Abstract
Background: Sickness absence in Sweden is high, particularly in young women and the reasons are unclear. Many Swedish women combine parenthood and work and are facing demands that may contribute to impaired health and well-being. We compared mothers and women without children under different conditions, assuming increased sickness absence in mothers, due to time-based stress and psychological strain. Methods: All women born in 1960–79 (1.2 million) were followed from 1993 to 2003. Information on children in the home for each year was related to medically certified sickness absence with insurance benefits the year after. We used age and time-stratified proportional hazard regression models accounting for the individual's changes on study variables over time. Data were retrieved from national administrative registers. Results: Sickness absence was higher in mothers than in women without children, the relative risks decreased by age, with no effect after the age of 35 years. An effect appeared in lonely women irrespective of age, while in cohabiting women only for the ages 20–25 years. Mothers showed increased sickness absence in all subgroups of country of birth, education, income, sector of employment and place of residence. The relation between number of children and sickness absence was nonlinear, with the highest relative risks for mothers of one child. The upward trend of sickness absence at the end of 1990s was steeper for mothers compared to women without children. Conclusion: Despite the well-developed social security system and child care services in Sweden, parenthood predicts increased sickness absence, particularly in young and in lone women.
Introduction
After a period of falling sickness absence in Sweden during the 1990s, there was a rapid increase from 1997 through 2002 that was steeper in women than in men. Since 2003, the rates are now decreasing.1 Nevertheless, sickness absence in Sweden, particularly absence of long duration, is still high compared to the OECD average.2
In general, female employees in European countries have more sickness absence than men.1 In Sweden, around two-thirds of all days with sickness benefits from the social insurance system can be ascribed to women.3 The reasons for the high level of sickness absence in women are not fully understood. To some extent, the high level depends on medical problems related to pregnancy, which have been estimated to account for ∼4% of sickness benefit costs among women.3,4
There is evidence that certain jobs are related to sickness absence, such as employment in the health care, educational and social sector, jobs that most often are held by women.3 Further, the psychosocial work environment is influential, with low job satisfaction 5,6, high demands, low or high decision latitude increasing the risk of sickness absence in women.7–16 Work-related conditions have been suggested as the most important explanation for the gender difference in sickness absence in Sweden.3
The potential health effects in women of combining work and family life have been debated for a long time, often in terms of the ‘role enhancement’ and the ‘role overload’ hypotheses.17–21 ‘Role enhancement’ meaning that multiple roles entail beneficial effects by increased stimulation, extended access to environmental resources and social affirmation. ‘Role overload’ meaning that the ‘double burden’ is detrimental due to time- and strain-based overload or conflicts. Certainly, both hypotheses have validity and a pertinent question should be to identify specific conditions leading to an overload that may affect health and work ability.
A Finnish research group found that having children increased the domestic work hours from 15.5 to 23.1 per week in women and that a high level of total work hours was associated with sickness absence, attributed to high levels of domestic work and commuting hours.10,22 Other studies have found associations between having children, or difficulties to combine employment and care of children/family and sickness absence,23–28 while others have reached other conclusions.9,29–31
In two previous studies, we found that women with children had higher risks of poor self-rated health and fatigue than women without children, and that the risk estimates were most pronounced among lone women, high-income earners and women with fulltime employment.32,33 The current study has its focus on sickness absence and the idea is to explore if an impaired health in mothers may be observed also by increased sickness absence. We used a prospective population study design, taking different demographical and socio-economical conditions into consideration. The study is unique because of the size and representativeness of young Swedish women holding all kinds of occupations.
Sickness absence with economic compensation from the Swedish Social Insurance System (SSIS), a measure of medically certified illness tied to reduced work ability, was studied. The measure is more directly related to societal costs and may therefore be perceived as more relevant among policy makers, compared to self-reported health symptoms.
Methods
Study base
The population comprised all women in Sweden born in 1960–79 provided, they had reached the age of 20 years, in total 1 233 701 women. The time of observation was from 1 January 1993 through 2003. Data were retrieved from the Longitudinal integration database for health insurance and labour market studies (LISA), a register which in turn is based on more than 10 national administrative registers.
Exposure
Having children was treated as a time-dependent exposure variable. For each year of observation, the prevalence of any children <18 years of age living in the home was assessed as well as the number of children (no children, one, two and three or more children).
Outcome variable
We studied medically certified sickness absence with sickness benefits from the SSIS, in 1993–2003. Sickness benefits were paid by the SSIS if a spell of absence exceeded 14 days. Except for one qualifying day (with no economic compensation), the employer covered the sick pay from the 2nd to the 14th day of absence. This was the rule for all years in 1993–2003, except for 15 months from January 1997 through March 1998, when the employer's sick pay period was 28 days.
A woman was recorded as a case if she had at least one spell of sickness absence lasting for ≥15 (or 29) days during a year. One day of sickness absence corresponds to a calendar day without adjustment for part-time compensation.
Stratification variables
The relation between having children and the incidence of sickness absence was studied overall and in demographic and socio-economic subgroups to reveal potential effect modification. The stratification also reduces the potential for confounding within the subgroups.
Demographical and socio-economic characteristics were assessed on a yearly basis:
control for age and calendar year (1-year intervals) was built into the programme. In the explicit analyses of age, 5-year intervals were used starting at the age of 20 and with 35–43 years as the upper category;
place of residence comprised metropolitan areas including Stockholm, Gothenburg or Malmö (with surrounding municipalities), city areas (municipalities with more than 90 000 inhabitants within 30 km from the centre) and rural areas (remaining areas);
partner status was dichotomized into cohabiting (married or cohabiting with children in common) and lone women, also including women living with a partner but with no children in common, divorced and widowed. According to the registration system, an unmarried woman is classified as cohabiting only if the couple has children in common. This means that the reference group (no children) for cohabiting women only comprises married women without children;
education was classified as low (≤9 years), medium (10–12 years) and high education (>12 years);
income corresponds to the individual's total income including salary, social benefits and financial compensation. High income was above the upper quartile of the income distribution, low income below the lower quartile and medium income comprised the values in between. Other family income was not included;
employment sector was divided into state governmental, local governmental or county council employment and private sector employment;
country of birth was classified into three groups: Sweden, other Nordic countries (Norway, Denmark, Finland and Iceland) and countries outside the Nordic region.
Furthermore, some socio-economic variables were combined: partner status with age group and income, income level with education and employment sector (table 2).
Table 2.
Incidence of sickness absence with insurance benefits in Swedish women with and without children, by combined socio-economic strata
| Person-years | Total no.a (in 1000s) | Crude rate | Number of children |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Any number vs. none |
1 vs. none |
2 vs. none |
≥3 vs. none |
||||||||
| noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | ||||
| Partner status and Age group, 1993–2003 | |||||||||||
| Cohabiting and 20–25 years | 254 306 | 40 | 0.16 | 32 | 1.25 (1.22–1.28) | 23 | 1.33 (1.30–1.37) | 8 | 1.05 (1.02–1.09) | 1 | 1.14 (1.06–1.22) |
| Cohabiting and 26–30 years | 907 939 | 131 | 0.14 | 111 | 0.98 (0.97–1.00) | 54 | 1.15 (1.13–1.17) | 45 | 0.83 (0.81–0.84) | 12 | 0.97 (0.95–0.99) |
| Cohabiting and ≥30 years | 2 105 989 | 248 | 0.12 | 232 | 0.78 (0.77–0.79) | 56 | 1.02 (1.00–1.04) | 114 | 0.68 (0.67–0.70) | 62 | 0.80 (0.78–0.81) |
| Lone and 20–25 years | 1 940 601 | 121 | 0.06 | 10 | 2.41 (2.36–2.46) | 8 | 2.39 (2.34–2.45) | 2 | 2.49 (2.37–2.61) | 0.14 | 2.43 (2.06–2.87) |
| Lone and 26–30 years | 1 191 830 | 119 | 0.10 | 27 | 1.89 (1.86–1.92) | 16 | 1.83 (1.80–1.87) | 9 | 1.94 (1.90–1.98) | 2 | 2.18 (2.09–2.28) |
| Lone and ≥30 years | 1 036 237 | 137 | 0.13 | 68 | 1.40 (1.39–1.42) | 29 | 1.36 (1.34–1.38) | 28 | 1.37 (1.35–1.39) | 12 | 1.63 (1.59–1.66) |
| Partner status and Income, 1993–2003 | |||||||||||
| Cohabiting and High | 1 036 108 | 125 | 0.12 | 110 | 0.91 (0.89–0.92) | 27 | 1.10 (1.08–1.12) | 49 | 0.76 (0.75–0.78) | 34 | 0.99 (0.97–1.01) |
| Cohabiting and Medium | 1 736 515 | 235 | 0.14 | 213 | 0.87 (0.86–0.89) | 78 | 1.06 (1.04–1.07) | 100 | 0.73 (0.72–0.74) | 35 | 0.82 (0.80–0.83) |
| Cohabiting and Low | 486 148 | 57 | 0.12 | 51 | 1.18 (1.15–1.21) | 28 | 1.41 (1.37–1.44) | 17 | 0.93 (0.90–0.96) | 5 | 0.78 (0.75–0.81) |
| Lone and High | 1 022 290 | 118 | 0.12 | 64 | 1.88 (1.86–1.91) | 23 | 1.79 (1.76–1.82) | 28 | 1.87 (1.84–1.90) | 12 | 2.18 (2.13–2.22) |
| Lone and Medium | 1 969 292 | 198 | 0.10 | 37 | 1.49 (1.47–1.51) | 26 | 1.53 (1.51–1.55) | 9 | 1.38 (1.35–1.41) | 1 | 1.37 (1.30–1.44) |
| Lone and Low | 1 157 094 | 60 | 0.05 | 4 | 1.42 (1.37–1.47) | 3 | 1.53 (1.47–1.59) | 1 | 1.17 (1.08–1.25) | 0.15 | 1.07 (0.91–1.26) |
| Education and Income, 1993–2003 | |||||||||||
| High-High | 854 638 | 82 | 0.10 | 49 | 1.19 (1.18–1.21) | 18 | 1.55 (1.52–1.58) | 22 | 0.98 (0.96–1.00) | 9 | 1.07 (1.04–1.10) |
| High-Medium | 1 140 009 | 106 | 0.09 | 56 | 1.25 (1.23–1.26) | 27 | 1.63 (1.60–1.65) | 23 | 0.94 (0.92–0.96) | 6 | 0.92 (0.90–0.95) |
| High-Low | 573 506 | 28 | 0.05 | 13 | 1.87 (1.82–1.93) | 8 | 2.32 (2.25–2.39) | 4 | 1.32 (1.27–1.37) | 1 | 1.07 (0.99–1.15) |
| Medium-High | 1 012 885 | 128 | 0.13 | 97 | 1.41 (1.39–1.43) | 26 | 1.58 (1.55–1.60) | 44 | 1.25 (1.23–1.27) | 27 | 1.51 (1.49–1.54) |
| Medium-Medium | 2 243 430 | 275 | 0.12 | 160 | 1.23 (1.22–1.24) | 64 | 1.51 (1.49–1.52) | 72 | 1.02 (1.01–1.04) | 24 | 1.10 (1.09–1.12) |
| Medium-Low | 879 526 | 70 | 0.08 | 33 | 1.53 (1.50–1.56) | 19 | 1.86 (1.83–1.90) | 11 | 1.15 (1.12–1.18) | 3 | 0.92 (0.89–0.96) |
| Low-High | 188 965 | 32 | 0.17 | 28 | 1.41 (1.36–1.46) | 6 | 1.42 (1.36–1.48) | 12 | 1.36 (1.32–1.42) | 10 | 1.46 (1.40–1.51) |
| Low-Medium | 317 361 | 52 | 0.16 | 34 | 1.14 (1.12–1.16) | 13 | 1.26 (1.23–1.29) | 14 | 1.05 (1.02–1.07) | 7 | 1.06 (1.03–1.09) |
| Low–Low | 185 292 | 19 | 0.10 | 9 | 1.13 (1.10–1.17) | 5 | 1.36 (1.31–1.41) | 3 | 0.96 (0.92–1.00) | 1 | 0.78 (0.74–0.84) |
| Employment sector and Income, 1993–2003 | |||||||||||
| Public and High | 863 378 | 108 | 0.12 | 84 | 1.42 (1.40–1.45) | 21 | 1.63 (1.60–1.66) | 37 | 1.27 (1.25–1.30) | 26 | 1.48 (1.46–1.51) |
| Public and Medium | 1 891 135 | 231 | 0.12 | 139 | 1.28 (1.27–1.29) | 55 | 1.59 (1.57–1.61) | 63 | 1.06 (1.05–1.07) | 21 | 1.12 (1.10–1.14) |
| Public and Low | 589 981 | 46 | 0.08 | 22 | 1.99 (1.95–2.04) | 13 | 2.37 (2.32–2.43) | 7 | 1.50 (1.45–1.55) | 2 | 1.23 (1.17–1.30) |
| Private and High | 1 161 165 | 130 | 0.11 | 86 | 1.46 (1.44–1.48) | 28 | 1.68 (1.65–1.70) | 39 | 1.26 (1.24–1.28) | 19 | 1.59 (1.56–1.62) |
| Private and Medium | 1 683 633 | 186 | 0.11 | 98 | 1.37 (1.35–1.38) | 45 | 1.67 (1.65–1.69) | 41 | 1.10 (1.08–1.11) | 12 | 1.19 (1.17–1.22) |
| Private and Low | 786 990 | 54 | 0.07 | 22 | 1.76 (1.73–1.80) | 13 | 2.18 (2.13–2.23) | 7 | 1.28 (1.25–1.32) | 2 | 1.11 (1.05–1.16) |
a: the total number of years with sickness absence in the study population and in women with children (exposed cases)
b: adjusted for age and year of observation within each stratum
Statistical methods
The analytical approach was to take into account the individual's changes over time regarding the exposure, the potential confounders and the stratification variables. We based the analyses on the SAS MPHREG macro developed at the Channing Laboratory.34 The programme has been used in other studies also.35,36 The difference from a traditional Cox proportional hazard regression was that the units of observation did not correspond to individuals. Instead, a new personal data record was created for each year at which the participant was at risk of sickness absence, which allowed the values of the study variables to change for each person-year at risk. The method means that all individual changes in e.g. educational level or family composition across time were taken into account. Person-years at risk for different exposure categories in a year were linked to case status, i.e. sickness absence/no sickness absence in the following year. The relative risk (RR) was estimated by the pooled RR with a 95% confidence interval. A joint control for age and calendar year was built into the programme. The analyses were performed on subgroups according to the descriptions of demographical and socio-economical characteristics given above.
The exposure classification started in 1993 or the year of entry into the cohort and was related to case status during the following year. If the woman was on sick leave during two or more subsequent years, the exposure classification started/restarted the next year to come with no sickness absence. Thus, if a woman had a record of sickness absence during two consecutive years, the exposure classification was restarted in the third year provided she was still at risk of sickness absence. The classification was discontinued in case of emigration, disability pension or death.
A prerequisite for exposure classification was that the woman had an income tax declaration with a registered employer for the year in question. Unemployment was treated as person time at risk. In total, 1128 894 women were included in the analysis corresponding to 7436 902 person-years.
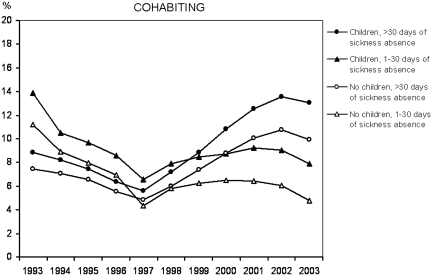
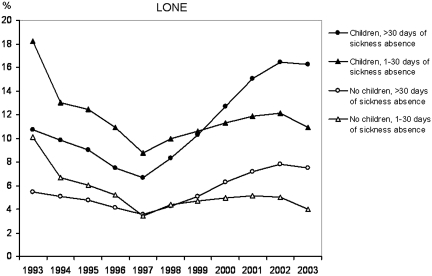
Furthermore, the prevalence of sickness absence of different duration across the years was computed. The total number of days of sickness absence with benefits from the SSIS was classified into no days, 1–30 days (short duration), or >30 days (long duration) for 1993–2003. The percentages of women with sickness absence of shorter and longer duration among lone and cohabiting women with and without children, standardized to the age distribution for all years combined, were calculated. The analysis was done to explore if the results from the main analyses (which did not take the amount of absence into account) were attributed to long or short duration of absence or both (figures 1 and 2).
Figure 1.
Cohabiting women: prevalence (%) of medically certified sickness absence with social insurance benefits (1–30 days, >30 days in a year) in women with and without children, by year (1993–2003), based on cross-sectional data. Proportions standardized to the age distribution of all years combined
Figure 2.
Lone women: prevalence (%) of medically certified sickness absence with social insurance benefits (1–30 days, >30 days in a year) in women with and without children, by year (1993–2003), based on cross-sectional data. Proportions standardized to the age distribution of all years combined
Results
Incidence of sickness absence, by demographical and socio-economic strata
The risk of sickness absence was 44% higher in mothers compared with women without children and the RR was highest for the first 5-year period (1993–97). There was no evidence of a linear increase in risk of sickness absence with increasing number of children. The risk was higher in women with three or more children than in women with two children in the home. However, the highest RR was found for having one child in the home, which pertained to all strata, except for lone women (table 1).
Table 1.
Incidence of sickness absence with insurance benefits in Swedish women with and without children, by demographical and socio-economic strata
| Person-years | Total no.a (in 1000s) | Crude rate | Number of children |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Any number vs. none |
1 vs. none |
2 vs. none |
≥3 vs. none |
||||||||
| noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | noa (in 1000s) | RRb (95%CI) | ||||
| Period of observation | |||||||||||
| 1993–2003 | 7 436 902 | 795 | 0.11 | 480 | 1.44 (1.43–1.44) | 186 | 1.73 (1.72 to1.74) | 205 | 1.20 (1.19–1.21) | 89 | 1.35 (1.33–1.36) |
| 1993–1997 | 3 324 940 | 301 | 0.09 | 172 | 1.51 (1.50–1.53) | 74 | 1.83 (1.81 to1.85) | 70 | 1.24 (1.22–1.25) | 28 | 1.38 (1.36–1.40) |
| 1998–2003 | 4 130 074 | 497 | 0.12 | 310 | 1.38 (1.37–1.39) | 113 | 1.65 (1.64–1.67) | 136 | 1.17 (1.16–1.18) | 61 | 1.31 (1.30–1.33) |
| Age group, 1993–2003 | |||||||||||
| 20–25 years | 2 194 907 | 160 | 0.07 | 41 | 2.41 (2.39–2.44) | 31 | 2.54 (2.51–2.57) | 10 | 2.08 (2.04–2.13) | 1 | 2.18 (2.05–2.32) |
| 26–30 years | 2 099 769 | 249 | 0.12 | 138 | 1.57 (1.56–1.58) | 70 | 1.78 (1.77–1.80) | 54 | 1.35 (1.33 to1.36) | 14 | 1.55 (1.52–1.58) |
| 31–35 years | 1 989 776 | 245 | 0.12 | 184 | 1.09 (1.08–1.10) | 59 | 1.36 (1.35 to1.38) | 85 | 0.95 (0.94–0.96) | 39 | 1.11 (1.09–1.12) |
| ≥36 years | 1 152 450 | 140 | 0.12 | 117 | 0.98 (0.97–1.00) | 26 | 1.19 (1.17–1.21) | 56 | 0.90 (0.88–0.91) | 34 | 1.01 (0.99–1.02) |
| Country of birth | |||||||||||
| Sweden | 6 669 992 | 706 | 0.11 | 420 | 1.45 (1.44–1.46) | 164 | 1.77 (1.76 to1.78) | 180 | 1.20 (1.19–1.21) | 75 | 1.33 (1.32–1.35) |
| Nordic countries | 177 398 | 22 | 0.13 | 15 | 1.29 (1.25 1.33) | 5 | 1.44 (1.39–1.50) | 7 | 1.15 (1.11–1.20) | 4 | 1.34 (1.28–1.40) |
| Other countries | 589 512 | 66 | 0.11 | 45 | 1.37 (1.35–1.40) | 17 | 1.46 (1.43–1.49) | 18 | 1.26 (1.23–1.29) | 10 | 1.42 (1.39–1.46) |
| Place of residence, 1993–2003 | |||||||||||
| Metropolitan areas | 2 971 007 | 305 | 0.10 | 164 | 1.45 (1.44–1.46) | 73 | 1.76 (1.74–1.78) | 67 | 1.18 (1.16–1.19) | 25 | 1.32 (1.30–1.34) |
| City areas | 2 651 452 | 270 | 0.10 | 169 | 1.45 (1.44–1.46) | 63 | 1.71 (1.69–1.73) | 74 | 1.23 (1.21–1.24) | 32 | 1.38 (1.36–1.40) |
| Rural areas | 1 812 773 | 219 | 0.12 | 146 | 1.32 (1.31–1.34) | 51 | 1.59 (1.57–1.61) | 63 | 1.12 (1.11–1.13) | 32 | 1.24 (1.22–1.26) |
| Partner status, 1993–2003 | |||||||||||
| Cohabiting | 3 268 234 | 418 | 0.13 | 374 | 0.94 (0.93–0.95) | 133 | 1.14 (1.12–1.15) | 166 | 0.79 (0.78–0.80) | 75 | 0.91 (0.90–0.92) |
| Lone | 4 168 668 | 377 | 0.09 | 105 | 1.66 (1.64–1.67) | 53 | 1.66 (1.64–1.67) | 38 | 1.61 (1.59–1.62) | 14 | 1.83 (1.70–1.86) |
| Education 1993–2003 | |||||||||||
| High | 2 577 746 | 217 | 0.08 | 117 | 1.29 (1.28–1.31) | 53 | 1.68 (1.66–1.70) | 49 | 1.00 (0.99–1.02) | 16 | 1.03 (1.01–1.05) |
| Medium | 4 146 187 | 473 | 0.11 | 290 | 1.31 (1.31–1.32) | 109 | 1.57 (1.56–1.58) | 127 | 1.11 (1.10–1.12) | 54 | 1.24 (1.23–1.26) |
| Low | 700 973 | 103 | 0.15 | 71 | 1.27 (1.25–1.29) | 24 | 1.37 (1.34–1.39) | 29 | 1.18 (1.16–1.21) | 18 | 1.23 (1.20–1.25) |
| Income 1993–2003 | |||||||||||
| High | 2 058 398 | 243 | 0.12 | 175 | 1.47 (1.46–1.48) | 51 | 1.68 (1.66–1.70) | 77 | 1.29 (1.28–1.31) | 47 | 1.57 (1.55–1.59) |
| Medium | 3 705 807 | 434 | 0.12 | 250 | 1.32 (1.31–1.33) | 104 | 1.62 (1.61–1.63) | 109 | 1.09 (1.08–1.10) | 37 | 1.17 (1.15–1.18) |
| Low | 1 643 242 | 117 | 0.07 | 55 | 1.81 (1.78–1.83) | 31 | 2.20 (2.17–2.24) | 18 | 1.36 (1.34–1.39) | 5 | 1.11 (1.07–1.14) |
| Employment sector 1993–2003 | |||||||||||
| Public | |||||||||||
| State government | 557 291 | 53 | 0.10 | 29 | 1.39 (1.37–1.42) | 13 | 1.69 (1.65–1.73) | 12 | 1.13 (1.10–1.15) | 4 | 1.38 (1.33–1.43) |
| Local government and County council | 2 718 684 | 326 | 0.12 | 212 | 1.35 (1.34–1.36) | 75 | 1.64 (1.62–1.66) | 93 | 1.14 (1.12–1.15) | 44 | 1.24 (1.22–1.25) |
| Private | 3 288 129 | 333 | 0.10 | 184 | 1.46 (1.45–1.47) | 77 | 1.75 (1.74–1.77) | 78 | 1.20 (1.18–1.21) | 29 | 1.40 (1.38–1.42) |
| Other | 415 164 | 43 | 0.10 | 25 | 1.40 (1.37–1.43) | 10 | 1.72 (1.68–1.77) | 10 | 1.18 (1.15–1.21) | 4 | 1.22 (1.17–1.26) |
a: the total number of years with sickness absence in the study population, and in women with children (exposed cases)
b: adjusted for age and year of observation within each stratum
The RRs decreased by age with the highest estimate in women in the age group of 20–30 years; whereas in the oldest age group (>35 years), there was no difference between mothers and other women (table 1).
Regardless of country of birth, there was an effect on sickness absence of having children. The RR was highest among women born in Sweden. The place of residence did also make a slight difference, in that the RR was somewhat lower in women living in rural areas (table 1).
Cohabitation status was an important effect modifier. Mothers had a 66% increase in risk compared with women without children among lone women. Married or cohabiting mothers showed a lower risk of sickness absence compared to married women without children (table 1).
In all educational groups, the risk of sickness absence was increased in mothers, with small differences between the strata. A similar pattern was found for income and employment sector. For income, the highest RR pertained to women with low income, followed by the high-income group. For employment sector, the highest estimate was found for the private sector followed by state governmental employment (table 1).
Incidence of sickness absence, by combined socio-economic strata
In cohabiting women, aged 20–25 years, the risk of sickness absence in mothers was increased, but a reverse relationship was seen in higher age groups. Lone mothers showed an effect regardless of age and the RR decreased by age (table 2).
Among lone women, the RR of sickness absence was highest in the high-income group and decreased with decreasing income. In cohabiting women, on the other hand, the RR was highest in women with low income and the RRs were below unity in high- and medium-income earners (table 2).
When education and income were combined, all subgroups showed increased risks in mothers, particularly among women with high- or medium education combined with a low income. For different employment sectors and income, again, all subgroups revealed increased risks in mothers, particularly in women employed in the public sector with a low income, although working in the private sector on a low income did also show a clear increase in risk in mothers (table 2).
The relatively high RRs for mothers of three or more children among lone women with a high income, among women in private or public employment with a high income and among women with medium or low education with a high-income level should also be pointed out (table 2).
Before 1997, sickness absence of 1–30 days with insurance benefits in a year was more prevalent than >30 days, while >30 days of absence became more prevalent thereafter—the sickness absence spells were prolonged by time. The upward trend for long duration in women with children raised from 6% in 1997 to about 15% in 2002–03 (data not shown). The dip coincides partly with the extended employer responsibility for benefits but the causation is uncertain. Figures 1 and 2 show a consistently higher prevalence of sickness absence in mothers than in women without children over the years and the association was attributed to both short and long duration of absence.
In cohabiting women, the upward trend for long duration after 1997 was slightly more pronounced in mothers compared with cohabiting women without children (figure 1). Also in lone women, the shift towards more days of sickness absence during the last part of the period was evident. The prevalence of long sick leave duration increased steeply in lone mothers after 1997 (figure 2).
Discussion
We studied sickness absence in employed women, with a focus on the implications of having children in the home, and the results showed a 44% increase in risk of sickness absence in mothers. From previous studies, we know that mothers compared with women without children are less burdened by chronic diseases, ‘a healthy mother effect’,26,32 a selection mechanism that may have suppressed the effect of having children. Another mechanism which counteracts an increased risk of sickness absence in mothers is the comparatively long periods of parental leave. Illness that would have caused sickness absence during active work may often go unregistered among women on parental leave. Concurrently, we could not exclude pregnancy-related medical problems from the sickness absence measure. However, the effect of pregnancy-related sickness absence was partly limited by the requirement of no sickness absence in the year of exposure assessment, since sickness absence during a year was always linked to the number of children the year before without sickness absence. Thus, if sickness absence was pregnancy related, it was linked to no children or the number of children before delivery of the new child, yielding a bias working against an association.
The increased risk of medically certified sickness absence exceeding 2 weeks in women with children may be due to illness such as post-delivery depression and persistent respiratory infections in families with children, but we also believe that specific socio-economic conditions may contribute to seriously reduced work ability leading to sickness absence. The results suggest that these conditions may be found particularly among young employed mothers and lone employed mothers, and we assume that a heavy total workload and poor coping resources (e.g. financial and social) may be crucial.
The non-linear relationship between number of children and sickness absence, with a lower RR for the second child could signify that women with no health problems related to the first child are more inclined to have another child. The acquired experience may also facilitate the care of a second child and the children may care for each other. Three or more children may add substantially to household duties and may also include difficulties to cope with both teenagers and small children. Probably, the most demanding transformation of women's everyday life occurs with the first child. The results of a non-linear relationship between number of children and sickness absence, partly confirm previous findings.29
The consistent results, with few exceptions across the socio-economic strata, suggest that the association should not be explained by confounding. The effect was clearly modified by age; in that, there was no association in women ≥36 years. Possibly, women approaching middle age without children have more health problems according to ‘the healthy mother effect’. Alternatively, mothers’ ability to cope with parenthood and work get better by increasing age and maturity. Also for self-rated health, we saw no effect of having children after age 35.32 Cohabitation status was also an important effect modifier. Among married or cohabiting women there was no effect, except for the youngest age group (20–25 years). The results are in line with the findings by e.g. Voss et al.31 In our study on self-rated health,32 on the other hand, there was an effect of having children not only in lone but also among cohabiting women. Possibly, the perception of poor health in cohabiting mothers does not lead to sickness absence to the same extent as among lone mothers, because the partner may take care of the children with parental benefits, should the mother fall ill and mothers in dual couples may be cared for by a wider social network, including the partner. The results for partner status and age combined, with decreasing RRs, particularly in cohabiting women, could indicate that married (or cohabiting) women with children remain married/cohabiting if they experience good work-family conditions. Less favourable conditions may by time (and age) lead to separation and a successive drain of vulnerable individuals from married into the group of lone mothers.
Lone mothers often have high financial obligations, holding them back from absence from work when ill. An even stronger association with ill-health could be hidden by sickness presence in this group, due to financial pressure. Swedish studies have shown a rather strong association between a bad financial situation and high sickness presence.37,38 A financial pressure may also cause lone mothers to work long hours with shortage of time for child care. Having three or more children, more than doubled the risk of sickness absence in lone high-income earners. We analysed further the impact of a socio-economic influence behind the increased risk in lone mothers by comparing different age groups who had achieved different levels of education. The highest RR of having children was found for the youngest women with high education [RR=3.21, 95% CI (3.05–3.38)], the lowest for the oldest with medium education [RR = 1.12, 95% CI (1.11–1.14)].
A limitation of the study was the coding rules of the central registries, mostly treating cohabitation with no children in common as being lone. Those classified as ‘lone women without children’ thus comprised women living with a partner (who might have children of his own). The ‘lone women with children’ also included women living with a partner (who also might have children of his own). If partnership improves health and well-being it may be that sickness absence is ‘underestimated’ in the groups classified as lone. The implications of the coding, as well as the importance of shared/unshared custody need further study.
Sickness absence varied considerably during the time of observation, with a decline towards 1997. After 1997, sickness absence started to rise until 2003, followed by a decline that has continued. In the beginning of 1993, a qualifying day was introduced with salary withdrawal for the first day of sick leave. The introduction of the qualifying day was followed by a decrease in sickness absence, which in women also included absence >14 days.39 The qualifying day may have been a general signal of the necessity to reduce sickness absence. Later, in 1997 the sickness benefits rose from 75% to 80% of the salary (an ‘allowing’ signal), which may have contributed to more sickness absence after 1997, a trend that was particularly steep in women with children.
It may be surprising that motherhood is associated with sickness absence, considering the well-developed social security system and child care services in Sweden. The system comprise the possibility of 10 days of temporary paternal benefits when the child is born, it allows parents to stay away from work with parental benefits for a total of 480 days until the child attains the age of 8 years, it allows temporary parental benefits for taking care of sick children for up to 120 days per child and year until the age of 12 years. In addition, the parents have access to subsidized day care services. The current system seems to serve older mothers and mothers in dual couple families well, but not young mothers and lone women with children. The social security systems vary between countries and are continuously developing. The generalizability of the present results are limited to nations with similar structures. In particular, the Nordic countries with high levels of labour market participation among women and generous social security systems may be able to learn from these results.
Funding
The Swedish Council for Working Life and Social Research (grant no 2004-1101) approved by the regional research ethics committee (Dnr: 2005/32-31).
Conflicts of interest: None declared.
Key points.
Female employees in Europe have a high level of sickness absence causing high societal expenses.
There is no consensus about the impact of combined work and parenthood on sickness absence in women and it is unclear to what extent an effect of having children might be dependent on demographic and socio-economic conditions.
This population study of Swedish women in the age group of 20–43 years of age show that having children in the home increases the risk of sickness absence, particularly among young women and lone women and that an association seems to be valid in most socio-economic strata.
Governmental policy makers and employers should aim at increasing economic and total workload equality not only between men and women, but also among women with particular attention to family composition.
References
- 1.Försäkringskassan [The Swedish Social Insurance Agency] Sjukfrånvaron i Sverige – på väg mot europeiska nivåer? [Abstract in English] Social Insurance Report. 2009;10 Stockholm Sweden: The Swedish Social Insurance Agency. [Google Scholar]
- 2.OECD. Sickness, Disability and Work: Breaking the Barriers. Sweden: Will the Recent Reforms Make it? Paris: OECD; 2009. [Google Scholar]
- 3.RFV Riksförsäkringsverket [The Swedish National Social Insurance Board] Orsaker till skillnader i kvinnors och mäns sjukskrivningsmönster – en kunskapsöversikt. RFV Analyserar. 2004;16 Stockholm, Sweden: The Swedish National Social Insurance Board [In Swedish] [Google Scholar]
- 4.RFV Riksförsäkringsverket [The Swedish National Social Insurance Board] Vad kostar sjukdomarna för kvinnor och män? RFV Redovisar. 2004;5 Stockholm, Sweden: The Swedish National Social Insurance Board [In Swedish] [Google Scholar]
- 5.Hansson T, Jensen I. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 6. Sickness absence due to back and neck disorders. Scand J Public Health Supp. 2004;63:109–51. doi: 10.1080/14034950410021862. [DOI] [PubMed] [Google Scholar]
- 6.Sandmark H. Job mismatching, unequal opportunities and long-term sickness absence in female white-collar workers in Sweden. Scand J Public Health. 2009;37:43–9. doi: 10.1177/1403494808098916. [DOI] [PubMed] [Google Scholar]
- 7.North F, Syme SL, Feeney A, et al. Explaining socioeconomic differences in sickness absence: the Whitehall II Study. BMJ. 1993;306:361–6. doi: 10.1136/bmj.306.6874.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krantz G, Ostergren PO. Do common symptoms in women predict long spells of sickness absence? A prospective community-based study on Swedish women 40 to 50 years of age. Scand J Public Health. 2002;30:176–83. doi: 10.1080/14034940210133816. [DOI] [PubMed] [Google Scholar]
- 9.Ala-Mursula L, Vahtera J, Kivimäki M, et al. Employee control over working times: associations with subjective health and sickness absences. J Epidemiol Commun Health. 2002;56(4):272–8. doi: 10.1136/jech.56.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ala-Mursula L, Vahtera J, Linna A, et al. Employee worktime control moderates the effects of job strain and effort-reward imbalance on sickness absence: the 10-town study. J Epidemiol Commun Health. 2005;59:851–7. doi: 10.1136/jech.2004.030924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lidwall U, Marklund S. What is healthy work for women and men? - A case-control study of gender- and sector-specific effects of psycho-social working conditions on long-term sickness absence. Work. 2006;27:153–63. [PubMed] [Google Scholar]
- 12.Nielsen ML, Rugulies R, Christensen KB, et al. Psychosocial work environment predictors of short and long spells of registered sickness absence during a 2-year follow up. Occup Environ Med. 2006;48:591–8. doi: 10.1097/01.jom.0000201567.70084.3a. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen ML, Rugulies R, Smith-Hansen L, et al. Psychosocial work environment and registered absence from work: estimating the etiologic fraction. Am J Ind Med. 2006;49:187–96. doi: 10.1002/ajim.20252. [DOI] [PubMed] [Google Scholar]
- 14.Head J, Kivimäki M, Martikainen P, et al. Influence of change in psychosocial work characteristics on sickness absence: The Whitehall II Study. J Epidemiol Commun Health. 2006;60:55–61. doi: 10.1136/jech.2005.038752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suominen S, Vahtera J, Korkeila K, et al. Job strain, life events, and sickness absence: a longitudinal cohort study in a random population sample. Occup Environ Med. 2007;49:990–6. doi: 10.1097/JOM.0b013e3181343e2b. [DOI] [PubMed] [Google Scholar]
- 16.Holmgren K, Dahlin-Ivanoff S, Björkelund C, et al. The prevalence of work-related stress, and its association with self-perceived health and sick-leave, in a population of employed Swedish women. BMC Public Health. 2009;9:73. doi: 10.1186/1471-2458-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thoits PA. Multiple identities and psychological well-being: a reformulation and test of the social isolation hypothesis. Am Sociol Rev. 1983;48:174–87. [PubMed] [Google Scholar]
- 18.Frone MR. Work-family conflict and employee psychiatric disorders: the National Comorbidity Survey. J Appl Psychol. 2000;85:888–95. doi: 10.1037/0021-9010.85.6.888. [DOI] [PubMed] [Google Scholar]
- 19.Grzywacz J, Marks NF. Reconceptualizing the work-family interface: an ecological perspective on the correlates of positive and negative spillover between work and family. J Occup Health Psychol. 2000;5:111–26. doi: 10.1037//1076-8998.5.1.111. [DOI] [PubMed] [Google Scholar]
- 20.Väänänen A, Kevin MV, Ala-Mursula L, et al. The double burden of and negative spillover between paid and domestic work: associations with health among men and women. Women Health. 2004;40:1–18. doi: 10.1300/j013v40n03_01. [DOI] [PubMed] [Google Scholar]
- 21.Emslie C, Hunt K, Macintyre S. Gender, work-home conflict, and morbidity amongst white-collar bank employees in the United Kingdom. Int J Behav Med. 2004;11:127–34. doi: 10.1207/s15327558ijbm1103_1. [DOI] [PubMed] [Google Scholar]
- 22.Ala-Mursula L, Vahtera J, Kouvonen A, et al. Long hours in paid and domestic work and subsequent sickness absence: does control over daily working hours matter? Occup Environ Med. 2006;63:608–16. doi: 10.1136/oem.2005.023937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandmark H. Work and family: associations with long-term sick-listing in Swedish women - a case-control study. BMC Public Health. 2007;7:287. doi: 10.1186/1471-2458-7-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Väänänen A, Kumpulainen R, Kevin MV, et al. Work-family characteristics as determinants of sickness absence: a large-scale cohort study of three occupational grades. J Occup Health Psychol. 2008;13:181–96. doi: 10.1037/1076-8998.13.2.181. [DOI] [PubMed] [Google Scholar]
- 25.Åkerlind I, Alexanderson K, Hensing G, et al. Sex differences in sickness absence in relation to parental status. Scand J Soc Med. 1996;24:27–35. doi: 10.1177/140349489602400105. [DOI] [PubMed] [Google Scholar]
- 26.Bratberg E, Dahl SA, Risa AE. “The double burden” – Do combinations of career and family obligations increase sickness absence among women? Eur Sociol Rev. 2002;18:233–49. [Google Scholar]
- 27.Bekker M, Croon M, Bressers B. Childcare involvement, job characteristics, gender and work attitudes as predictors of emotional exhaustion and sickness absence. Work Stress. 2005;19:221–37. [Google Scholar]
- 28.Jansen NW, Kant IJ, van Amelsvoort LG, et al. Work-family conflict as a risk factor for sickness absence. Occup Environ Med. 2006;63:488–94. doi: 10.1136/oem.2005.024943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mastekaasa A. Parenthood, gender and sickness absence. Soc Sci Med. 2000;50:1827–42. doi: 10.1016/s0277-9536(99)00420-7. [DOI] [PubMed] [Google Scholar]
- 30.Blank N, Diderichsen F. Short-term and long-term sick-leave in Sweden: relationships with social circumstances, working conditions and gender. Scand J Soc Med. 1995;23:265–72. doi: 10.1177/140349489502300408. [DOI] [PubMed] [Google Scholar]
- 31.Voss M, Josephson M, Stark S, et al. The influence of household work and of having children on sickness absence among publicly employed women in Sweden. Scand J Public Health. 2008;36:564–72. doi: 10.1177/1403494807088459. [DOI] [PubMed] [Google Scholar]
- 32.Floderus B, Hagman M, Aronsson G, et al. Self-reported health in mothers: the impact of age, and socioeconomic conditions. Women Health. 2008;47:63–86. doi: 10.1080/03630240802092308. [DOI] [PubMed] [Google Scholar]
- 33.Floderus B, Hagman M, Aronsson G, et al. Work status, work hours and health in women with and without children. Occup Environ Med. 2009;66:704–10. doi: 10.1136/oem.2008.044883. [DOI] [PubMed] [Google Scholar]
- 34.Hertzmark E, Spiegelman D. The SAS MPHREG macro. Boston, MA: Channing Laboratory; 2001. [Google Scholar]
- 35.Wise LA, Palmer JR, Harlow B, et al. Reproductive factors, hormonal contraception, and risk of uterine leiomyomata in African-American women: A prospective study. Am J Epidemiol. 2004;159:113–123. doi: 10.1093/aje/kwh016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boyton-Jarrett R, Rich-Edwards J, Malspeis S, et al. A prospective study of hypertension and risk of uterine leiomyomata. Am J Epidemiol. 2005;161:628–638. doi: 10.1093/aje/kwi072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Commun Health. 2000;54:502–9. doi: 10.1136/jech.54.7.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aronsson G, Gustafsson K. Sickness presenteeism: prevalence, attendance-pressure factors, and an outline of a model for research. J Occup Environ Health. 2005;47:958–966. doi: 10.1097/01.jom.0000177219.75677.17. [DOI] [PubMed] [Google Scholar]
- 39.Voss M, Floderus B, Diderichsen F. Changes in sickness absenteeism following the introduction of a qualifying day for sickness benefit–findings from Sweden Post. Scand J Public Health. 2001;29:166–74. [PubMed] [Google Scholar]