Abstract
Objective
Evaluate a selective prevention program targeting both eating disorder symptoms and unhealthy weight gain in young women.
Method
Female college students at high-risk for these outcomes by virtue of body image concerns (N = 398; M age = 18.4 SD = 0.6) were randomized to the Healthy Weight group-based 4-hour prevention program, which promotes gradual lasting healthy improvements to dietary intake and physical activity, or an educational brochure control condition.
Results
Compared to controls, intervention participants showed significantly greater reductions in body dissatisfaction and eating disorder symptoms, and greater increases in physical activity, at posttest and significantly greater reductions in body mass index (BMI) and self-reported dieting at 6-mo follow-up. Moderator analyses revealed significantly greater reductions in eating disorder symptoms for those with initially elevated symptoms and pressure to be thin and significantly greater reductions in BMI for those with initially elevated eating disorder symptoms.
Conclusions
Results indicate that this intervention reduced both eating disorder symptoms and unhealthy weight gain, but suggest it should be improved to produce stronger and more persistent effects, and that it may be useful to target young women with both body image and eating disturbances.
Keywords: prevention, body dissatisfaction, eating disorder symptoms, weight gain, BMI
Effective prevention programs have been developed for eating disorders, which are marked by impairment, morbidity, and mortality, but the fact that obesity is much more prevalent and related to even greater morbidity and mortality has prompted calls for interventions that also reduce unhealthy weight gain (Irving & Neumark-Sztainer, 2002; Stice & Ragan, 2002). Four prevention programs have reduced both eating disorder symptoms and unhealthy weight gain (Austin, Field, Wiecha, Peterson, & Gortmaker, 2005; Jones et al., 2008; Stice, Marti, Spoor, Presnell, & Shaw, 2008). For instance, a 26-hour universal prevention program that promotes less media use, a healthy diet, and regular exercise reduced unhealthy weight control behaviors (e.g., vomiting, diet pill use) and BMI among female, but not male preadolescents (Austin et al., 2005). However, only one has produced long-term reductions in eating disorder symptoms and BMI, and reduced onset of future eating disorders and obesity. The 3-hour Healthy Weight selective prevention program, which promotes incremental lasting healthy improvements to dietary intake and physical activity in young women with body image concerns, reduced eating disorder symptoms and BMI relative to assessment-only controls and alternative interventions through 3-yr follow-up, reduced eating disorder onset relative to assessment-only controls through 3-yr follow-up (7% vs. 15%), and reduced obesity onset relative to assessment-only controls and an alternative intervention at 1-yr follow-up (1% vs. 12% and 9% respectively) and assessment-only controls at 3-yr follow-up (8% vs. 18%; Stice et al., 2008).
Because the effects for Healthy Weight were moderate in magnitude we sought to increase its potency by adding principles that should facilitate healthy changes to dietary intake drawn largely from nutrition research (Ello-Martin, Roe & Rolls, 2004), including (a) replacing high-energy dense foods with low-energy dense foods, (b) eating complex carbohydrates with high water content at the start of meals (e.g., soup, fruit, salad), (c) reducing portions sizes, (d) eating meals with less variety in the types of foods, and (e) keeping only healthy foods in the living area (e.g., not having unhealthy snacks in the home/dorm). We added these principles because experiments suggest that they should contribute to larger weight gain prevention effects (e.g., Ello-Martin et al., 2004). We also added principles to facilitate increases in physical activity, including (a) scheduling time for exercise on a weekly basis, (b) making daily routines more active (e.g., taking the stairs, biking instead of driving to work), and (c) being creative about how to exercise (e.g., doing yard work, walking around an airport during long layovers). To accommodate this new information and provide more time for dietary and activity changes, we increased the intervention from 3 to 4 1-hour sessions. Healthy Weight 2 is described as a body acceptance program to facilitate recruitment and avoid stigmatization. Young women with body dissatisfaction are targeted because they are at increased risk for escalation in both eating disorder symptoms and unhealthy weight gain (Haines et al., 2007; Johnson & Wardle, 2005). Body dissatisfaction may also motivate people to make healthy dietary and activity changes. The healthy lifestyle change plan is participant-driven, to promote internalization of the health goals and development of executive control over lifestyle choices.
Aim 1 was to test whether Healthy Weight 2 participants would show greater reductions in eating disorder symptoms and BMI (primary outcomes) by posttest and 6-mo follow-up than educational brochure controls. Aim 2 was to test for effects on secondary outcomes targeted in this intervention: dietary intake, dietary restraint, and physical activity. Because a reduction in BMI might improve body satisfaction and affect, we also tested for intervention effects on these outcomes. Aim 3 was to test whether intervention effects on the primary outcomes would be stronger for youth with initial elevations in eating disorder symptoms and BMI, as it should be easier to affect change among individuals with more room for improvement, yet weaker for youth with elevated risk factors not addressed by the intervention, including depressive symptoms and perceived pressure for thinness.
Methods
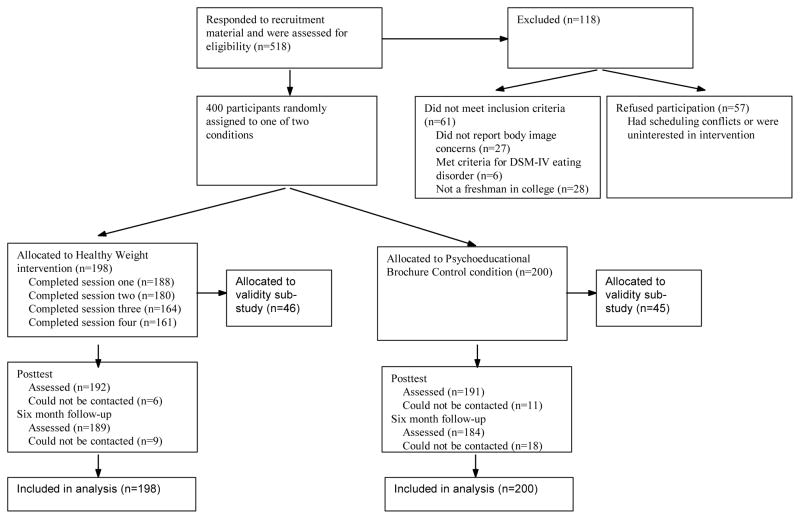
Participants were 398 young women (M age=18.4, SD=0.6; M BMI=23.7, SD=4.3; 83% White, 8% Latino, 7% Asian, 2% Black) recruited from a university using mailings, flyers, and leaflets inviting freshman women with body image concerns to participate in a trial evaluating body acceptance interventions; written consent was obtained. We focused on this population because they are at increased risk for weight gain and eating disorders. The sole exclusion criterion was current anorexia nervosa, bulimia nervosa, or binge eating disorder. Participants were randomized to the Healthy Weight 2 intervention or an educational brochure control condition via coin toss (Fig. 1 provides a participant flowchart). See Table 1 for a description of the intervention, which consisted of 4 weekly 1-hour group sessions with 6–10 participants, facilitated by clinical graduate students. Facilitators read the intervention script and attended a 4-hr workshop to role-play core session elements and discuss process issues. Drs. Rohde and Shaw independently coded a randomly selected 50% of the audiotaped sessions for fidelity and competence (fidelity and competence rating inter-rater agreement; ICC=.92 & .96 respectively). Supervision was provided based on tape review. The educational brochure was Ten Steps to Positive Body Image from the National Eating Disorders Association. Participants provided data at pre, post, and 6-mo follow-up. Assessors attended 24 hrs of training and had to demonstrate inter-rater agreement (k > .80) with supervisors using recorded interviews before collecting data. Participants received $30 per assessment. The local IRB approved this project.
Figure 1.
Participant Flow Throughout the Study
Table 1.
Description of the Healthy Weight 2 Intervention
| Session 1. Participants are told that making small lasting healthy changes to dietary intake and physical activity to bring their energy intake into balance with their energy output, and thus achieve and maintain a healthier body weight and body satisfaction, should reduce unhealthy weight control behaviors that increase risk for obesity and eating disorders. They make public voluntary commitment to making lasting healthy changes to their diet and activity level. Participants are told that this class is about pursuing the healthy-ideal (not the thin-ideal) through lifestyle changes that produce energy homeostasis (not transient dieting). Principles for improving dietary intake are discussed (substituting healthy foods with healthy ones, starting meals with high-water content/high-fiber foods, reducing portion sizes, limiting food variety per meal, not having unhealthy foods in the living environment). Next, principles for increasing physical activity are discussed (scheduling in exercise, adding incidental exercise to current routine, being creative about adding activity). Each then publically commits to making a healthy change to their dietary intake and physical activity, which reinforce lifestyle changes and fostered self-efficacy. Over the next week, participants complete a 3-day food and exercise diary to identify ways to make small improvements in their diet and activity levels. |
| Session 2. To enhance motivation, participants brainstorm benefits of maintaining a healthy body weight. Participant then review the eating and exercise diaries and the dietary and exercise changes made during the past week. To further enhance motivation, participants then discuss the importance of exercise and list the benefits of regular activity. Participants discuss ways to incorporate regular activity into their schedules, with an emphasis on overcoming challenges. They are cautioned against using unhealthy weight control behaviors (e.g., cigarettes) and are encouraged to focus on body shape instead of weight. The homework assignment is to list 10 personally meaningful reasons for pursuing the healthy ideal, to complete the eating and exercise diaries, make one additional improvement to both their diet and activity level in the following week, and continue the individual changes selected in the first session. |
| Session 3. For motivational purposes, participants share the top reasons for pursuing the healthy ideal generated for homework. They then discuss the successes and barriers they encountered when trying to improve dietary intake and make public commitments to making further healthy alterations to their diet in the next week. They are encouraged to substitute an unhealthy food in their diet with a fruit or vegetable. Emotional eating is discussed and alternative methods for coping are brainstormed. Then they share changes in their activity level during the past week and commit to make additional healthy changes to their activity level in the next week. The importance of variety in exercise and balancing cardiovascular, strength, and flexibility training are emphasized. Homework consists of continuing to complete the eating and exercise diaries, making one additional improvement in both diet and activity domains, and maintaining previous changes. |
| Session 4. To enhance motivation, participants share the benefits of attaining a healthy weight and the positive effects of being in the group. They discuss the successes and problems they encountered when trying to improve dietary intake and activity levels, and make public commitments to further healthy changes to their diet and exercise levels that they will maintain for the next 6 months. Members provide support for each other and suggest ways to overcome barriers created by resistance to change and the college environment. To reduce risk for relapse, participants discuss future obstacles that might arise that would cause them to stop the healthy lifestyle changes, differentiating a “lapse” from a “relapse” in terms of health behavior change. They share their reasons for signing up for the group and what they had hoped to accomplish. They are asked to e-mail the facilitators regarding their progress in making lifestyle changes in the upcoming week. |
The Eating Disorder Diagnostic Interview assessed DSM-IV eating disorder symptoms. Items assessing symptoms in the past month were summed.1 The symptom composite showed internal consistency (α=.84), inter-rater agreement (ICC r=.93), and 1-week test-retest reliability (ICC r=.95) in this study, as well as sensitivity to detect intervention effects (Stice et al., 2008). Age-adjusted BMI percentile was used to reflect height-adjusted weight, which correlates with direct measures of body fat (r=.80–.90) (Pietrobelli et al., 1998). The Block Food Frequency Questionnaire assessed frequency of consumption of specific food types over the past 2 weeks; this scale has shown 2-week test-retest reliability (M r=.69) and correlated (r=.57) with 4-day food record estimates for energy intake (Block & Subar, 1992). The Dutch Restrained Eating Scale assesses the frequency of dieting behaviors; this scale has shown internal consistency (α=.95), 2-week test-retest reliability (r=.82), and convergent validity with self-reported caloric intake (but not objectively measured caloric intake)(Stice, Fisher, & Lowe, 2004; van Strien et al., 1986). The Paffenbarger Activity Questionnaire (Paffenbarger, Wing, & Hyde, 1978) assessed physical activity during the past 2 weeks; this scale has shown 1-mo test-retest reliability (r=.72) and convergent validity with physical activity records (r=.28–.86, Ainsworth et al., 1993). The Body Dissatisfaction Scale assessed discontent with 9 body parts; this scale has shown internal consistency (α=.94), 3-week test-retest reliability (r=.90), and predictive validity for eating disorder onset (Stice, Marti, & Durant, 2011b). Sixteen items assessing major depressive symptoms were drawn from the Schedule for Affective Disorders and Schizophrenia for School-Age Children, a semi-structured diagnostic interview: this symptom composite has shown internal consistency (α=.75), 1-week test-retest reliability (r=.93), and inter-rater agreement (r=.85, Stice, Rohde, Gau, & Wade, 2010). Participants reported the amount of pressure to be thin they perceived from family, friends, dating partners, and the media on the 8-item Perceived Sociocultural Pressure Scale (Stice et al., 2011b); this scale has shown internal consistency (α=.88), 2-week test-retest reliability (r=.93), and predictive validity for increases in bulimic symptoms (Stice et al., 2011b).2 A randomly selected 88 participants completed an objective biological measure of energy expenditure and caloric intake to validate self-reported physical activity and energy intake. Doubly labeled water (DLW) was used to estimate energy expenditure and intake over a 2-week period (see Stice et al., 2011a).
Results
In total, 67% of Healthy Weight 2 participants attended all 4 sessions, 18% attended 3 sessions, 5% attended 2 sessions, and 10% attended 1 session. Implementation fidelity ratings (1–10 scale) had a mean of 7.3 (SD = .62). Facilitator competence ratings (10-point scale) had a mean of 7.3 (SD = .75).3 DLW estimated intake correlated with reported intake (r=.36, p=.001) and DLW estimated expenditure correlated with reported expenditure (r=.22, p=.05), but the magnitude of these relations imply these self-reported measures should be interpreted with care.
Random effects Analysis of Covariance models, with pretest values of the dependent variable as covariates, tested for intervention effects. If group or group × time effects were even marginal (p<.10), we tested for intervention effects at posttest and 6-mo follow-up, as it is often the case that significant intervention differences exist with marginal omnibus tests. We used multiple-imputation to account for missing data. Missing data were imputed using the Amelia package of the R project. We created 20 imputed data sets and used SAS PROC MIXED to analyze each data set and MIANALYZE to generate inferential statistics, where parameters are averaged across the results of the 20 analyses and the standard errors combine within and between analysis variability. Table 2 provides average means and standard deviations for the 20 imputed data sets. Table 3 presents results for the outcomes. For the eating disorder symptom outcome, there were significant effects for group, time, and group × time interaction; follow-up contrasts examining the effects of condition at each time point, controlling for pretest values of the outcome, found that the intervention participants showed significantly fewer eating disorder symptoms than controls at posttest (p=.003, d=.30), but not at 6-mo follow-up (n.s.). There was a marginal group × time interaction for BMI; follow-up contrasts indicated that intervention participants showed significantly lower BMI than controls at 6-mo follow-up (p=.035, d=.21), but no significant differences at posttest (n.s.).4 There were no significant effects for depressive symptoms or caloric intake. There was a marginal main effect indicating less dieting in the intervention group; follow-up contrasts found that relative to controls, intervention participants showed marginally less dieting at posttest (p=.071, d=.18) and significantly less dieting at 6-mos (p=.040, d=.21). There was a significant time and group effect for body dissatisfaction; follow-up contrasts indicated that intervention participants showed significantly lower body dissatisfaction than controls at posttest (p=.012, d=.25), but not at 6-mo follow-up (n.s.). There was a significant group × time interaction for physical activity; follow-up contrasts indicated that intervention participants reported significantly higher amounts of physical activity than controls at posttest (p=.010, d=.26), but not at 6-mo follow-up (n.s.).
Table 2.
Means (SD) for Outcomes in the Control and Intervention Conditions
| Variable | Condition | Pretest M (SD) |
Posttest M (SD) |
6-Months M (SD) |
|
|---|---|---|---|---|---|
| Primary | Eating Disorder Symptoms | Control | 10.44 (8.63) | 8.27 (9.38) | 6.43 (6.96) |
| Intervention | 10.22 (10.95) | 6.11 (6.51) | 6.05 (7.13) | ||
| BMI | Control | 23.99 (4.48) | 24.09 (4.51) | 24.21 (4.56) | |
| Intervention | 23.51 (4.14) | 23.62 (4.14) | 23.53 (4.13) | ||
| Secondary | Body Dissatisfaction | Control | 3.37 (0.67) | 3.23 (0.73) | 3.04 (0.74) |
| Intervention | 3.37 (0.71) | 3.09 (0.81) | 2.97 (0.88) | ||
| Depressive Symptoms | Control | 1.40 (0.45) | 1.15 (0.24) | 1.21 (0.37) | |
| Intervention | 1.43 (0.44) | 1.12 (0.23) | 1.21 (0.39) | ||
| Dieting | Control | 2.98 (0.79) | 2.87 (0.76) | 2.74 (0.84) | |
| Intervention | 2.88 (0.78) | 2.69 (0.75) | 2.54 (0.84) | ||
| Dietary Intake | Control | 1357.14 (491.04) | 1285.47 (497.27) | 1300.90 (520.17) | |
| Intervention | 1344.39 (643.84) | 1205.83 (463.94) | 1239.40 (487.86) | ||
| Physical Activity | Control | 7356.36 (6437.07) | 6401.69 (5759.14) | 6357.44 (5627.12) | |
| Intervention | 6085.46 (4203.74) | 7018.53 (4566.51) | 5665.06 (4587.22) |
Table 3.
Intervention Effects on Primary and Secondary Outcomes
| Variable | Model Component | Parameter | B | SE | t | p | d |
|---|---|---|---|---|---|---|---|
| Eating Disorder Symptoms | Fixed | Intercept | 4.34 | 0.69 | 6.29 | 0.000 | 0.63 |
| Pretest Eating Disorder Symptoms | 0.30 | 0.08 | 3.73 | 0.000 | 0.37 | ||
| Quadratic Pretest Eating Disorder Symptoms | 0.00 | 0.00 | 2.11 | 0.035 | 0.21 | ||
| Group | −1.97 | 0.65 | −3.02 | 0.003 | −0.30 | ||
| 6-month | −1.84 | 0.58 | −3.15 | 0.002 | −0.32 | ||
| Group X 6-month | 1.78 | 0.83 | 2.15 | 0.032 | 0.22 | ||
| BMI | Fixed | Intercept | 0.56 | 0.22 | 2.48 | 0.013 | 0.25 |
| W1bmi | 0.98 | 0.01 | 109.44 | 0.000 | 10.97 | ||
| Group | −0.00 | 0.10 | −0.03 | 0.975 | −0.00 | ||
| 6-month | 0.11 | 0.09 | 1.28 | 0.203 | 0.13 | ||
| Group X 6-month | −0.20 | 0.12 | −1.69 | 0.092 | −0.17 | ||
| Body Dissatisfaction | Fixed | Intercept | 0.45 | 0.12 | 3.58 | 0.000 | 0.36 |
| Pretest Body Dissatisfaction | 0.83 | 0.04 | 23.52 | 0.000 | 2.36 | ||
| Group | −0.14 | 0.06 | −2.52 | 0.012 | −0.25 | ||
| 6-month | −0.19 | 0.04 | −4.66 | 0.000 | −0.47 | ||
| Group X 6-month | 0.08 | 0.06 | 1.41 | 0.160 | 0.14 | ||
| Depressive Symptoms | Fixed | Intercept | 1.17 | 0.14 | 8.61 | 0.000 | 0.86 |
| Pretest Depressive Symptoms | −0.31 | 0.17 | −1.78 | 0.075 | −0.18 | ||
| Quadratic Pretest Depressive Symptoms | 0.19 | 0.05 | 3.73 | 0.000 | 0.37 | ||
| Group | −0.03 | 0.03 | −1.22 | 0.222 | −0.12 | ||
| 6-month | 0.06 | 0.02 | 2.59 | 0.010 | 0.26 | ||
| Group X 6-month | 0.03 | 0.03 | 0.84 | 0.401 | 0.08 | ||
| Dieting | Fixed | Intercept | 0.69 | 0.10 | 6.76 | 0.000 | 0.68 |
| Pretest Dieting | 0.73 | 0.03 | 23.47 | 0.000 | 2.35 | ||
| Group | −0.10 | 0.06 | −1.81 | 0.071 | −0.18 | ||
| 6-month | −0.13 | 0.04 | −2.91 | 0.004 | −0.29 | ||
| Group X 6-month | −0.02 | 0.06 | −0.28 | 0.783 | −0.03 | ||
| Caloric Intake | Fixed | Intercept | 385.33 | 76.98 | 5.01 | 0.000 | 0.50 |
| Pretest DFFQ | 0.77 | 0.08 | 9.54 | 0.000 | 0.96 | ||
| Quadratic Pretest DFFQ | −0.00 | 0.00 | −3.59 | 0.000 | −0.36 | ||
| Group | −59.70 | 40.81 | −1.46 | 0.144 | −0.15 | ||
| 6-month | 15.43 | 37.11 | 0.42 | 0.678 | 0.04 | ||
| Group X 6-month | 18.14 | 51.71 | 0.35 | 0.726 | 0.04 | ||
| Physical Activity | Fixed | Intercept | 2971.90 | 409.56 | 7.26 | 0.000 | 0.73 |
| Pretest Paffenbarger | 0.47 | 0.03 | 14.13 | 0.000 | 1.42 | ||
| Group | 1209.40 | 464.44 | 2.60 | 0.010 | 0.26 | ||
| 6-month | −40.61 | 435.09 | −0.09 | 0.926 | −0.01 | ||
| Group X 6-month | −1312.86 | 616.39 | −2.13 | 0.034 | −0.21 | ||
| Intercept | 2660155 | ||||||
| Residual | 17641829 |
Moderator analyses revealed three significant interactions. First, pretest eating disorder symptoms moderated the intervention effects on eating disorder symptoms: the intervention × eating disorder symptom interaction was significant (p=.003, d=.30), and the intervention × time × eating disorder symptom interaction was marginal (p=.072, d=.18). Follow-up analyses compared simple slopes of the outcome at posttest and 6-mo follow-up for participants at one standard deviation above and below the pretest eating disorder symptom mean. Intervention participants showed significantly lower eating disorder symptoms than controls at 6-mo follow-up (p<.001, d=.42) for participants with initial elevations in eating disorder symptoms; no other simple slope comparisons were significant. Second, pretest pressure to be thin moderated the intervention effects on eating disorder symptoms: the intervention × time × pressure to be thin interaction was significant (p=.017, d=.24). Follow-up analyses found that intervention participants showed significantly lower eating disorder symptoms than controls at posttest follow-up than controls (p=.003, d=.30) for participants at one SD above the pretest mean on pressure to be thin: no other simple slope comparisons were significant. Third, pretest eating disorder symptoms moderated the intervention effects on BMI: the intervention × time × eating disorder symptom interaction was significant (p=.037, d=.21). Follow-up analyses found that intervention participants showed significantly lower BMI scores than controls at 6-mo follow-up (p=.015, d=.25) for participants at one SD above the mean in pretest eating disorder symptoms; no other simple slope comparisons were significant.
Discussion
Healthy Weight 2 participants showed greater reductions in eating disorder symptoms at posttest (but not at 6-mo follow-up). This is noteworthy as only a few programs have reduced interview-assessed DSM-IV eating disorder symptoms, other programs targeting both eating pathology and obesity have only reduced selected eating disorder symptoms, and the Healthy Weight 2 intervention was only 4 hrs in duration, which is much shorter than the 16–26 hour duration of other prevention programs targeting these dual outcomes. Intervention participants also showed smaller increases in BMI at 6-mo follow-up (but not at posttest), which is notable as it suggests that behavioral changes made after intervention termination contributed to the reduced risk for unhealthy weight gain, implying maintenance of healthy lifestyle changes. The fact that this prevention program produced significant intervention effects for both eating disorder symptoms and BMI is encouraging, as only three other prevention programs have reduced risk for eating disorder symptoms and unhealthy weight gain. However, the eating disorder symptom effect was not significant at 6-mo follow-up and the BMI effect was not significant at posttest, suggesting a limited persistent of effects. It may have been difficult to show an effect at posttest because weight change can be quite slow. Further, the fact that the original 3 hr Healthy Weight intervention produced larger and more persisting effects for eating disorder symptoms and BMI (Stice et al., 2008) implies that adding principles to facilitate healthy dietary and exercise changes, largely drawn from nutrition research, did not improve intervention effects. The lack of such guidelines in the original Healthy Weight intervention may have put more of the onus of change on each participant, increasing personal investment in and motivation to maintain the selected dietary and exercise changes. However, it is equally possible that the effects were weaker because the mean eating disorder symptom score at baseline was nearly half a SD lower and because participants were 1.4 years older on average relative to the past trial (Stice et al., 2008), implying participants in the present trial were at lower risk. The limited effects in the present trial were apparently not due to limited statistical power.
Intervention versus control participants reported increased exercise at posttest, reduced dieting at posttest (marginally) and 6-mo follow-up, and reduced body dissatisfaction at posttest, but there were no intervention effects for depression or reported caloric intake. Although the effect for physical activity was encouraging, it should be interpreted with care given the validity of self-reported activity. The significant decrease in reported dieting was consistent with the Healthy Weight 2 goal of lasting lifestyle changes in dietary intake and physical activity, rather than transient dieting. The pattern of findings suggests that the improved body satisfaction at posttest may have resulted from increased physical activity or the therapeutic effects of working toward making healthy lifestyle changes, rather than actual weight loss. It is reassuring that an intervention that promoted lasting reductions in caloric intake and increases in physical activity did not produce iatrogenic effects. Further, the overall pattern of findings also suggests that the reduced eating disorder symptoms and ineffective transient weight loss dieting behaviors, and the increased physical activity and body satisfaction at posttest may have contributed to the reductions in BMI by 6-mo follow-up. The fact that there were significant reductions in both reported dieting and BMI by 6-mo follow-up may imply that this intervention will reduce risk for onset of threshold/subthreshold eating disorders over longer-term follow-up.
Moderator analyses indicated that intervention effects on eating disorder symptoms were stronger for participants with initially greater symptoms and pressure to be thin. The former finding suggests that gradually improving dietary intake and increasing activity allows young women to discontinue unhealthy eating disordered behaviors that may be used for the purposes of weight control. Likewise, this intervention may help young women who perceive elevated pressure to be thin to engage in healthier weight control behaviors, rather than escalate pathological eating behaviors aimed at weight control. This interpretation also fits with the evidence that the Healthy Weight 2 intervention reduced weight gain for participants with initially elevated eating disorder symptoms, but not those with initially low eating disorder symptoms. Results collectively imply that there may be an intriguing interplay between eating disorder symptoms and unhealthy weight gain in young women with body image concerns.
It is important to consider the study limitations. First, our validity sub-study indicated that self-reported dietary intake and activity showed modest correlations with biologically estimated total energy intake and total energy expenditure, converging with a broad literature on the limited validity of self-reported dietary intake and activity level. Second, the sample included college students who were predominantly White, suggesting that care should be taken in generalizing the results to more ethnically and educationally diverse populations, who also suffer from eating disorders and show elevated obesity prevalence. Third, the sample consisted solely of young women, implying that results should not be generalized to young men.
With regard to clinical implications, the fact that a very brief group intervention resulted in intervention effects for both eating disorder symptoms and weight gain is novel, as other programs that have attempted to affect both outcomes have produced limited effects for DSM-IV eating disorder symptoms. However, prior to dissemination, it will be vital to enhance the efficacy of this intervention, potentially by increasing its duration, which would provide even more time for healthy behavior change. We also suspect that adding dissonance-induction procedures to produce greater internalization of healthy lifestyle goals and lasting behavior change could contribute to larger effects. Further, the fact that the Healthy Weight 2 intervention produced a larger unhealthy weight gain effect for the subset of young women with elevated eating disorder symptoms suggests that another way to improve the efficacy of this intervention would be to target young women with both body image concerns and subthreshold eating disorder symptoms. Finally, it may be advantageous to design interventions that reduce negative affect, unlike the present intervention, as it is a risk factor for both weight gain and eating disordered behaviors (Stice et al., 2011b). Although clearly encouraging, this intervention may, with continued refinement, succeed in more robustly preventing both eating pathology and obesity.
Acknowledgments
This study was supported by grant (DK072932) from the National Institutes of Health.
We thank project research assistants Cara Bohon, Shelley Durant, Erica Marchand, Janet Ng, and Alex Stanton, as well as the undergraduates who volunteered to participate in this trial.
Footnotes
Items assessing the behavioral (e.g., frequency of binge eating episodes, vomiting, laxative/diuretic use, fasting, and excessive exercise) and attitudinal features (e.g., fear of weight gain, overvaluation of weight/shape, feelings of depression or guilt about overeating) of anorexia nervosa, bulimia nervosa, and binge eating disorder over the past month were summed to form the overall symptom composite. This symptom composite was normalized with a log base10 transformation, though raw items are reported in Table 2.
Please note, we asked participants to report on attitudes and behaviors since the last assessment at posttest and at 6-mo follow-up.
Implementation fidelity scores ranged from 3 to 9 (only 6.7% of the components had less than “fair” adherence, defined as a score of < 5). Facilitator competence scores ranged from 4 to 10 (only 5.6% of items were rated less than “good/average” competence, defined as a score of 5 or less). Mean values for individual fidelity and competence items showed limited variability (range = 6.4–8.0 for fidelity and 6.9–8.0 for competence ratings).
It should be noted that there was no evidence that the intervention resulted in unhealthy weight loss. While three controls transitioned from above a BMI of 18 at baseline to slightly below during follow-up, only two intervention participants made this transition. Further, the absolute reduction in weight for these five participants was 0.80 kg at follow-up and 0.88 kg at 6-mos.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Austin S, Field A, Wiecha J, Peterson K, Gortmaker S. The impact of a school-based obesity prevention trial on disordered weight-control behaviors in early adolescent girls. Archives of Pediatric Medicine. 2005;159:225–230. doi: 10.1001/archpedi.159.3.225. [DOI] [PubMed] [Google Scholar]
- Block G, Subar AF. Estimates of nutrient intake from a food frequency questionnaire. Journal of the American Dietetic Association. 1992;92:969–977. [PubMed] [Google Scholar]
- Ello-Martin J, Roe L, Rolls B. A diet reduced in energy density results in greater weight loss than a diet reduced in fat. Obesity Research. 2004;12:A23–A23. [Google Scholar]
- Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity. 2007;15:2748–2760. doi: 10.1038/oby.2007.327. [DOI] [PubMed] [Google Scholar]
- Irving L, Neumark-Sztainer D. Integrating primary prevention of eating disorders and obesity: Feasible or future? Prevention Medicine. 2002;34:299–309. doi: 10.1006/pmed.2001.0997. [DOI] [PubMed] [Google Scholar]
- Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: A prospective analysis. Journal of Abnormal Psychology. 2005;114:119–124. doi: 10.1037/0021-843X.114.1.119. [DOI] [PubMed] [Google Scholar]
- Jones M, Luce K, Osborne M, Taylor K, Cunning D, Doyle A, et al. Randomized, controlled trial of an Internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics. 2008;121:453–462. doi: 10.1542/peds.2007-1173. [DOI] [PubMed] [Google Scholar]
- Paffenbarger R, Wing A, Hyde R. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology. 1978;108:161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A, Faith M, Allison D, Gallagher D, Chiumello G, Heymsfield S. Body mass index as a measure of adiposity among children and adolescents: A validation study. Journal of Pediatrics. 1998;132:204–210. doi: 10.1016/s0022-3476(98)70433-0. [DOI] [PubMed] [Google Scholar]
- Stice E, Durant S, Burger K, Schoeller D. Weight suppression and risk for future increases in body mass: Effects of suppressed resting metabolic rate and energy expenditure. American Journal of Clinical Nutrition. 2011a;94:7–11. doi: 10.3945/ajcn.110.010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Fisher M, Lowe M. Are dietary restraint scales valid measures of dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment. 2004;16:51–59. doi: 10.1037/1040-3590.16.1.51. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Durant S. Risk factors for onset of eating disorders: Evidence of multiple risk pathways from an 8-year study. Behaviour Research and Therapy. 2011b;49:622–627. doi: 10.1016/j.brat.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Ragan J. A controlled evaluation of an eating disturbance psychoeducational intervention. International Journal of Eating Disorders. 2002;31:159–171. doi: 10.1002/eat.10018. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010;78:856–867. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T, Frijters J, Van Staveren W, Defares P, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]