Abstract
Purpose
Our previous study found it feasible for a preschooler with cerebral palsy (CP) to use a power mobility device in his classroom but noted a lack of typical socialization. The purpose of this follow-up study was to determine the feasibility of providing mobility and socialization training for this child.
Methods
Will, a 3-year-old with CP, one comparison peer, two preschool teachers, and two therapists were filmed daily during a training and post-training phase. Adult-directed training was provided in the classroom by therapists and teachers during the training phase. Mobility and socialization measures were coded from video.
Outcomes
During training, Will demonstrated higher socialization but less mobility than the comparison peer. Post training, Will socialized less but was more mobile, though less mobile than the comparison peer.
Discussion
Short-term, adult-directed power mobility and socialization training appears feasible for the preschool classroom. Important issues regarding socialization and power mobility are discussed.
Keywords: assistive devices; cerebral palsy/psychology; cerebral palsy/rehabilitation; child, preschool; humans; male; motor activity/physiology; motor skills/physiology; physical therapy modalities/instrumentation; socialization
Introduction
Independent mobility is a causal factor in development starting in early infancy.1–4 Thus children with significant mobility impairments who cannot crawl and walk independently are at risk for additional secondary, mobility-related delays.5 The effect of immobility may, in fact, increase when children become toddlers and then preschoolers, as their peers’ mobility and the use of that mobility for socialization and learning increases rapidly. Power mobility (i.e. power wheelchairs) is one option for independent mobility for children unable to walk. Although given potential positive developmental outcomes of starting power mobility in infancy,6–8 most children currently receive power mobility training starting when they are 3 to 6 years of age, if not older.9 In this case report, we continue to follow a 3 year old child, Will, who was the subject of a recent case report focused on the feasibility of using an experimental power mobility device in a preschool classroom.10 The specific focus of this follow-up report is to determine the feasibility of providing an intervention to increase the use of power mobility for his socialization in the preschool classroom.
We specifically focus in this paper on mobility and socialization training in preschool, as it is during the preschool years that complex socialization emerges11 and is thus when an immobility-related social delay may become apparent. Socialization encompasses a complex set of knowledge and behaviors.12 For this paper, we focus on the development of ‘social interaction,’ which is the reciprocal process of initiating and responding to social stimuli presented by others.13 We followed the work of Howes14 and quantified the amount of time spent in 4 categories: peer interaction and teacher interaction, which are both referred to as ‘interactive’ behaviors, as well as parallel play and solitary, which are referred to as ‘non interactive’ behaviors.
Children with mobility impairments may find the preschool classroom a particularly challenging setting to learn to fully interact with peers and teachers for several interrelated reasons. First, mobility impairments can limit a child’s ability to initiate and maintain social interactions with their highly mobile peers.5,10 Second, preschool group activities often require bouts of mobility in tight spaces such as during dramatic play or ‘sensory’ table activities, which are difficult for children with mobility impairments with or without power mobility.15 Given the tight spaces of a preschool classroom, however, noting how a child spends the majority of his non-interacting time - in parallel play (within 3 feet of another peer) or as solitary (more than 3 feet from others) – may provide more information on the extent to which the child is socially isolated. Third, children with mobility impairments may not fully use nor understand nonverbal communication, thereby creating a communication barrier.5 Lastly, by preschool years, children with mobility impairments, their families, teachers and peers may have together created a stable social system built around the immobile child.10 As a result, the child, his teachers, peers and family may be accustomed to the child playing alone for extended periods. In turn, peers may learn that immobile children do not display typical participation and avoid, if not ostracize, them.16 Ultimately, we propose that a ‘snowball effect’ may occur where the lack of full and active participation in the physical and social life inside and outside the classroom may result in these children being avoided by peers, or set up with activities and left by teachers, and the child may become content, at least in the short term, with a low level of participation. If a social impairment is not ‘caught’ and adequately addressed by the end of preschool years, the child will likely progress to kindergarten and grade school where socialization is suppressed and retrained to fit the mold of the classroom, where children are rewarded for being quiet and non-interactive for large portions of indoor time. A child without the ability to socialize at first grade may mistakenly be seen as the ‘perfect classroom student’ and it may never be recognized that this child does not possess age-typical social skills.
In a previous case report, we found it was feasible for a 3 year old child (Will) with cerebral palsy (CP) to use our small experimental power mobility device (‘UD2’, Fig. 1a) in a preschool classroom and to quantify his mobility and socialization with peers and teachers.10 Although he readily used power mobility in the gym and outdoor playground, interacted with adults who approached him, and could drive throughout the classroom, we noted a striking lack of socialization with teachers and peers coupled with less use of UD2 in the classroom. That is, he had the potential to increase his mobility to interact with others within the classroom with UD2; however, he did not.
Figure 1.
A) Will in UD2 in his preschool classroom. B) Example of interventionist engaging Will in active, one-on-one instruction. C) Example of interventionist performing supplemental, group guidance. D) Example of Will playing with his peers immediately after an interventionist left the scene.
There are several potential reasons for his lack of mobility and socialization. One reason may have been that without supportive training by teachers and therapists, Will did not have the social skills in the classroom to independently interact with peers and teachers. Although intervention focused on mobility and socialization may be available clinically to children with certain pediatric diagnoses in certain early education settings, the present case report is the first to attempt to construct and quantify a standardized ’mobility and socialization’ training protocol for a young child with CP using power mobility in the classroom. The specific purposes were 1) to determine the feasibility of providing a short term, supportive ‘mobility and socialization’ training to increase Will’s mobility and socialization within the classroom, and 2) to quantify changes in his mobility and socialization during training as compared to periods before and after training.
Description of Case
This case report describes the mobility and socialization of Will, a 3-year-old, diagnosed with spastic quadriplegic CP with an athetoid component, over a total period of 30 days. Specifically, we compare a period of 17 days (comprising a 10-day ‘training phase’ and 7-day ‘post-training phase’) to our previous case report’s 10-day ‘baseline phase’ and 13-day ‘mobility phase’ when Will received UD2 for the first time to drive in his classroom but no additional training. As noted in our previous case report, Will’s independent mobility is significantly limited without the use of power mobility. Although he has full passive range of motion in all limbs, he demonstrates spasticity and stiffness, and reduced isolation and control of gross movements. Since the age of 13 months, Will received therapy to address his delays in sitting, reaching and walking, as well as his movement impairments. His Gross Motor Function Classification System (GMFCS) level remains a III, reflecting his ability to sit independently with minimal support but his need for assistive technology to travel community distances. His GMFM-66 score at age 3 years was 40.91%, which is below average for his age and GMFCS level.17 When sitting in a standard power chair or UD2, Will has full head movement and control, adequate trunk control to play with toys and draw, and adequate bilateral grasp to manipulate a standard joystick. He also has some difficulty isolating and controlling his fine movements, such as precise movement of individual fingers needed for grasping and manipulating objects and toys. He uses utensils with modified handles to eat independently. His toddler and preschool teachers have not noted significant limitations in Will’s cognitive or language level, including his ability to understand and produce verbal communication, but he does appear to interact less with others as compared to his peers. His ability to understand nonverbal communication has not been assessed, but it is clear that he is not able to produce appropriate nonverbal communication (body language) due to his limited active range of motion of his upper extremities. Will has no known visual or auditory acuity deficits.
Will continued to drive a standard power chair (Permobil Koala, Lebanon, TN) with minimal verbal cues in the hallways, gym and outdoor playground but did not have power mobility in his home or community. Prior to the training reported in this case report, Will had been using UD2 for approximately 13 days in his classroom, which was the ‘mobility phase’ of the previous case report. Will’s parents, teachers, and the family of the comparison peer provided informed consent for participation and for use of photos as approved by the University of Delaware Institutional Review Board.
Description of Intervention
Will is enrolled in an Early Learning Center, an inclusive childcare center with 250 children in classrooms for infants through Kindergarten. Will’s preschool classroom consists of 10–15 children ages 3–4 years and 2 teachers. Will, the 2 classroom teachers, plus 1 child who is typically developing, which we term his ‘comparison peer’, were filmed each day.
Intervention Strategy
In terms of mobility training, studies training young children to drive power mobility devices have focused on general, personalized instruction of driving and obstacle avoidance versus specific training protocols.6,8,18–31 In terms of socialization training, we know of no interventions for children with mobility impairments, however a variety exist for improving social interactions for preschoolers with social impairments, particularly for children with autism. Two common modes of delivering social intervention in the classroom are adult-directed intervention, where an adult is the primary source of social modeling and teaching for the child, and peer-mediated intervention, where a typical peer is trained to be the primary influence for the child with social impairments.32
The decision of whether to use adult-directed or peer-mediated interventions and for which children is an area of active research. One view is that children with more severe social, cognitive, emotional and behavioral problems may benefit from adult-directed intervention with some component of peer partner play.16 Considering Will’s age, his low level of social interaction with peers and teachers, and the need to determine the feasibility of intervention in the classroom over a relatively short time frame, we opted for an adult-directed training strategy that included peer participation in specific activities.
Our ‘mobility and socialization’ training program was designed to increase Will’s participation in classroom activities via ‘incidental teaching’ – systematic instruction that takes place in response to the natural stimulus conditions of everyday environments.33 In other words, the adult interventionists used naturally occurring situations such as Will sitting alone, peers playing together on an activity that Will wants to join, Will having difficulty in driving to a specific area, etc., to stimulate learning opportunities in which the adult interventionist could teach appropriate behaviors. Our incidental teaching was composed of the following 3 general training categories:
Active one-on-one instruction (Figure 1b): An adult interventionist brings attention to desired social behaviors; coaches, models, and prompts age-appropriate social behaviors; encourages Will to drive to desired activities; and encourages Will to ask peers for assistance such as to help move obstacles out of his driving path.
Supplemental group guidance (Figure 1c): An adult interventionist invites Will to join others’ activities; points out and acknowledges Will’s efforts and accomplishments by watching, listening, and imitating and repeating Will’s actions and words; and comments out loud on what children are doing especially related to goals.
Environmental modification (Figure 1d): An adult interventionist modifies the physical environment to make it easier for Will to drive and engage in group play; provides time and opportunity in the class schedule for Will to do things independently; organizes specific activities that foster participation with others; and problem solves with Will and his peers various ways for UD2 to fit into tight spaces. Figure 1d illustrates Will interacting with his peers on his own, in part due to the environmental modification of placing toys within everyone’s reach, as well as establishing roles in a role playing game of ‘grocery store’ such that Will is an integral part of the activity.
Procedure
Will had access to UD2, an experimental mobility device that is small enough for use in his 593 sq. ft. classroom (Figure 1a).10 Our previous case report documented Will’s mobility and socialization for a 10-day ‘baseline phase’ followed by a 13 day ‘mobility phase’ when Will received UD2 to drive in his classroom but no additional training. The present case report compares Will’s mobility and socialization during a 10-day ‘training phase’ followed by a 7-day ‘post-training phase’ to the previous case report data. During the ‘training phase’, Will used UD2 for 10 days while supported by an interdisciplinary training team of a pediatric physical therapist, a pediatric occupational therapist, the head teacher of his preschool classroom, and an additional classroom teacher with experience with children with special needs. During the post-training phase, Will used UD2 for 7 days without training, as he did during the mobility phase of the previous report.
As in our previous report, we videotaped classroom activities each morning for 2 hours during morning free play period during each of the phases. Videotaping took place for 2 hours per day, however Will had access to UD2 in the classroom all day. We used multiple ceiling-mounted cameras within the classroom and a camcorder (Sony Hard Disk Drive DCR SR40, San Diego, CA) recording through a 1-way window within the classroom’s observation booth. Experimenters remained out of sight of the classroom. Of the 2 hours filmed each day during both phases, each child’s 30 ‘most active’ minutes were selected for coding according to our previously established coding protocol.10
Measures
As with our previous report10, the following measures were obtained during the ‘training’ and ‘post-training’ phases via coding video footage. We have included certain data from the ‘baseline’ and ‘mobility’ phases of the previous report for ease of comparison with the ‘training’ and ‘post training’ phases of the current report.
Mobility
Percent time Will was in UD2: The percent time Will was sitting in UD2 during his 30 most active minutes was determined. During this time, he may or may not have been driving.
Percent time Will drove UD2: The percent time Will drove UD2 during his 30 most active minutes was calculated. Although we observed in our video footage the mobility levels of the comparison child in each phase, we collected no formal mobility data for this child.
Socialization
During all phases, the following measures were obtained from video footage of both Will and the comparison child using the coding definitions of Howes and Matheson.34
Amount of time solitary: The amount of time spent greater than 3 feet away from a peer or teacher and not engaged in verbal or physical interaction with a peer or teacher.
Amount of time in parallel play/parallel awareness (we term ‘Parallel play/Aware’): The amount of time spent within 3 feet of a peer where both children are playing with similar toys but either show no awareness of each other or are aware of but not interacting with each other.
Amount of time in teacher interaction (we term “Teacher-Peer Interaction”): The amount of time spent interacting verbally and/or physically with a teacher. If a teacher is interacting with a group of peers then this is coded as only teacher interaction and not peer interaction.
Amount of time in peer interaction (we term “Peer-Peer Interaction”): The amount of time spent interacting verbally and/or physically with 1 or more peers.
Coding Reliability
The coding procedure was the same as used in the previous report.10 In brief, a primary rater coded each social category for each day for each child. The first 20 percent of video in each phase (approximately 2 days of video) was coded by a secondary coder. At least 90 percent inter-rater reliability was achieved between coders.
Outcomes
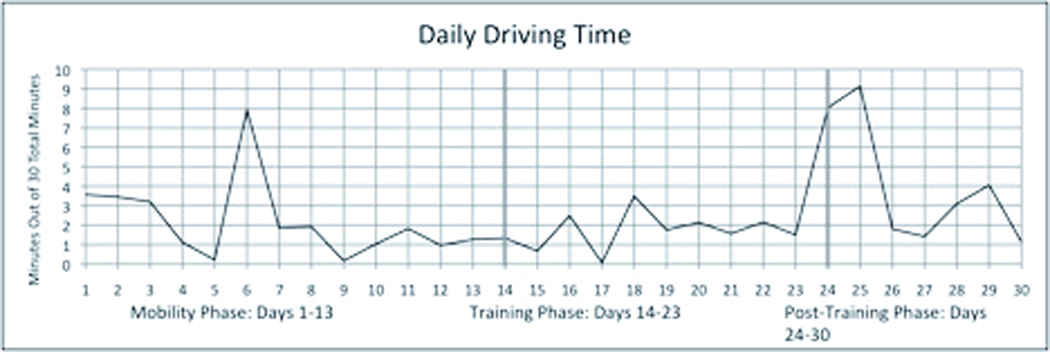
Mobility (Figure 2)
Figure 2.
The number of minutes that Will drove the robot during the 30 most active minutes coded each day of the ‘mobility’, ‘training’, and ‘post-training’ phases. The ‘mobility phase’ data is from our previous case report.10
During the ‘training phase’, Will did not appear to increase his mobility as compared to before training (‘mobility phase’). He drove UD2 for about 1 to 4 minutes (on average about 10%) of his most active 30 minutes per day, although he spent 100% of that time in UD2. During the ‘post-training phase’, Will drove for about 2 to 10 minutes (about 25%) of his most active 30 minutes/day, which appears to be more than during the training phase and at a similar level to his level before training. In contrast, our observations and video footage of the other preschool children in the classroom, including the comparison child, confirmed that they were highly mobile -- walking, running, jumping, falling -- for the majority of their most active minutes. Thus, the difference in mobility between Will using UD2 and his peers was striking even during Will’s somewhat increased mobility during the post training phase.
Socialization
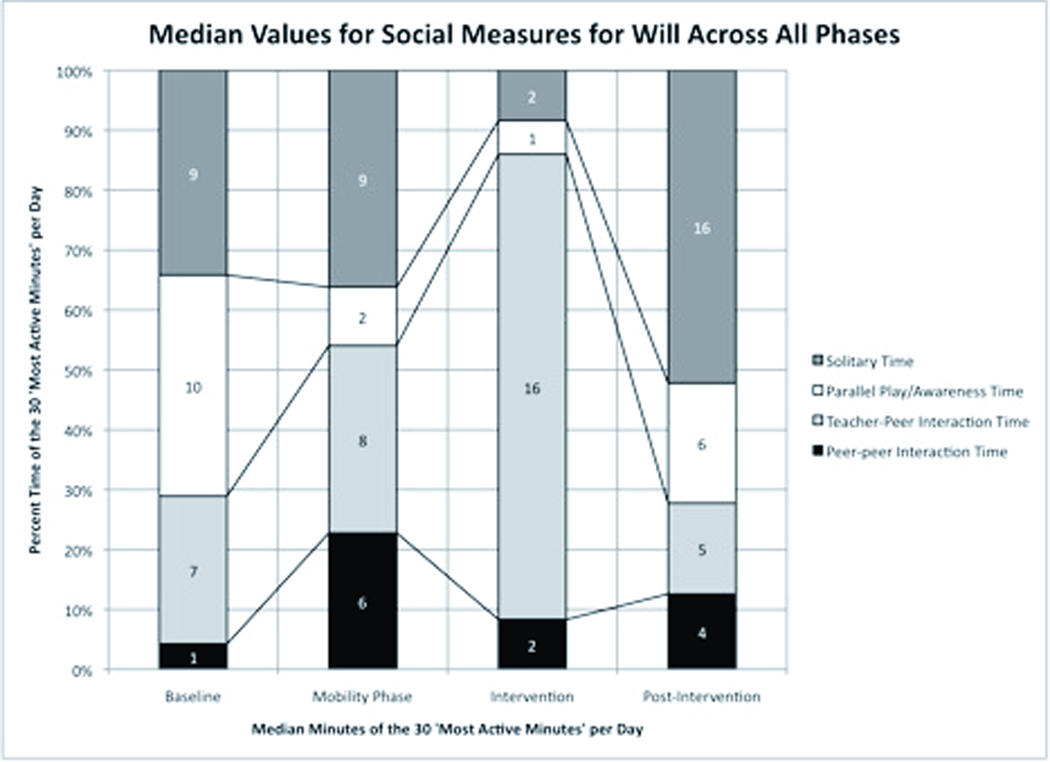
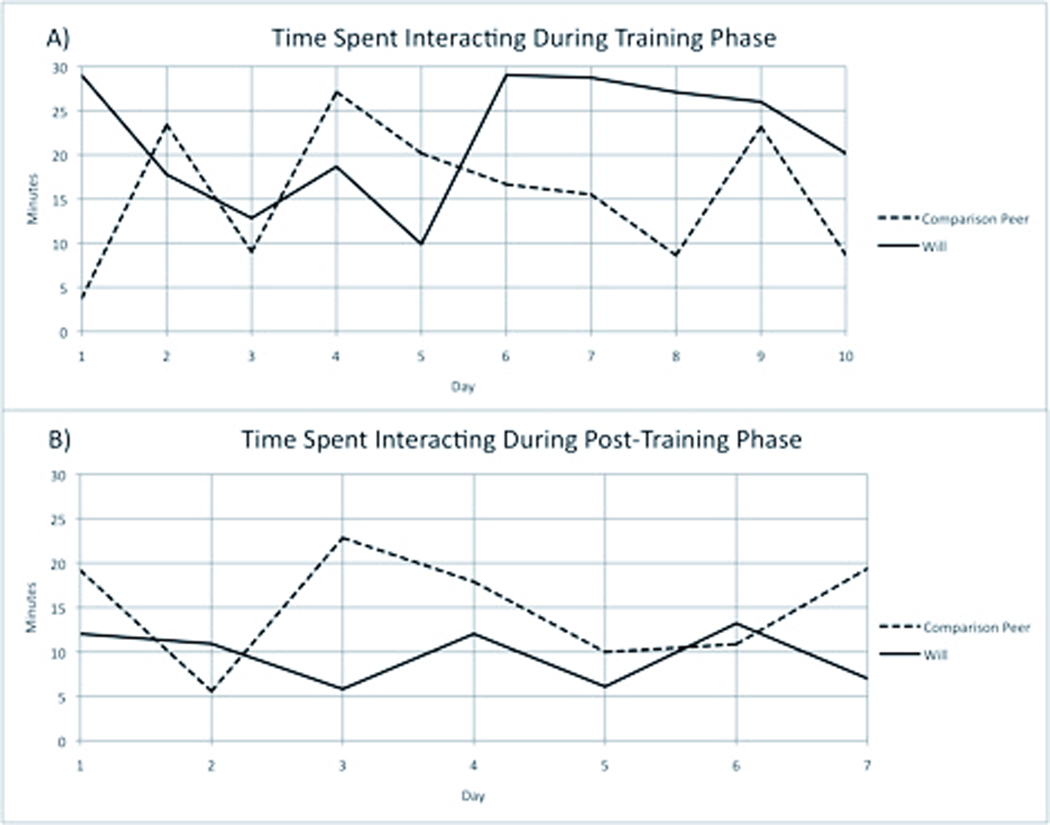
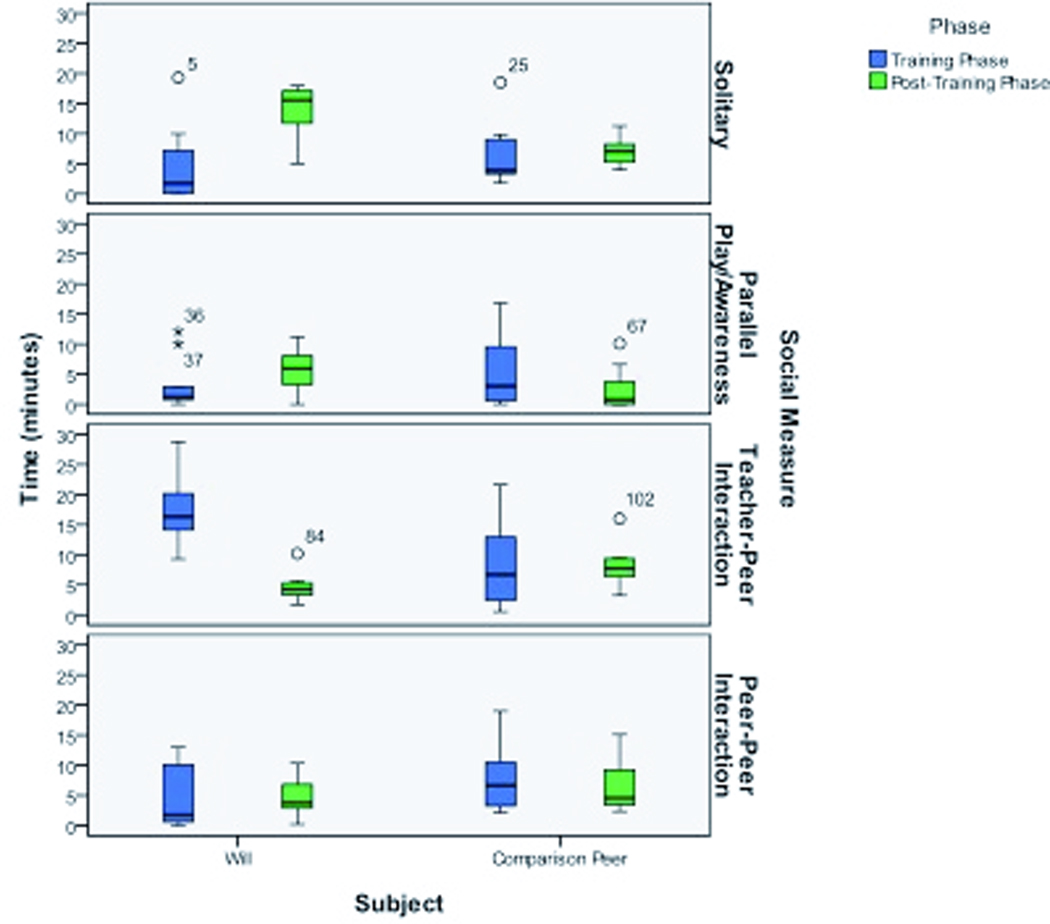
Will did appear to increase his socialization during the ‘training phase’ compared to the mobility and baseline phases (Figure 3). During the ‘training phase’, Will’s total median time interacting with teachers and peers (sum of median teacher-peer interaction and median peer-peer interaction) was approximately 85% (approximately 18 minutes per day) of his most active minutes. This was greater than his total time interacting during the ‘mobility phase’ before training, which was approximately 55% (about 14 minutes per day). Figure 4a suggests that Will interacted more than the comparison peer for 7 of the 10 training days. In addition, both Will’s maximum and minimum times spent interacting during the ‘training phase’ exceeded those of the comparison peer (Figure 4a). Furthermore, during the ‘training phase’, Will spent less time on average in solitary and parallel play and more time in teacher-peer and peer-peer interactions than the comparison peer (Figure 5).
Figure 3.
The median number of minutes and the percentage of the 30 ‘most active minutes’ per day that Will spent in each social measure across the Baseline and Mobility phases (for comparison, from previous case report: Baseline is before Will received UD2, and the ‘mobility phase’ is 13 days when Will drove UD2 with no additional training), as well as the ‘training’ and ‘post-training phases’ (present case report). The Baseline and Mobility phases are from our previous case report.10
Figure 4.
The number of minutes during the 30 most active minutes coded each day that each subject interacted with either teachers and/or peers during A) the ‘training phase’ and B) the ‘post-training phase’. The black line represents Will’s interaction times; the dashed line represents the comparison peer’s interaction data.
Figure 5.
Box plots of time (minutes) that each subject spent solitary, in parallel play/awareness, teacher-peer interactions, and peer-peer interactions. Blue boxes represent ‘training phase’ values; green boxes represent ‘post-training phase’ values. The central horizontal line marks the median value per subject. The top and bottom edges of the box mark the limits within which fall the central 50% of the values. The whiskers extend to the highest and lowest scores for each subject. Circles are the outliers within 1.5 to 3 box lengths from the 75th percentile (top edge of box); asterisks are outliers greater than 3 box lengths from the 75th percentile.
During the ‘post-training’ phase, Will appeared to decrease his socialization to approximately 30% (approximately 9 minutes per day) as compared to the ‘training phase’ (Figure 3), thus decreasing back to interactive levels of the ‘baseline’ phase (approximately 30%, approximately 8 minutes per day). In addition, Will interacted less than the comparison peer for 5 of the 7 post-training days and his maximum time interacting was less than the comparison peer’s (Figure 4b). Furthermore, during the ‘post-training phase’, Will spent more time on average solitary and in parallel play and less time in teacher-peer and peer-peer interactions than the comparison peer (Figure 5).
Discussion
This report provides 4 main points for clinical and research consideration. First, providing adult-directed mobility and socialization training for a 3-year-old with CP in a preschool classroom appears feasible. Specifically, the intervention team successfully embedded themselves during free play hours without significant disruption of the classroom routine. Will’s increase in interaction time during the ‘training phase’ suggests that our team effectively engaged him in more classroom interactions than he had previously experienced. Interventionists, coded as teachers, were almost constantly engaging him and his peers in activities, hence the steep increase in teacher-peer interactions, the decrease in interactions with peers with no teachers present, and of the decrease in total non-interactive time. Our adult-directed, short-term mobility and socialization training appears to be a feasible option for future studies focused on socialization with or without mobility in a preschool classroom.
Second, though it may seem intuitive considering the goals of this study, deliberate and perhaps even compartmentalized attention should be devoted to both socialization and mobility during training. That is, one unexpected result was that Will did not increase his driving time during the ‘training phase’ (Figure 2). One explanation is that the training team emphasized increasing Will’s socialization over his mobility. Team members may have inadvertently assumed that an increase in socialization during training would in turn increase mobility post training. Although power mobility increases the opportunities for children to interact,27 we know of no studies suggesting if or when children actually take advantage of their newfound power mobility to initiate and maintain social interactions. Another explanation is that Will did not transfer his mobility skills from one context to another in this short time period. This lack of transfer has been noted in preschool children35 and may, in part, explain that although Will was a proficient, independent driver on the playground and in large indoor spaces such as the gym and hallways, he did not automatically transfer this level of mobility to the classroom. With these explanations in mind, we propose that a combination of longer training that more equally emphasizes mobility with socialization in the classroom may be required for a complete transfer of driving abilities between contexts.
Third, there appears to be a period of time when the child is learning power mobility before actually using mobility for socialization and vise versa. Until the child views the mobility device as a means to a social end, a disconnect may be apparent between moving and socializing. That is, we observed that Will’s mobility and socialization did not appear to simultaneously increase or decrease. During training, Will increased his interaction time but decreased his driving time. Post training, Will decreased his interaction time but increased his driving time. These preliminary observations suggest 3 factors for clinical consideration and future study: 1) device characteristics, 2) past history with peers and adults, and 3) style of intervention. First, even at top speed UD2 drives at a slower pace than a typical preschool aged child’s walking and running speed. As a result, he may have often been left trailing his faster peers from activity to activity. While UD2 is smaller than a commercial pediatric power chair, other characteristics such as speed need additional adjustment. Second, although a preschool classroom is a dynamic environment, previous experience results in expectations and predictability between peers and teachers. Given Will’s multiple years of immobility, his teachers and peers may need more experience with a ‘mobile Will’ to more permanently change their physical and social interactions with him, which are likely based in part on his immobility. These interactions may have simply been too stable to be positively perturbed by any short-term changes seen during training. Whether or not past experiences were a factor in Will’s post training response, the literature is clear that children with disabilities experience varying degrees of social isolation due to peer ‘rejection’ and/or the inability to keep up with physical activities typical of peers.5,36 Consequently, peers who are typically developing may have fewer positive interactions, and at times, no interactions with a peer with special needs.16 Research on interventions designed for children with social impairments such as those for children with autism suggest simply placing a child in an inclusive classroom is not enough. Classroom integration must be a deliberate goal to achieve significant improvement in socialization.32 Finally, the intense adult interaction during the training phase may have decreased the chance for Will to learn how to independently seek out and then sustain peer interactions on his own. This may, in part, explain his decrease in interaction post-training (Figures 3–5) as has been noted in adult-directed interventions for preschoolers with autism.32 Adults may also have been less likely to move about as much as peers, and therefore Will’s intense interaction with teachers during training may explain the concomitant low level of mobility. Common alternatives to primarily adult-directed interventions include the use of peer-mediated interventions.37,38 To be clear, in this study Will’s peers were not taught how to interact with him. It may be more effective in the future, however, to train certain key peers or all of the children specific strategies to better interact with Will given his physical impairments. That is, when a child is delayed in social skills, teaching other children how to initiate and sustain verbal and nonverbal interactions can be helpful, as has also been seen to be effective with certain preschool aged children with autism.39 In summary, an appropriate mobility device, as well as the duration and frequency of mobility and socialization training in combination with more peer-mediated activities are important features to consider in planning a treatment strategy.
Finally, comprehensive mobility and socialization training may need to start earlier than preschool. If by preschool immobility and socialization have co-developed such that the physical and social environment surrounding a child who is immobile has become stable, then a relatively large positive perturbation from any intervention may be required. Our previous and current work suggests that starting power mobility in infancy for certain populations such as those with spina bifida and CP is feasible both with our experimental devices (Figure 6a), and modifications of commercial pediatric power chairs (Figure 6b). The idea being that if basic driving skills can be acquired by toddlerhood, the child along with peers and adults may experience mobility and socialization co-emerging along a more typical time line.
Figure 6.
A) An infant driving UD2. B) An infant driving our modified standard power chair (Permobil Koala, Lebanon, TN).
In conclusion, short-term, adult-directed power mobility and socialization training appears feasible for the preschool classroom. Moreover, socialization may have increased from constant adult direction during training, but may not have remained at high levels post-training due to a lack of practice with independent peer interactions. Considering longer duration, more peer-mediated training, earlier intervention, and device characteristics may result in more effective outcomes. All of these issues are open questions, and a future group study is needed to validate the observations of this report. These findings combined with the previous case report10 raise an important issue for therapists and educators working with children using power mobility: intervention that is focused on either socialization or power mobility may increase each, but may not ultimately result in the use of mobility for socialization. We suspect that immobility and atypical socialization co-develop during the first years of life, and we believe that starting power mobility earlier than age 3 years within all key environments and with all key adults and children will allow for a more typical co-development of mobility and socialization.
Acknowledgments
Grant Support: Supported in part by the National Science Foundation and National Institute of Health.
This work was completed as part of the PhD work of Christina Ragonesi in the Biomechanics and Movement Sciences graduate program, University of Delaware.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anderson DI, Campos JJ, Anderson DE, et al. The flip side of perception–action coupling: Locomotor experience and the ontogeny of visual–postural coupling. Human Movement Science. 2001;20(4–5):461–487. doi: 10.1016/s0167-9457(01)00063-x. [DOI] [PubMed] [Google Scholar]
- 2.Bertenthal BI, Campos JJ. New directions in the study of early experience. Child Dev. 1987;58(3):560–567. [PubMed] [Google Scholar]
- 3.Campos JJ, Anderson DI, Barbu-Roth MA, Hubbard EM, Hertenstein MJ, Witherington D. Travel broadens the mind. Infancy. 2000;1(2):149–219. doi: 10.1207/S15327078IN0102_1. [DOI] [PubMed] [Google Scholar]
- 4.Thelen E. The Central Role of Action in Typical and Atypical Development: A Dynamic Systems Perspective. In: Stockman IJ, editor. Movement and Action in Learning and Development. London: Elsevier Academic Press; 2004. pp. 49–73. [Google Scholar]
- 5.Larkin D, Summers J. Implications of Movement Difficulties for Social Interaction, Physical Activity, Play, and Sports. In: Dewey D, Tupper DE, editors. Developmental motor disorders: A neuropsychological perspective. Guilford Press; 2004. pp. 443–460. [Google Scholar]
- 6.Deitz J, Swinth Y, White O. Powered mobility and preschoolers with complex developmental delays. Am J Occup Ther. 2002;56(1):86–96. doi: 10.5014/ajot.56.1.86. [DOI] [PubMed] [Google Scholar]
- 7.Lynch A, Ryu JC, Agrawal S, Galloway JC. Power Mobility Training for a 7-Month-Old Infant with Spina Bifida. Pediatric Physical Therapy. 2009;21(4):362. doi: 10.1097/PEP.0b013e3181bfae4c. [DOI] [PubMed] [Google Scholar]
- 8.Butler C, Okamoto GA, McKay TM. Powered mobility for very young disabled children. Dev Med Child Neurol. 1983;25(4):472–474. doi: 10.1111/j.1469-8749.1983.tb13792.x. [DOI] [PubMed] [Google Scholar]
- 9.Guerette P, Refft D, Furumasu J. Pediatric Powered Wheelchairs: Results of a National Survey of Providers. Assistive Technology: The Official Journal of RESNA. 2005;17:144–158. doi: 10.1080/10400435.2005.10132104. [DOI] [PubMed] [Google Scholar]
- 10.Ragonesi C, Chen X, Agrawal S, Galloway JC. Power Mobility and Socialization in Preschool: A Case Report on a Child with Cerebral Palsy. Pediatric Physical Therapy. 2010;22(3):322–329. doi: 10.1097/PEP.0b013e3181eab240. [DOI] [PubMed] [Google Scholar]
- 11.Hay DF, Payne A, Chadwick A. Peer relations in childhood. Journal of Child Psychology and Psychiatry. 2004;45(1):84–108. doi: 10.1046/j.0021-9630.2003.00308.x. [DOI] [PubMed] [Google Scholar]
- 12.Bauminger N, Shulman C, Agam G. Peer interaction and loneliness in high-functioning children with autism. J.Autism Dev.Disord. 2003;33(5):489–507. doi: 10.1023/a:1025827427901. [DOI] [PubMed] [Google Scholar]
- 13.Shores RE. Overview of Research on Social Interaction: A Historical and Personal Perspective. Behavioral Disorders. 1987;12(4):233–241. [Google Scholar]
- 14.Howes C, Matheson CC. Sequences in the development of competent play with peers: Social and social pretend play. Dev.Psychol. 1992;28(5):961–974. [Google Scholar]
- 15.Berry ET, McLaurin SE, Sparling JW. Parent/caregiver perspectives on the use of power wheelchairs. Pediatric Physical Therapy. 1996;8(4):146. [Google Scholar]
- 16.Mize J. Social skills intervention and peer relationship difficulties in early childhood: Comments on Bierman and Erath, Manz and McWayne, and Odom. In: Tremblay RE, Barr RG, Peters RD, editors. Encyclopedia on Early Childhood Development [online] Montreal, Quebec: Centre of Excellence for; 2005. pp. 1–7. [Google Scholar]
- 17.Rosenbaum PL, Walter SD, Hanna SE, et al. Prognosis for gross motor function in cerebral palsy: creation of motor development curves. JAMA. 2002;288(11):1357. doi: 10.1001/jama.288.11.1357. [DOI] [PubMed] [Google Scholar]
- 18.Zazula JL, Foulds RA. Mobility device for a child with phocomelia. Arch Phys Med Rehabil. 1983;64(3):137–139. [PubMed] [Google Scholar]
- 19.Douglas J, Ryan M. A pre-school severely disabled boy and his powered wheelchair: A case study. Child Care, Health Development. 1987;13:303–309. doi: 10.1111/j.1365-2214.1987.tb00547.x. [DOI] [PubMed] [Google Scholar]
- 20.Jones MA, McEwen IR, Hansen L. Use of power mobility for a young child with spinal muscular atrophy. Phys Ther. 2003;83(3):253. [PubMed] [Google Scholar]
- 21.Galloway JC, Ryu JC, Agrawal SK. Babies driving robots: self-generated mobility in very young infants. Intelligent Service Robotics. 2008;1(2):123–134. [Google Scholar]
- 22.Chiulli C, Corradi-Scalise D, Donatelli-Schultheiss L. Powered mobility vehicles as aids in independent locomotion for young children. Phys Ther. 1988;68(6):997–999. doi: 10.1093/ptj/68.6.997. [DOI] [PubMed] [Google Scholar]
- 23.Butler C, Okamoto GA, McKay TM. Motorized wheelchair driving by disabled children. Arch Phys Med Rehabil. 1984;65(2):95–97. [PubMed] [Google Scholar]
- 24.Bottos M, Bolcati C, Sciuto L, Ruggeri C, Feliciangeli A. Powered wheelchairs and independence in young children with tetraplegia. Dev Med Child Neurol. 2001;43(11):769–777. doi: 10.1017/s0012162201001402. [DOI] [PubMed] [Google Scholar]
- 25.Butler C. Effects of powered mobility on self-initiated behaviors of very young children with locomotor disability. Dev Med Child Neurol. 1986;28(3):325–332. doi: 10.1111/j.1469-8749.1986.tb03881.x. [DOI] [PubMed] [Google Scholar]
- 26.Buning ME, Angelo JA, Schmeler MR. Occupational performance and the transition to powered mobility: a pilot study. Am J Occup Ther. 2001;55(3):339–344. doi: 10.5014/ajot.55.3.339. [DOI] [PubMed] [Google Scholar]
- 27.Nilsson LM, Nyberg PJ. Driving to learn: a new concept for training children with profound cognitive disabilities in a powered wheelchair. American Journal of Occupational Therapy. 2003;57(2) doi: 10.5014/ajot.57.2.229. [DOI] [PubMed] [Google Scholar]
- 28.McEwen IR, Jones MA, Neas B. Effects of Power Wheelchairs on the Development of Children Aged 14–30 Months with Severe Motor Impairments. 3rd International Cerebral Palsy Conference; February 2009; Sydney, Australia. 2009. [Google Scholar]
- 29.Nisbet P, Craig I. Mobility and mobility training for severely disabled children: results of the “Smart” Wheelchair project. 1994;94:17–22. [Google Scholar]
- 30.Okamoto GA, Butler C. Physical Medicine and Rehabilitation: Powered Mobility for Very Young Disabled Children. West J Med. 1986;144(6):733. [PMC free article] [PubMed] [Google Scholar]
- 31.Paulsson K CM. Psychosocial aspects of technical aids-how does independent mobility affect the psychosocial and intellectual development of children with physical difficulties. 1989:282–285. [Google Scholar]
- 32.Rogers SJ. Interventions that facilitate socialization in children with autism. J Autism Dev Disord. 2000;30(5):399–409. doi: 10.1023/a:1005543321840. [DOI] [PubMed] [Google Scholar]
- 33.McGee GG, Morrier MJ, Daly T. An incidental teaching approach to early intervention for toddlers with autism. The Journal of the Association for Persons with Severe Handicaps. 1999;24(3):133–146. [Google Scholar]
- 34.Howes C, Matheson CC. Sequences in the development of competent play with peers: Social and social pretend play. Dev Psychol. 1992;28(5):961–974. [Google Scholar]
- 35.Flavell JH, Miller PH, Miller SA. Cognitive development. 3rd ed. Englewood Cliffs, NJ: Prentice Hall; 1993. [Google Scholar]
- 36.Krigger KW. Cerebral palsy: an overview. Am Fam Physician. 2006;73(1):91–100. [PubMed] [Google Scholar]
- 37.Fantuzzo JW, Jurecic L, Stovall A, Hightower AD, Goins C, Schachtel D. Effects of adult and peer social initiations on the social behavior of withdrawn, maltreated preschool children. J Consult Clin Psychol. 1988;56(1):34–39. doi: 10.1037//0022-006x.56.1.34. [DOI] [PubMed] [Google Scholar]
- 38.Fantuzzo J, Sutton-Smith B, Atkins M, et al. Community-based resilient peer treatment of withdrawn maltreated preschool children. J Consult Clin Psychol. 1996;64(6):1377–1386. doi: 10.1037//0022-006x.64.6.1377. [DOI] [PubMed] [Google Scholar]
- 39.McGee GG, Almeida MC, Sulzer-Azaroff B, Feldman RS. Promoting reciprocal interactions via peer incidental teaching. Journal of applied behavior analysis. 1992;25(1):117–126. doi: 10.1901/jaba.1992.25-117. [DOI] [PMC free article] [PubMed] [Google Scholar]