Abstract
Introduction
We examined the relationship of physical, mental, and neurocognitive function with employment and occupational status in the Childhood Cancer Survivor Study.
Methods
We included survivors ≥25 years of age with available Short Form-36 (physical and mental health component scores), Brief Symptom Inventory (depression, anxiety and somatization), and Neurocognitive Questionnaire (task efficiency, emotional regulation, organization, and memory). We generated relative risks (RR) from generalized linear models for these measures on unemployment (N=5386) and occupation (N=3763) outcomes adjusted for demographic and cancer-related factors, and generated sex-stratified models.
Results
Poor physical health was associated with an almost 8-fold higher risk of health-related unemployment (p<0.001) compared to survivors with normal physical health. Male survivors with somatization and memory problems were approximately 50% (p<0.05 for both) more likely to report this outcome, while task efficiency limitations was significant for both sexes (males: RR=2.43, p<0.001; females: RR=2.28, p<0.001). Employed female survivors with task efficiency, emotional regulation, and memory limitations were 13%-20% (p<0.05 for all) less likely to work in professional or managerial occupations than unaffected females.
Conclusions
Physical problems may cause much of the health-related unemployment among childhood cancer survivors. While both male and female survivors with neurocognitive deficits – primarily in task efficiencies – are at risk for unemployment, employed female survivors with neurocognitive deficits may face poor occupational outcomes more often than males.
Impact
Childhood cancer survivors are at risk for poor employment outcomes. Screening and intervention for physical, mental and neurocognitive limitations could improve employment outcomes for this population.
Keywords: pediatric cancer, employment status, physical health, mental health, neurocognitive function
Introduction
Psychosocial, physical and neurocognitive dysfunction are of particular importance to clinicians, patients, and families of children affected by cancer. These problems can arise years after primary treatment and may eventually affect survivors’ opportunities to participate fully in adult life roles, including their ability to find or maintain employment. Adult childhood cancer survivors are approximately two times more likely to be unemployed (1) and are more likely to report that health problems prohibit employment (2, 3) in contrast to healthy comparison groups. Employed survivors are at risk for working in lower-skill positions that typically have lower salaries and offer fewer benefits and chances for career mobility (4).
Physical, mental and neurocognitive deficits may affect survivors’ education and later career development. Adverse psychosocial outcomes are found in adolescent survivors (5), and several studies report physical and mental health limitations in adulthood for survivors (6-8). Neurocognitive difficulties often arise for survivors in adolescence when organization, reasoning and time management skills become increasingly important (9). Central nervous system (CNS) tumor and acute lymphoblastic leukemia survivors, who received the highest amounts of cranial radiation, are at the greatest risk of developing cognitive problems following treatment, although patients receiving neck or head radiation and other treatments also report dysfunction (10).
The types of neurocognitive deficits reported by childhood survivors typically include processing speed, memory and concentration problems; survivors with these problems are more likely to be unemployed (11, 12). While neurocognitive deficits play an obvious role in work ability, survivors with physical limitations and emotional health deficits are also less likely to be employed and have lower educational attainment and incomes than non-affected survivors (13-15). Additionally, unemployment is associated with psychological distress among survivors (16, 17).
Due to different diagnoses, treatments, and diagnosis ages, all which can affect education and the transition to adulthood, childhood cancer survivors are a heterogeneous population with a variety of employment needs. Psychosocial, physical and neurocognitive deficits have been linked to unemployment in earlier studies of childhood cancer survivors, but no research has reported on these measures in association with detailed employment outcomes. While assessing overall unemployment is important, research that informs tailored interventions is required to meet the unique employment needs of survivors.
The current study examines the association of psychosocial, physical and neurocognitive deficits with the report of being unable to work due to health or disability problems and being unemployed but seeking work. We examined the associations of psychosocial, physical and neurocognitive disability with type of occupation, which have not been examined in adult childhood cancer survivors. We hypothesized that poor psychosocial, physical and neurocognitive functioning would be significantly associated with unemployment due to health or disability (“health-related unemployment”), report of being unemployed but seeking work, and part-time employment. We also hypothesized that poor psychosocial, physical and neurocognitive functioning in employed survivors would be associated with less skilled occupations. Because men and women typically differ in their participation in the labor force, we generated sex-stratified models in addition to combined models.
Methods
Participants and Procedures
The Childhood Cancer Survivor Study (CCSS) is a multi-institutional research initiative started in 1994 to investigate health and behavioral outcomes in childhood and adolescent cancer survivors. The original cohort includes 14,357 survivors diagnosed with cancer when younger than age 21 years (18). Survivors were diagnosed between January 1, 1970 and December 31, 1986 and had survived at least five years from the time of diagnosis (19, 20). Eligible diagnoses included leukemia, CNS malignancies (all histologies), Hodgkin’s lymphoma (HL), non-Hodgkin lymphoma (NHL), kidney cancer, neuroblastoma, soft tissue sarcoma, or malignant bone tumor. The Human Subjects Committees at the 26 participating institutions approved the CCSS study protocol and participants provided informed consent.
CCSS survivors have completed a baseline survey (1994-96) and four follow-up surveys. The current analyses were based on data from the second follow-up survey (referred to as 2003 Follow-up, although completed from 2003-2005), because this survey contained the most detailed employment information. Detailed information on cancer type, treatments received, and clinical characteristics of the survivors was obtained from medical records.
There were 9308 survivors who completed the 2003 Follow-up survey. Of these, 2268 received a short form of the survey that did not include the relevant psychosocial questions described below, leaving 7040 survivors. In addition to completing the relevant psychosocial measures, participants had to meet eligibility of being age 25 and older at the time of the 2003 Follow-up survey, due to potential differences in employment status for participants still in school. The oldest participants were 54 years, so we used no upper age limit. Of the 5448 eligible survivors, 62 (1.1%) were missing employment status information. This left 5386 survivors (4093 employed and 1293 unemployed) for analyses examining current employment status. Of the 4093 employed survivors, 330 (8.1%) did not report their occupation resulting in 3763 available for the occupational comparisons.
The survivors missing employment status and occupation were more often male (53% and 58%, respectively vs. 50% for the eligible sample) and more likely to have a high school education or less (39% and 23%, respectively, vs. 15%). Central nervous system tumors were more common among those missing employment (23%) compared to those missing occupation (13%) and all eligible survivors (12%). Cranial radiation doses ≥18 Gy were more common among survivors missing employment status (33%) and occupation (28%) compared to the eligible sample (24%).
Measures
Independent Variables of Interest
Short Form-36 (SF-36)
Health-related quality of life was determined by the Medical Outcomes Study 36-item Short-form Health Survey, which is a widely-used generic health profile (21). We used the 8 subscale domains of mental health, physical health, emotional role function, physical role function, social health, pain, vitality and energy to calculate 2 overall component scores (physical health and mental health). Raw scores were converted to T-scores (range 0-100) and dichotomized so that a score at or below 40 (1 standard deviation below the population mean) indicated impairment for the two component scores (21, 22).
Brief Symptom Inventory (BSI)
The BSI-18, an 18-item checklist, measured acute symptoms of anxiety, depression, and somatic distress. Responses were scored to generate the anxiety, somatization and depression subscales. Subjects with T-scores of 63 or higher were classified as having psychological distress (23) for each of the three subscales.
CCSS-Neurocognitive Questionnaire (NCQ)
We used the CCSS-NCQ, a 25-item instrument developed and tested for relevant psychometric properties in the CCSS population and a sibling cohort (24). Four reliable factors discriminate survivors who were at “high risk” for neurocognitive dysfunction from healthy “low-risk” survivors: Task Efficiency, Emotional Regulation, Organization, and Memory. Raw scores for each factor were converted to T-scores, with higher scores (≥63) indicative of significant neurocognitive impairment.
Outcome Measures
Employment Status
Survivors reported their current employment status. We created mutually-exclusive outcomes to designate survivors who were either currently unemployed due to being: 1) unable to work due to illness or disability (health-related unemployment) or 2) unemployed but seeking work. To designate survivors voluntarily out of the labor market, we created a third category: 3) not in the labor force (caring for home or family and not seeking work; retired; student; and other), based on the Bureau of Labor Statistics not in the labor force definition (25). Our employment status categories are described elsewhere (3). Employed was designated as full-time (≥30 hours per week) or part-time (<30 hours per week).
Occupational Categories
Employed participants listed their main job title and primary tasks. These were coded according to the 2000 Standard Occupational Classification (SOC) System developed by the US Department of Labor (26). The SOC has 23 major occupational groups that include detailed information on occupations requiring similar job duties, skills, education, or experience. We excluded military occupations (10 survivors) because of potential differences in skill requirements. The remaining 22 groups were classified into 3 mutually exclusive occupational categories. First, occupations were coded as “Professional/Managerial” or “Service/Blue Collar”. We grouped Professional/Managerial positions according to assessment of skill levels and/or experience to capture higher-skill and higher experience jobs. Participants in the Service/Blue Collar group reporting mostly physically demanding work were coded as “Physical” and those reporting primarily sitting, standing, or walking while at work were coded as “Nonphysical”.
We used the 5-point Job Zone classification developed by occupational experts from the Occupational Information Network (O*Net) database to assess agreement with our occupational categories (27). Occupations with higher Job Zone scores require more education, preparation, and training, and the Professional/Managerial average Job Zone scores (3.4-5.0) were higher than those for Service/Blue Collar Physical and Nonphysical (1.0-2.7), which supports our classification process (4).
Other measures
Demographic and cancer-related variables are listed in Table 1. Cancer recurrence and secondary cancers (excluding nonmelanoma skin cancers) were examined to account for subsequent events. We hypothesized that cranial radiation would be highly related to neurocognitive function and created a categorical variable to investigate cranial doses: no radiation, scatter low (no treatment to head/brain, but patient received radiation to some part of the body [>0 to <1 Gy]), scatter high (no direct treatment to head/brain segment, but treatment was nearby [dose range ≥1 to ≤5 Gy]), or within radiation field doses <18 Gy, 18-24 Gy, and ≥25 Gy.
Table 1.
Survivor Demographics and Cancer-Related Variables by Sex
| Survivors N=5386a | P-value | ||||
|---|---|---|---|---|---|
|
| |||||
| Male N=2682 |
Female N=2704 |
||||
|
| |||||
| Demographics | N | % | N | % | |
| Current age (years) | |||||
| 25-34 | 1497 | 55.8 | 1500 | 55.5 | 0.02 |
| 35-44 | 966 | 36.0 | 932 | 34.5 | |
| 45+ | 219 | 8.2 | 272 | 10.0 | |
| Race/ethnicity | |||||
| White, non-Hispanic | 2355 | 88.1 | 2372 | 88.0 | 0.02 |
| Black, non-Hispanic | 56 | 2.0 | 64 | 2.4 | |
| Hispanic | 66 | 2.5 | 98 | 3.6 | |
| Other/mixed | 196 | 7.3 | 161 | 6.0 | |
| Education b | |||||
| High school education or less | 438 | 16.4 | 374 | 13.9 | <0.001 |
| Some college or more | 2240 | 83.6 | 2323 | 86.1 | |
| Marital status b | |||||
| Married | 1372 | 51.3 | 1488 | 55.3 | <0.001 |
| Not married | 1302 | 48.7 | 1204 | 44.7 | |
| Household Income b | |||||
| <$20,000 | 248 | 9.9 | 300 | 12.0 | 0.03 |
| $20,000-39,999 | 558 | 22.4 | 555 | 22.2 | |
| $40,000-59,999 | 548 | 22.0 | 511 | 20.5 | |
| $60,000-79,999 | 438 | 17.6 | 449 | 18.0 | |
| ≥$80,000 | 702 | 28.1 | 683 | 27.3 | |
|
| |||||
|
Cancer-Related Variables
| |||||
| Cancer Diagnosis | |||||
| Leukemia | 793 | 29.6 | 829 | 30.7 | <0.001 |
| Central Nervous System | 335 | 12.5 | 295 | 10.9 | |
| Hodgkin Disease | 433 | 16.1 | 478 | 17.7 | |
| Non-Hodgkin Lymphoma | 323 | 12.0 | 154 | 5.7 | |
| Wilms Tumor | 150 | 5.6 | 236 | 8.7 | |
| Neuroblastoma | 91 | 3.4 | 132 | 4.9 | |
| Sarcoma | 275 | 10.3 | 267 | 9.9 | |
| Bone Tumor | 282 | 10.5 | 313 | 11.6 | |
| Cancer recurrence | |||||
| Yes | 310 | 11.6 | 298 | 11.0 | 0.37 |
| No | 2372 | 88.4 | 2406 | 89.0 | |
| Secondary cancers | |||||
| Yes | 85 | 3.2 | 201 | 7.4 | <0.001 |
| No | 2597 | 96.8 | 2503 | 92.6 | |
| Years since diagnosis | |||||
| ≤20 | 641 | 23.9 | 620 | 22.9 | 0.23 |
| 21-30 | 1666 | 62.1 | 1689 | 62.5 | |
| >30 | 375 | 14.0 | 395 | 14.6 | |
| Cranial radiation | |||||
| None | 722 | 26.9 | 767 | 28.4 | 0.01 |
| Cumulative dose | |||||
| Scatter lowc | 747 | 27.9 | 859 | 31.8 | |
| Scatter highc | 92 | 3.4 | 64 | 2.4 | |
| <18 Gy | 237 | 8.8 | 222 | 8.2 | |
| 18-24 Gy | 344 | 12.8 | 348 | 12.9 | |
| ≥25 Gy | 251 | 9.36 | 218 | 8.06 | |
| Missing | 289 | 10.8 | 226 | 8.4 | |
5386 survivors had available information on employment and the measures of interest
Race reported by 2673 males and 2695 females; Education reported by 2678 males and 2697 females; Martial status reported by 2674 males and 2692 females; Household income reported by 2494 males and 2498 females.
Scatter Low=no treatment to head or brain, but patient received radiation to some part of the body (dose range >0 to <1 Gy); Scatter high=no direct treatment to segment, but treatment was nearby (≥1 to ≤5 Gy)
Statistical Methods
We compared overall demographic characteristics of survivors, and cancer- and treatment-specific variables by employment status and occupational categories. We calculated proportions reporting low and normal scores on the SF-36, BSI and NCQ for each outcome.
Two sets of analyses were used to explore the association of the SF-36, BSI and NCQ with the outcomes. First, we used generalized linear models (28) to generate relative risks (RR) and 95% confidence intervals (CI) to examine the associations among the SF-36, BSI and NCQ with employment status and occupational categories for survivors. We fit models to examine the specific reasons for unemployment (health or disability or seeking work) or for not being in the labor force. For the regression models examining health-related unemployment and unemployed but seeking work. The 639 survivors who were not in the labor force (retired, in school, or taking care of family) were excluded from the regression analyses, because such individuals are not typically included in labor force calculations (25). Sensitivity analyses that included these survivors were similar to the reported results. Because of collinearity with the other NCQ factors and the small number of survivors with organizational limitations for those reporting health-related unemployment and unemployed but seeking work, the organizational factor was not included in the models for these outcomes.
Among employed survivors, models were also fit to examine full-time versus part-time employment, professional/managerial occupations, and blue collar/service physical and nonphysical occupations. Because of potential differences for male and female survivors, we generated sex-stratified models. All models were adjusted for age, race, time since treatment, recurrence and secondary cancers, and as relevant, sex. As secondary analyses, models were fit to examine the impact of educational attainment and cranial radiation exposure on our outcomes. Because higher doses of cranial radiation are associated with educational difficulties (9, 29), these variables were examined separately.
Finally, we calculated proportions reporting limitations within each of the 6 mutually-exclusive employment status and occupational categories (not in the labor force, health-related unemployment, unemployed but seeking work, professional occupation, nonphysical occupation or physical occupation) adjusted for age, sex, and race. We compared these to the expected proportions of impairment using the standardization samples for the SF-36 and BSI and normed sibling data for the CCSS-NCQ. Analyses were performed using Stata version 11.0 (Stata Corp, College Station, TX). All reported p-values are two-sided, considered significant at α=0.05, and were not adjusted for multiple comparisons. The sex-specific models are sub-analyses of the total models, so these are not independent tests. Due to the large number of statistical tests being carried out, p-values between 0.05 and 0.01 should be viewed with some caution.
Results
Survivors tended to be less than 35 years of age (55.6%) and non-Hispanic white (88%), and were similarly composed of males (49.8%) and females (50.2%). The most frequently occurring cancer diagnosis was leukemia (30.1%), and the majority of survivors (72.4%) were exposed to some level of cranial radiation. When examined by sex (Table 1), female survivors were married more often than males (55.3% vs. 51.3%), less likely to have NHL than other cancers (5.7% vs. 12.0% of males), and more likely to report secondary malignancies than males (7.4% vs. 3.2%).
Female survivors were more likely to not be in the labor force (20% vs. 5% of males). However, if employed, female survivors were in Professional/Managerial occupations more often than males (59% compared to 53%), while only 3% of employed females held Blue Collar/Service jobs requiring physical activity compared to 15% of males. In Table 2, survivors who were unemployed due to health had the highest levels of functional loss, most notably in physical health (72%), task efficiency (62%) and memory (54%).
Table 2.
Proportions of survivor reporting normal and low SF-36, BSI and NCQ by employment and occupational status
| Employment Status |
Occupational Categories |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not currently employed N=1293 |
Employed N=4093c |
N=3763d |
||||||||||||||||
| Total | Not in the labor forceb N=639 (11.9%) |
Health-related unemploymentb N=399 (7.4%) |
Unemployed but seeking workb N=255 (4.7%) |
Full-time N=3699 (68.7%) |
Part-time N=394 (7.3%) |
Total | Professional/ Managerial N=2094 (55.6%) |
Service/Blue Collar |
||||||||||
| Nonphysical N=1317 (35.0%) |
Physical N=352 (9.4%) |
|||||||||||||||||
|
|
|
|
||||||||||||||||
| N=5386 | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N=3763 | N | (%) | N | (%) | N | (%) | |
|
SF-36
a
|
|
|||||||||||||||||
| Physical Health | ||||||||||||||||||
| ≥40 (normal) | 4509 | 534 | (84) | 113 | (28) | 205 | (80) | 3335 | (90) | 322 | (82) | 3369 | 1896 | (91) | 1159 | (88) | 314 | (89) |
| <40 (low) | 877 | 105 | (16) | 286 | (72) | 50 | (20) | 364 | (10) | 72 | (18) | 394 | 198 | (9) | 158 | (12) | 38 | (11) |
| Mental Health | ||||||||||||||||||
| ≥40 (normal) | 4429 | 515 | (81) | 254 | (64) | 160 | (63) | 3191 | (86) | 309 | (78) | 3218 | 1802 | (86) | 1107 | (84) | 309 | (88) |
| <40 (low) | 957 | 124 | (19) | 145 | (36) | 95 | (37) | 508 | (14) | 85 | (22) | 545 | 292 | (14) | 210 | (16) | 43 | (12) |
|
|
|
|||||||||||||||||
|
BSI
a
|
|
|||||||||||||||||
| Depression | ||||||||||||||||||
| <63 (normal) | 4771 | 572 | (90) | 273 | (68) | 189 | (74) | 3393 | (92) | 344 | (87) | 3433 | 1935 | (92) | 1185 | (90) | 313 | (89) |
| ≥63 (low) | 615 | 67 | (10) | 126 | (32) | 66 | (26) | 306 | (8) | 50 | (13) | 330 | 159 | (8) | 132 | (10) | 39 | (11) |
| Somatization | ||||||||||||||||||
| <63 (normal) | 4629 | 557 | (87) | 207 | (52) | 199 | (78) | 3326 | (90) | 340 | (86) | 3376 | 1912 | (91) | 1159 | (88) | 305 | (87) |
| ≥63 (low) | 757 | 82 | (13) | 192 | (48) | 56 | (22) | 373 | (10) | 54 | (14) | 387 | 182 | (9) | 158 | (12) | 47 | (13) |
| Anxiety | ||||||||||||||||||
| <63 (normal) | 4987 | 599 | (94) | 319 | (80) | 219 | (86) | 3482 | (94) | 368 | (93) | 3531 | 1981 | (95) | 1229 | (93) | 321 | (91) |
| ≥63 (low) | 399 | 40 | (6) | 80 | (20) | 36 | (14) | 217 | (6) | 26 | (7) | 232 | 113 | (5) | 88 | (7) | 31 | (9) |
|
|
|
|||||||||||||||||
|
NCQ
a
|
|
|||||||||||||||||
| Task efficiency | ||||||||||||||||||
| <63 (normal) | 4183 | 480 | (75) | 152 | (38) | 164 | (64) | 3127 | (85) | 260 | (66) | 3117 | 1786 | (85) | 1039 | (79) | 292 | (83) |
| ≥63 (low) | 1203 | 159 | (25) | 247 | (62) | 91 | (36) | 572 | (15) | 134 | (34) | 646 | 308 | (15) | 278 | (21) | 60 | (17) |
| Emotional regulation | ||||||||||||||||||
| <63 (normal) | 4297 | 487 | (76) | 230 | (58) | 175 | (68) | 3104 | (84) | 301 | (76) | 3128 | 1797 | (86) | 1051 | (80) | 280 | (80) |
| ≥63 (low) | 1089 | 152 | (24) | 169 | (42) | 80 | (31) | 595 | (16) | 93 | (24) | 635 | 297 | (14) | 266 | (20) | 72 | (20) |
| Organization | ||||||||||||||||||
| <63 (normal) | 4701 | 556 | (87) | 302 | (76) | 211 | (83) | 3307 | (89) | 325 | (82) | 3332 | 1842 | (88) | 1172 | (89) | 318 | (90) |
| ≥63 (low) | 685 | 83 | (13) | 97 | (24) | 44 | (17) | 392 | (11) | 69 | (18) | 431 | 252 | (12) | 145 | (11) | 34 | (10) |
| Memory | ||||||||||||||||||
| <63 (normal) | 4065 | 467 | (73) | 183 | (46) | 173 | (68) | 2983 | (81) | 259 | (66) | 2976 | 1718 | (82) | 972 | (74) | 286 | (81) |
| ≥63 (low) | 1321 | 172 | (27) | 216 | (54) | 82 | (32) | 716 | (19) | 135 | (34) | 787 | 376 | (18) | 345 | (26) | 66 | (19) |
SF-36: component scores <40 indicate low physical or mental health functioning; BSI: ≥63 indicates psychological distress; NCQ: ≥63 indicates poor functioning
Not in the labor force (retired, in school, or taking care of family); Health-related unemployment (unable work due to illness or disability); Unemployed but seeking work (unemployed but actively looking for work)
Employed=Currently full time (≥30 hours per week) or part time (<30 hours per week)
Occupation limited to participants currently employed that reported their occupation
Employment Status
None of the physical, emotional, or neurocognitive risk factors were associated with not participating in the labor force (retired, student, or taking care of family; data not shown). The results of the regression models examining the association between physical, emotional, or neurocognitive health and health-related unemployment, unemployed but seeking work, and full- vs. part-time employment are shown in Table 3. Overall, survivors with impaired physical health were at a high risk for health-related unemployment (RR=7.83, 95% CI 6.11-10.04) when compared to those reporting normal physical health. In sex-stratified models, male survivors with deficits in physical health, somatization, task efficiency, and memory were at a higher risk for health-related unemployment, whereas among female survivors, only physical health (RR=7.75, 95% CI 5.57-10.77) and task efficiency (RR=2.28, 95% CI 1.70-3.05) were significant.
Table 3.
Survivor Relative Risks (RR) and 95% Confidence Intervals for Employment Status by Sex
| Health-related unemployment | Unemployed but seeking work | Full-time vs. Part-time work | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| TOTAL N=4735 |
MALE N=2546 |
FEMALE N=2189 |
TOTAL N=4735 |
MALE N=2546 |
FEMALE N=2189 |
TOTAL N=4085 |
MALE N=2241 |
FEMALE N=1844 |
||||||||||
|
| ||||||||||||||||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
|
SF-36
a
| ||||||||||||||||||
| Physical Health | ||||||||||||||||||
| ≥40 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| <40 | 7.83d | 6.11-10.04 | 7.75d | 5.35-11.24 | 7.75d | 5.57-10.77 | 0.94 | 0.65-1.37 | 1.04 | 0.58-1.83 | 0.88 | 0.55-1.45 | 0.94c | 0.90-0.98 | 0.93b | 0.87-0.98 | 0.94 | 0.88-1.01 |
| Mental Health | ||||||||||||||||||
| ≥40 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| <40 | 1.20 | 0.98-1.48 | 1.35 | 0.98 -1.85 | 1.09 | 0.83-1.43 | 2.08d | 1.48-2.91 | 2.50d | 1.53-4.11 | 1.76b | 1.11-2.75 | 0.98 | 0.94-1.02 | 1.02 | 0.99-1.06 | 0.96 | 0.89-1.02 |
|
| ||||||||||||||||||
|
BSI
a
| ||||||||||||||||||
| Depression | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 1.15 | 0.92-1.43 | 0.99 | 0.69-1.40 | 1.30 | 0.97-1.73 | 1.57b | 1.10-2.24 | 1.62b | 1.00-2.63 | 1.39 | 0.81-2.43 | 0.99 | 0.94-1.04 | 0.96 | 0.92-1.01 | 1.00 | 0.89-1.12 |
| Somatization | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 1.32c | 1.08-1.61 | 1.48b | 1.08-2.02 | 1.23 | 0.95-1.59 | 1.14 | 0.79-1.66 | 1.35 | 0.79-2.31 | 0.98 | 0.60-1.53 | 1.03 | 0.99-1.07 | 1.02 | 0.97-1.07 | 1.04 | 0.97-1.12 |
| Anxiety | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 0.88 | 0.69-1.12 | 0.77 | 0.53-1.12 | 0.95 | 0.70-1.30 | 0.77 | 0.52-1.15 | 0.86 | 0.51-1.45 | 0.66 | 0.35-1.24 | 1.04 | 0.99-1.09 | 1.00 | 0.96-1.06 | 1.09 | 0.97-1.22 |
|
| ||||||||||||||||||
|
NCQ
a
| ||||||||||||||||||
| Task efficiency | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 2.38d | 1.89-3.01 | 2.43d | 1.67-3.53 | 2.28d | 1.70-3.05 | 1.39b | 1.02-1.91 | 1.35 | 0.85-2.13 | 1.46 | 0.96-2.23 | 0.91d | 0.87-0.94 | 0.93c | 0.89-0.97 | 0.87d | 0.81-0.94 |
| Emotional regulation |
||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 0.92 | 0.75-1.13 | 0.82 | 0.59-1.13 | 1.02 | 0.78-1.34 | 1.08 | 0.79-1.49 | 1.11 | 0.71-1.74 | 1.11 | 0.71-1.72 | 1.00 | 0.98-1.04 | 1.04b | 1.00-1.07 | 0.98 | 0.92-1.04 |
| Organization | ||||||||||||||||||
| <63 (ref) | NA | NA | NA | NA | NA | NA | 1 | 1 | 1 | |||||||||
| ≥63 | 0.99 | 0.95-1.04 | 0.96 | 0.93-1.00 | 1.04 | 0.97-1.12 | ||||||||||||
| Memory | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 1.23b | 1.01-1.50 | 1.45b | 1.04-2.03 | 1.15 | 0.90-1.47 | 0.91 | 0.67-1.24 | 0.78 | 0.50-1.22 | 1.01 | 0.73-1.53 | 0.97 | 0.94-1.01 | 0.97b | 0.93-1.00 | 0.97 | 0.91-1.03 |
Outcomes: Health-related unemployment (unable work due to illness or disability); Seeking work (unemployed but actively looking for work); Currently employed full time (≥30 hours per week) vs. part time (<30 hours per week) employment. Models adjusted for age, race, time since treatment, recurrence and secondary cancers. The “total” models are also adjusted for sex. Due to collinearity with the other NCQ factors and the small number of survivors with organizational limitations for those reporting health-related unemployment and seeking work, we did not include organization in the models for these outcomes. Models for unemployment exclude 639 survivors who are not in the labor force (retired, in school, or taking care of family); 12 additional survivors were missing covariate information.
SF-36: component scores <40 indicate low physical or mental health functioning; BSI: ≥63 indicates psychological distress; NCQ: ≥63 indicates poor functioning
Significant at <0.05
Significant at <0.01
Significant at <0.001
Because of the complex relationship among demographic factors, treatment and functioning, we ran separate secondary analyses to assess the impact of cranial radiation therapy and educational attainment (data not shown in tables). Adjusting for cranial radiation exposure did not substantially change the estimates, although memory was no longer significant for males. When adjusted for educational attainment, the relative risks for physical health attenuated but remained significant.
Poor mental health, depression, and task efficiency problems were associated with a higher risk of being unemployed but seeking work (Table 3). In gender-stratified models, poor mental health was associated more strongly with the outcome for males (RR=2.50, 95% CI 1.53-4.11) than females (RR=1.76, 95% CI 1.11-2.75; interaction P-value=0.03), while task efficiency was not significant for either sex. Depression was moderately associated with a 62% higher risk for males (RR=1.62, 95% CI 1.00-2.63). Neither cranial radiation nor education changed the estimates except that depression was no longer significant in the male-stratified models.
The third set of models examined full-time versus part-time employment status among employed survivors. Physical health deficits were associated with a 7% decreased likelihood of full-time employment for males and a similar, although non-significant, risk for females. Task efficiency limitations resulted in a lower likelihood of working full-time for both male (RR=0.93, 95% CI 0.89-0.97) and female (RR=0.87, 95% CI 0.81-0.94) survivors. For males, emotional regulation limitations had a slightly elevated association with full-time employment (RR=1.04, 95% CI 1.00-1.07), and a decreased association with memory limitations (RR=0.97, 95% CI 0.93-1.00), although the significance for both were eliminated when cranial radiation was included.
Occupational Categories
Professional/Managerial
Somatization and problems in task efficiency, emotional regulation and memory all conferred a 10%-15% lower likelihood of working in a professional occupation (Table 4). In sex-stratified models, female survivors with task, emotion and memory problems were 13%-20% less likely to be working in professional occupations, whereas there were no significant associations with these factors for males. Organizational problems for males and females were associated with an approximately 20% higher likelihood of this outcome, and female survivors reporting anxiety were at a higher risk (RR=1.24, 95% CI 1.00-1.53). Including either cranial radiation or education eliminated the association of task completion for females.
Table 4.
Survivor Relative Risks (RR) and 95% Confidence Intervals for Occupational Categories by Sex
| Professional/Managerial | Blue Collar-Service: Nonphysical | Blue Collar-Service: Physical | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| TOTAL N=3757 |
MALE N=2050 |
FEMALE N=1707 |
TOTAL N=3757 |
MALE N=2050 |
FEMALE N=1707 |
TOTAL N=3757 |
MALE N=2050 |
FEMALE N=1707 |
||||||||||
|
| ||||||||||||||||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
|
SF-36
a
| ||||||||||||||||||
| Physical Health | ||||||||||||||||||
| ≥40 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| <40 | 0.93 | 0.84-1.03 | 0.84 | 0.70-1.01 | 1.00 | 0.88-1.13 | 1.09 | 0.95-1.28 | 1.18 | 0.95-1.47 | 1.03 | 0.86-1.23 | 1.09 | 0.76-1.55 | 1.21 | 0.82-1.77 | 0.75 | 0.30-1.90 |
| Mental Health | ||||||||||||||||||
| ≥40 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| <40 | 1.07 | 0.97-1.18 | 1.09 | 0.93-1.27 | 1.06 | 0.93-1.19 | 0.99 | 0.86-1.14 | 0.99 | 0.79-1.26 | 0.97 | 0.82-1.15 | 0.72 | 0.50-1.05 | 0.77 | 0.50-1.19 | 0.58 | 0.26-1.32 |
|
| ||||||||||||||||||
|
BSI
a
| ||||||||||||||||||
| Depression | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 0.95 | 0.83-1.09 | 0.94 | 0.78-1.13 | 0.94 | 0.77-1.16 | 1.05 | 0.88-1.26 | 1.08 | 0.85-1.39 | 1.04 | 0.81-1.34 | 1.11 | 0.75-1.65 | 1.03 | 0.65-1.63 | 1.71 | 0.66-4.40 |
| Somatization | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 0.88b | 0.78-0.99 | 0.86 | 0.71-1.05 | 0.90 | 0.78-1.04 | 1.06 | 0.91-1.23 | 1.03 | 0.81-1.31 | 1.09 | 0.91-1.32 | 1.51b | 1.07-2.12 | 1.39 | 0.95-2.03 | 1.91 | 0.89-4.08 |
| Anxiety | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| ≥63 | 1.05 | 0.90-1.22 | 0.94 | 0.75-1.16 | 1.24b | 1.00-1.53 | 0.88 | 0.72-1.07 | 1.07 | 0.81-1.40 | 0.69b | 0.51-0.93 | 1.16 | 0.75-1.80 | 1.06 | 0.66-1.69 | 1.71 | 0.49-5.95 |
|
| ||||||||||||||||||
|
NCQ
a
| ||||||||||||||||||
| Task efficiency | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| ≥63 | 0.90b | 0.82-1.00 | 0.93 | 0.80-1.07 | 0.87b | 0.76-1.00 | 1.14b | 1.00-1.29 | 1.14 | 0.94-1.39 | 1.16 | 0.99-1.36 | 1.00 | 0.73-1.36 | 0.94 | 0.66-1.33 | 1.22 | 0.58-2.57 |
| Emotional regulation |
||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| ≥63 | 0.85c | 0.77-0.94 | 0.88 | 0.76-1.02 | 0.82c | 0.72-0.94 | 1.12b | 1.00-1.26 | 0.97 | 0.80-1.17 | 1.26c | 1.09-1.46 | 1.47c | 1.13-1.92 | 1.55c | 1.16-2.07 | 1.16 | 0.55-2.45 |
| Organization | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| ≥63 | 1.21d | 1.11-1.33 | 1.21c | 1.07-1.37 | 1.22c | 1.08-1.39 | 0.80c | 0.69-0.93 | 0.85 | 0.69-1.05 | 0.74c | 0.61-0.91 | 0.77 | 0.54-1.09 | 0.71 | 0.48-1.05 | 1.19 | 0.56-2.56 |
| Memory | ||||||||||||||||||
| <63 (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| ≥63 | 0.86c | 0.78-0.94 | 0.93 | 0.81-1.06 | 0.80d | 0.71-0.90 | 1.27d | 1.13-1.42 | 1.18 | 0.99-1.42 | 1.32d | 1.14-1.53 | 0.89 | 0.66-1.20 | 0.86 | 0.62-1.19 | 1.08 | 0.52-2.28 |
SF-36: component scores <40 indicate low physical or mental health functioning; BSI: ≥63 indicates psychological distress; NCQ: ≥63 indicates poor functioning. Of the 3763 survivors with available occupation, 6 were missing covariate information.
Significant at <0.05
Significant at <0.01
Significant at <0.001
Service-Blue Collar – nonphysical and physical
NCQ factors of task efficiency, emotional regulation, and memory problems were associated with a higher likelihood of a Blue Collar or Service job that did not require physical activity (Table 4). Only females showed significant differences for working in nonphysical occupations, with emotional (RR=1.26, 95% CI 1.09-1.46) and memory problems (RR=1.32, 95% CI 1.14-1.53) imparting a higher risk and anxiety and organizational problems associated with a lower risk. For physical jobs, only emotional regulation deficit was significant for males in sex-stratified models (RR=1.55, 95% CI 1.16-2.07). When cranial radiation was included, organizational deficits became significantly associated with a lower likelihood of having a physical occupation for males (RR=0.63, 95% CI 0.40-0.99).
Unemployment and Occupations – adjusted proportions
Figure 1 displays the proportions reporting limitations in the SF-36, BSI and NCQ by employment status adjusted for age, sex, and race. Low physical health was reported by 70% of survivors unemployed because of health and 20% who were currently seeking employment. Approximately 35% of survivors indicating health-related unemployment or seeking work had poor mental health. Physical health and mental health did not differ substantially among employed survivors or those not in the labor force, and were similar to population norms.
Figure 1. Adjusted proportions and 95% confidence intervals (95% CI) of survivors reporting limitations by employment statusa.
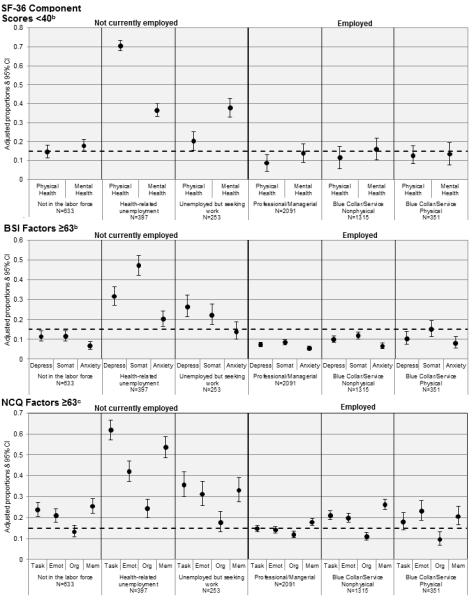
aProportions adjusted for age, sex and race; Unemployed categories: Not in the labor force (retired, in school, or taking care of family); Health-related (unable work due to illness or disability); Seeking work (unemployed but actively looking for work)
bDashed line represents SF-36 and BSI expected proportions of impairment using a threshold developed in the standardization sample; BSI categories: Depress=Depression; Somat=Somatization
cDashed line represents NCQ expected proportions of impairment using a threshold developed in the CCSS sibling data; NCQ categories: Task=Task efficiency; Emotion=Emotional regulation; Org=Organization; Mem=Memory
For the BSI and NCQ subscales, again both the health-related unemployment and seeking work groups reported the highest frequency of limitations. Survivors reporting health-related unemployment were most impaired; 47% of them reported somatization, 62% had task limitations and 54% had memory problems. Survivors unemployed but seeking work also had depression, somatization, and neurocognitive deficts in levels above the norms. While the employed survivors had BSI scores at or below population norm levels, for the Blue Collar/Service occupations, task, emotion, and memory limitations were all somewhat higher than the normed sibling comparison.
Discussion
This study is the first to explore the relationships of psychosocial, physical and neurocognitive health on different aspects of unemployment and occupational status for adult survivors of childhood cancer. Our findings suggest that multiple health domains influence unemployment and occupational status, and that these factors may be dissimilar among male and female survivors. Although comparisons by sex should be interpreted cautiously because males and females often have different attachments to the labor force, our findings suggest that interventions to improve employment outcomes for childhood cancer survivors may need to consider how limitations affect work status differentially for males and females. We also found that neurocognitive limitations are associated with a decreased likelihood of working in higher skill occupations for survivors. Additionally, survivors reporting health-related unemployment or being unemployed but seeking work are likely to have limitations in physical, mental and neurocognitive function at levels above comparison norms.
Childhood cancer survivors face health-related barriers to employment more often than sibling or population-based samples (2, 3), and our analyses suggest that limitations due to physical functioning may drive much of this difference. Survivors with poor physical health were almost eight times more likely to be unemployed due to health or disability, and this was consistent for both male and female survivors. Survivors with poor physical health were also more likely to work part-time, suggesting that even employed survivors could benefit from strategies to address physical limitations in the workplace. Physical limitations, however, were not significant for the seeking work group. Instead, both active depression and low mental health were associated with being unemployed but seeking work.
Survivors report more frequent executive functioning problems compared to siblings (11). In our analyses male survivors with task efficiency and memory problems were more likely to report health-related unemployment or to work part-time. Female survivors with task efficiency problems also were at a higher risk for these outcomes. However, we found no association with neurocognitive deficits or for females or males who were retired, in school, or taking care of family – that is, survivors with neurocognitive problems may not be selecting themselves out of the labor force. Instead, survivors with neurocognitive problems may want to work, but face cognitive or health status barriers to gaining or maintaining employment.
Employed female survivors with task efficiency, emotional regulation and memory limitations were less likely to report working in higher-skilled professional or managerial occupations. Deficits in task efficiency (e.g., ability to finish work or multitask), emotional regulation (e.g., becoming easily frustrated or upset), and memory (e.g., forgetting instructions, difficulty with recall) may be more of an impediment for females in obtaining higher-skilled jobs than males. When we adjusted the models for education and cranial radiation, these associations for females attenuated or disappeared, suggesting that efforts to mitigate educational barriers or late effects from cranial radiation for female survivors could reduce the burden of neurocognitive deficits on their occupational achievement.
In our multivariable models, both female and male survivors with organization problems were more likely to work in professional occupations, compared to the other NCQ factors that conferred a decreased likelihood. The statements comprising the organizational factor – I am disorganized, I have trouble finding things in my bedroom, closet, or desk, and My desk/workspace is a mess – may indicate different things for survivors depending on their underlying health status or their type of occupation. Organizational problems may not become apparent until the survivor is confronted with a busy lifestyle that includes occupational or other higher level obligations. Additionally, fewer survivors report organizational limitations compared to the other NCQ factors, suggesting that deficits of task attention, emotion and memory may be more important to target in employment interventions for this population.
This study has limitations that should be considered when interpreting the results. Firstly, we did not postulate specific hypotheses regarding the relationship of the SF-36, BSI and NCQ on our outcomes, in particular by sex. Because of the multiple outcomes investigated, our results should be interpreted cautiously. Secondly, we did not have information on how long survivors had been unemployed or looking for work, which could differ substantially according a survivor’s limitations. Also, alternatives to the ≥63 T-score cut-point to indicate psychological distress using for the Global BSI have been suggested (30). Because we were interested in the BSI subscales, we used this cut-point to be consistent with the current literature on cancer survivors and to be conservative in classifications of emotional distress.
These survivors were diagnosed during childhood. We have no information on when the psychosocial, physical and neurocognitive limitations first emerged nor do we know about their relationship with education or other social outcomes such as marriage, all which may impact adult work status over time. Finally, although the proportions missing employment status and occupation were minimal, comparison to the sample eligible for this analysis suggest that those missing employment and occupation may be at higher risk for poor employment outcomes due to having a lower education and higher levels of central nervous system tumors and cranial radiation. Our findings may underestimate the relationship between our measures of interest and unemployment.
In the general population, individuals with health limitations or disabilities are more likely to be unemployed (31). With the recent economic downturn, such individuals may be increasingly vulnerable in the workplace (32) and childhood cancer survivors may face additional risks due to neurocognitive, physical and mental deficits as a result of their treatment history. Unemployed survivors often lack the necessary resources, such as affordable health insurance, to obtain occupational services to address physical, mental and neurocognitive deficits that can hamper employment. Although there are legal protections that safeguard survivors from blatant employment discrimination and that obligate employers to provide reasonable accommodations for individuals with limitations (33), childhood cancer survivors continue to be unemployed and underemployed.
Interventions to improve employment outcomes for childhood cancer survivors should target physical health barriers to employment coupled with screening for mental health and neurocognitive problems. Currently employed survivors, especially women reporting neurocognitive deficits, may need education or training services in order to maximize their occupational potential, whereas unemployed survivors could benefit from assistance in managing any physical barriers to work. Moreover, longitudinal research is needed to identify survivors at risk for physical, mental and neurocognitive limitations during important developmental periods, such as adolescence, to provide early occupational intervention. Information about the risk of neurocognitive and other deficits, their effect on employment, and survivors’ legal rights, as well as recommendations for strategies to improve employment success, need to be widely distributed to survivors, their families, primary care clinicians, and professionals involved in vocational and rehabilitation services.
Acknowledgments
The Childhood Cancer Survivor Study is funded by the National Cancer Institute (U24 CA55727, principal investigator: (L. L. Robison). Support to St. Jude Children’s Research Hospital also provided by the Cancer Center Support (CORE) grant (CA 21765) and by the American, Syrian, Lebanese Associated Charities (ALSAC).
Footnotes
There are no conflicts of interest to report.
References
- 1.de Boer AG, Verbeek JH, van Dijk FJ. Adult survivors of childhood cancer and unemployment: A metaanalysis. Cancer. 2006;107(1):1–11. doi: 10.1002/cncr.21974. [DOI] [PubMed] [Google Scholar]
- 2.Dowling E, Yabroff KR, Mariotto A, McNeel T, Zeruto C, Buckman D. Burden of illness in adult survivors of childhood cancers: findings from a population-based national sample. Cancer. 2010;116(15):3712–21. doi: 10.1002/cncr.25141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirchhoff AC, Leisenring W, Krull KR, Ness KK, Friedman DL, Armstrong GT, et al. Unemployment among adult survivors of childhood cancer: a report from the childhood cancer survivor study. Med Care. 2010;48(11):1015–25. doi: 10.1097/MLR.0b013e3181eaf880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirchhoff AC, Krull KR, Ness KK, Park ER, Oeffinger KC, Hudson MM, et al. Occupational outcomes of adult childhood cancer survivors: A report from the childhood cancer survivor study. Cancer. 2011 doi: 10.1002/cncr.25867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schultz KA, Ness KK, Whitton J, Recklitis C, Zebrack B, Robison LL, et al. Behavioral and social outcomes in adolescent survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2007;25(24):3649–56. doi: 10.1200/JCO.2006.09.2486. [DOI] [PubMed] [Google Scholar]
- 6.Gurney JG, Krull KR, Kadan-Lottick N, Nicholson HS, Nathan PC, Zebrack B, et al. Social Outcomes in the Childhood Cancer Survivor Study Cohort. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeltzer LK, Recklitis C, Buchbinder D, Zebrack B, Casillas J, Tsao JC, et al. Psychological Status in Childhood Cancer Survivors: A Report From the Childhood Cancer Survivor Study. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ness KK, Hudson MM, Ginsberg JP, Nagarajan R, Kaste SC, Marina N, et al. Physical Performance Limitations in the Childhood Cancer Survivor Study Cohort. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitby PA, Robison LL, Whitton JA, Zevon MA, Gibbs IC, Tersak JM, et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. 2003;97(4):1115–26. doi: 10.1002/cncr.11117. [DOI] [PubMed] [Google Scholar]
- 10.Oeffinger KC, Nathan PC, Kremer LC. Challenges after curative treatment for childhood cancer and long-term follow up of survivors. Hematol Oncol Clin North Am. 2010;24(1):129–49. doi: 10.1016/j.hoc.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Kadan-Lottick NS, Zeltzer LK, Liu Q, Yasui Y, Ellenberg L, Gioia G, et al. Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. J Natl Cancer Inst. 2010;102(12):881–93. doi: 10.1093/jnci/djq156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellenberg L, Liu Q, Gioia G, Yasui Y, Packer RJ, Mertens A, et al. Neurocognitive status in long-term survivors of childhood CNS malignancies: a report from the Childhood Cancer Survivor Study. Neuropsychology. 2009;23(6):705–17. doi: 10.1037/a0016674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ness KK, Gurney JG, Zeltzer LK, Leisenring W, Mulrooney DA, Nathan PC, et al. The impact of limitations in physical, executive, and emotional function on health-related quality of life among adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Arch Phys Med Rehabil. 2008;89(1):128–36. doi: 10.1016/j.apmr.2007.08.123. [DOI] [PubMed] [Google Scholar]
- 14.Nathan PC, Ness KK, Greenberg ML, Hudson M, Wolden S, Davidoff A, et al. Health-related quality of life in adult survivors of childhood wilms tumor or neuroblastoma: A report from the childhood cancer survivor study. Pediatr Blood Cancer. 2006 doi: 10.1002/pbc.20949. [DOI] [PubMed] [Google Scholar]
- 15.Langeveld NE, Stam H, Grootenhuis MA, Last BF. Quality of life in young adult survivors of childhood cancer. Support Care Cancer. 2002;10(8):579–600. doi: 10.1007/s00520-002-0388-6. [DOI] [PubMed] [Google Scholar]
- 16.Zebrack BJ, Zevon MA, Turk N, Nagarajan R, Whitton J, Robison LL, et al. Psychological distress in long-term survivors of solid tumors diagnosed in childhood: a report from the childhood cancer survivor study. Pediatr Blood Cancer. 2007;49(1):47–51. doi: 10.1002/pbc.20914. [DOI] [PubMed] [Google Scholar]
- 17.Zebrack BJ, Gurney JG, Oeffinger K, Whitton J, Packer RJ, Mertens A, et al. Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2004;22(6):999–1006. doi: 10.1200/JCO.2004.06.148. [DOI] [PubMed] [Google Scholar]
- 18.Leisenring WM, Mertens AC, Armstrong GT, Stovall MA, Neglia JP, Lanctot JQ, et al. Pediatric Cancer Survivorship Research: Experience of the Childhood Cancer Survivor Study. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robison LL, Mertens AC, Boice JD, Breslow NE, Donaldson SS, Green DM, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: a multi-institutional collaborative project. Med Pediatr Oncol. 2002;38(4):229–39. doi: 10.1002/mpo.1316. [DOI] [PubMed] [Google Scholar]
- 20.Robison LL, Armstrong GT, Boice JD, Chow EJ, Davies SM, Donaldson SS, et al. The Childhood Cancer Survivor Study: A National Cancer Institute-Supported Resource for Outcome and Intervention Research. J Clin Oncol. 2009 doi: 10.1200/JCO.2009.22.3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 22.Ware JE, Jr., Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. The Health Institute; Boston: 1994. [Google Scholar]
- 23.Derogatis LR. Administration, Scoring, and Procedures Manual. NCS Pearson, Inc.; Minneapolis, MN: 2001. Brief Symptom Inventory (BSI)-18. [Google Scholar]
- 24.Krull KR, Gioia G, Ness KK, Ellenberg L, Recklitis C, Leisenring W, et al. Reliability and validity of the Childhood Cancer Survivor Study Neurocognitive Questionnaire. Cancer. 2008;113(8):2188–97. doi: 10.1002/cncr.23809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bureau of Labor Statistics [Internet] U.S. Department of Labor, Labor Force Characteristics; [Cited April 25, 2011]. Available from: http://www.bls.gov/cps/lfcharacteristics.htm#laborforce. [Google Scholar]
- 26.U.S. Department of Labor [Cited April 25, 2011];Standard Occupational Classification System (SOC) [Internet] Available from: http://www.bls.gov/SOC/
- 27.Peterson NG, Mumford MD. Understanding work using the Occupational Information Network (O*NET): Implications for practice and research. Personnel Psychology. 2001;54(2):451–492. [Google Scholar]
- 28.Hosmer DW, Lemeshow L. Applied logistic regression. 2nd ed John Wiley and Sons; 2000. [Google Scholar]
- 29.Barrera M, Shaw AK, Speechley KN, Maunsell E, Pogany L. Educational and social late effects of childhood cancer and related clinical, personal, and familial characteristics. Cancer. 2005;104(8):1751–60. doi: 10.1002/cncr.21390. [DOI] [PubMed] [Google Scholar]
- 30.Recklitis CJ, Rodriguez P. Screening childhood cancer survivors with the brief symptom inventory-18: classification agreement with the symptom checklist-90-revised. Psychooncology. 2007;16(5):429–36. doi: 10.1002/pon.1069. [DOI] [PubMed] [Google Scholar]
- 31.Brault M. In: Americans With Disabilities: 2005, Current Population Reports. Bureau C, editor. Washington, DC: 2008. pp. P70–117. [Google Scholar]
- 32.Autor DH, Duggan M. Supporting Work: A Proposal for Modernizing the U.S. Disability Insurance System. The Center for American Progress and The Hamilton Project; 2010. [Google Scholar]
- 33.Short PF, Vargo MM. Responding to employment concerns of cancer survivors. J Clin Oncol. 2006;24(32):5138–41. doi: 10.1200/JCO.2006.06.6316. [DOI] [PubMed] [Google Scholar]


