Abstract
Obsessive-compulsive disorder (OCD) and generalized anxiety disorder (GAD) are both defined by excessive negatively-valenced cognitions. Although obsessional thoughts are considered essential to OCD and perseverative worry is considered essential to GAD, these excessive cognitions have been found to co-occur in both disorders. Accordingly, a common diathesis may influence the emergence of excessive thoughts in both disorders. The present study examined deficits in attentional control as a cognitive vulnerability that may contribute to both obsessional thought and perseverative worry. Patients with OCD (n = 30), GAD (n = 29), and non-clinical controls (NCC; n = 29) completed measures of obsessional thoughts, perseverative worry, and attentional control. Deficits in self-reported attentional control were found in both OCD and GAD relative to the NCC. However, attentional control was only related to excessive cognition in the GAD patient group, where deficits were associated with increased perseverative worry. Mediational modeling suggested that trait anxiety mediated the relationship between attentional control and perseverative worry in GAD. Implications of these findings for conceptualizing the role of attentional control in the genesis of excessive cognitions in OCD and GAD are discussed.
Keywords: OCD, GAD, obsession, worry, rumination, attention
Among the anxiety disorders in the DSM-IV (American Psychiatric Association [APA], 2000), two are defined primarily by excessive negatively-valenced cognitions: obsessive-compulsive disorder (OCD) and generalized anxiety disorder (GAD) (Brown, Moras, Zinbarg, & Barlow, 1993). In OCD, excessive emotionally-valenced cognition can be seen in obsessions, which are unwanted, repetitive thoughts considered inappropriate or harmful. Obsessional thoughts motivate compulsions, rigid behaviors performed ritualistically to undo harm related to obsessions (APA, 2000). In GAD, excessive anxiogenic cognition takes the form of perseverative worry, which consists of apprehensive thoughts about everyday concerns, such as finances, academic performance, and household maintenance (Burns, Keortge, Formea, & Sternberger, 1996). Perseverative worry sustains a high level of negative affect and physiological arousal, which may lead to tension, fatigue, and other somatic complaints (APA, 2000). Research examining the nature of these excessive cognitions supports their diagnostic specificity, as patients with OCD report more obsessional thoughts than patients with GAD, and patients with GAD report more perseverative worry than patients with OCD (Brown, Antony, & Barlow, 1992; Brown et al., 1993). However, obsessional thoughts and perseverative worry often co-occur in clinical and non-clinical samples (Brown et al., 1993; Clark &Claybourn, 1997).Indeed, self-report measures of obsessional thoughts and perseverative worry have been found to share a considerably degree of variance (Zinbarg& Barlow, 1996; Burns et al., 1996; Freeston et al., 1994).
Rumination is yet another form of excessive cognition that has been implicated in OCD and GAD. Rumination involves passive, repetitive dwelling on one's distress, as well as its causes and consequences (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). By keeping individuals fixated on their problems, rumination is believed to maintain or worsen negative affect and prevent active coping strategies that could alleviate distress. Rumination has been investigated mostly in the context of depression (e.g., Nolen-Hoeksema, 1991); however, increased rumination has also been observed in OCD (Fineberg, Fourie, Gale, Sivakumaran, 2005) and GAD (Rector, Antony, Laposa, Kocovski, & Swinson, 2008), and may partially explain comorbid depression frequently found in these disorders. In addition, self-report measures of rumination have been found to share a considerable degree of variance with measures of worry (Fresco, Frankel, Mennin, Turk, & Heimberg, 2002; Muris, Roelofs, Rassin, Franken, & Mayer, 2005), and symptoms of OCD (Grisham & Williams, 2009).
The association between obsessional thoughts commonly observed in OCD, perseverative worry that is characteristic of GAD, and rumination that is associated with both disorders may suggest that these cognitive symptoms derive from a common underlying mechanism. Alternatively, these cognitive processes may only share phenomenology; while obsessions, worries, and ruminations may all be described as unpleasant, they may arise from unrelated processes. An intermediate viewpoint argues that while obsessional thoughts, perseverative worry, and rumination are all distinct in terms of content and form, they are all exacerbated by a common cognitive vulnerability. One such cognitive vulnerability may be deficits in attentional control (Derryberry & Reed, 2002). Attentional control refers to one's top-down command over different components of attention, and is necessary for the flexible regulation of cognitive resources. Attentional control has two dimensions, corresponding to the components of attention that may be brought under voluntary control. Attentional Focus encompasses one's ability to maintain attentional engagement in the face of distraction, while Attentional Shifting encompasses one's ability to execute attentional disengagement, in order to shift attention away from a distraction or towards a new task. Reliable individual differences arise on measures of attentional control, and as such attentional control may be conceptualized as a trait capturing the control of information processing (Derryberry & Reed, 2002).
Diminished attentional control may confer risk for perseverative worry, obsessional thoughts, and rumination by undermining one's ability to manage attentional resources towards the prevention of “unwanted negative thoughts” (Brown et al., 1993; Levens, Muhtadie, & Gotlib, 2009). Excessive negatively-valencedcognition may be facilitated by deficits in attentional focus, which would allow unwanted thoughts to gain entry into working memory despite suppression attempts (Rosen & Engle, 1998). The inability to disengage attention from obsessional thoughts, perseverative worries, and rumination post-intrusion may be exacerbated by weakened attentional shifting. Thus, deficits in attentional control could account for the intrusion of obsessional thoughts, perseverative worries, and rumination as well as difficulty coping with these excessive cognitions. Although no studies have directly investigated the relationship between excessive cognitions in OCD and GAD, and attentional control, indirect evidence supports the proposed associations. For example, deficits in “cognitive control,” a construct similarly defined by control over attention and susceptibility to distraction, have been found in patients with OCD (Barrett & Healy, 2003) and GAD (Jazbec, McClure, Hardin, Pine, & Ernst, 2006).
If attentional control deficits indeed contribute to symptoms of OCD or GAD, the treatment implications may be significant, as attentional control shows considerable plasticity and may be a potential treatment target (Posner & Rothbart, 2007). Both meditation and computer-based training procedures have shown initial success in augmenting attentional control (Tang & Posner, 2009). In addition, procedures that train attention away from threat have been shown to reduce symptoms of anxiety disorders (Hakamata et al., 2010), and there is some evidence that these procedures work in part by augmenting attentional control (Browning, Holmes, Murphy, Goodwin, & Harmer, 2009; Klumpp & Amir, 2009).
The present study sought to directly examine the relationship between excessive negatively-valenced cognitions in OCD and GAD and components of self-reported attentional control. It was predicted that individuals with OCD and GAD would show comparable attentional control deficits relative to controls, and that within each disorder, deficits in attentional control would be most highly correlated with the primary excessive cognition, such that in OCD, attentional control would be correlated most highly with obsessional thoughts, whereas in GAD, attentional control would be most highly correlated with perseverative worry. Attentional control was predicted to show weaker correlations with rumination, compared to obsessional thoughts or perseverative worry, in OCD and GAD, respectively. Lastly, trait anxiety was assessed in order to gain further insight into the nature of relations between attentional control and excessive cognitions in GAD. Trait anxiety has been found to be associated with self-report (Derryberry & Reed, 2002), behavioral (Pacheco-Unguetti, Acosta, Callejas & Lupiáñez, 2010), and neural (Bishop, 2009) measures of attentional control, and is also strongly correlated with measures of perseverative worry (e.g., Davey, 1994), but not obsessional thoughts (Lee & Telch, 2005).Accordingly, mediational modeling of the relations between attentional control, trait anxiety, and perseverative worry was conducted to explore the relations between these constructs in GAD.
Method
Participants
A total of 88 adults participated: 30 patients with obsessive compulsive disorder (OCD; age M = 39.23, SD = 11.90; % female = 50; % Caucasian = 96.7, % multi-ethnic/other = 3.3; % college graduate = 65.51), 29 patients with generalized anxiety disorder (GAD; age M = 38.00, SD = 10.91; % female = 48, % Caucasian = 86, African-American = 3.4, % Asian = 6.9, % multi-ethnic/other = 3.4; % college graduate 56.67), and 29 non-clinical controls without a history of any anxiety disorder (NCC; age M= 39.76, SD = 10.37; % female = 52; % Caucasian = 72.4; % African-American = 17.2, % Asian = 3.4, % multi-ethnic/other = 6.9; % college graduate = 72.41). Groups did not differ in terms of age, gender, ethnicity, or education level (ps> .05). NCC and GAD participants were recruited from community advertisements or referral from Vanderbilt Adult Psychiatry Outpatient Clinic. An initial dichotomous phone screen with the Generalized Anxiety Disorders Questionnaire 4th Edition (GADQ-IV; Newman, Zuellig, Kachin, Constantino, & Cashman, 2002) was performed for individuals calling in response to GAD symptom community advertisements. OCD participants were mainly recruited from the Obsessive Compulsive Disorder/Tourette Syndrome Program at Vanderbilt University. Given that some OCD participants were receiving treatment, the Yale-Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989) was administered to determine if symptoms were currently at moderate levels or higher (≥16) for OCD participants. The Structured Clinical Interview for the DSM–IV (SCID-I; First, Spitzer, Gibbon, & Williams, 2002) was administered to determine diagnoses for all participants. Exclusionary criteria for all groups were a diagnosis of bipolar disorder, substance abuse, attention deficit hyperactivity disorder, pervasive developmental disorders, mental retardation, or current or past central nervous system diseases. The clinical groups were non-overlapping (i.e., OCD participants could not have a current diagnosis or history of GAD and vice versa). SCIDs were conducted by a graduate-level clinician and phone screening was conducted by a research assistant; both were trained and supervised by a licensed clinical psychologist. All participants provided informed consent and the study was approved by the Vanderbilt Institutional Review Board.
Measures
SCID-I, Research Version, Patient Edition
(First et al., 2002). The SCID-I is a semi-structured clinical interview used to diagnosis mental disorders as delineated in the DSM-IV. Inter-rater and test-retest reliability estimates for the SCID-I vary, but have generally been found to be in the fair to good range (e.g., Lobbestael, Leurgans, & Arntz, 2011).
Generalized Anxiety Disorders Questionnaire 4th Edition
(GADQ-IV; Newman et al., 2002). The GADQ-IV is a 9-item self-report measure intended for use as an initial screen in the diagnosis of Generalized Anxiety Disorder (GAD) based on the DSM-IV criteria. The GADQ-IV has been found to have acceptable test-retest reliability and convergent and discriminant validity, as well as clinical validity in predicting DSM-IV diagnosis of GAD (Newman et al., 2002). During phone screenings, the GAD-IV items were read to patients, without additional questions besides those for clarification.
Yale-Brown Obsessive-Compulsive Scale
(Y-BOCS; Goodman et al., 1989). The Y-BOCS is a semi-structured interview used to assess OCD symptom subtype and symptom severity. A 10-item self-report measure derived from the semi-structured clinical interview measures the following five parameters of obsessions (Items 1-5) and compulsive rituals (Items 6-10): (a) time occupied/frequency, (b) interference, (c) distress, (d) resistance, and (e) perceived control. Each item is rated on a five-point Likert Scale from 0 (no symptoms) to 4 (severe symptoms). The Y-BOCS has been found to have satisfactory reliability and validity (Goodman et al., 1989).
Attentional Control Scale
(ACS; Derryberry& Reed, 2002). The ACS is a 20-item self-report questionnaire that assesses control of attention across two domains; focusing, the ability to maintain attention on a given task, and shifting, the ability to reallocate attention to a new task or to engage attention on multiple tasks. Each item is rated on a 4-point Likert scale from “1” (almost never) to “4” (always) with higher scores indicative of better attentional control. The ACS total score had adequate internal consistency (α = .86), as did the focus and shifting subscales (α = .82 and α =.75, respectively), in the present sample. It is important to note that the ACS does not contain questions related to emotionally-valenced situations, and as such attempts to capture a general information processing trait uncontaminated by reactions to emotional stimuli or cognitions.
Obsessive Compulsive Inventory – Revised
(OCI-R; Foa et al., 2002). The OCI-R is an 18-item questionnaire of OCD symptoms experienced in the past month rated on a 5-point Likert scale, “0 = not at all” up to “4 = very much.” The OCI-R has six dimensional subscales, of which only the Obsessing subscale was relevant to the present study. The obsessing subscale of the OCI-R had adequate internal consistency (α = .88) in the present sample.
Penn State Worry Questionnaire
(PSWQ; Meyer, Miller, Metzger, &Borkovec, 1990). The PSWQ assesses a person's overall tendency to experience worry with 16 self-report items rated on a 5-point Likert scale that ranges from “1 = not typical of me” to “5 = very typical of me.” PSWQ had excellent internal consistency (α = .95)in the present sample.
Rumination-Reflection Questionnaire
(RRQ; Trapnell & Campbell, 1999). The RRQ is a 24-item measure of self-attentiveness composed of two 12-item subscales that parse neurotic self-attentiveness (rumination) and intellectual self-attentiveness (reflection). Items are rated on a 5-point Likert scale ranging from “1 = strongly disagree” to “5 = strongly agree.” Only the rumination subscale was relevant to the present study. The RRQ Rumination subscale had excellent internal consistency (α = .95) in the present sample.
The State Trait Anxiety Inventory--Trait Version, Form Y
(STAI-T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) is a 20-item scale that measures the enduring or chronic experience of anxiety. The STAI-T had excellent internal consistency (α = .94) in the present sample.
Procedure
Participants provided informed consent and were administered the SCID-I (preceded by the Y-BOCS for OCD participants). Subsequently, participants were seated at a computer where they completed the self-report questionnaires. Participants were debriefed regarding the nature of the research and provided financial compensation following completion of the study.
Results
Group differences in attention control and excessive cognitions
One-Way Analysis of Variance (ANOVA) revealed a main effect of group for the ACS Focus subscale [F (2, 85) = 14.51, p< .001] and the ACS Shift subscale [F (2, 85) = 13.26, p< .001]). As predicted, follow-up Tukey's HSD tests revealed that compared to the control group, the OCD and GAD groups reported greater deficits in attentional focus and shifting (ps< .001). The two patient groups did not differ from each other in the severity of these deficits (p> .10).
One-Way ANOVAs also revealed a main effect of group for the OCI-R Obsessing subscale [F (2, 85) = 58.35, p< .001], PSWQ [F (2, 85) = 65.53, p< .001], and RRQ rumination subscale [F (2, 85) = 32.70, p< .001]. Follow-up Tukey's HSD tests revealed that compared to the control group, the OCD and GAD groups reported more obsessional thoughts, perseverative worry, and rumination (ps< .001). Although the OCD group reported significantly more obsessional thoughts than the GAD group (p< .001), the two groups did not differ from each other in perseverative worry or rumination (ps> .10). Means and standard deviations for all measures are provided in Table 1.
Table 1. Means and SDs for symptom measures.
| OCD | GAD | NCC | |
|---|---|---|---|
| N | 30 | 29 | 29 |
| ACS Shift | 27.27 (5.23) | 26.72 (4.70) | 32.52 (4.22)a |
| ACS Focus | 20.07 (5.36) | 20.48 (4.54) | 26.00 (4.09)a |
| OCI-R Obsessing | 7.47 (3.34) | 3.45 (2.49)b | 0.52 (0.99)a |
| PSWQ | 61.83 (11.83) | 62.00 (10.34) | 35.48 (8.82)a |
| RRQ Rumination | 47.03 (8.90) | 45.28 (7.78) | 30.28 (9.36) a |
| STAI-T | 53.67 (10.41) | 53.34 (10.24) | 35.59 (8.88) a |
Note: Means in the same row with different superscripts are significantly different (all p's < .001); OCD = obsessive-compulsive disorder; GAD = generalized anxiety disorder; NCC = non-clinical control; ACS Shift = Attentional Control Scale – Shifting Subscale; ACS Focus = Attentional Control Scale – Focus Subscale; OCI-R-Obsessing = Obsessive Compulsive Inventory – Revised – Obsessing subscale; PSWQ = Penn State Worry Questionnaire; STAI-T =State Trait Anxiety Inventory—Trait Version, Form Y
Association between cognitions and attention control
Correlations between cognitive symptom measures and components of attentional control were examined within each group (Table 2). Using the Bonferroni correction procedure for multiple comparisons, the family wise Type 1 error rate was set to .05 for each ACS subscale in each group. In the GAD group, both attentional focus and attentional shifting were specifically correlated with perseverative worry (Focus: r = -.54, p< .01; Shift: r = -.48, p< .01), in line with predictions. However, in the OCD group, the predicted correlations between deficits in components of attentional control and obsessional thoughts were not found; in patients with OCD, there were no significant correlations between components of attentional control and any type of excessive cognition (ps> .017). In the NCC group, the only significant correlation was between attentional focus and rumination (r = -.56, p< .01).
Table 2. Correlations between attentional control and cognitive symptom measures.
| OCD | GAD | NCC | ||||
|---|---|---|---|---|---|---|
| ACS Focus | ACS Shift | ACS Focus | ACS Shift | ACS Focus | ACS Shift | |
| OCI-R Obsessing | -.10 | .04 | -.11 | -.18 | -.10 | -.14 |
| PSWQ | -.20 | .06 | -.54* | -.48* | -.43 | -.18 |
| RRQ Rumination | .05 | -.01 | -.28 | -.31 | -.56* | -.25 |
Note:
p< .017; OCD = obsessive-compulsive disorder; GAD = generalized anxiety disorder; NCC = non-clinical control; ACS Shift = Attentional Control Scale – Shifting Subscale; ACS Focus = Attentional Control Scale – Focus Subscale; OCI-R-Obsessing = Obsessive Compulsive Inventory – Revised – Obsessing subscale; PSWQ = Penn State Worry Questionnaire; RRQ Rumination = Rumination-Reflection Questionnaire – Rumination subscale
Trait Anxiety as a Mediator in GAD
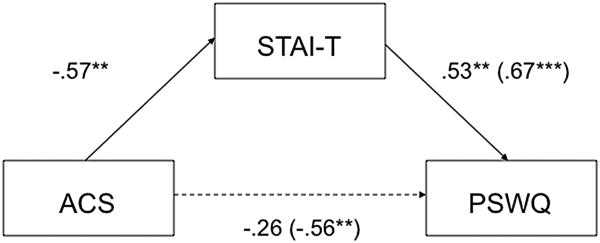
Prior research suggests that the presence of trait anxiety may largely account for levels of worry and its maladaptive consequences (Mathews, 1990; Olatunji, Schottenbauer, Rodriguez, Glass, &Arnkoff, 2007). Accordingly, trait anxiety was examined as a mediator of the relationship between attentional control and perseverative worry in GAD, based on the recommendations of Baron and Kenny (1986). For this mediational analysis (depicted in Figure 1), attentional control was assessed using the ACS total score. Evidence of mediation requires the following conditions to be present: (a) a significant relationship between trait anxiety and attentional control (r = -.57. p< .01), (b) a significant association between perseverative worry and attentional control (r = -.56. p< .01), (c) a significant relationship between trait anxiety and perseverative worry (r = .67. p< .01), and (d) the statistically significant relationship between perseverative worry and attentional control diminishes or disappears when trait anxiety is controlled. Pearson correlation coefficients indicated that conditions (a), (b), and (c) above were met. Condition (d), the critical test of mediation, was investigated by examining the magnitude of the relationship between attentional control and perseverative worry after controlling for trait anxiety. A two-step regression equation was estimated predicting perseverative worry with attentional control entered in the first step and trait anxiety in the second step as predictors. The key comparison involved the change in standardized regression coefficients for attentional control from step 1 (total effect) to step 2 (direct effect controlling for trait anxiety). The highly significant (p< .01) relationship between attentional control and perseverative worry became non-significant (p> .10) after controlling for trait anxiety. Moreover, trait anxiety emerged as a significant, unique predictor of perseverative worry. Thus, all a priori conditions were met, indicating that trait anxiety mediated the relationship between attentional control and perseverative worry. The significance of this mediated effect was statistically tested via the Sobel (1982) procedure, and the results of this test suggest that the effect of attentional control on perseverative worry is transmitted via trait anxiety (Sobel test of the significance of the indirect path: z = 2.31, p < .05). Complete results of these analyses are provided in Table 3.1
Figure 1. Mediational model of the relations between attentional control, trait anxiety, and perseverative worry in GAD.
Note: ** p< .01, *** p< .001; GAD = generalized anxiety disorder; ACS = Attentional Control Scale; STAI-T =State Trait Anxiety Inventory—Trait Version, Form Y; PSWQ = Penn State Worry Questionnaire
Table 3. Reductions in standardized regression coefficients for attentional control in the prediction of worry after controlling for trait anxiety in patients with GAD.
| Steps in regression | Values |
|---|---|
| Step 1 | |
| ΔR2 for ACS | .31** |
| β for ACS | -.56** |
| Step 2 | |
| ΔR2 for STAI-T | .45** |
| β for ACS controlling for STAI-T | -.26 |
| β for STAI-T | .53** |
| Overall R2 | .50 |
| F (2, 26) | 12.74*** |
Note:
p< .01,
p < .001; GAD = generalized anxiety disorder; ACS = Attentional Control Scale; STAI-T = State Trait Anxiety Inventory—Trait Version, Form Y
Discussion
Efforts to delineate the nature of GAD and OCD have had difficulty accounting for the co-occurance and phenomenological overlap between perseverative worry and obsessional thoughts. The present study sought to further delineate excessive cognitions in these disorders by examining their differential relations to a possible cognitive diathesis: deficits in attentional control. In terms of the diagnostic specificity of excessive cognitions, the present findings were only partially consistent with previous studies. Whereas patients with OCD reported more obsessional thoughts than patients with OCD, patients with GAD did not report more perseverative worry than patients with OCD. Previous studies have found that worry, in addition to obsessional thoughts, provided significant differentiation between these patient groups (Brown et al., 1992; Brown et al., 1993), yet it has also been found that obsessional thoughts discriminate between these groups better than perseverative worry, in line with the present findings (Brown et al., 1993).
Although patients with GAD and OCD were not distinguished by levels of perseverative worry, they were distinguished by relations between perseverative worry and attentional control. The present study found evidence of diminished attentional control in patients with GAD and OCD compared to controls, suggesting that both disorders indeed involve deficits in executive control of attention; however, only in patients with GAD were attentional control deficits associated with perseverative worry. As predicted, deficits in both focusing and shifting attention were specifically associated with increased perseverative worry in GAD. In contrast, attentional control deficits were not associated with increased obsessional thoughts or perseverative worry in OCD patients. Although patients with OCD and GAD showed elevated levels of rumination compared to the NCC group, consistent with prior research (Fresco et al., 2002; Grisham & Williams, 2009) rumination was not associated with attentional control in either patients with OCD or GAD, suggesting that elevated levels of rumination in these disorders may not be a function of diminished attentional control. One possibility is that elevated levels of rumination in OCD and GAD, as observed in the present study relative to NCC participants, may be the result of co-morbid depressionor negative affect, as opposed to a general cognitive diathesis.
The association between deficits in attentional control and perseverative worry observed in the GAD group is consistent with a growing body of research implicating attentional control in anxiety disorders. Deficits in attentional control observed in self-report (Moriya & Tanno, 2008), behavioral (Pacheco-Unguetti et al., 2010), and neural (Telzer et al., 2008) responding have been linked to anxiety disorder symptoms. Research on attention modification in anxiety disorders suggests that this association could reflect a causal influence of attentional control on symptoms of anxiety. In particular, Browning et al. (2009) found that training attention away from threat, which has been found to reduce symptoms of GAD (Amir, Beard, Burns, & Bomyea, 2009), appeared to occur through alterations in brain regions underlying attentional control (e.g., lateral prefrontal cortex; Bishop, Duncan, Brett, & Lawrence, 2004). While no studies have experimentally examined the causal relations between attentional control and perseverative worryper se, attention retraining has also been shown to reduce symptoms of anxiety in individuals with clinical levels of perseverative worry (Hazen, Vasey, & Schmidt, 2009).
Although there is evidence suggesting that attentional control influences anxiety-related processes related to worry, another possibility is that perseverative worry instead causes deficits in attentional control. In light of evidence that attentional control is contingent upon working memory capacity (Barrett, Tugade, & Engle, 2004), one possibility is that perseverative worry impairs attentional control through the costs of maintaining apprehensive content in working memory. Indeed, the deleterious effects of worry on attention and working memory capacity have been stressed in prominent accounts of anxiety (e.g., processing theory; Eysenck & Calvo, 1992).
Alternatively, there may be no direct relation between attentional control and worry in GAD; instead, the relation observed in the present study may be mediated by a third variable. Specifically, trait anxiety has been found to be associated with both deficits in attentional control (e.g., Bishop, 2009) and perseverative worry (e.g., Eysenck & Van Berkum, 1992).Indeed, mediational modeling of the relations between attentional control, perseverative worry, and trait anxiety suggested that diminished attentional control is associated with increased perseverative worry in GAD through the mediation of trait anxiety. The effect of attentional control on trait anxiety may be understood in the context of theory and research suggesting that attentional control is critical to emotion regulation, including the regulation of anxiety (Derryberry & Rothbart, 1988, Lonigan & Phillips, 2001). For example, Lonigan and Phillips (2001) propose that deficits in attentional control may undermine disengagement from distressing stimuli and situations, leading to increased frequency and intensity of anxiety. In turn, elevated trait anxiety may increase the use of worry as a means of preparing for threat (Mathews, 1990): trait anxiety has been linked to a tendency to over estimate the likelihood of harmful outcomes (Tomarken, Mineka, & Cook, 1989), and individuals with GAD have been found to hold positive beliefs about worry as a coping strategy for dealing with future threats (Borkovec, Hazlett-Stevens, & Diaz, 1999).
The independence of obsessional thoughts and attentional control in OCD observed in this study may suggest that obsessive thoughts in OCD are not related to the same inhibitory deficits involved in GAD-related worry. Some have suggested that obsessional thoughts derive from dysfunction in habit formation, as individuals with OCD show abnormalities in basal ganglia function that is thought to underlie the development of both routinized cognitive and behavioral patterns (Graybiel & Rauch, 2000). Indeed, if obsessional thoughts are developed and maintained in the same manner as other habits––that is, if they become fixed and automated through repetition learning––then they may not be modulated by attention, both in terms of their generation and their inhibition (Graybiel, 2008). Perseverative worry, by contrast, is thought to depend upon attention to a given concern (e.g., Mathews, 1990) and appears to be modulated by top-down cognitive control (e.g., Nitschke et al., 2009). This dynamic has not featured prominently in neurobiological accounts of obsessions (Graybiel& Rauch, 2000; Friedlander &Desrocher, 2006; Wilson, 1996), which is consistent with the present finding that deficits in attentional control are not related to increased obsessional thought in OCD.
The present findings may have implication for the treatment of GAD and OCD, in light of converging evidence that deficits in attentional control can be directly treated. As Tang and Posner (2009) note, a number of different procedures, ranging from repetitive visuo-spatial tasks to mindfulness exercises, have been shown to strengthen the executive control of attention, and there is evidence that these procedures also reduce symptoms of anxiety and depression (Tang et al., 2007). Another line of research has focused on training attention specifically in the context of anxiety disorders. These procedures, which ostensibly “reverse” attentional bias towards threat by training attention away from threat, have been found to provide lasting symptom improvement (Hakamata et al., 2010). Although the mechanisms mediating these effects are still unclear, there is some evidence that augmented attentional control may play a role. For example, Klumpp and Amir (2009) observed that symptom reductions occurred regardless of the direction of training (i.e., towards or away from threat), suggesting that improved attentional control, in addition to the attenuation of a specific bias, may mediate treatment effects.
The present findings suggest that patients with GAD may benefit not only from training attention away from threat (Amir et al., 2009), but also from more generalized attention augmentation. Indeed, inhibiting orienting toward threat may be just one context in which augmented attentional control has beneficial effects. As Tang et al. (2007) note, improved attentional control may enhance emotion regulation and thereby reduce anxiety, consistent with the proximal effects of attentional control on trait anxiety observed in the present study. However, generalized attention training may not be as effective in patients with OCD. In the present study, deficits in attentional control were not found to be related to obsessional thoughts, which are believed to be the source of distress in OCD, and in turn, the motivation for impairing compulsive behaviors. Accordingly, augmenting attentional control may not provide leverage towards alleviating distress or functional impairment in OCD. Alternatively, training attention away from a specific obsessional threat may be a more effective means of providing symptom relief in OCD (Najmi & Amir, 2010). However, not all OCD patients present with a specific obsessional threat that could provide the content for an attentional bias (Summerfeldt & Endler, 1998).
Although the present study provides novel insight into the relations between attentional control and excessive cognitions in GAD and OCD, several limitations should be considered in interpreting the findings. First, despite the use of mediational modeling, any conclusions regarding the causal relations between attentional control and perseverative worry in GAD are tentative, due to the correlational nature of the study. Examining the effects of an experimental manipulation of attentional control, such as an augmentation procedure (Tang & Posner, 2009) or a depletion procedure (e.g., prior use of top-down resources; see Muraven & Baumeister, 2000) on anxiety and perseverative worry in GAD would further elucidate the causal relations between these constructs. Second, a self-report measure of attentional control was used, as opposed to a behavioral measure of actual performance on a task requiring attentional control. Although self-report and behavioral performance measures of attention have shown evidence of convergent validity (Derryberry & Reed, 2002), the present findings require corroboration with a behavioral measure of attentional control. Future research addressing these limitations may further clarify the role of attention control in the genesis of excessive cognitions in OCD and GAD.
Footnotes
All possible mediational models of relations between attentional control, trait anxiety, and perseverative worry were tested; only the present model was supported by the data.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000. [Google Scholar]
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Healy L. An examination of the cognitive processes involved in childhood obsessive-compulsive disorder. Behaviour Research and Therapy. 2003;41:285–299. doi: 10.1016/s0005-7967(02)00011-6. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Tugade MM, Engle R. Individual differences in working memory capacity and dual-process theories of the mind. Psychological Bulletin. 2004;130:553–573. doi: 10.1037/0033-2909.130.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SJ. Trait anxiety and impoverished prefrontal control of attention. Nature Neuroscience. 2009;12:92–98. doi: 10.1038/nn.2242. [DOI] [PubMed] [Google Scholar]
- Bishop SJ, Duncan J, Brett M, Lawrence A. Prefrontal cortical function and anxiety: controlling attention to threat-related stimuli. Nature Neuroscience. 2004;7:184–8. doi: 10.1038/nn1173. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Hazlett-Stevens H, Diaz ML. The role of positive beliefs about worry in generalized anxiety disorder and its treatment. Clinical Psychology and Psychotherapy. 1999;6:126–138. [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–38. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown T, Moras K, Zinbarg R, Barlow DH. Differentiating generalized anxiety disorder and obsessive compulsive behavior. Behavior Therapy. 1993;24:227–240. [Google Scholar]
- Browning M, Holmes EA, Murphy SE, Goodwin GM, Harmer CJ. Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biological Psychiatry. 2010;67:919–25. doi: 10.1016/j.biopsych.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Keortge SG, Formea GM, Sternberger LG. Revision of the Padua Inventory of obsessive-compulsive disorder symptoms: Distinctiveness between worry, obsessions, and compulsions. Behaviour Research and Therapy. 1996;34:163–173. doi: 10.1016/0005-7967(95)00035-6. [DOI] [PubMed] [Google Scholar]
- Clark DA, Claybourn M. Process characteristics of worry and obsessive intrusive thoughts. Behaviour Research and Therapy. 1997;35:1139–1141. [PubMed] [Google Scholar]
- Davey GCL. Worrying, social problem solving abilities, and problem-solving confidence. Behaviour Research and Therapy. 1994;32:327–33. doi: 10.1016/0005-7967(94)90130-9. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology. 2002;2:225–23. doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Rothbart MK. Affect, arousal, and attention as components of temperament. Journal of Personality and Social Psychology. 1988;55:958–966. doi: 10.1037//0022-3514.55.6.958. [DOI] [PubMed] [Google Scholar]
- Eysenck MW, Calvo MG. Anxiety and performance: The processing efficiency theory. Cognition and Emotion. 1992;6:409–434. [Google Scholar]
- Eysenck MW, Van Berkum JJA. Trait anxiety, defensiveness, and the structure of worry. Personality and Individual Differences. 1992;13:1285–1290. [Google Scholar]
- Fineberg NA, Fourie H, Gale TM, Sivakumaran T. Comorbid depression in obsessive compulsive disorder (OCD): Symptomatic differences to major depressive disorder. Journal of Affective Disorders. 2005;87:327–330. doi: 10.1016/j.jad.2005.04.004. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, research version, patient edition (SCID-I/P) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive–Compulsive Inventory: Development and validation of a short version. Psychological Assessment. 2002;14:485–496. [PubMed] [Google Scholar]
- Freeston MH, Ladouceur R, Rheaume J, Letarte H, Gagnon F, Thibodeau N. Self-report of obsessions and worry. Behaviour Research and Therapy. 1994;32:29–36. doi: 10.1016/0005-7967(94)90081-7. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Frankel A, Mennin DS, Turk CL, Heimberg RG. Distinct and overlapping features of rumination and worry: The relationship of cognitive production to negative affective states. Cognitive Therapy and Research. 2002;26:179–188. [Google Scholar]
- Friedlander L, Desrocher ME. Neuroimaging Studies of Obsessive-Compulsive Disorder in Adults and Children. Clinical Psychology Review. 2006;26:32–49. doi: 10.1016/j.cpr.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown obsessive compulsive scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Graybiel AM. Habits, rituals, and the evaluative brain. Annual Review of Neuroscience. 2008;31:359–87. doi: 10.1146/annurev.neuro.29.051605.112851. [DOI] [PubMed] [Google Scholar]
- Graybiel AM, Rauch SL. Toward a neurobiology of obsessive-compulsive disorder. Neuron. 2000;28:343–347. doi: 10.1016/s0896-6273(00)00113-6. [DOI] [PubMed] [Google Scholar]
- Grisham JR, Williams AD. Cognitive control of obsessional thoughts. Behaviour Research and Therapy. 2009;47:395–402. doi: 10.1016/j.brat.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, et al. Attention bias modification treatment: A meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazen RA, Vasey MW, Schmidt NB. Attentional retraining: A randomized clinical trial for pathological worry. Journal of Psychiatric Research. 2009;43:627–633. doi: 10.1016/j.jpsychires.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Jazbec S, McClure E, Hardin M, Pine DS, Ernst M. Cognitive control under contingencies in anxious and depressed adolescents: an antisaccade task. Biological Psychiatry. 2005;58:632–639. doi: 10.1016/j.biopsych.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Klumpp H, Amir H. Preliminary Study of Attention Training to Threat and Neutral Faces on Anxious Reactivity to a Social Stressor in Social Anxiety. Cognitive Therapy and Research. 2010;34:263–271. [Google Scholar]
- Lee HJ, Telch MJ. Autogenous/reactive obsessions and their relationship with OCD symptoms and schizotypal personality features. Journal of Anxiety Disorders. 2005;19:793–805. doi: 10.1016/j.janxdis.2004.10.001. [DOI] [PubMed] [Google Scholar]
- Levens SM, Muhtadie L, Gotlib IH. Impaired resource allocation and rumination in depression. Journal of Abnormal Psychology. 2009;118:757–766. doi: 10.1037/a0017206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology and Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM. Temperamental basis of anxiety disorders in children. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. New York: Oxford University Press; 2001. pp. 60–91. [Google Scholar]
- Mathews A. Why worry? The cognitive function of anxiety. Behaviour Research and Therapy. 1990;28:455–468. doi: 10.1016/0005-7967(90)90132-3. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Moriya J, Tanno Y. Relationships between negative emotionality and attentional control in effortful control. Personality and Individual Differences. 2008;44:1348–1355. [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin. 2000;126:247–259. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Muris P, Roelofs J, Rassin E, Franken I, Mayer B. Mediating effects of rumination and worry on the links between neuroticism, anxiety and depression. Personality and Individual Differences. 2005;39:1105–1111. [Google Scholar]
- Najmi S, Amir N. The effect of attention training on a behavioral test of contamination fears in individuals with subclinical obsessive-compulsive symptoms. Journal of Abnormal Psychology. 2010;119:136–142. doi: 10.1037/a0017549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Cashman L. The reliability and validity of the GAD-Q-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy. 2002;33:215–233. [Google Scholar]
- Nitschke JB, Sarinopoulos I, Oathes DJ, Johnstone T, Whalen PJ, Davidson RJ, et al. Anticipatory activation in the amygdala and anterior cingulate in generalized anxiety disorder and prediction of treatment response. American Journal of Psychiatry. 2009;166:302–310. doi: 10.1176/appi.ajp.2008.07101682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Olatunji BM, Schottenbauer MA, Rodriguez BF, Glass CR, Arnkoff DB. The structure of worry: Relations between positive/negative predispositions and the Penn State Worry Questionnaire. Journal of Anxiety Disorders. 2007;21:540–553. doi: 10.1016/j.janxdis.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Pacheco-Unguetti A, Acosta A, Callejas A, Lupianez J. Attention and Anxiety: Different Attentional Functioning Under State and Trait Anxiety. Psychological Science. 2010;30:1–25. doi: 10.1177/0956797609359624. [DOI] [PubMed] [Google Scholar]
- Posner MI, Rothbart MK. Research on attention networks as a model for the integration of psychological science. Annual Review of Psychology. 2007;58:1–2. doi: 10.1146/annurev.psych.58.110405.085516. [DOI] [PubMed] [Google Scholar]
- Rector NA, Antony MM, Laposa JM, Kocovski NL, Swinson RP. Assessing content domains of repetitive though in the anxiety spectrum: Rumination and worry in nonclinical and clinically anxious samples. International Journal of Cognitive Therapy. 2008;1:352–376. [Google Scholar]
- Rosen VM, Engle RW. Working memory capacity and suppression. Journal of Memory and Language. 1998;39:418–436. [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Vol. 1982. Washington DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press, Inc.; 1983. [Google Scholar]
- Summerfeldt LJ, Endler NS. Examining the evidence for anxiety related cognitive biases in obsessive–compulsive disorder. Journal of Anxiety Disorders. 1998;12:579–598. doi: 10.1016/s0887-6185(98)00035-8. [DOI] [PubMed] [Google Scholar]
- Tang Y, Ma Y, Wang J, Fan Y, Feng S, Lu Q, et al. Short-term meditation training improves attention and self-regulation. Proceedings of the National Academy of Sciences. 2007;104:17152–17156. doi: 10.1073/pnas.0707678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y, Posner MI. Attention training and attention state training. Trends in Cognitive Science. 2009;13:222–227. doi: 10.1016/j.tics.2009.01.009. [DOI] [PubMed] [Google Scholar]
- Telzer EH, Mogg K, Bradley BP, Mai X, Ernst M, Pine DS, et al. Relationship between trait anxiety, prefrontal cortex, and attention bias to angry faces in children and adolescents. Biological Psychology. 2008;79:216–22. doi: 10.1016/j.biopsycho.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomarken AJ, Mineka S, Cook M. Fear-relevant selective associations and covariation bias. Journal of Abnormal Psychology. 1989;98:381–394. doi: 10.1037//0021-843x.98.4.381. [DOI] [PubMed] [Google Scholar]
- Trapnell PD, Campbell JD. Private self-consciousness and the five factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76:284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- Wilson KD. Issues surrounding the cognitive neuroscience of obsessive-compulsive disorder. Psychonomic Bulletin & Review. 1998;5:161–172. [Google Scholar]
- Zinbarg R, Barlow DH. The structure of anxiety and the DSM-III-R anxiety disorders: A hierarchical model. Journal of Abnormal Psychology. 1996;105:181–193. doi: 10.1037//0021-843x.105.2.181. [DOI] [PubMed] [Google Scholar]