Summary
Background
Epidemiologic studies have documented higher rates of asthma prevalence and morbidity in minority children compared to non-Latino white (NLW) children. Few studies focus on the mechanisms involved in explaining this disparity, and fewer still on the methodological challenges involved in rigorous disparities research.
Objectives and Methods
This article provides an overview of challenges and potential solutions to research design for studies of health disparities. The methodological issues described in this article were framed on an empirical model of asthma health disparities that views disparities as resulting from several factors related to the healthcare system and the individual/community system. The methods used in the Rhode Island–Puerto Rico Asthma Center are provided as examples, illustrating the challenges in executing disparities research.
Results
Several methods are described: distinguishing ethnic/racial differences from methodological artifacts, identifying and adapting culturally sensitive measures to explain disparities, and addressing the challenges involved in determining asthma and its severity in Latino and other minority children. The measures employed are framed within each of the components of the conceptual model presented.
Conclusions
Understanding ethnic and/or cultural disparities in asthma morbidity is a complicated process. Methodologic approaches to studying the problem must reflect this complexity, allowing us to move from documenting disparities to understanding them, and ultimately to reducing them.
Keywords: asthma, health disparities, Latino, Puerto Rican, children, research methods
INTRODUCTION
Epidemiologic studies have documented higher rates of asthma in African American and Latino children compared to NLW children.1,2 The magnitude and complexity of this problem led to an initiative sponsored by the National Heart, Lung and Blood Institute (NHLBI), through which four Collaborative Centers were established to respond to the disparities identified in the prevalence, morbidity, and treatment of asthma among minorities. In this article we describe the methods used in one of the funded centers: the Rhode Island–Puerto Rico Asthma Center (RIPRAC).
Puerto Rican (PR) children from the US (mainland) and island have the highest rates of asthma and are more likely to die because of their asthma than any other ethnic group.1,3–6 Dominican children who reside in the US also have higher asthma prevalence and morbidity rates than other Latino ethnic subgroups.7 The main purpose of RIPRAC was to identify the factors contributing to disparities in asthma morbidity among non-Latino white (NLW) children and island and mainland PR and Dominican minority children (henceforth referred to as Latino children).
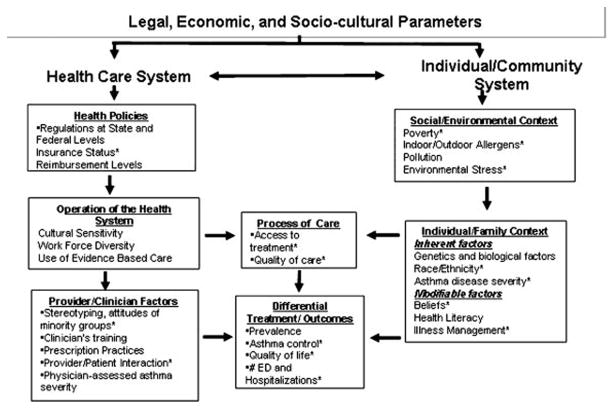
Health disparities research is a relatively new, yet highly important area of investigation.8 To date, a majority of studies in this area focus on processes that may be associated with disparities in asthma outcomes between ethnic groups of children residing in the mainland US. Given that the etiology of asthma and the components of its treatment are determined by multiple factors (see Figure 1), health disparities research must involve the examination of potential mechanisms across multiple levels (e.g., individual, environment) through a careful methodological approach. In this article, we review methodological efforts to studying health disparities based on an empirically driven conceptual model of pediatric asthma disparities, using RIPRAC as an example.
Fig. 1.
Framework of asthma disparities.
A Conceptual Model for Health Disparities Research
The conceptual model of asthma disparities that guides the central questions of RIPRAC is based on a modification made9,10 to the Institute of Medicine (IOM) model8 in order to include variables related to asthma disparities. The model (see Figure 1) includes two main domains: the healthcare system and the individual/community domain. Each of these domains is composed of components that interact with each other to affect the process of care (quality and access) that, in turn, may influence disparity outcomes such as prevalence and morbidity of asthma. The healthcare system domain is composed of health policies, the operation of the healthcare system, and provider characteristics and interactions with patients. The individual/community domain is composed of the social/environmental context and the individual/family context. Within each of these components there are factors that have been found in prior research or are hypothesized to be associated with health disparities. The model is multilevel and the different domains and components of the model are hypothesized to interact in determining asthma disparities.
Our study objectives were to assess the different variables across sites, family/individual characteristics, the healthcare service delivery system, and other contextual factors that may contribute to asthma disparities in Latino children. We were not able to measure all of the variables included in the model; instead, we focused on modifiable variables so that the information obtained could be used for the development of future family interventions.
In Figure 1, a star is placed beside each of the factors in our model that were assessed in RIPRAC. Within the individual domain, we measured ethnicity as an inherent individual variable, and asthma severity as a genetic/biological variable. We also assessed modifiable variables such as family management practices and medication beliefs. Within the environmental domain, we measured poverty, environmental stress and reported exposure to allergens and triggers. Within the healthcare system domain, we measured insurance status and other barriers to care, as well as perception of patient provider communication and discrimination. We hypothesized that the components described in the individual/community and healthcare system domains would interact to affect the quality and access to care and that this in turn would be related to outcomes such as asthma control, and healthcare utilization (emergency department [ED] use and hospitalization).
In what follows, we describe the methods used to examine the hypothesized variables involved in evaluating disparities in asthma among Latino children. We start with a discussion of some methodologic challenges faced by researchers who study disparities with diverse populations, followed by a description of the measures used. Means, standard deviations, and Cronbach’s alphas of the instruments utilized are provided in Table 1.
TABLE 1.
RIPRAC Self-Report and Interview Assessments
| Measure/scale | Mean (SD), Cronbach’s alpha
|
||
|---|---|---|---|
| Informant | English | Spanish | |
| Individual, family and environmental level assessments | |||
| Perceived poverty (adapted from Gore et al.63): Measures caregiver’s perception of economic status in general and compared to other families | Parent | 2.71 (0.81), α = 0.81 | 2.56 (0.80), α = 0.80 |
| Scale score is the mean across two items having response options ranging from 1 to 5. Higher scores indicate more perceived poverty | |||
| Cultural stress—Adult version (adapted from Cervantes et al.49): Measures stress related to acculturation, immigration, family/culture, marriage, and occupational/economic factors | Parent | ||
| Twenty-six items with response options ranging from 0 (rarely/never) to 2 (often). Mean scores are calculated across items, with higher scores indicating more stress | |||
| Immigration stress (9 items) | 0.32 (0.43), α = 0.91 | 0.29 (0.35), α = 0.84 | |
| Marital stress (1 item) | 0.55 (0.71) | 0.45 (0.66) | |
| Family stress (7 items) | 0.62 (0.49), α = 0.80 | 0.34 (0.38), α = 0.78 | |
| Racial stress (9 items) | 0.49 (0.52), α = 0.90 | 0.21 (0.27), α = 0.79 | |
| Total cultural stress score (26 items) | 0.47 (0.41), α = 0.94 | 0.28 (0.28), α = 0.90 | |
| Cultural stress—Youth version (adapted from Cervantes et al.49): Sixteen items with response options ranging from 0 (rarely/never) to 2 (often). Mean scores are calculated across items, with higher scores indicating more stress | Child | ||
| Younger child stress (4 items) | 0.10 (0.19), α = 0.41 | 0.18 (0.24), α = 0.51 | |
| Older child stress (12 items) | 0.14 (0.16), α = 0.64 | 0.15 (0.14), α = 0.68 | |
| Total cultural stress (16 items) | 0.13 (0.14), α = 0.68 | 0.15 (0.14), α = 0.73 | |
| Neighborhood Unsafety Scale47: Measures perception of neighborhood disadvantage during the previous year. 7 items assess perceptions of safety of different elements of the neighborhood (e.g., feeling safe outside at night, trusting neighbors). Response options range from 1 (very true) to 4(not at all true). Scale score is the mean across items, with higher scores indicating lower levels of perceived safety | Parent | 1.84 (0.75), α = 0.90 | 1.93 (0.63), α = 0.75 |
| Language proficiency in English and Spanish (adapted from Felix-Ortiz et al.56): Six items with response options ranging from 1 (poor) to 6 (excellent) assess English and Spanish proficiency. Proficiency scores are means across items, with higher scores indicating more proficiency. Measure was administered only to Latino participants. Scale characteristics are listed by site (island Puerto Ricans and RI Latinos, respectively) | Parent and child | ||
| Island PR | RI Latino | ||
| Parent English proficiency (3 items) | 2.01 (0.81), α = 0.95 | 2.24 (0.96), α = 0.90 | |
| Parent Spanish proficiency (3 items) | 3.43 (0.59), α = 0.93 | 3.43 (0.73), α = 0.89 | |
| Child English proficiency (3 items) | 2.13 (0.72), α = 0.63 | 3.40 (0.55), α = 0.73 | |
| Child Spanish proficiency (3 items) | 3.43 (0.57), α = 0.83 | 2.23 (0.91), α = 0.73 | |
| Language preference in English and Spanish (selected items from Marin et al.57): Three items assess respondent’s preference for speaking English or Spanish with friends and family and when thinking. Response options range from 1 (Spanish all the time) to 5 (English all the time). No scale score is computed | Parent and child | n/a | n/a |
| Emotion Expression Scale for Children64: Assesses children’s awareness of and comfort with negative emotions such as anger and sadness. Response options range from 1 (not at all true) to 4 (very true). Scores are the sum across scale items, with higher scores indicating more difficulties with emotion expression | Child | ||
| Poor Awareness scale (8 items) | 16.50 (6.79), α = 0.80 | 15.27 (6.86), α = 0.84 | |
| Expressive Reluctance scale (8 items) | 17.62 (6.64), α = 0.78 | 15.72 (6.38), α = 0.78 | |
| Child Somatization Inventory65: Assesses child’s somatic complaints in the previous 2 weeks. Respondents are presented with a list of 35 symptoms (e.g., headaches) with response options ranging from 0 to 3, with higher scores indicating higher symptom frequency. Scores are the sum across scale items, with higher scores indicating more somatic complaints | Child | 15.6 (14.3), α = 0.91 | 14.7 (14.8), α = 0.91 |
| Patient Health Questionnaire, Somatic Symptom Severity Scale66: 15 items assessing parent somatic symptoms. Response options range from 0 to 2. The sum across scale items comprises the scale score, with higher values indicating more somatic complaints | Parent | 8.78 (5.71), α = 0.85 | 9.83 (5.99), α = 0.84 |
| Beliefs about Medication24: 11-item measure accesses parental beliefs and concerns about their children’s asthma medications. Parents indicate on a 5-point scale how much they agree with statements about asthma medications. Scale scores are means across items, with higher scores indicating stronger beliefs and concerns | Parent | ||
| Necessity of medications score (5 items) | 3.54 (0.82), α = 0.82 | 3.37 (0.93), α = 0.82 | |
| Concerns about medications score (6 items) | 2.67 (0.80), α = 0.75 | 3.13 (0.85), α = 0.74 | |
| Family Asthma Management System Scale34,35: Semi-structured interview. Families are rated on 7 domains of asthma management. Ratings range from 1 to 9, with higher values indicating better management in a given domain. The FAMSS total score is the mean across ratings and represents the overall of adequacy of the family’s asthma management system | Parent and child | 5.34 (1.25), α = 0.81 | 4.29 (1.44), α = 0.89 |
| Provider and Healthcare System Level Assessments | |||
| Health Services Research Questionnaire (adapted from Ortega et al.51): 36 items assess access to and continuity of asthma care, insurance type, acute healthcare utilization, and barriers to care. No scale scores are calculated | Parent | n/a | n/a |
| Provider Communication and Partnership Questionnaire59: 11-item scale that assesses caregiver’s perception of physician behaviors related to the quality of communication, partnership, and decision-making in treatment process. Response options range from 1 to 7. Scale score is the mean across all items, with higher scores indicating better patient–provider partnership | Parent | 5.20 (0.85), α = 0.96 | 5.47 (0.80), α = 0.97 |
| Perceived Discrimination60: 9 items measure daily experiences of discrimination. Response categories modified from original version range from 1 to 6. Three additional items tap perception of discrimination due to Latino ethnicity. Response options range from 1 to 4. Both scales are calculated by summing across items. Higher scores indicate higher levels of perceived discrimination | Parent | ||
| Daily discrimination (9 items) | 44.65 (8.25), α = 0.84 | 47.78 (7.35), α = 0.82 | |
| Race/ethnicity-related discrimination (3 items) | 4.99 (2.22), α = 0.82 | 4.78 (2.16), α = 0.80 | |
| Disparity outcome measures | |||
| Pediatric Asthma Caregiver’s Quality of Life Questionnaire62: Subscales assess limitations to emotional functioning and family activities. Item response options range from 1 to 7. Both scale means across selected items, with higher scores indicating poorer functioning | Parent | ||
| Activity limitation (4 items) | 1.56 (1.07), α = 0.88 | 2.20 (1.50), α = 0.87 | |
| Emotional functioning (9 items) | 1.85 (1.05), α = 0.89 | 3.08 (1.35), α = 0.86 | |
| Total score | 1.76 (1.00), α = 0.92 | 2.81 (1.32), α = 0.91 | |
| Asthma Functional Severity Scale (adapted from Rosier et al.61): Items assess frequency of asthma episodes, symptoms between episodes, physical activity limitation, and intensity of impairment during an episode. Response options range from 0 to 4, with higher values indicating more frequent symptoms. Scale scores (4 weeks and 12 months recall) are the means across items, with higher scores indicating increasing functional severity | Parent | ||
| AFSS score—4 weeks recall (6 items) | 1.03 (0.89), α = 0.81 | 1.05 (0.89), α = 0.83 | |
| AFSS score—12 months recall (6 items) | 1.52 (0.78), α = 0.74 | 1.53 (0.78), α = 0.72 | |
METHODS
Methodological Challenges in Disparity Research
Distinguishing Ethnic Differences From Methodological Artifact
An important methodologic strategy in health disparities research is to assure comparability of the methods and protocol used across ethnic/cultural groups in order to disentangle whether any differences observed are a result of a health disparity and not a methodological artifact. The RIPRAC study was carried out in two settings, PR and Rhode Island (RI), and with four distinct groups of children 7–15 years: (1) PR children living on the island, (2) PR children living in RI, (3) Dominican children living in RI, and (4) NLW children living in RI. The study design was the same in both sites and for all the aims of the study: a cross-sectional, observational approach with repeated measurements (four sessions across a 4-month period) of selected variables.
Demographic Comparability
Differences in ethnicity may be confounded by differences in socioeconomic status (SES) and education level. There is evidence that poor children living in predominantly low SES communities are at greater risk of current asthma,11 and experience higher rates of hospitalizations.12 But it is important to have variability in income levels across the different ethnic groups in order to determine the extent to which poverty, independent of ethnicity, and other demographic variables is related to high prevalence and morbidity of asthma. In RI, most of the Dominican and PR families were of low SES, but it was possible to obtain middle- and high-income children with asthma in PR. Our design thus targeted the recruitment of at least 25% of the sample in PR to be of higher income levels. Additionally, we recruited our NLW sample in RI from a range of income levels to insure that within-site differences between NLWs and Latinos were not due only to income differences.
Comparability of Recruitment Settings
It is also important to assure comparability in recruitment settings both within sites (across ethnicities), and, for multisite designs, across sites. In RIPRAC, study participants from both sites were recruited primarily from convenience samples of primary care pediatric clinics. Given that the sample was not a probability sample, population-based inferences cannot be made. Variability across sites by clinic type was inevitable given the difficulty in recruiting Latino children in only one place in RI. Thus, in RI, participant recruitment for both Latino and NLW children occurred at a variety of locations including the Ambulatory Pediatric Clinics at the Hasbro Children’s Hospital (12% of recruited subjects), community primary care clinics (29%), a hospital-based asthma educational program (20%), health fairs and other community events (18%), schools in the greater Providence area (8%), and various grassroots sources (e.g., word of mouth, flyers, 13%). In Puerto Rico, 68.7% of the children were recruited from four independent provider organizations and two ambulatory pediatric clinics from two Hospitals serving mostly medically indigent patients. In order to recruit middle to upper income children with asthma, 29.4% of the sample was recruited from 26 private practice pediatric offices. Families in these private offices were screened regarding type of insurance with the assumption that those with private insurance would be in the middle to higher income category. Two percent of children were recruited from private referrals.
Protocol Comparability
Assuring protocol comparability for all participants, across sites and often in different languages, is also an important component of health disparities research. In RIPRAC, questionnaires and verbal procedures used among the PR and Dominican Spanish speaking families were translated and adapted from English using multistage, state-of-the-art methods employed previously by the Puerto Rican team of investigators.13–15 These methods insured cross-cultural semantic equivalence (similar meaning of items in each culture), content equivalence (content is relevant for population), and technical equivalence (original and translated versions must yield comparable data). Questionnaires were also reviewed to insure that wording and complexity of the items were appropriate for subjects with low literacy levels.
Comparability in Data Management and Quality
Disparities research conducted at multiple sites may involve research teams with different institutional policies and access to different resources. Therefore, careful attention must be paid to implementing data collection, data entry, and data management procedures in parallel across sites. Similar written parent consent and child assent were obtained in accordance with institutional review board guidelines at both participating institutions (RI Hospital and University of Puerto Rico). During RIPRAC project startup, at a joint training session, all research assistants and project staff were rigorously trained to follow similar procedures in both sites. A detailed description of patient flow, protocol procedures, and data processing instructions was written for use at both institutions (and translated into Spanish). Monthly phone calls and regular face-to-face meetings amongst project staff served to monitor the ongoing comparability of data collection across sites.
Determining the Diagnosis of Asthma and Clinical Diagnostic Comparability
Disparities research involving medical disorders must account for potential cultural difference, not only in patient symptom presentation, but also in the procedures to determine the medical diagnosis. Careful attention to diagnostic procedures and processes was required to insure that any diagnostic differences found between sites were due to true differences, not to differences in definition, the process of diagnosis, or idiosyncrasies of diagnosticians. Pediatric asthma specialists in RI and PR made the critical “gold standard” diagnosis of asthma and assigned the I–IV Severity Level based on national16 and international17 asthma guidelines. Physician-diagnosed asthma was confirmed through medical history, physical examination, and lung function testing. A manual was devised for implementation at both sites, which included a clinician interview of key items to consider for asthma diagnosis, and a visual algorithm for severity if asthma diagnosis was confirmed.
Pulmonary function test was performed by using the same USB spirometer at both sites (Koko pneumotachometer, nSpire Health, Inc., Longmont, CO) and protocol and equipment specifications that met American Thoracic Society standards.18 Pulmonary function tests were expressed as a percent of predicted values, utilizing prediction equations from Polgar and Promadhat19; however, since there are no established norms for Puerto Ricans or Dominicans, all ethnicities were classified as Caucasian for spirometric purpose.
Periodic group discussions of individually rated diagnostic cases were conducted in order to prevent drift and to insure reliability and consistent implementation of the manualized procedure. Meetings were conducted among asthma specialists internally at each site, and then across sites, both in-person and through quarterly teleconferences to agree upon whether newly enrolled participants had asthma, and to determine their asthma severity level. Any disagreement between clinicians on individual ratings was discussed until consensus was established. This process sometimes uncovered interesting differences between sites, such as widely varying reasons for utilizing emergency services or different expectations for level of symptom control. This process continued until consistent agreement in ratings was established.
Self-Report Assessments: Individual/Family Domain
Individual/Family Inherent Characteristics
Race/ethnicity
Race/ethnicity was an important inclusion variable of our design. A family was determined eligible if either biological parent self-identified as Puerto Rican, Dominican (independent of their self-identified race), or NLW and the child belonged to any of these three groups. The child’s race/ethnicity was determined by the primary caretaker (the biological mother in 94.2% of the cases, 2.3% of biological fathers, and 3.3% of other female relatives).
Asthma severity was determined by study clinicians. After medical history, physical examination, and pulmonary function testing, the clinician provided an assessment of asthma severity utilizing a visual worksheet that classified severity based on reported symptom frequency, pre-albuterol FEV1, and current controller medication dose. The worksheet was derived from both Global Initiative for Asthma (GINA) and NAEPP guidelines, and has been described in detail elsewhere.20 Severity was classified as “mild intermittent,” “mild persistent,” “moderate persistent,” or “severe persistent.”
Individual/Family Modifiable Characteristics
Beliefs about medication
Parental beliefs about asthma and medications relate to patterns of medication use and healthcare use. Data have indicated that relative to non-minority parents, minority parents’ concerns about asthma medication more frequently outweighed belief in the necessity of medication.21 Additionally, use of complementary alternative medicine (CAM), widely accepted in certain Latino groups,22 may delay timely treatment if used as an initial response to symptoms.23 In RIPRAC we used the Beliefs about Medicine Questionnaire24 to assess the perceived benefits and concerns about asthma medications.
Family asthma management
Medication Adherence Assessment
How patients understand and approach disease management may be central to understanding the process through which disparities in health outcomes may occur and medication adherence is an important component of this process. Research has demonstrated that minority children take significantly fewer doses of inhaled steroids relative to non-minority children,25 and these results persist when controlling for SES.26 During RIPRAC, actual adherence to inhaled asthma medications was assessed by electronic monitoring for metered-dose inhaler (MDI-Log device, Westmed/LifeLink Monitoring, Norcross, CA), and oral medication (TrackCap, Aardex, Inc., Union City, CA, www.aardexgroup.com), or by dosage counter when no electronic methods were available. Devices were attached to the child’s medications for 5 weeks between research sessions.
Symptom Perception
Children’s ability to accurately sense that asthma symptoms are occurring is required for treatment initiation and is an important factor in asthma management. The relation between deficits in perceptual accuracy of asthma symptoms and higher morbidity due to pediatric asthma has been demonstrated.27 While there exists no empirical evidence of cultural factors influencing asthma symptom perception, there are studies linking cultural differences to the perception and expression of pain,28 to the tendency to report physically unexplained symptoms,29 and to the expression of emotional distress.30 If Latino children have levels of perceptual accuracy that differ from NLW children, we would expect these differences to be associated with differences in asthma morbidity and healthcare utilization.
Our measurement of symptom perception is derived through a standardized method developed with our group.31,32 This method uses home-based spirometry. In brief, children are trained to use the device, a hand-held, programmable spirometer (the AM2; Jaeger USA/Viasys Healthcare, Yerba Linda, CA, www.viasy.shealthcare.com), capable of collecting pulmonary function indices and concurrent subjective estimates of pulmonary function. Over the course of approximately 5 weeks, children repeatedly estimate their peak flow, input it into the device, and then do a pulmonary function test. A month’s use provides subjective (PEFR “guess”) and objective (lung function parameter) data that are summarized into three scores: an “accuracy” score, a “danger zone” score, and a “symptom magnification” score.33
A Global Measure of Family Management
In addition to the above objective measures of medication adherence and symptom perception, we included a family-based assessment of disease management, the Family Asthma Management System Scale.34,35 The FAMSS is a 45-min semi-structured clinical interview that assesses family’s knowledge of the child’s illness, medication regimen; preventive steps, and response to symptoms; threshold and timeliness for seeking medical care; medication adherence, including use of complementary/alternative medications; and overall collaboration with their clinician. We conducted regular meetings to assess interview quality and comparability across both sites and in both languages. Both sites had a proportion of experienced bilingual raters who insured standard implementation of the interview, and who could provide input into consensus ratings for any possible interview.
The Social/Environmental Domain
Poverty
People with low incomes in general have poorer health and shorter life expectancy.36 In addition, minorities and poor individuals are more likely to engage in high-risk behaviors associated with asthma exacerbations such as smoking, and are also less likely to quit smoking than high-income populations.37,38 Because of this and because we were concerned that poverty might have different meaning and consequences in both sites we employed several measures of poverty and SES. Prior research in the island had shown that, contrary to other studies carried out in the mainland that demonstrated a relation between low SES and asthma morbidity across ethnic groups,12,39 studies in PR had not shown an association between the risk for asthma and income.3 We thus included multiple measures indicative of SES, including actual annual family income level, an “income to needs” ratio, perception of poverty, financial strain, parental level of education, and neighborhood characteristics.
The “income-to needs” ratio was calculated for each family by dividing yearly household family income by the poverty threshold for that family size.40,41 A family was considered at or below the poverty line if the ratio was less than or equal to 1.0 during year of study participation. Neighborhood characteristics were indexed by measures derived from the U.S. Census. Each participant’s address was geocoded to identify the census block group of the residence. In turn, the block group was characterized by the number of the following conditions reflected in the aggregate of all households in the block group: (1) household income less than 25% national average, (2) % less than high school graduate greater than 25% of national average, (3) % unemployed greater than 25% of national average, (4) % non-English speakers greater than 25% of national average, (5) % minority racial/ethnic status greater than 25% of national average, (6) % vacant housing greater than 25% of national average, (7) % small housing units greater than 25% of national average, and (8) % below poverty threshold greater than 25% of national average.
Allergens and triggers
Latinos have high rates of poverty relative to the majority group. As a result, many families living in poor neighborhoods are exposed to indoor and outdoor pollutants.42 Housing in low-income neighborhoods is also more likely to have poor ventilation and to have water leaks that allow a higher concentration of indoor allergens, and infestations of cockroaches, mites, and mice, allergens that are associated with asthma attacks.43 Our protocol included questionnaires that assessed exposure to most environmental allergens (e.g., environmental tobacco smoke, pet dander). However, we acknowledge that the use of questionnaires for the determination of environmental sampling typically underestimates exposure44 and is certainly a limitation of our study.
Neighborhood/environmental stress
Higher levels of neighborhood stresses (e.g., exposure to violence) have been associated with less optimal asthma management behaviors in urban children.45,46 To assess the extent to which neighborhood stressors accounted for the disparity observed we included a questionnaire on neighborhood disadvantage.47 In addition, we include additional indicators of SES that provide further description of the quality of families’ context based on caregiver report (e.g., poverty threshold, perception of poverty). As described above, we also included questionnaires that assessed common sources of stress among immigrants such as cultural stress.48,49
The Healthcare System
RIPRAC focused primarily on the individual/family domain in order to tailor future family-based interventions to address asthma disparities. For this reason, we did not conduct a comprehensive assessment of the healthcare system, but instead collected data on a salient variables in this domain, such as insurance, and access to health care was measured as part of the health policy component, and patient provider interaction and perception of discrimination were measured as features of the provider characteristics component (Figure 1).
Insurance and other barriers to care
We devised an instrument that assessed elements of the healthcare system that have been associated with healthcare disparities between Latinos and other groups in prior research, such as insurance status,50 type of insurance,51,52 lack of usual source of care,53 and poor access to care.
English language proficiency also appears to be a central predictor of healthcare use. For example, English language use and proficiency are related to healthcare access, healthcare use, and satisfaction with health care among Latinos.54,55 In the RIPRAC protocol we included questionnaires that assessed language proficiency, language use in different contexts, and language preference56,57 (see Table 1).
Provider/patient communication
The interaction of the patient/family and provider may have a significant effect on the ability to understand, appreciate, and follow through with treatment recommendations. Minorities report being treated with disrespect or being looked down upon more commonly (14.1% of Blacks, 19.4% of Latinos, and 20.2% of Asians) than NLWs (9.4%), and patients who report being treated with disrespect are less likely to receive optimal care for a chronic condition, or to follow their doctor’s advice.58 We included self-report measures on patient–provider communication59 and perceptions of discrimination60 to assess these elements of patient–provider interaction.
Asthma Outcomes
The term “asthma disparities” itself is evolving, and there is not yet a clear consensus as to which morbidity outcomes are relevant to include. We chose to be broad and inclusive in our RIPRAC outcomes of interest, under the premise that empirical data are first needed to determine the salient variables and included measures of asthma morbidity/control, quality of life, and healthcare utilization (past year utilization of the ED and hospitalization). The Asthma Functional Severity Scale61 assessed four components of asthma morbidity: frequency of episodes, frequency of symptoms between episodes, and level of impairment during and between episodes. The Pediatric Asthma Caregivers Quality of Life Questionnaire62 was employed to quantify health-related quality-of-life issues.
CONCLUSION
It is increasingly apparent that understanding ethnic and/or cultural disparities in asthma morbidity is a complicated process. Simple variables that lead directly to large differences in outcomes are not to be found, and methodologic approaches to studying the problem must reflect this complexity. This description of the RIPRAC methodology exemplifies the multimodal approach designed and implemented by experts in various disciplines, to assess important constructs in a number of domains.
Disparities research by definition involves cultural differences, but a project such as RIPRAC which was conducted in two different sites (Rhode Island and the island of Puerto Rico) under two remarkably different healthcare systems in both Spanish and English is especially challenging. The potential for artifact or “noise” to be introduced because of unintended methodologic differences—such as subtle inconsistencies in language due to translation problems, or biases resulting from different diagnostic practices—is substantial. The solutions entail rigorous training, constant reliability monitoring in every domain, and a high level of familiarity at each site of the realities of life at the other site. A methodologic approach that reflects the complexity of the problem of asthma disparities and that allocates sufficient resources to insure rigor and comparability is both costly and time consuming. It is only such an approach, however, that will allow us to move from documenting disparities to understanding them, and then ultimately to removing them.
CLINICAL IMPLICATIONS
The careful design and implementation of health disparities research are important preliminary steps in understanding and ultimately reducing disparities.
Acknowledgments
Funds for this study were provided by Grants # U01-Hl072438 (G. Canino and G. Fritz, P.I.s) from the National Heart, Lung and Blood Institute. Dr. Canino’s time was also supported by Grant # 5P60 MD002261-02 funded by the National Center for Minority Health Disparities.
ABBREVIATIONS
- FAMSS
Family Asthma Management System Scale
- NHLBI
National Heart, Lung and Blood Institute
- PR
Puerto Rican, Puerto Rico
- RI
Rhode Island
- RIPRAC
Rhode Island—Puerto Rico Asthma Center
- SES
socioeconomic status
- NLW
non-Latino white
References
- 1.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–1995. Am J Respir Crit Care Med. 2000;161:504–509. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 2.Beckett WS, Belanger K, Gent JF, Holford TR, Leaderer BP. Asthma among Puerto Rican Hispanics: a multi-ethnic comparison study of risk factors. Am J Respir Crit Care Med. 1996;154:894–899. doi: 10.1164/ajrccm.154.4.8887582. [DOI] [PubMed] [Google Scholar]
- 3.Cohen RT, Canino GJ, Bird HR, Shen S, Rosner BA, Celedon JC. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131:1331–1338. doi: 10.1378/chest.06-1917. [DOI] [PubMed] [Google Scholar]
- 4.Findley S, Lawler K, Bindra M, Maggio L, Penachio M, Maylahn C. Elevated asthma and indoor environmental exposures among Puerto Rican children of East Harlem. J Asthma. 2003;40:557–569. doi: 10.1081/jas-120019028. [DOI] [PubMed] [Google Scholar]
- 5.Loyo-Berrios N, Orengo J, Serrano-Rodriguez R. Childhood asthma prevalence in northern Puerto Rico, the Rio Grande, and Loíza experience. J Asthma. 2006;43:619–624. doi: 10.1080/02770900600878693. [DOI] [PubMed] [Google Scholar]
- 6.Ortega A, McQuaid E, Canino G, Ramirez R, Fritz G, Klein R. Association of psychiatric disorders and different indicators of asthma in island Puerto Rican children. Soc Psychiatry Psychiatr Epidemiol. 2003;38:220–226. doi: 10.1007/s00127-003-0623-6. [DOI] [PubMed] [Google Scholar]
- 7.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: Institute of Medicine; 2002. [Google Scholar]
- 9.Canino G, Koinis Mitchell D, Ortega A, McQuaid E, Fritz G, Alegria M. Asthma disparities in the prevalence, morbidity and treatment of Latino children. Soc Sci Med. 2006;63:2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Canino G, McQuaid E, Rand C. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123(6):1209–1217. doi: 10.1016/j.jaci.2009.02.043. NIHMS(93823):PN.ID: 19028025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Claudio L, Stingone JA, Godbold J. Prevalence of childhood asthma in urban communities: the impact of ethnicity and income. Ann Epidemiol. 2006;16:332–340. doi: 10.1016/j.annepidem.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 12.Claudio L, Tulton L, Doucette J, Landrigan P. Socioeconomic factors and asthma hospitalization rates in New York City. J Asthma. 1999;36:343–350. doi: 10.3109/02770909909068227. [DOI] [PubMed] [Google Scholar]
- 13.Canino G, Bravo M. The adaptation and testing of diagnostic and outcome measures for cross-cultural research. Int Rev Psychiatry. 1994;6:281–286. [Google Scholar]
- 14.Matías-Carrelo L, Chavez LM, Negrón G, Canino G, Aguilar-Gaxiola S, Hoppe S. The Spanish translation and cultural adaptation of five outcome measures. Cult Med Psychiatry. 2003;27:291–313. doi: 10.1023/a:1025399115023. [DOI] [PubMed] [Google Scholar]
- 15.Canino G, Shrout P, Alegría M, Rubio-Stipec M, Chavez L, Ribera J, Bravo M, Bauermeister J, Fabregas L, Horwitz S. Methodological challenges in assessing children’s mental health services utilization. Mental Health Serv Res. 2002;4:97–107. doi: 10.1023/a:1015252217154. [DOI] [PubMed] [Google Scholar]
- 16.National Heart, Lung and Blood Institute. Asthma statistics, Data fact sheet. Bethesda, MD: National Institute of Health; 2002. [Google Scholar]
- 17.Global Initiative for Asthma. Original: Workshop Report, Global strategy for asthma management and prevention. Global Strategy for Asthma Management and Prevention; 2002. [Google Scholar]
- 18.American Thoracic Society. Standardization of spirometry: 1994. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 19.Polgar G, Promadhat V. Pulmonary function testing in children: techniques and standards. Philadelphia: Saunders; 1971. [Google Scholar]
- 20.Esteban C, Klein RB, McQuaid E, Fritz G, Seifer R, Kopel S, et al. Conundrums in asthma severity, control, and healthcare utilization in children living in Puerto Rico and Rhode Island. J Allergy Clin Immunol. doi: 10.1016/j.jaci.2009.05.014. (in preparation) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conn K, Halterman J, Lynch K, Cabana M. The impact of parents’ medication beliefs on asthma management. Pediatrics. 2007;120:e521–e526. doi: 10.1542/peds.2006-3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bearison DJ, Minian N, Granowetter L. Medical management of asthma and folk medicine in a Hispanic community. J Pediatr Psychol. 2002;27:385–392. doi: 10.1093/jpepsy/27.4.385. [DOI] [PubMed] [Google Scholar]
- 23.Koinis-Mitchell D, McQuaid EL, Friedman D, Colon A, Soto J, Rivera DV, Fritz GK, Canino G. Latino caregivers’ beliefs about asthma: causes, symptoms, and practices. J Asthma. 2008;45:205–210. doi: 10.1080/02770900801890422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horne R, Weinman R. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 25.Bender BG, Wamboldt FS, O’Connor SL, Rand C, Szefler S, Milgrom H, et al. Measurement of children’s asthma medication adherence by self report, mother report, canister weight, and Doser CT. Ann Allergy Asthma Immunol. 2000;85:416–421. doi: 10.1016/s1081-1206(10)62557-4. [DOI] [PubMed] [Google Scholar]
- 26.McQuaid E, Kopel S, Klein R, Fritz G. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28:323–333. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 27.Fritz G, McQuaid E, Spirito A, Klein R. Symptom perception in pediatric asthma: relationship to functional morbidity and psychological factors. J Am Acad Child Adolesc Psychiatry. 1996;35:1033–1041. doi: 10.1097/00004583-199608000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Edwards R, Fillingim R. Ethnic differences in thermal pain response. Psychosom Med. 1999;61:316–323. doi: 10.1097/00006842-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Canino I, Rubio-Stipec M, Canino G, Escobar J. Functional somatic symptoms: a cross-ethnic comparison. Am J Orthopsychiatry. 1992;62:605–612. doi: 10.1037/h0079376. [DOI] [PubMed] [Google Scholar]
- 30.Zahn-Waxler C, Friedman RJ, Cole PM, Mizuta I, Hiruma N. Japanese and United States pre-school children’s response to conflict and distress. Child Dev. 1996;67:2462–2477. [PubMed] [Google Scholar]
- 31.Fritz GK, Adams SK, McQuaid EL, Klein R, Kopel S, Nassau J, et al. Symptom perception in pediatric asthma: resistive loading and in vivo assessment compared. Chest. 2007;132:884–889. doi: 10.1378/chest.06-2140. [DOI] [PubMed] [Google Scholar]
- 32.McQuaid EL, Koinis Mitchell D, Walders N, Nassau JH, Kopel SJ, Klein RB, et al. Pediatric asthma morbidity: the importance of symptom perception and family response to symptoms. J Pediatr Psychol. 2007;32:167–177. doi: 10.1093/jpepsy/jsj112. [DOI] [PubMed] [Google Scholar]
- 33.Klein RB, Walders N, McQuaid EL, Adams S, Yaros D, Fritz GK. The asthma risk grid: clinical interpretation of symptom perception. Allergy Asthma Proc. 2004;25:1–6. [PubMed] [Google Scholar]
- 34.Klinnert M, McQuaid E, Gavin L. Assessing the family asthma management system. J Asthma. 1997;34:77–88. doi: 10.3109/02770909709071206. [DOI] [PubMed] [Google Scholar]
- 35.McQuaid E, Walders N, Kopel S, Fritz G, Klinnert M. Pediatric asthma management in the family context: the family asthma management system scale. J Pediatr Psychol. 2005;30:492–502. doi: 10.1093/jpepsy/jsi074. [DOI] [PubMed] [Google Scholar]
- 36.Pearlman DN, Zierler S, Meersman S, Kim HK, Viner-Brown SI, Caron C. Race disparities in childhood asthma: does where you live matter? J Natl Med Assoc. 2006;98:239–247. [PMC free article] [PubMed] [Google Scholar]
- 37.Link BG, Phelan JC. Understanding sociodemographic differences in health—the role of fundamental social causes. Am J Public Health. 1996;86:471–473. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clark N, Brown R, Joseph C, Anderson E, Liu M, Valerio M, et al. Issues in identifying asthma and estimating prevalence in an urban school population. J Clin Epidemiol. 2002;55:870–881. doi: 10.1016/s0895-4356(02)00451-1. [DOI] [PubMed] [Google Scholar]
- 39.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in U.S. asthma mortality. Am J Public Health. 2000;90:1923–1925. doi: 10.2105/ajph.90.12.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Duncan GJ, Brooks-Gunn J. Consequences of growing up poor. New York: Russel Sage Publications; 1997. [Google Scholar]
- 41.U.S. Department of Health and Human Services. The 2005 HHS poverty guidelines. Washington, DC: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 42.Kattan M, Stearns SC, Crain EF, Stout JW, Gergen PJ, Evans R, III, et al. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. J Clin Immunol. 2005;116:1058–1063. doi: 10.1016/j.jaci.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 43.Rosenstreich D, Eggleston P, Kattan M, Baker D, Slavin R, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 44.Crain EF, Walter M, O’Connor GT, Mitchell H, Gruchalla RS, Kattan M, et al. Home and allergic characteristics of children with asthma in seven U.S. urban communities and design of an environmental intervention: the Inner-City Asthma Study. Environ Health Perspect. 2002;110:939–945. doi: 10.1289/ehp.02110939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the inner-city asthma study. Am J Public Health. 2004;94:625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Esteban C, Canino G, et al. Multiple urban and asthma-related risks and their association with asthma morbidity in children. J Pediatr Psychol. 2007;32:582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Resnick M, Bearman P, Blum R, Bauman K, Harris K, Jones J, et al. Protecting adolescents from harm. Findings in the National Longitudinal Study on Adolescent Health. J Am Med Assoc. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 48.Cervantes RC, Padilla AM, Salgado de Snyder N. Reliability and validity of the Hispanic Stress Inventory. Hispanic J Behav Sci. 1990;12:76–82. [Google Scholar]
- 49.Cervantes R, Padilla A, Salgado de Snyder W. The Hispanic Stress Inventory: a culturally relevant approach to psychological assessment. Psychol Assessment. 1991;3:438–447. [Google Scholar]
- 50.Flores G, Abreu M, Chaisson C, Meyers A, Sachdeva R, Fernandez H, et al. A randomized controlled trial of the effectiveness of community-based case management in insuring uninsured Latino children. Pediatrics. 2005;116:1433–1441. doi: 10.1542/peds.2005-0786. [DOI] [PubMed] [Google Scholar]
- 51.Ortega A, Belanger K, Paltiel A, Horwitz SM, Bracken MB, Leaderer BP. Use of health services by insurance status among children with asthma. Med Care. 2001;39:1065–1074. doi: 10.1097/00005650-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 52.Zambrana R, Carter-Pokras O. Improving health insurance coverage for Latino children: a review of barriers, challenges and state strategies. J Natl Med Assoc. 2004;96:508–523. [PMC free article] [PubMed] [Google Scholar]
- 53.Ortega A, Gergen P, Paltiel A, Bauchner H, Belanger K, Leaderer B. Impact of site care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109:E1. doi: 10.1542/peds.109.1.e1. [DOI] [PubMed] [Google Scholar]
- 54.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152:1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 55.Morales L, Cunningham W, Brown J, Liu H, Hays R, Liu H, et al. Are Latinos less satisfied with communication by health care providers? J Gen Am Med Assoc. 1999;14:409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Felix-Ortiz M, Newcomb MD, Myers H. A multidimensional measure of cultural identity for Latino and Latina adolescents. Hispanic J Behav Sci. 1994;16:99–115. [Google Scholar]
- 57.Marin G, Sabogal F, VanOss Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic J Behav Sci. 1987;9:183–205. [Google Scholar]
- 58.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53:721. [PubMed] [Google Scholar]
- 59.Little P, Dorward M, Warner G, Stephens K, Senior J, Moore M. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referral, and prescribing in primary care: nesting observational study. Br Med J. 2004;328:444. doi: 10.1136/bmj.38013.644086.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jackson J, Williams D Detroit Area Study. 1995: social influence on health: stress, racism, and health protective resources. Ann Arbor, MI: University of Michigan; 1995. [Google Scholar]
- 61.Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. Am J Respir Crit Care Med. 1994;149:1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- 62.Juniper E, Guyatt G, Feeny D, Ferrie P, Griffith L, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 63.Gore S, Aseltine R, Colton M. Social structure, life stress and depressive symptoms in high school-aged population. J Health Soc Behav. 1992;33:97–113. [PubMed] [Google Scholar]
- 64.Penza-Clyve S, Zeman J. Initial validation of the Emotional Expression Scale for Children (EESC) J Clin Adolesc Psychol. 2002;31:540–547. doi: 10.1207/S15374424JCCP3104_12. [DOI] [PubMed] [Google Scholar]
- 65.Garber J, Walker L, Zeman J. Somatization symptoms in a community sample of children and adolescents: further validation of the Children’s Somatization Inventory. J Consult Clin Psychol. 1991;3:588–595. [Google Scholar]
- 66.Kroenke K, Spitzer R, Williams J. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]