(3):465–481. doi: 10.1016/j.psc.2009.06.004. doi: S0193-953X(09)00058-610.1016/j.psc.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Lieb R, Pfister H. The waxing and waning of mental disorders: evaluating the stability of syndromes of mental disorders in the population. Comprehensive Psychiatry. 2000;41:122–132. doi: 10.1016/s0010-440x(00)80018-8. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Lieb R, Schuster P. When is onset? Investigations into early developmental stages of anxiety and depressive disorders. In: Rapoport JL, editor. Childhood onset of "adult" psychopathology. Clinical and research advances. American Psychiatric Press, Inc.; Washington, D.C.: 1999. pp. 259–302. [Google Scholar]
- Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med. 1998;28(1):109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1086–1093. doi: 10.1097/00004583-200109000-00018. doi: S0890-8567(09)60451-210.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH. Structure of anxiety and the anxiety disorders: a hierarchical model. J Abnorm Psychol. 1996;105(2):181–193. doi: 10.1037//0021-843x.105.2.181. [DOI] [PubMed] [Google Scholar]