Summary
Vulvar lipoma is said to be so rare that only a few cases have been reported. We present two cases of vulvar lipoma that were diagnosed within six months in our centre in a 28 year-old para 2 and 35 year-old para 1 woman both of whom presented with slow-growing masses in the vulva. A detailed discussion of the clinical features and current management options are outlined, with emphasis on the need to subject all excised lesions to histopathological evaluation; to ensure accurate diagnosis and differentiate this benign swelling from cystic swellings and malignant neoplasms in the vulva.
Keywords: Vulva, lipoma, benign neoplasm, surgical excision
Introduction
Lipomas constitute the most common soft tissue tumors.1,2 They are widely disseminated benign mesenchymal neoplasms commonly found over the nape of the neck and upper back, shoulders, abdomen, buttocks, and proximal portions of the extremities.1,2 Their occurrence in the vulva is said to be so rare that only a few cases have been reported.1–4 However within a period of six months two cases in adults were detected in our centre. We present these cases, discuss the clinical features and current management options available for this vulvar pathology, and emphasise the need for histopathological evaluation of all excised lesions, where facilities allow.
Case Reports
Case 1: A 28-year-old para 2 presented to our department with a painless and slow-growing right vulvar mass of six months duration. She felt uncomfortable anytime she wore tight-fitting underwear. Physical examination revealed a single, soft, non-tender, and doughy mass in the right labium majus that measured about seven by five centimetres (cm) in its widest dimensions.
Case 2: A 35-year-old para1 woman was referred to our centre with a slow-growing left vulvar mass of a year's duration. Examination revealed a pedunculated, soft, non-tender and non-fluctuant vulvar mass located on the upper two-thirds of the left labium majus, measuring about ten by seven cm and covering the entire introitus of the vagina (Figure 1); the urethral orifice appeared normal.
Figure 1.
Soft mass on left labium majus
Both cases had no prior history of vulvar trauma or discharge from the masses. Their medical, obstetric and gynaecological histories were unremarkable. The overlying skin was freely mobile over each mass. There were no visible or palpable cough impulse or inguinal lymphadenopathy, and bimanual pelvic examinations were normal. A tentative diagnosis of vulvar lipoma was made in each case. Their laboratory investigations were unremarkable and they were prepared for surgical excision.
The masses were completely excised under general anaesthesia. The postoperative recoveries of both patients were uneventful.
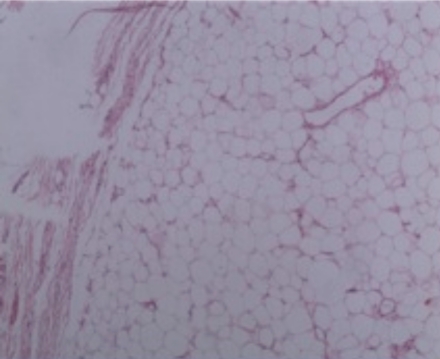
Cut sections of the tumours showed lobulated yellow tissue without haemorrhage or necrosis. Microscopic examination revealed circumscribed benign tumours composed of mature adipocytes (Figure 2) confirming the diagnosis of vulvar lipoma.
Figure 2.
Sections of tumour showing mature adipocytes with part of its capsule on the left (H&E x 4)
Discussion
Benign tumours of the vulva are usually classified according to their origin as epithelial or mesenchymal cell tumors.2 Vulvar lipomas are rare benign mesenchymal tumours consisting of mature fat cells, often interspersed with strands of fibrous connective tissue.2,4 Arising from the vulvar fatty pads, they present as soft, multiloculated subcutaneous neoplasms.4 They have been identified in various age groups ranging from infancy to the ninth decade.1–4 Though their precise aetiology and pathogenesis remain unclear, trauma has been implicated in some cases.2,5 Our patients were in their third and fourth decades of life respectively and neither had a previous history of trauma.
Lipomas usually present as single or multiple slowly growing, painless and mobile soft tissue swelling with a characteristic doughy feel. They appear as ill-defined, well-demarcated, or pedunculated masses that are nonadherent to the overlying skin.1,3–6 Consequently, they can be diagnosed correctly in most cases by clinical examination alone.3,5,6 Our patients presented as well-defined and pedunculated soft non-tender vulvar masses that were both diagnosed clinically. Clinically, vulvar lipomas must be differentiated from cystic swellings of the Bartholin's gland and the canal of Nuck1,3; they may be misdiagnosed as inguinal hernias especially in children.3 Like other lipomas, vulvar lipomas generally have a benign course. If left untreated, they may attain a remarkable size.1
Where the clinical diagnosis is not apparent, ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) are useful in differentiating vulvar lipomas from vulvar cysts, inguinal hernias and liposarcomas.1–4 Sonographically, vulvar lipoomas appear as nonspecific homogenous echogenic masses with lobular structures consistent with fat deposition.4 Since ultrasound is highly sensitive, specific and reliable4,5, where necessary in developing countries, we recommend ultrasound as the radiological investigation of choice as it is less expensive and relatively more available in such settings. CT scan and MRI are useful in evaluating the anatomical extensions of vulvar lipomas and differentiating them from liposarcomas.1–3 However, cost and availability limit their use in most developing world settings.
Histologically, they must be distinguished from well differentiated lipoma-like liposarcomas by extensive tumor sampling.1 Although nonexcisional treatments for lipomas (such as steroid injections and liposuction) have become common5,6, complete surgical excision remains the treatment of choice for vulvar lipomas.1–4 Steroid injections are best reserved for small lipomas while liposuction alone may not allow complete resection or histopathological evaluation of the tumour.5, 6
Diagnosing two cases of vulvar lipoma within six months in one centre may suggest that this condition is not as rare as the current thinking is, and emphasizes the need to subject all excised lesions to histopathological evaluation.
Conclusion
Two cases of vulvar lipoma detected within six months in adults are presented. The lipomas were removed by complete surgical excision and the diagnosis confirmed by histopatholology. Recognition of this benign vulvar swelling is important to differentiate it from cystic swellings and malignant neoplasms in the vulva.
Acknowledgement
We are grateful to the women for giving consent for their case records to be published.
References
- 1.Kehagias DT, Smyrniotis VE, Karvounis EE, Gouliamos AD, Creatsas G. Large lipoma of the vulva. Eur J Obstet Gynecol Reprod Biol. 1999 May;84(1):5–6. doi: 10.1016/s0301-2115(98)00247-4. [DOI] [PubMed] [Google Scholar]
- 2.Lee JH, Chung SM. Large vulvar lipoma in an adolescent: a case report. J Korean Med Sci. 2008 Aug;23(4):744–746. doi: 10.3346/jkms.2008.23.4.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oh JT, Choi SH, Ahn SG, Kim MJ, Yang WI, Han SJ. Vulvar lipomas in children: an analysis of 7 cases. J Pediatr Surg. 2009 Oct;44(10):1920–1923. doi: 10.1016/j.jpedsurg.2009.02.063. [DOI] [PubMed] [Google Scholar]
- 4.Sherer DM, Gorelick C, Wagreich A, Lee YC, Serur E, Zigalo A, et al. Sonographic findings of a large vulvar lipoma. Ultrasound Obstet Gynecol. 2007 Oct;30(5):786–787. doi: 10.1002/uog.5130. [DOI] [PubMed] [Google Scholar]
- 5.Aust MC, Spies M, Kall S, Gohritz A, Boorboor P, Kolokythas P, et al. Lipomas after blunt soft tissue trauma: are they real? Analysis of 31 cases. Br J Dermatol. 2007 Jul;157(1):92–99. doi: 10.1111/j.1365-2133.2007.07970.x. [DOI] [PubMed] [Google Scholar]
- 6.Salam GA. Lipoma excision. Am Fam Physician. 2002 Mar 1;65(5):901–904. [PubMed] [Google Scholar]