Abstract
The endoscopic sinus surgeons must have a detailed knowledge of inconsistent location of maxillary sinus openings in any interventional maxillary sinus surgeries as it relates to the orbital floor, ethmoid infundibulum and the nasolacrimal duct. Forty cadaver head and neck specimens had been cut sagittally through the nose, such that the lateral nasal wall had been preserved. The findings were documented with an emphasis on location of the maxillary sinus openings. In the present study maxillary sinus ostium opened more commonly into posterior third of the hiatus semilunaris. Accessory maxillary ostium was another variation seen in nearly three-fourths of the cases which opened into membranous meatus inferior to the uncinate process.
Keywords: Accessory maxillary ostium, Maxillary os, Maxillary sinus, Ostiomeatal unit
Introduction
Evolution is a gradual process by which man attained erect posture where by the principal or main maxillary ostium (PMO) came to be located at a higher level. Consequently drainage was no longer due to gravity. This factor along with the impendence to mucociliary action of the lining mucosa is the leading cause in the obstruction of the ostium which opens at the hiatus semilunaris. Maxillary sinusitis is therefore the demerited gift of erect posture [1].
The ostium of the maxillary sinus is on the highest part of the medial wall of the sinus and is therefore poorly placed from the point of view of free drainage; in addition it does not open directly into the nasal fossa but into the narrow ethmoidal infundibulum, inflammation of which can further interfere with drainage [2].
A critical area for Functional Endoscopic Sinus Surgery (FESS) is the ostiomeatal unit. The multiple airways that compromise it are divided into five passages. Of the five, the first three passages are responsible for draining the maxillary sinuses. The first, the maxillary ostium, is located on the superomedial aspect of the maxillary sinus. The ostium leads into the second passage, the ethmoid infundibulum, that conducts mucus from the maxillary sinus into the middle meatus via the third passage, the hiatus semilunaris. Obstruction of any of these interconnected passages results in disease of the maxillary sinus. The stagnation of secretion that may then become infected or perpetuate infection [3].
The surgical interventions of the functional endoscopic sinus surgery are designed to remove the blockage and to restore normal sinus ventilation and mucociliary function.
Materials and Methods
Forty bisected halves of the formalin fixed adult human head and neck specimens were procured from the Department of Anatomy. The anterior part of the skull was divided in the midline and then entire nasal septum was removed piecemeal taking care not to damage the ostiomeatal components. Middle concha was trimmed to view the relationship of structures within the middle meatus. The specimens were washed in normal saline. Then yellow coloured probes were used to locate the sinus ostium.
Results
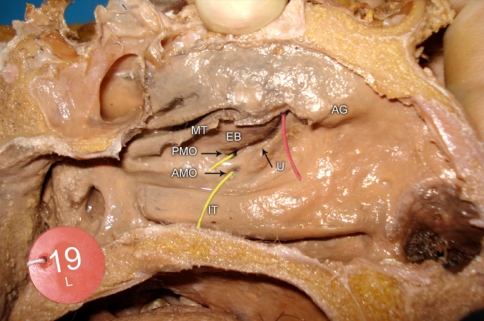
The primary maxillary ostium (Fig. 1) was found at the junction of the medial maxillary wall and the floor of the orbit, halfway between the anterior and posterior maxillary walls. The ostium was shaped like an oval or slit and was oriented horizontally or obliquely.
Fig. 1.
Sagittal section showing the primary maxillary ostium (PMO) (AG agger nasi, MT middle turbinate, EB ethmoid bulla, IT inferior turbinate, AMO accessory maxillary ostium)
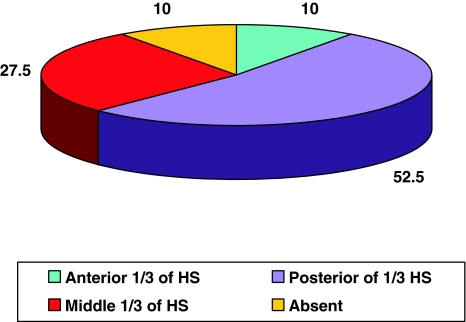
The position of the maxillary sinus ostium in 40 dissected specimens was as follows: The anterior 1/3 of hiatus semilunaris in 4 (10%), posterior 1/3 of hiatus semilunaris in 21 (52.5%), middle 1/3 of hiatus semilunaris in 11 (27.5%) and absent in 4 (10%). Statistical comparison of right and left side, male and female showed P value of 0.98 and 0.33, respectively; neither of the values were statistically significant. Accessory maxillary ostia (Fig. 2) were noted in 9 (22.5%) cases and absent in 31 (77.5%) cases (Table 1, Graph 1).
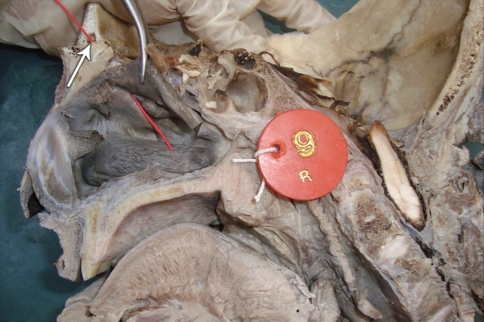
Fig. 2.
Sagittal section showing absent maxillary sinus ostium with frontal Sinus hypoplasia (arrowed)
Table 1.
Location Of The Maxillary Sinus Ostium
| Position | Male | Female | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Total | Right | Left | Total | Right | Left | Total | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Anterior 1/3 of HS | 2 (16.7) | 2 (16.7) | 4 (16.7) | – | – | – | 2 (10) | 2 (10) | 4 (10) |
| Posterior 1/3 HS | 5 (41.7) | 6 (50) | 11 (45.8) | 5 (62.5) | 5 (62.5) | 10 (62.5) | 10 (50) | 11 (55) | 21 (52.5) |
| Middle 1/3 HS | 4 (33.3) | 3 (25.0) | 7 (29.2) | 2 (25.0) | 2 (25.0) | 4 (25.0) | 6 (30) | 5 (25) | 11 (27.5) |
| Absent | 1 (8.3) | 1 (8.3) | 2 (8.3) | 1 (12.5) | 1 (12.5) | 2 (12.5) | 2 (10) | 2 (10) | 4 (10) |
| Total | 12 | 12 | 24 | 8 | 8 | 16 | 20 | 20 | 40 |
Graph 1.
Location of the maxillary sinus ostium
Discussion
Maxillary sinus begins as an outpouching of the nasal mucosa within the ethmoid infundibulum at 60–70 days of embryonic development. The primary maxillary sinus ostium represents this point of evagination [4].
The primary maxillary ostium may be found at any point along the course of the ethmoid infundibulum. In the present study, the ostium of the maxillary sinus was more commonly found to open into the posterior third of the infundibulum in 21 (52.5%) specimens, while it opened into the middle third in 11 (27.5%), anterior third in 4 (10%) and was absent in 4 (10%) specimens. Van Alyea reported similar observations and found the opening of maxillary ostium into the anterior third of the uncinate groove in 9 (5.53%), to the middle third in 18 (11.04%), to the posterior third in 117 (71.8%) and to the extreme posterior tip of the groove in 19 (11.65%) cases. Rosenberger has stated that maxillary ostium opens into the posterior third in 70% cases. Thus maxillary ostium commonly opens into the posterior third of the uncinate groove [2].
Myerson recognized that the ostium of the maxillary sinus is located immediately below the orbital floor, and thus below the lamina papyracea in the posterior part of the infundibulum, and that perforating the lateral wall of the infundibulum superior to the ostium violates the orbit. Hence the sinus surgeon must have a thorough knowledge of the relevant anatomic relationship to avoid injury to the orbit. Blind probing or nibbling with the forceps may lead to higher incidence of orbital complications [5].
A possible mechanism of formation of accessory ostia is obstruction of the primary ostium by maxillary sinusitis or due to anatomic and pathologic factors in the middle meatus resulting in the rupture of membranous areas known as fontanelle [1].
The incidence of accessory maxillary ostium (AMO) has been recorded to range from 0 to 43%. In the present study, accessory maxillary ostia were found within the membranous fontanelle of the lateral nasal wall in 9 (22.5%) specimens. Similar observations were earlier noted by Myerson in 30.7%, Schaffer in 41% and Van Alyea in 23% of specimens. Though most authors have not specified the location of the AMO with reference to the fontanelle, Stammberger and Kennedy reported their presence either in the ANF or PNF. May et al. however found their presence restricted to the PNF posteroinferior to natural ostia [1].
Van Alyea published his observations from the anatomic study of the surgical accessibility of the “ostium maxillare” in 163 specimens. He found that the natural ostia were easily accessible in 40% of specimens, but that in 20% the ostia could not be cannulated because of the anatomic configuration of the uncinate process or the bulla or the size of the ostia. In the remainder of the specimens, cannulation was only possible because of the skull, experience of the surgeon, or because an accessory ostium was present [6].
Clinically the AMO may be utilized in such cases by the endoscopic sinus surgeon to irrigate the maxillary sinus. Apart from the ostia the fontanelles may be used to create alternative passage which re-establishes ventilation and drainage during therapy of maxillary sinusitis [7].
Conclusion
The anatomy of the maxillary ostia should be well understood by an endoscopic sinus surgeon in order to perform the middle meatal antrostomy. Once located, the natural ostium can be widened posteriorly and anteriorly so that it communicates with the fontanelles to the extent permitted by any disease or stenosis that may be present. Furthermore, overzealous removal of bone anterior to the natural ostium may result in injury to the nasolacrimal duct and more superior extension accounts for a high rate of orbital complications. However, enlarging the accessory ostium or opening the membranous fontanelle may provide maxillary sinus aeration if the natural ostium is obstructed.
References
- 1.Kumar H, Choudhry R, Kakar S. Accessory maxillary ostia : topography and clinical application. J Anat Soc India. 2001;50(1):3–5. [Google Scholar]
- 2.Hollinshed WH, Rosse C. Text book of Anatomy. 4. Philadelphia: Herper and Row; 1985. pp. 976–985. [Google Scholar]
- 3.Sarna A, Hayman LA, Laine FJ, Taber KH. Coronal imaging of the ostiomeatal unit : anatomy of 24 variants. J Comput Assist Tomogr. 2002;26(1):153–157. doi: 10.1097/00004728-200201000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Anon JB, Rontal M, Zinreich SJ. Anatomy of the paranasal sinuses. New York: Thieme Medical Publishers; 1996. pp. 3–41. [Google Scholar]
- 5.May M, Sobol SM, Korzee K. The location of the maxillary os and its importance to the endoscopic sinus surgeon. Laryngoscope. 1990;100:1037–1042. doi: 10.1288/00005537-199010000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Alyea OE. The ostium maxillare. Anatomic study of its surgical accessibility. Arch Otolaryngol. 1936;24:553–569. [Google Scholar]
- 7.Levine HL, Mark M, Rontal M, Rontal E. Complex anatomy of lateral nasal wall simplified for endoscopic surgeon. Endoscopic sinus surgery. New York: Thieme Medical Publishers; 1993. pp. 1–28. [Google Scholar]