To the Editor:
We read with much interest the article by Loffroy et al published in the February 2009 issue of the Journal. We agree with the authors that transarterial embolization is extremely useful in treating bleeding duodenal ulcers, and that hemostasis can be expected in the majority of cases (1). Nevertheless, rebleeding after initially successful embolization, as mentioned by the authors, can occur and challenges the durability of the technique, the exact mechanism of which remains poorly understood (2). We highlight a possible mechanism with a recent case.
A 77-year-old man who underwent open cholecystectomy three months previously, presented with severe hypotension (blood pressure 70/30 mmHg) with massive hemetemesis. Endoscopy revealed a large Forrest 1a ulcer in the first part of the duodenum (D1) with active arterial spurts. Following failed attempts to secure hemostasis with endoscopic injection of vasopressin, emergent arterial embolization was performed.
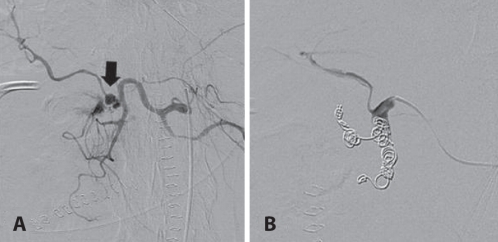
During angiography, active resuscitation was needed, including blood transfusion and continuous infusion of vasopressors (dopamine and noradrenaline). On arteriography, a large pseudoaneurysm arising from the right hepatic artery (RHA) with active extravasation was identified (Figure 1A, arrow), likely due to erosion of an ulcer into the artery. Additionally, the vasculature was noted to be small in calibre with segments of vasospasm, and the RHA measured approximately 2 mm in calibre. Super-selective coil embolization using a total of 11 microcoils (3 mm to 5 mm in diameter [VortX, Boston Scientific, Natick, USA]) achieved complete stasis in both the RHA and the gastroduodenal artery (Figure 1B), as well as hemodynamic stability.
Figure 1).
Pre-embolization celiac arteriogram. A Celiac arteriography showed a pseudoaneurysm arising from the right hepatic artery with active extravasation (arrow). In addition, the vessels are small in size with irregular dimensions due to severe vasoconstriction and vasospasm. B Postembolization arteriogram obtained during initial presentation. Stasis in the segment containing the pseudoaneurysm was achieved post microcoil embolization, using microcoils appropriately sized for the vessel dimension at the time of arteriography
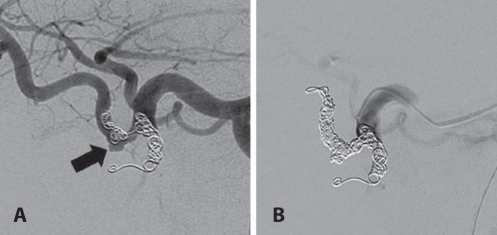
The patient was weaned off vasopressors over seven days, with restoration of hemodynamic stability. Eight days after embolization, however, repeated episodes of hemetemesis occurred with severe hypotension (blood pressure 60/30 mmHg). Urgent arteriography showed reperfusion of the embolized RHA and pseudoaneurysm (Figure 2A, arrow). Furthermore, there was a significant increase in the calibre of the RHA, which was no longer vasoconstricted, measuring 6 mm in calibre. The previously deployed coils were severely ‘undersized’ in relation to the native RHA calibre and were no longer occluding the vessel. Further superselective coil embolization using an additional 21 microcoils (4 mm to 6 mm in size) resulted in complete occlusion of the RHA (Figure 2B). The patient made an uneventful recovery and was discharged 10 days later.
Figure 2).
A Pre-embolization arteriogram. B Postembolization arteriogram obtained during second embolization following rebleed eight days later. The vasculature significantly increased in calibre following restoration of normovolemia, with the microcoils ‘undersized’ relative to the vessel. The previously occluded segment is reperfused, including the pseudoaneurysm (arrow) (A). Repeat coiling with larger coils is needed to achieved stasis and occlusion of this segment (B)
While we acknowledge that this is a single illustrative case, it raises a possible mechanism for the high failure rate associated with embolization using coils alone. First, significant vasoconstriction can occur in critically ill and hypovolemic patients, resulting in relative ‘undersizing’ of embolic coil size during the acute episode. Additionally, systemic vasopressors during resuscitation and endoscopically injected local vasopressin, a common clinical scenario, result in reduction of vessel size. Following restoration of normovolemia, reperfusion of a previously occluded vessel can then occur due to ‘re-expansion’ of vessels back to their native size.
In the literature, combining coils with particulate agents such as Gel-foam and polyvinyl alcohol particles has been shown to decrease the rate of early rebleeding (2). We believe that while coil embolization works by closing off the proximal pressure head to the bleeding site, particulate agents potentiate coil embolization by closing off the more distal vascular bed. This would potentially explain the lower rebleeding rate; because even if ‘reperfusion’ of the coil-embolized proximal segment were to occur, the additional particulate closure of the distal vascular bed would prevent rebleeding at the offending site.
REFERNCES
- 1.Holme JB, Nielsen DT, Funch-Jensen P, Mortensen FV. Transcatheter arterial embolization in patients with bleeding duodenal ulcer: An Alternative to surgery. Acta Radiol. 2006;47:244–7. doi: 10.1080/02841850600550690. [DOI] [PubMed] [Google Scholar]
- 2.Loffroy R, Guiu B, D’Athis P, et al. Arterial embolotherapy for endoscopically unmanageable acute gastroduodenal hemorrhage: Predictors of early rebleeding. Clin Gastroenterol Hepatol. 2009;7:515–23. doi: 10.1016/j.cgh.2009.02.003. [DOI] [PubMed] [Google Scholar]