Abstract
Background: The aim of this study is to assess the impact of combined work and family demands on all-cause sickness absence and to examine variation in this relationship by occupational grade and gender. Methods: The study sample consists of 13 179 employees of Electricité de France-Gaz de France (EDF-GDF) who were members of the GAZEL occupational cohort in 1995. Combined work and family demands are assessed based on measures of job strain and number of dependants assessed at baseline (1995). Covariates include occupational grade and demographic, behavioural and social variables assessed at baseline. Ratios of sickness absence days to total person-days contributed by each employee were established from administrative data between baseline and the end of follow-up in 2003. Rate ratios across levels of work–family demands were then calculated. Effect modification by gender and grade of employment was tested. Results: In fully adjusted models, individuals with the highest work–family demands had a rate ratio of sickness absence of 1.78 (95% CI 1.47–2.14) compared with low-demand workers. This association was independent of occupational grade and did not vary with gender. Results were not attributable solely to psychiatric sickness absences. Conclusion: High work–family demands at baseline predict long-term all-cause sickness absence across a socio-economically diverse occupational cohort.
Introduction
Absenteeism from work carries social and financial costs for employees and employers. Although rates of sickness absence vary depending on legal context, economic situation and labour force characteristics, evidence from several countries indicates that sickness absence is a good indicator of health status.1–4 While the impact of physical and psychosocial workplace hazards on sickness absence is well-documented,5,6 impacts of social factors involving combined work and non-work domains are less understood. Understanding these factors can help inform psychosocial workplace interventions.
In this study, we assess whether family-related demands add to known health impacts of job strain. High job strain—concurrent high psychological demands (i.e. workload) and low decision latitude (i.e. job control)7—is a well-studied risk factor for poor health.8 Much research has focused on long-term physical health effects of job strain,9 though recent research looks at more proximal health indicators.10,11 Occupational grade is highly predictive of job strain, as it occurs disproportionately among low-wage workers, who are also most prone to sickness absence.8 Effects of job strain may also differ by gender; women’s and men’s different responsibilities and roles outside of work may affect their experiences of work stress, including the ‘second shift’ burden in which working women also face a full load of domestic responsibilities.12 Thus, combined demands and strains of work and home life may be gender-variant. Research on role strain suggests that men are negatively affected by work-to-family conflict, while women are especially susceptible to family-to-work conflict.13,14 However, this differential relationship has not been fully explored in terms of its health effects.
Conflicting demands from work and home augment the demand–control model.15,16 These demands are often operationalised as work–family conflict, the inter-role conflict that arises when work and home demands are incompatible.17 Work–family conflict is associated with greater risk of occupational injury,18 alcohol abuse, reduced physical activity, obesity,19 high cholesterol and elevated blood pressure.20 In addition to physical health effects, work–family conflict has shown consistent associations with poor mental health, particularly depression, anxiety and general distress.21 All these characteristics increase risk of sickness absence.
At least two studies have examined relationships between work–family conflict and absenteeism.22.23 These studies found that work–family conflict predicted sickness absence, especially for women and lower grade workers. Additionally, a prior GAZEL study showed that high work–family demands predict psychiatric sickness absence, particularly depression related.24 However, that study did not examine the role of work–family demands in all-cause sickness absence, leaving a gap in understanding of the impact of psychosocial exposures on individuals’ overall health. Thus, we hypothesized that sickness absence would be most frequent among workers with high work–family demands, compared with those with lesser demands. Furthermore, we hypothesized that the relationship would be strongest for women and those in low occupational grades.
Methods
Study population
GAZEL is an occupational cohort of 15 010 men and 5614 women who were employed by the French gas and electricity company Electricité de France-Gaz de France (EDF-GDF) in 1989. At this time, all male employees between ages 40 and 50 years and all female employees between ages 35 and 50 years were invited to participate in a longitudinal follow-up (the age range for women is wider because women comprise only 20% of EDF-GDF employees). Participants complete annual self-report questionnaires, and EDF-GDF simultaneously report administrative data on cohort members’ occupational status, health status and absenteeism. Annually, approximately 75% of participants return the surveys and less than 1% have been lost to follow-up.25 Of the original cohort (n = 20 624), 13 179 were working in 1995 (not retired, lost to follow-up or deceased) and responded to the self-report survey that year, when self-reports of job strain were collected.
Measures
Exposure: work and family demands
Work demands were measured in 1995 using a French version of the Karasek Job Content Questionnaire.26 Three dimensions of work stress were measured: decision latitude (six items), psychological demands (five items) and social support from colleagues (five items). In each dimension, individuals with scores above the median were classified as exposed. We then summed the number of exposures to create an index of work stress (range: 0–3). Workers in the highest category had high psychological demands, low decision latitude and low workplace social support. Family demands were measured using number of dependants (0, 1–3, ≥4), reported by participants to EDF-GDF in 1995; EDF-GDF collects this information to calculate employees’ benefits. Dependants were defined as individuals without income whom the participant supports.
We used an established rubric (See Supplementary Figure 1) to estimate individuals’ combined work and family demands.24 Individuals with no dependants were classified as one group regardless of work stress, based on evidence in GAZEL that such individuals have higher rates of sickness absence than those with dependants.27 Those with three work stressors and four or more dependants were classified as having high work–family demands, whereas the lowest demand workers had 0–1 job stressors and 1–3 dependants. Individuals with either many work stressors but few dependants, or many dependants but few work stressors, were classified in the moderate demand group. See online version for full details of scoring rubric (Supplementary data).
Outcome: sickness absence
At EDF-GDF, all sickness absences from work (from first day of absence) must be physician certified and diagnosis verified. This procedure is occasionally omitted for short absence spells (<15 days), when company physicians do not have sufficient time to conduct the verification procedures. Company physicians established sickness absence diagnoses, based on ICD-9 and ICD-10 codes. We analysed rates of all-cause sickness absence days reported during 1995–03, based on EDF-GDFs total recorded number of days of sickness absence per employee, divided by the number of days the individual was employed during follow-up. Individuals who died, retired or were lost to follow-up were censored at death, retirement or last contact. We measured absence in total number of days, based on the evidence that number of days (as well as the more commonly used measure of absence spells) strongly predicts illness severity and disease burden.28,29 Number of absence days is also a more relevant metric than number of spells from an organizational perspective. Distribution of sickness absence has a strong right skew, with no evidence of bimodality or other deviance from Poisson distribution.
Covariates
We considered demographic, behavioural and personal characteristics thought to influence sickness absence: age (41–45, 46–50 or 51–56 years for women; 46–50 or 51–56 years for men); marital status (married/cohabitating, single, divorced/widowed/separated); current smoker (yes/no); alcohol consumption in number of alcoholic drinks per week (women: 0, 1–6, 7–20, ≥21; men: 0, 1–14, 15–27, ≥28); BMI (kg/m2; <20, 21–24.9, 25–29.9, ≥30); and social ties measured by Berkman’s Questionnaire on Social Networks and Social Support30 (sufficient/insufficient). Occupational grade was a three-level variable: high (executives/engineers), intermediate (administrative associate professionals/technicians) or low (manual workers/clerks). All baseline covariates were collected in 1995, except social ties, collected in 1994.
Statistical analyses
Our analysis was based on the 13 179 GAZEL cohort participants working in 1995. We calculated rate ratios of sickness absence by level of work–family demands, using the lowest demands group as the reference. We used log-linear Poisson regression, correcting over-dispersion by adjusting standard errors by a scale parameter equivalent to residual deviance divided by number of degrees of freedom. We controlled for occupational grade (a strong risk factor for sickness absence) in all models.31 Successive models were built as follows: (i) controlling for demographic factors; (ii) plus health behaviours; (iii) plus social support. We tested for statistical interactions between each level of work–family demands and low occupational grade. We also tested for interaction between gender and work–family demands.
We conducted several analyses to test the robustness of our associations. First, we analysed sickness absence from all causes except psychiatric illness (a large contributor to total sickness absence in this cohort, comprising 23% of total days taken during the follow-up). Since our exposure (work–family demands) was only available at baseline, we conducted two time-period analyses: the first half of the observation period (1995–98) and the second half (1999–2003) to determine whether associations differed with increased time since exposure assessment. We analysed absences in several diagnostic categories to help understand patterns observed in all-cause sickness absence.
All regressions were performed in SAS 9.1.
Results
The study population included 13 179 individuals employed in 1995 (9597 men and 3582 women). Table 1 shows characteristics of men and women separately, as well as bivariate relationships with sickness absence.
Table 1.
Characteristics of GAZEL cohort participants, 1995 (n = 13 179)
| Variable | Men (n = 9597) |
Women (n = 3582) |
||
|---|---|---|---|---|
| n (%) | Mean (SE) annual days sickness absence (P for inter-group difference) | n (%) | Mean (SE) annual days sickness absence (P for inter-group difference) | |
| Work and family demands | ||||
| No dependants | 502 (5.3) | 14.5 (1.9)*** | 394 (11.2) | 20.8 (2.4)** |
| Low demands | 4581 (48.2) | 9.9 (0.5) | 1436 (40.7) | 19.3 (1.1) |
| Moderate demands | 3735 (39.3) | 11.8 (0.6) | 1499 (42.4) | 21.6 (1.2) |
| High demands | 681 (7.2) | 16.3 (1.8) | 204 (5.8) | 34.4 (4.6) |
| Age (years) | ||||
| 42–45 | – | – | 1550 (43.3) | 20.4 (1.2)* |
| 45–50 | 4258 (44.4) | 15.0 (0.7)*** | 877 (24.5) | 23.6 (1.3) |
| 51–55 | 5339 (55.6) | 8.5 (0.4) | 1155 (32.2) | 18.8 (2.8) |
| Marital status | ||||
| Married/cohabitating | 8864 (92.5) | 11.0 (0.4)*** | 2686 (75.0) | 19.5 (0.8)*** |
| Single | 196 (2.0) | 20.4 (4.1) | 240 (6.7) | 19.4 (3.0) |
| Divorced/widow/separated | 527 (5.50) | 15.7 (1.9) | 654 (18.3) | 29.4 (2.2) |
| Occupational grade | ||||
| High | 3843 (40.0) | 6.6 (0.4)*** | 431 (12.0) | 9.9 (1.4)*** |
| Intermediate | 4739 (49.4) | 12.8 (0.5) | 2457 (68.6) | 20.1 (0.9) |
| Low | 1015 (10.6) | 23.5 (1.8) | 694 (19.4) | 27.6 (2.1) |
| Current smoker | ||||
| No | 7605 (79.3) | 10.5 (0.4)*** | 3012 (84.1) | 20.1 (0.9)*** |
| Yes | 1992 (20.8) | 15.0 (1.0) | 570 (15.9) | 27.5 (2.1) |
| Alcohol consumption | ||||
| None | 753 (8.8) | 22.1 (2.2)*** | 824 (27.22) | 25.6 (1.8)** |
| Light drinker | 4518 (53.0) | 10.9 (0.5) | 1488 (49.16) | 20.3 (1.1) |
| Moderate drinker | 1992 (23.4) | 9.9 (0.8) | 600 (19.82) | 18.9 (1.7) |
| Heavy drinker | 1265 (14.8) | 9.9 (0.8) | 115 (3.80) | 16.6 (3.9) |
| Body weight | ||||
| Underweight (BMI < 20 kg/m2) | 118 (1.5) | 19.3 (6.0)*** | 449 (14.0) | 22.2 (2.4)** |
| Normal (BMI 20–24.9 kg/m2) | 3498 (40.3) | 10.0 (0.6) | 2001 (62.7) | 19.5 (1.0) |
| Overweight (BMI 25–29.9 kg/m2) | 4341 (50.0) | 10.4 (0.5) | 561 (17.6) | 22.0 (1.9) |
| Obese (BMI ≥ 30 kg/m2) | 732 (8.4) | 14.6 (1.6) | 180 (5.6) | 31.2 (4.2) |
| Number work stress factors | ||||
| 0 | 2430 (25.6) | 9.3 (0.7)*** | 505 (14.3) | 17.3 (1.8)** |
| 1 | 4122 (43.4) | 10.2 (0.5) | 1347 (38.2) | 19.3 (1.2) |
| 2 | 2396 (25.2) | 13.4 (0.8) | 1256 (35.6) | 23.5 (1.4) |
| 3 | 546 (5.8) | 20.2 (2.4) | 421 (11.9) | 25.3 (2.1) |
| Number of dependants | ||||
| 0 | 502 (5.2) | 14.5 (1.9)** | 394 (11.0) | 20.9 (2.4) |
| 1 | 1306 (13.6) | 13.9 (1.2) | 723 (20.2) | 21.3 (1.7) |
| 2 | 3197 (33.3) | 11.4 (0.6) | 1449 (40.4) | 21.5 (1.9) |
| 3 | 2238 (23.3) | 9.4 (0.6) | 601 (16.8) | 20.0 (1.7) |
| ≥4 | 2354 (24.5) | 11.4 (0.8) | 415 (11.9) | 23.7 (2.6) |
| Personal social support | ||||
| Sufficient | 6118 (65.2) | 9.9 (0.4)*** | 1598 (45.9) | 20.2 (1.1) |
| Insufficient | 3270 (34.8) | 13.9 (0.8) | 1883 (54.1) | 22.0 (1.1) |
*P for inter-group difference in absence days <0.05, **P < 0.01, ***P < 0.001
Our primary exposure of interest—work and family demands—showed significant bivariate association with sickness absence, with a difference in annual absence days of 6.4 for men and 13.6 for women, comparing highest demand workers with lowest demand. Women had more sickness absence than men, on average, so we gender-stratified descriptive and bivariate analyses. Occupational grade, as previously demonstrated in GAZEL, has a gradient association with sickness absence across genders.
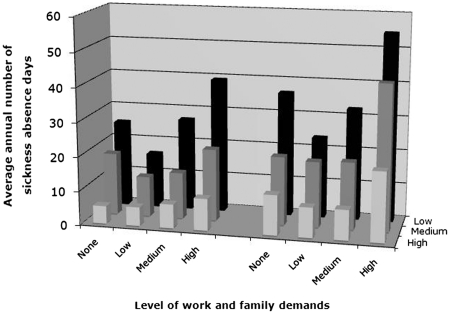
Figure 1 shows average number of sickness absence days per year by gender, occupational grade and work–family demands. We observed the lowest number of absence days among those with few dependants and low job demands, and progressively higher rates for those with greater work–family demands. We observed an occupational grade gradient within each level of work–family demands, with workers in lower status jobs experiencing more sickness absence than the highest-level workers. Men and women had significantly different numbers of sickness absence days per year as observed in figure 1. However, the primary exposure–outcome relationship was not statistically modified by gender, so men and women were combined for regression analyses.
Figure 1.
Days of sickness absence by gender, level of work–family demands and occupational grade in the GAZEL cohort (1995–2003)
In regression models (table 2) adjusted for demographic factors, we found higher levels of sickness absence among those with moderate (RR 1.17, 95% CI 1.07–1.29) and high (RR 1.86, 95% CI 1.60–2.17) work–family demands compared with those with low work–family demands. In fully adjusted models, we found higher rates of sickness absence among those with moderate work–family demands (RR 1.15, 95% CI 1.02–1.29) and high work–family demands (RR 1.78, 95% CI 1.47–2.14), though the relationship among those without dependants became statistically non-significant (RR 1.05 95% CI 0.85–1.30). Although work–family demands were statistically significantly modified by occupational grade, the impact of this modification on main-effect rate ratios was negligible and so those results are not reported.
Table 2.
Associations between work–family demands and all-cause sickness absence (1995–2003) in the GAZEL cohort study (n = 13 179) (RR, 95% CI)
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Work and family demands | |||
| No dependants | 1.20 (0.99–1.45) | 1.12 (0.90–1.40) | 1.06 (0.84–1.32) |
| Low | 1.0 | 1.0 | 1.0 |
| Moderate | 1.17 (1.07–1.29) | 1.20 (1.08–1.33) | 1.15 (1.02–1.29) |
| High | 1.86 (1.60–2.17) | 1.91 (1.61–2.27) | 1.78 (1.47–2.14) |
| Age (years) | |||
| 42–45 | 1.0 | 1.0 | 1.0 |
| 45–50 | 0.94 (0.83–1.08) | 0.95 (0.82–1.10) | 0.95 (0.82–1.10) |
| 51–55 | 0.84 (0.76–0.92) | 0.82 (0.73–0.91) | 0.83 (0.74–0.92) |
| Marital status | |||
| Married/cohabitating | 1.0 | 1.0 | 1.0 |
| Single | 1.17 (0.92–1.48) | 1.18 (0.90–1.54) | 1.13 (0.86–1.48) |
| Divorced/widow/separated | 1.32 (1.17–1.48) | 1.26 (1.10–1.45) | 1.26 (1.10–1.45) |
| Occupational grade | |||
| High | 1.0 | 1.0 | 1.0 |
| Intermediate | 2.19 (1.93–2.48) | 2.10 (1.83–2.40) | 2.08 (1.81–2.38) |
| Low | 3.49 (3.02–4.02) | 3.23 (2.76–3.78) | 3.18 (2.72–3.73) |
| Sex | |||
| Male | 1.0 | 1.0 | 1.0 |
| Female | 1.37 (1.23–1.52) | 1.39 (1.22–1.60) | 1.37 (1.20–1.56) |
| Current smoker | |||
| No | 1.0 | 1.0 | |
| Yes | 1.37 (1.22–1.53) | 1.35 (1.21–1.51) | |
| Alcohol consumption | |||
| None | 1.40 (1.24–1.57) | 1.40 (1.24–1.58) | |
| Light drinker | 1.0 | 1.0 | |
| Moderate drinker | 0.90 (0.79–1.02) | 0.91 (0.80–1.03) | |
| Heavy drinker | 0.83 (0.69–1.00) | 0.83 (0.69–1.00) | |
| Body weight | |||
| Underweight (BMI < 20 kg/m2) | 1.15 (0.96–1.37) | 1.14 (0.95–1.37) | |
| Normal (BMI 20–24.9 kg/m2) | 1.0 | 1.0 | |
| Overweight (BMI 25–29.9 kg/m2) | 1.12 (1.01–1.25) | 1.12 (1.00–1.25) | |
| Obese (BMI ≥ 30 kg/m2) | 1.49 (1.26–1.76) | 1.51 (1.28–1.78) | |
| Personal social support | |||
| Sufficient | 1.0 | ||
| Insufficient | 1.10 (0.98–1.23) |
Given high sickness absence burden contributed by psychiatric illness (23% of total absence days), we conducted analyses restricting our outcome to physical illness. In these fully adjusted models, rate ratios were 1.10 (95% CI 0.97–1.24) and 1.40 (95% CI 1.13–1.73) for moderate and high work–family demands, respectively.
To understand potential mechanisms behind observed associations, we conducted analyses by cause-specific absence. In fully adjusted models, for the workers with the highest demands compared with the lowest demand workers, rate ratios for sickness absences were 0.88 (95% CI 0.37–2.08) for cancer absences, 1.59 (95% CI 1.23–2.07) for gastrointestinal absences, 1.59 (95% CI 1.20–1.93) for circulatory absences, 1.52 (95% CI 1.20–1.93) for occupational injury-related absences and 1.34 (1.08–1.66) for orthopaedic absences.
We had operationalised work–family demands as a time-invariant construct, so we tested whether the relationship between demands and sickness absence remained constant over time. We found the relationship slightly attenuated over the follow-up period but remained statistically significant (for high-demand vs. low-demand workers, fully adjusted RR = 1.84, 95% CI 1.49–2.25 in 1995–98, vs. RR = 1.67, 95% CI 1.30–2.16 in 1999–2003) (data not shown).
Finally, we evaluated the validity of our work–family demands measure. We examined social support across levels of work–family demands and found that 19.5% of high-demand workers reported sufficient social support, compared with 83.2% of low-demand workers. However, social support was not significantly associated with sickness absence in regression models, so it was not retained. Second, our measure of work–family demands had divergent validity with respect to occupational grade, suggesting that the two measures represent distinct constructs. Third, we found low correlation between each level of work demands and each level of family demands (r = 0.01–0.05), indicating that domains of work demands and family demands are statistically non-overlapping.
Discussion
Findings
The present study finds elevated rates of all-cause sickness absence among workers with high concurrent demands from work and home, with workers in the highest exposure group experiencing rates of sickness absence 79% higher than those with low work and family demands. This association is significant when psychiatric absences are removed. With the exception of gender and occupational-grade interactions, our initial hypotheses were supported.
This study builds on literature documenting negative health effects of high work and family demands. Two prior studies showed associations between work–family conflict and sickness absence, with heterogeneity by occupational grade and gender.22,23 However, these studies were either cross-sectional or had short follow-up times, potentially biasing away from the null if less healthy (and thus frequently absent) employees incurred or perceived higher demands at work and at home. This is especially plausible among those with mental health problems such as depression. Our results held in analyses of non-psychiatric sickness absences, suggesting that differential reporting of work–family demands by mental health status does not account for our findings.
In contrast to previous research, our sample is an established cohort of employees at a single company, rather than a random population sample. This inherently controls for factors such as sickness absence policies and physician consistency in sick leave verification. Given high job security, long average tenure and universal pension plans at EDF-GDF, we would not likely see differential study attrition based on work and family demands. Although conducting the study in a single company may reduce external validity, our strong control for selection and attrition address two threats to internal validity of previous studies. In sum, the study strengthens evidence on negative health effects of work and family demands on workers, especially those in lower status jobs.
We explored several possible explanations for our findings, performing fully adjusted analyses of cause-specific absences (table 3). Of the five categories we analysed, only cancer absences did not show a gradient by work and family demands (RR 0.88, 95% CI 0.37–2.08). Other categories of absences were significantly elevated among those with the highest work–family demands. These categories can be divided into systemic illnesses (circulatory and gastrointestinal disease) vs. work-related accidents and orthopaedic problems. Both classes of absences have plausible mechanisms that could help explain our study findings. Several studies show cross-sectional associations between occupational stressors (including work–family conflict) and physical strain.18,32 This relationship may arise either from employee preoccupation with home duties while at work, or from rushing at work with less attention to safety. Similarly, work–family demands may affect both gastrointestinal and circulatory (including cardiovascular) illness and absence via stress pathways impacting cardiometabolic factors related to blood pressure, metabolic regulation and immune responses.20,33
Table 3.
Fully adjusteda associations between work–family demands and non-psychiatric/cause-specific sickness absence (1995–2003) in the GAZEL cohort study, RR (95% CI)
| Variable | Non-psychiatric absence days | Cancer absence spells | Gastro-intestinal spells | Circulatory spells | Work-related accident spells | Orthopaedic spells |
|---|---|---|---|---|---|---|
| Work and family demands | ||||||
| No dependants | 1.04 (0.83–1.32) | 0.68 (0.29–1.63) | 0.91 (0.66–1.25) | 0.94 (0.63–1.41) | 1.02 (0.77–1.35) | 1.13 (1.11–1.34) |
| Low | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Moderate | 1.10 (0.97–1.25) | 0.66 (0.42–1.06) | 1.09 (0.92–1.27) | 1.23 (1.01–1.48) | 1.10 (0.95–1.27) | 1.11 (0.99–1.26) |
| High | 1.39 (1.3–1.73) | 0.88 (0.37–2.08) | 1.59 (1.23–2.07) | 1.59 (1.15–2.19) | 1.52 (1.20–1.93) | 1.34 (1.08–1.66) |
| Occupational grade | ||||||
| High | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Intermediate | 2.04 (1.78–2.35) | 1.26 (0.80–2.44) | 1.86 (1.57–2.22) | 1.73 (1.41–2.12) | 2.29 (1.95–2.69) | 2.42 (2.08–2.81) |
| Low | 2.85 (2.41–3.37) | 1.30 (0.69–2.44) | 2.56 (2.07–3.16) | 2.38 (1.84–3.06) | 3.14 (2.39–3.81) | 4.42 (3.73–5.23) |
a: Adjusted for occupational grade, sex, age, marital status, smoking, body weight and alcohol consumption
Although the interaction between gender and work–family demands was non-significant in the present analysis, given strong evidence in prior studies of gender differences in work–family conflict,13,14 we further investigated this null finding. We tested the hypothesis that work–family demands may exert similar effects on sickness absence for men and women but for different reasons (and thus our combined measure was potentially masking these differential effects) by comparing genders on the components of our composite measure. In unadjusted models, men with the most job stress (vs. the least stress) had rate ratios for sickness absence of 2.19 (95% CI 1.76–2.73); in women the corresponding rate ratio was 1.51 (95% CI 1.16–1.96). Conversely, men with the highest number of dependants (vs. the lowest) had rate ratios for sickness absence of 1.27 (95% CI 1.11–1.47); in women the corresponding rate ratio was 1.57 (95% CI 1.29–1.93). Thus, work factors may be more predictive of sickness absence for men, while family-related demands may be more salient for women. Of note, this pattern may have occurred because the Karasek model is generally a better predictor of health outcomes in men.34 Our results point to a need for work–family interventions that can be tailored to meet heterogeneous needs of working populations.
Limitations
The current study has several limitations. Most notably, we used a simple index of work and family demands by summing number of work stressors and number of dependants. We were unable to directly assess work/family conflict or spillover, but found that the measure had both construct and divergent validity.
We could only obtain information about work–family demands at study baseline, so we could not test how varying levels of work–family demands and health change over time. Separate analyses for the latter and former halves of follow-up yielded similar results as the overall model. We cannot, however, assess whether this reflects stable levels of work–family demands or long-lasting effects of exposure to high levels of stress; this should be examined in future research.
Finally, our measure does not require respondents to evaluate quality of joint work and family demands, so we may have missed ‘positive spillover’, or beneficial aspects of joint demands.35 However, such effects would bias towards the null.
Although our study included many participants, most were exposed to low or moderate work–family demands. Future research should focus on populations with greater work and family stressors. Recent research in long-term care suggests that risks are particularly high for low-wage female workers with high work–family demands, young children and little job flexibility.36
Implications
This study was conducted among French employees with high job security, stable income and benefits, as well as multiple state-administered programmes and laws to protect workers’ health. If work–family demands predict sickness absence in this particular population, the effect is likely stronger in settings with fewer resources to help workers balance work and non-work obligations.37
In addition to the public health burden of poor health as represented by sickness absence, high absenteeism is a source of business-related consequences such as higher turnover and reduced productivity. Our results suggest that negative health and business outcomes could be jointly mitigated by creating more family friendly workplaces, which would improve workers’ abilities to balance work and family life. While interventions to reduce work–family demands are challenging, addressing root causes of sickness absence holds clear benefit for both employees and organizations.
Supplementary data
Supplementary data are available at Eurpub online.
Funding
The GAZEL Cohort Study was funded by EDF-GDF and the French National Institute of Health and Medical Research (INSERM), and received grants from the ‘Cohortes Santé TGIR Program’, Agence nationale de la recherché (ANR) and Agence française de sécurité sanitaire de l’environnement et du travail (AFSSET).’ M.M. is the recipient of a Young Researcher Award from the ANR. The authors would also like to express their thanks to the Work, Family and Health Network (NIA 5U01AG027669-05).
Conflicts of interest: None declared.
Key points.
Combined work and family demands predict all-cause sickness absence in a socio-economically diverse occupational cohort.
The effect of work and family demands on sickness absence is driven by physical, as well as psychiatric, illness.
Although the effect of work–family demands on sickness absence is similar for men and women, work demands are more strongly predictive of absence for men and family demands are more predictive of absence for women.
Organizations may be able to reduce absenteeism by helping mitigate job strain for workers with high family demands.
Supplementary Material
Acknowledgements
The authors express their thanks to EDF-GDF, especially to the Service Général de Médecine de Contrôle, and to the ‘Caisse centrale d’action sociale du personnel des industries électrique et gazière’. The authors also wish to acknowledge the Cohortes team of the Unité 1018 INSERM responsible for the GAZEL data base management. Preliminary results of this analysis were presented at the American Public Health Association National Meeting, Philadelphia, PA USA, November 2009.
References
- 1.Kivimäki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ. 2003;327:364. doi: 10.1136/bmj.327.7411.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kivimaki M, Head J, Ferrie JE, et al. Sickness absence as a prognostic marker for common chronic conditions: analysis of mortality in the GAZEL study. Occup Environ Med. 2008;65:820–6. doi: 10.1136/oem.2007.038398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Virtanen P, Siukola A, Luukkaala T, et al. Sick leaves in four factories: do characteristics of employees and work conditions explain differences in sickness absence between workplaces? Scand J Work, Environ Health. 2008;34:260–6. doi: 10.5271/sjweh.1225. [DOI] [PubMed] [Google Scholar]
- 4.Melchior M, Ferrie JE, Alexanderson K, et al. Does Sickness Absence Due to Psychiatric Disorder Predict Cause-specific Mortality? A 16-Year Follow-up of the GAZEL Occupational Cohort Study. Am J Epidemiol. 2010;172:700–7. doi: 10.1093/aje/kwq186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voss M, Floderus B, Diderichsen F. Physical, psychosocial, and organisational factors relative to sickness absence: a study based on Sweden Post. Occup Environ Med. 2001;58:178–84. doi: 10.1136/oem.58.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexanderson K. Sickness absence: a review of performed studies with focused on levels of exposures and theories utilized. Scand J Public Health. 1998;26:241–9. doi: 10.1177/14034948980260040301. [DOI] [PubMed] [Google Scholar]
- 7.Karasek R, Brisson C, Kawakami N, et al. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 8.Melchior M, Krieger N, Kawachi I, et al. Work factors and occupational class disparities in sickness absence: findings from the GAZEL cohort study. Am J Public Health. 2005;95:1206–12. doi: 10.2105/AJPH.2004.048835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kristensen TS. Job stress and cardiovascular disease: A theoretic critical review. J Occup Health Psychol. 1996;1:246–60. doi: 10.1037//1076-8998.1.3.246. [DOI] [PubMed] [Google Scholar]
- 10.Lerner DJ, Levine S, Malspeis S, D’Agostino RB. Job Strain and Health-Related Quality of Life in a National Sample. Am J Public Health. 1994;84:1580–5. doi: 10.2105/ajph.84.10.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Head J, Kivimaki M, Martikainen P, et al. Influence of change in psychosocial work characteristics on sickness absence: the Whitehall II study. J Epidemiol Community Health. 2006;60:55–61. doi: 10.1136/jech.2005.038752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochschild A, Machung A. The Second Shift: Working Parents and the Revolution at Home. New York: Viking; 1989. [Google Scholar]
- 13.Duxbury LE, Higgins CA. Gender differences in work-family conflict. J Applied Psychol. 1991;76:60–73. [Google Scholar]
- 14.Cinamon RG, Rich Y. Gender Differences in the Importance of Work and Family Roles: Implications for Work–Family Conflict. Sex Roles. 2002;47:531–41. [Google Scholar]
- 15.Frone MR, Russell M, Cooper ML. Antecedents and outcomes of work-family conflict: Testing a model of the work-family interface. J Appl Psychol. 1992;77:65–78. doi: 10.1037/0021-9010.77.1.65. [DOI] [PubMed] [Google Scholar]
- 16.Kelly EL, Kossek EE, Hammer LB, et al. Chapter 7: Getting There from Here: Research on the Effects of Work/Family Initiatives on Work/Family Conflict and Business Outcomes. Acad Manag Ann. 2008;2:305–49. doi: 10.1080/19416520802211610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenhaus JH, Beutell NJ. Sources of Conflict between Work and Family Roles. Acad Manag Rev. 1985;10:76–88. [Google Scholar]
- 18.Cullen JC, Hammer LB. Developing and testing a theoretical model linking work-family conflict to employee safety. J Occup Health Psychol. 2007;12:266–78. doi: 10.1037/1076-8998.12.3.266. [DOI] [PubMed] [Google Scholar]
- 19.Roos E, Lahelma E, Rahkonen O. Work-family conflicts and drinking behaviours among employed women and men. Drug Alcohol Depend. 2006;83:49–56. doi: 10.1016/j.drugalcdep.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Frone M, Russel M, Cooper ML. Relation of work-family conflict to health outcomes: A four-year longitudinal study of employed parents. J Occup Organ Psychol. 1997;70:325–35. [Google Scholar]
- 21.Frone MR. Work-family conflict and employee psychiatric disorders: The national comorbidity survey. J Appl Psychol. 2000;85:888–95. doi: 10.1037/0021-9010.85.6.888. [DOI] [PubMed] [Google Scholar]
- 22.Jansen NWH, Kant IJ, van Amelsvoort LGPM, et al. Work-family conflict as a risk factor for sickness absence. Occup Environ Med. 2006;63:488–94. doi: 10.1136/oem.2005.024943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Väänänen A, Kumpulainen R, Kevin MV, et al. Work-family characteristics as determinants of sickness absence: A large-scale cohort study of three occupational grades. J Occup Health Psychol. 2008;13:181–96. doi: 10.1037/1076-8998.13.2.181. [DOI] [PubMed] [Google Scholar]
- 24.Melchior M, Berkman LF, Niedhammer I, et al. The mental health effects of multiple work and family demands. A prospective study of psychiatric sickness absence in the French GAZEL study. Soc Psychiatry Psychiatr Epidemiol. 2007;42:573–82. doi: 10.1007/s00127-007-0203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberg M, Leclerc A, Bonenfant S, et al. Cohort profile: the GAZEL Cohort Study. Int J Epidemiol. 2007;36:32–9. doi: 10.1093/ije/dyl247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York: Basic Books; 1990. [Google Scholar]
- 27.Melchior M, Niedhammer I, Berkman LF, Goldberg M. Do psychosocial work factors and social relations exert independant effects on sickness absence? A six year prospective study of the GAZEL cohort. J Epidemiol Community Health. 2003;57:285–93. doi: 10.1136/jech.57.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hensing G, Wahlstrom R. Chapter 7. Sickness absence and psychiatric disorders. Scandinavian. J Public Health. 2004;32:152. doi: 10.1080/14034950410021871. [DOI] [PubMed] [Google Scholar]
- 29.Chevalier A, Luce D, Blanc C, Goldberg M. Sickness absence at the French National Electric and Gas Company. Br J Ind Med. 1987;44:101–10. doi: 10.1136/oem.44.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melchior M, Berkman LF, Niedhammer I, et al. Social relations and self-reported health: a prospective analysis of the French Gazel cohort. Soc Sci Med. 2003;56:1817–30. doi: 10.1016/s0277-9536(02)00181-8. [DOI] [PubMed] [Google Scholar]
- 31.Feeney A, North F, Head J, et al. Socioeconomic and sex differentials in reason for sickness absence from the Whitehall II Study. Occup Environ Med. 1998;55:91–8. doi: 10.1136/oem.55.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Probst T, Brubaker T. The effects of job insecurity on employee safety outcomes: Cross-sectional and longitudinal explorations. J Occup Health Psychol. 2001;6:139–59. [PubMed] [Google Scholar]
- 33.Tüchsen F, Jeppesen J, Bach E. Employment Status, Non-Daytime Work and Gastric Ulcer In Men. Int J Epidemiol. 1994;23:365–70. doi: 10.1093/ije/23.2.365. [DOI] [PubMed] [Google Scholar]
- 34.Vermeulen M, Mustard C. Gender differences in job strain, social support at work, and psychological distress. J Occup Health Psychol. 2000;5:428–40. doi: 10.1037//1076-8998.5.4.428. [DOI] [PubMed] [Google Scholar]
- 35.Hammer LB, Cullen JC, Neal MB, et al. The longitudinal effects of work-family conflict and positive spillover on depressive symptoms among dual-earner couples. J Occup Health Psychol. 2005;10:138–54. doi: 10.1037/1076-8998.10.2.138. [DOI] [PubMed] [Google Scholar]
- 36.Berkman LF, Ertel K, Buxton O, Okechukwu C. Manager’s practices related to work-family balance predict employee cardiovascular risk and sleep duration in extended care settings. J Occup Health Psychol. 2010;15:316–29. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berkman L, Melchoir M. The Shape of Things to Come. How social policy impacts social integration and family structure to produce population health. In: Siegrist J, Marmot M, editors. Social Inequalities in Health. Oxford: Oxford University Press; 2006. pp. 55–72. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.