Summary
Intussusceptions is the telescoping or invagination of a portion of intestine (intussusceptum) into an adjacent segment (intussuscipiens). It is one of the common causes of bowel obstruction in infants and toddlers.
Sonography has now been accepted as a method for guiding hydrostatic reduction of intussusception with tap water, normal saline or Ringer's lactate solution. This method is currently being used at Korle Bu Teaching Hospital. It is a very simple, efficient, economical and quick method of managing intussusception. The duration of the procedure ranges between two minutes and thirty minutes, with the majority being under ten minutes. A total of twenty intussusceptions were managed in eighteen patients over a nine month period. In fifteen patients (75%) the intussusception was reduced successfully. In five patients (25%), the procedure failed to reduce the intussusceptions.
Keywords: Intussusception, Intussuscetum, Intussuscepiens, hydrostatic reduction, Intestinal obstruction
Introduction
Intussusception is the telescoping or invagination of a portion of intestine (intussusceptum) into an adjacent segment (intussuscipiens). It is one of the common causes of bowel obstruction in infants and toddlers.1,2,3,4 Though intussusception was first described by Barbette in 16741, it took over three centuries before its sonographic features were described in 19775Many researchers have since used ultrasound to diagnose this condition with a high specificity and sensitivity of nearly 100%.3In 1982, Kim and his group did the first ultrasound guided hydrostatic reduction (USGHR) with normal saline.3 Sonography has now been accepted as a method for guiding hydrostatic reduction of intussusception with tap water, normal saline or Ringer's lactate solution.2,5 USGHR of intussusception has several advantages (Box 1).
Despite these enormous benefits, USGHR of intussusception had not been a common part of the management of intussusception in the Korle-Bu Teaching Hospital in the period before March 2008. In this period, the main management was surgery. As a result of very good interdepartmental collaboration between the paediatric surgery and the radiology departments from the middle of 2007. Currently, most children who present with a clinical suspicion of intussusception and do not fall within the exclusion criteria mentioned below are likely to have a trial of either pneumatic reduction or ultrasound guided hydrostatic reduction. It is only when this has failed that surgical management is done.
This has so far been a success, reducing drastically the number of children taken to theatre for intussusception reduction. This study presents initial findings of USGHR of intussusception at Korle Bu Teaching Hospital.
Box 1 Some advantages of USGHR.
It is relatively simple, effective, economical and quick.2
Associated with less morbidity and shorter hospital stay.2
It can trace the change of the mass closely; both on transverse and longitudinal scans and can provide a clear echogram, thus definite criteria of reduction can be obtained.3
Ileo-ileo-colic intussusception can be diagnosed during reduction.3
One can easily assess changes in the child's general condition, including breathing and abdominal distension.3
Intestinal perforation during reduction can be accurately and promptly recognised.3
In cases where partial reduction is achieved, the operating time is markedly reduced.
Recurrence can be treated by the same method.2
Materials and Methods
Patients who presented at the Child Health Department of the Korle Bu Teaching Hospital from March to December 2008 with a clinical suspicion of intussusception were recruited if the following criteria were met:
Symptoms less than 4 days old,
No significant abdominal distension or signs of peritonitis.
Intussusceptum should not have prolapsed out of the rectum.
The procedure was explained to the parents and an informed consent obtained. The patient was adequately resuscitated and a nasogastric tube was passed. In addition, intravenous cefuroxime and metronidazole were given and all the other preparations necessary for surgery were made as a safeguard in case surgery became necessary in the event of failed reduction or a complication arising during the reduction. The patient was then taken to the Radiology Department for radiological examination.
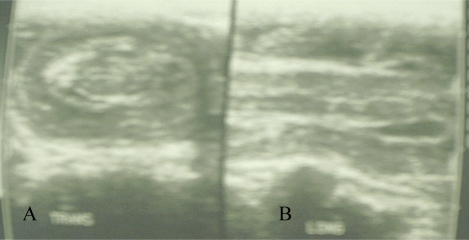
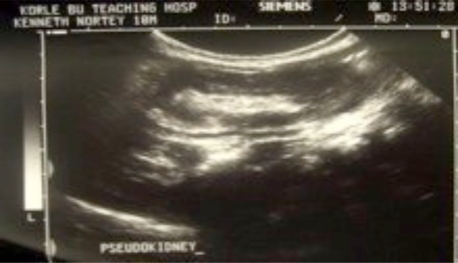
An initial abdominal ultrasound scan was done with a linear 8.5MHz probe of a Siemens Sonoline Adara machine to confirm the diagnosis (Figures 1 and 2).
Figure1.
Ultrasound features of intussusception. A. Target Sign B. Sandwich Sign
Figure 2.
Psuedo-kidney sign of intussusception on ultrasound
The child was sedated with 1–2mg/Kg of Ketamine hydrochloride. An enema bag with a rectal tube fitted was then filled with warm normal saline and hung on a drip stand at an initial height of 100cm above the couch. This height may be increased gradually to 130cm depending on how difficult it was to reduce the mass.
The rectal tube was inserted into the rectum, the balloon inflated and the normal saline (1 litre) allowed to flow into the colon. The ultrasound machine was then used to guide the reduction (Figure 3) till the mass went beyond the ileocaecal valve.
Figure 3.
Ultrasound image of the interface between intussusceptum and water during reduction
The intussusception was only said to have reduced if the following criteria were met:
Disappearance of the intussusceptum.
Visualisation of reflux of fluid and air bubbles through the caecum and ascending colon into the ileum through the ileocaecal valve
Demonstration of fluid distended ileum and
Absence of intussusceptum noted during the postevacuation ultrasound examination.
Once complete reduction was achieved, the fluid was evacuated from the colon by connecting a drainage bag to the rectal tube and allowing the fluid to drain under gravity. The abdomen was then re-examined to determine whether there was any residual lesion or recurrence of intussusception.The procedure was abandoned if the intussusceptum failed to reduce/move after three attempts, each lasting about 3 minutes. After successful reduction, the patient was admitted to the ward and discharged only when he/she tolerated a regular diet and had normal bowel movement which on the average took two days. Partially reduced cases of intussusceptions and those that failed to or had complications were managed surgically.
Results
A total of twenty intussusceptions were managed in eighteen patients in this study. There were five females and thirteen males, giving a ratio of 1:2.6.
The ages of the patients ranged between two months and forty-one months. The mean age was 11.7 months and a standard deviation of 2.6 months. Eight patients (40%) were between ages seven and twelve months, followed by seven (35%) patients aged zero to six months, two patients (10%) each aged between 13 to 18 and 19 to 24 months and one patient aged more than 24 months.
Two of the children had recurrent intussusception. One occured a day after the procedure and the other was three and half months later. In eight of the patients (40%) the intussusception was seen at the transverse colon, five patients (25%) at the descending colon, four patients (20%) at the hepatic flexure, two patients (20%) at the sigmoid colon and only one patient(5.9%) had the intussusception in the ascending colon. The duration of the procedure ranged between two minutes and thirty minutes, with majority being under ten minutes from when the normal saline was released. Seventy-five percent of the intussusception cases were reduced successfully.
In five patients (25%), USGHR of intussusception failed. Of these five patients two had bowel perforation during the procedure which was seen at surgery to be due to gangrene of bowel while onehad ischaemia of bowel; all three patients required bowel resection and anastomosis. For the remaining two, one had inflamed payer's patches and the other had inflamed payers patches as well as ileo-ileo-colic intussusception. In two of these patients the intussusception was at the transverse colon. The remaining three were in the hepatic flexure, sigmoid colon and descending colon.
Discussion
Intussusception is a common emergency in infants and children.2,4,5,7 It is commoner in males than females. In this study the ratio was 2.6:1 which compares with other studies.1,4,5The commonest site of intussusception was the transverse colon which was also the case the study of Sarin et al in 1999.3
However, when we consider the lesions that occurred in the other parts of the colon, we saw more lesions in the descending and sigmoid colon compared to Sarin et al which showed more lesions in the caecum and ascending colon.3 This difference could have been due to the delay in arrival of our patients. This is because with time the intussusceptum would move from the right side of the colon to the left. Korle Bu Teaching Hospital is a referral centre thus it only when the doctor at the clinic or polyclinic makes the diagnosis would he would refer to us, hence the delay.
There was no case of colo-colic intussusception, only one case of ileo-ileo-colic and all the others were ileocolic and this compares with other studies.3
Surgery is a sure way of managing both the intussusception and the complications that may be associated with it.1 It is however a long and arduous process of getting the child to theatre, getting an anaesthetist, a recovery ward and longer post-operative stay in hospital not to mention the adhesions the patient may develop later in life. Unfortunatelythe chances of recurrence following surgery are no better than non-operative management. Ultrasound guided hydrostatic reduction is a relatively simple procedure, which does not need an anaesthetist and the other requirements for surgical intervention. It is associated with less morbidity and patients have a relatively shorter hospital stay.2
In this study there were two cases of recurrent intussusception. One was a day after successful reduction of intussusception using USGHR which was successfully reduced for the second time. In the other patient, USGHR failed to reduce the intussusception the first time so the child had surgical reduction. At surgery it was noted that the intussusception was the ileo-ileo-colic type which is usually difficult to reduce by USGHR. Three and half months later he presented with a recurrence which was ileo-colic and was successfully reduced with USGHR. Only two out of eighteen patients had complications, which were bowel perforation. Both patients had ischaemic bowel which predisposed them to perforation.
Another type of non-operative management of intussusception is pneumatic reduction. Advocates of pneumatic reduction claim that if perforation occurs it causes less morbidity than USGHR which causes significant peritoneal soiling following perforation. However the advantages of using air for treatment of intussusception have been questioned recently, with the most serious charge being a greater risk of perforation and the possibility of developing a tension pneumoperitoneum.3,5
It is worth noting that majority of the intussusceptions would reduce within ten minutes of starting the flow of the normal saline making it a relatively short procedure compared with surgery which takes not less than forty-five minutes. This is a significant positive finding weighting initial management of intussusception in favour of USGHR. Finally the relatively high success rate of 75% which compares with other studies1,2,3,4,6 is encouraging to use USGHR as the primary management option, failing which surgery can be used.
Conclusion
USGHR is a very simple, effective, economical and quick method of managing intussusception. It has a high success rate especially when patients are carefully selected and associated acceptable complications both short and long term. It is therefore prudent to consider it as the primary modality of intussusception management in Ghana.
References
- 1.Irish M S. Intussusception: Surgical Perspective. Emedicine. 2006 Jul [Google Scholar]
- 2.Krishnakumar, Hameed S, Umamaheshwari Ultrasound Guided Hydrostatic Reduction in the Management of Intussusception. Indian J Pediatr. 2006;73(3):217–220. doi: 10.1007/BF02825484. [DOI] [PubMed] [Google Scholar]
- 3.Sarin Y K, Rao J S, Stephen E. Ultrasound guided water enema for hydrostatic reduction of childhood intussusception - a preliminary experience. Gastrointestinal Radiology. 1999;9(2):59–63. [Google Scholar]
- 4.Crystal P, Barki Y. Using Color Doppler Sonography-Guided Reduction of Intussusception to Differentiate Edematous Ileocecal Valve and Residual Intussusception. AJR. 2004;182:1345. doi: 10.2214/ajr.182.5.1821345. [DOI] [PubMed] [Google Scholar]
- 5.Peh W C G, Khong P L, Chan K L, Lam C, Cheng W, Lami W W M, Mya G H, Saing H, Leong L L Y, Low L C K. Sonographically Guided Hydrostatic Reduction of Childhood Intussusception Using Hartmann's Solution. AJR. 1996;167:1237–1241. doi: 10.2214/ajr.167.5.8911188. [DOI] [PubMed] [Google Scholar]
- 6.Atalabi O M, Ogundoyin OO, Ogunlana D I, Onasanya O M, Lawal A T, Olarinoye A S. Hydrostatic Reduction of Intussusception under Ultrasound Guidance: An Initial Experience in a Developing Country. African J Paed Surg. 2007;4(2):68–71. [Google Scholar]
- 7.Van den Ende E D, Allema J H, Hazebroek F W J, Breslau P J. Success with hydrostatic reduction of intussusception in relation to duration of symptoms. Arch Dis Child. 2005;90:1071–1072. doi: 10.1136/adc.2004.066332. [DOI] [PMC free article] [PubMed] [Google Scholar]