Access to effective but unfunded cancer drugs varies across Canada. Policymakers must consider whether this is consistent with articulated values of the system and whether currently planned processes address these inconsistencies.
Abstract
Purpose:
New anticancer drugs are improving outcomes for patients with cancer but at significant cost, and some publically funded health care systems have chosen not to fund these medications. Accessing these unfunded drugs concerns patients, challenges their physicians, and raises important policy and legal issues. We assessed Canadian medical oncologists' access to and attitudes toward accessing unfunded intravenous cancer drugs.
Methods:
Two hundred twenty-two Canadian medical oncologists outside of Québec were surveyed.
Results:
Response rate was 62% (138 of 222). Respondents could access unfunded cancer drugs (49% at their government-funded hospitals; 70% at nongovernment-funded private infusion clinics), but access varied across the country. A majority of respondents (52% to 67%) were comfortable with accessing unfunded drugs in their own institutions and uncomfortable with accessing these drugs in private clinics in Canada or the United States (52% to 61%), but substantial minorities had opposing opinions. The majority of respondents felt all methods of accessing unfunded intravenous cancer drugs should be available (76% in their own center; 60% in private clinics) and used these methods to access these medications (81% in their own institution; 62% in private clinics).
Conclusion:
Access to effective but unfunded cancer drugs varies across Canada. Policymakers need to consider whether this is consistent with articulated values of the system and whether currently planned processes address these inconsistencies. Key stakeholders need to consider the merits of the different means of accessing these drugs to appropriately and fairly integrate access into publically funded health care systems like that of Canada and other systems like that of the United States, which could face similar limits in the future.
Introduction
Newly developed cancer therapies have been improving outcomes for patients with cancer in modest increments but at significantly higher costs,1 challenging publically funded health care systems like that of Canada, which face constrained resources. The Canada Health Act,2 the federal statute governing health care in Canada, states “that continued access to quality health care without financial or other barriers will be critical to maintaining and improving the health and well-being of Canadians” and requires that provincial governments fund “medically necessary” intravenous (IV) drugs administered in hospitals. The specific process each province uses to make drug-funding decisions varies, but many Canadian provinces have been cooperating in the interim Joint Oncology Drug Review3 process that uses comparative and cost-effectiveness data to make drug-funding decisions. The Canadian system differs from the nonuniversal, multipayer US system, which rarely implements comparative effectiveness evidence in coverage decisions. Some Canadian provinces have not funded some of these expensive new medications when they have not met cost-effectiveness benchmarks, even for drugs that have demonstrated survival benefits and been endorsed in rigorous evidence-based guidelines. For example, for the treatment of metastatic colorectal cancer, funding for the monoclonal antibodies to the epidermal growth factor receptor (ie, cetuximab and panitumumab) not available in all provinces. Bevacizumab is now funded in almost all provinces for the treatment of metastatic colorectal cancer. Some provinces funded the drug soon after the first randomized trial was published, but it was rejected for funding in several provinces based on their economic analyses, and many years elapsed before most provinces funded the drug.
In provinces where these drugs are not funded, they are only available to patients who can pay for them (out of pocket or through private insurance) in nongovernment-funded private infusion clinics or in some government-funded public hospitals. In health care systems like those of Canada and the United Kingdom, in which access to appropriate medications, in particular in public hospitals, has traditionally been based on medical need and not ability to pay, integrating access to these medications has challenged medical oncologists, policymakers, and legal analysts.4,5 A national advocacy group has noted the variation in provincial access and means of accessing IV and oral cancer drugs in Canada.6–8 However, there has been only limited systematic assessment9 of how Canadian cancer physicians are accessing these unfunded drugs for their patients or their attitudes regarding this complex new treatment environment. In this study, we report on a national survey assessing Canadian medical oncologists' access to unfunded IV cancer drugs and their attitudes regarding the different means of accessing them.
Methods
The section of the survey assessing the use of and attitudes toward the methods of accessing unfunded cancer drugs was part of a broader survey on the value of new cancer medications. Results of other sections of the survey have been reported elsewhere.10 The component reported here (full text available in the Data Supplement) assessed medical oncologists' access to effective IV drugs, where effective was defined as “a drug that has shown a clinically significant improvement in survival for the treatment of a metastatic cancer in larger randomized phase III trials and has been recommended for use by a respected provincial evidence-based guideline group.” We assessed the following: first, which means of accessing unfunded cancer drugs was available to medical oncologists (including where [at their government-funded institution, in a nongovernment-funded private infusion clinic, and/or in the United States] and how [through private insurance or out-of-pocket payment]); and second, the medical oncologists' use of and opinions regarding the different means of accessing unfunded drugs. The survey was pilot tested before use to ensure coherence and the face and content validity of the instrument.
We distributed the survey to all 356 Canadian medical oncologists identified using the following sources to ensure completeness: the Canadian Association of Medical Oncologists membership list, the Canadian Medical Directory, and the directory of Fellows of the Royal Canadian College of Physicians and Surgeons. Participants received an e-mail invitation to complete a Web-based version of the survey as well as a hardcopy version by mail. Resources were not available for translation of the survey into French (and the requisite translation of comments back into English), and the response rate from oncologists in Québec was therefore inordinately low (13%). To exclude these potentially biased data from our study, results were included only from provinces where responses would not have been influenced by the language of the survey (N = 222). Reminders were sent via e-mail to enhance the response rate. All respondents were surveyed between February and April 2008. The Research Ethics Board of Sunnybrook Health Sciences Centre approved the study.
Descriptive statistics were used to characterize respondent demographics and their access to unfunded cancer drugs. Univariate logistic regression analysis was performed to determine if accessing unfunded cancer drugs (ie, means, comfort level, whether means should be available) was influenced by any of the key demographic characteristics of respondents. Only one demographic characteristic was ever statistically significantly related to accessing unfunded cancer drugs, so multivariate analyses were not required. A two-sided P value of less than .05 was considered statistically significant. SAS version 9.2 for Windows (SAS Institute, Cary, NC) was used. To ensure confidentiality, data from individual provinces where there were fewer than five respondents were pooled with similarly responding provinces so that reported responses could not be identified as responses from individuals.
Results
One hundred thirty-eight medical oncologists responded, representing a response rate of 62% (138 of 222). Respondent demographics are listed in Table 1. In the Canadian system, all oncologists practice in government-funded institutions—either in university-based centers (generally affiliated with comprehensive cancer centers), non–university-affiliated comprehensive cancer centers, or non–university-affiliated community practices based at general hospitals. Oncologists do not practice at the private clinics referred to throughout the study; these are nongovernment-funded clinics established for the infusion of unfunded cancer systemic therapies.
Table 1.
Participant Demographics (N = 138)
| Demographic | % |
|---|---|
| Sex | |
| Male | 63 |
| Female | 37 |
| Graduation year | |
| < 1966 | 3 |
| 1966-1975 | 24 |
| 1976-1985 | 22 |
| 1986-1995 | 26 |
| > 1995 | 25 |
| Practice setting | |
| University-based practice | 64 |
| Comprehensive cancer center (non–university affiliated) | 22 |
| Community-based practice | 14 |
| Respondents by province | |
| Ontario | 51 |
| British Columbia | 18 |
| Alberta | 18 |
| Nova Scotia | 7 |
| Manitoba, Prince Edward Island, Newfoundland, New Brunswick | 6 |
| Disease site* | |
| Breast | 59 |
| GI | 57 |
| Lung | 48 |
| Genitourinary | 33 |
| Hematologic | 28 |
| Gynecologic | 22 |
| Melanoma | 22 |
| Head and neck | 20 |
| Sarcoma | 17 |
| Other | 7 |
| Half-day clinics per week | |
| < 5 | 22 |
| 5-7 | 60 |
| > 7 | 17 |
Not mutually exclusive.
Means of Accessing Unfunded Cancer Drugs
Half of respondents nationally had access to unfunded cancer drugs for their patients at their hospital (49% via patients paying out of pocket, 51% via patients' private insurance), whereas approximately two thirds of respondents had access to unfunded drugs via private clinics or clinics in the United States (70% via patients paying at a private clinic; 68% via private insurance at a private clinic, 67% via clinics in the United States). However, there were differences in access across the country.
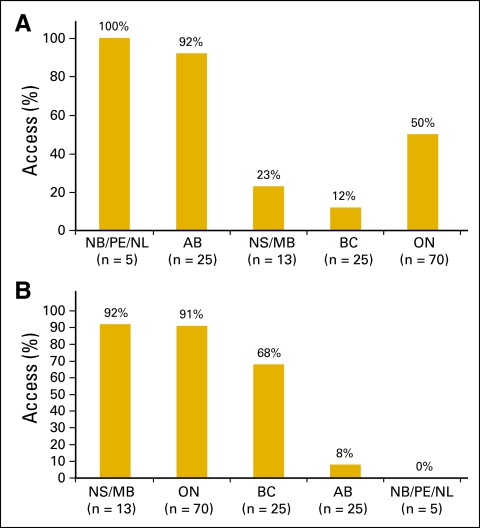
The respondent's province of origin was the only demographic characteristic that was statistically significantly associated with where they could access unfunded cancer drugs. Figure 1A summarizes proportions of respondents from different provinces accessing unfunded cancer drugs at their own institutions. Alberta had a statistically significantly higher rate of access to unfunded drugs in respondents' own institutions compared with Ontario (92% v 49%, P < .001). All respondents from New Brunswick, Prince Edward Island, and Newfoundland had access in their own institutions, but there were only a total of five respondents from these provinces. Respondents in British Columbia had lower rates of access to unfunded drugs in their own institutions compared with Ontario (out-of-pocket payment: British Columbia, 12% v Ontario, 49%, P = .001; private insurance: British Columbia, 12% v Ontario, 50%, P = .006).
Figure 1.
(A) Access to unfunded drugs in Canada at respondent's institution. (B) Access to unfunded drugs in private clinics. Results are for access via private insurance. Access via out-of-pocket payment was essentially the same (Data Supplement). AB, Alberta; BC, British Columbia; MB, Manitoba; NB, New Brunswick; NL, Newfoundland; NS, Nova Scotia; ON, Ontario; PE, Prince Edward Island.
Figure 1B summarizes proportions of respondents accessing unfunded drugs at private clinics. The majority of respondents from Manitoba, Nova Scotia, Ontario, and British Columbia had access. Respondents from Alberta had a statistically significantly lower rate of access to unfunded drugs in private clinics compared with Ontario (8% v 93%, P < .001). No respondents from New Brunswick, Prince Edward Island, and Newfoundland had access to unfunded drugs in private clinics (n = 5).
The majority of respondents had access to unfunded drugs in US clinics in New Brunswick (100%) and Ontario (86%), with a minority having access to US clinics in Prince Edward Island, Nova Scotia, and Manitoba (29%). Approximately half of respondents had access to unfunded cancer drugs in the United States in British Columbia (56%), Alberta (52%), and Newfoundland (50%).
Comfort With Accessing Unfunded Drugs Through Different Methods
Table 2 summarizes respondents' comfort levels with accessing unfunded cancer drugs. A majority of respondents (52% to 67%) were comfortable with accessing unfunded drugs in their own institutions but were uncomfortable with accessing these drugs in private clinics in Canada or the United States (52% to 61%). However, a substantial minority of patients were uncomfortable accessing drugs in their own institutions (23% to 43%) or comfortable with accessing drugs in private clinics or in the United States (32% to 40%). Overall, respondents were more comfortable with accessing unfunded drugs through their patients' private insurance compared with methods that required patients to pay out of pocket.
Table 2.
Comfort With Different Methods of Accessing Unfunded Cancer Drugs
| Setting | Very or Somewhat Comfortable (%) | Neither Comfortable nor Uncomfortable (%) | Very or Somewhat Uncomfortable (%) |
|---|---|---|---|
| Hospital | |||
| Out of pocket | 52 | 5 | 43 |
| Private insurance | 67 | 10 | 23 |
| Private clinic | |||
| Out of pocket | 32 | 7 | 61 |
| Private insurance | 40 | 8 | 52 |
| US clinic | 34 | 11 | 55 |
NOTE. Respondents who replied “don't use” were excluded.
In the univariate logistic regression analysis, only the respondent's practice setting was associated with comfort with the various means of accessing these medications. Respondents from community practice settings were more likely to be comfortable or very comfortable with accessing drugs at their own institutions compared with those practicing in the university setting (88% v 47% for out-of-pocket access at their own institutions, P = .0063; 94% v 66% for private insurance access at their own institutions, P = .021).
Attitudes on Which Methods for Accessing Unfunded Drugs Should Be Available
The majority of respondents felt that all methods of accessing unfunded IV cancer drugs should be available (76% in the respondent's own institution; 60% in private clinics) and used these methods to access these medications for their patients (81% in their own institutions; 62% in private clinics). In univariate logistic regression analysis, again only the respondent's practice setting influenced respondents' opinions regarding where unfunded drugs should be available. Respondents in the community practice setting were more likely than respondents at comprehensive cancer centers to believe that unfunded drugs should be available at their treatment facilities by private insurance payment (95% v 67%, P = .022).
Discussion
This study describes medical oncologists' access to unfunded cancer drugs for their patients and their attitudes toward the means of accessing these drugs in a publically funded system in which payers have restricted access to some effective drugs. Our survey revealed that approximately two thirds of respondents had access to these drugs at private clinics, and approximately half had access to these drugs at their own hospitals. However, access varied across Canada. Most respondents were comfortable with their patients accessing unfunded drugs in their hospitals and were uncomfortable with their patients accessing unfunded drugs in private clinics, but substantial minorities had opposing opinions. Despite varying comfort levels, most respondents felt all of these means of accessing unfunded cancer drugs should be available and used these methods.
The Cancer Advocacy Coalition of Canada 6–8 has noted the variation in provincial access and means of accessing IV and oral cancer drugs in Canada. Our systematic study confirms this provincial variation and provides a quantitative description of the substantial variation between the different provinces. Publically funded health care systems need to make difficult choices on which of the new and expensive cancer medications they fund, given the resource constraints they face. However, the impact of policymakers' decisions on providers and patients must be considered in light of the articulated values of the health care system. The patchwork availability of many effective IV cancer drugs across the country seems inconsistent with the requirement of the Canada Health Act2,6 that medically necessary medications be provided in hospitals without financial barriers and the ethical principle of fundamental justice. There are some uniquely Canadian features to the legal and policy issues surrounding accessing appropriate but unfunded treatments,4 but other similar systems face similar challenges.5 Since 2007, there has been an attempt to improve consistency of cancer drug funding decisions across the country through the interim Joint Oncology Drug Review2 (and its replacement, the pan-Canadian Oncology Drug Review process, which began in November 2011), but challenges remain because the decisions of these bodies are not binding for participating provinces.2,11 In Ontario, policymakers developed guidelines to ensure geographic equity in accessing unfunded IV cancer drugs in public hospitals.12 However, we found only 50% of medical oncologists in Ontario had access to unfunded cancer drugs in their own institutions, likely because of uneven implementation of the guidelines. Clearer policies on how these drugs should be accessed within their systems might improve the fairness of access to these medications in Canada and other countries with publically funded health care systems.5 Variation in access and use of US clinics across the country are likely largely functions of geography and the ease of access to US oncology centers among the population centers of a province.
Our study also examined medical oncologists' comfort levels with different means of accessing appropriate treatments when payers limit access. Most physicians were more comfortable with patients accessing unfunded drugs in their own institutions than in private clinics, but substantial minorities had opposing opinions. It is unclear whether the different comfort levels were related to issues that have been identified (ie, patient safety and continuity of care or moral distress regarding equal access4,5) or to other issues. Further study using qualitative methods might provide a deeper understanding of oncologists' comfort levels in this complex environment and how respondents' practice setting influenced their comfort levels. The varied comfort levels with the means of accessing appropriate but unfunded treatments suggests that further discussion among key stakeholders should be encouraged, so advantages and disadvantages of the different means of providing these drugs can be better understood, and substantive concerns can be addressed.
The findings that the majority of respondents felt that all means of accessing unfunded drugs should be available and that they used these methods despite varying comfort levels are consistent with previous findings. A previous qualitative study of Canadian medical oncologists that found that when faced with limits on appropriate treatment options for their patients, they advocated for access to those treatments.13 The finding that the majority of respondents felt that all means of accessing unfunded cancer drugs should be available does not necessarily lead to the conclusion that all methods ought to be available. However, the results of this study might be able to stimulate and inform the political, ethical, and legal debates that surround which of the different means of providing unfunded IV cancer drugs4,5 should be available in publically funded health care systems.
Respondents from a community practice were more likely than their colleagues in other settings to be more comfortable with their patients accessing unfunded drugs in their own institutions and in their belief that unfunded drugs should be available in their institutions in some circumstances. Although further study would be required to determine the reasons for these differing opinions, they may result from the fact that community oncologists work in smaller practices and hospitals than their counterparts at university- or community-based comprehensive cancer centers. Smaller centers may have been better able to accommodate the smaller numbers of patients requiring certain unfunded cancer drugs in the past, allowing the physicians there to become more comfortable with the practice.
There are some limitations to our study. Our estimates regarding access and attitudes are limited by the exclusion of oncologists in Québec and the small numbers of respondents from provinces with only a few oncologists (Newfoundland, Prince Edward Island, New Brunswick, Manitoba); however, these are unlikely to have changed our major finding that access to unfunded IV cancer drugs varied across the country. Finally, the issues involved in accessing unfunded cancer drugs are in constant evolution, and our findings describe only one point in time. However, variability in access to cancer drugs remains a concern in Canada11 and other publically funded systems5 and may emerge as an issue in the US system.14
Smith et al14 recently suggested that the US cancer care system will be sustainable only if some limits on cancer care, based on cost-effectiveness or comparative-effectiveness data, are accepted. The findings of this study could be helpful to the United States if limits to care become a reality, and US patients, oncologists, and policymakers must deal with varied access to effective but unfunded cancer drugs. How can a Canadian study be helpful to the United States when their health care systems are so different? Despite the differences between the two health care systems that we described in a recent report,10 US and Canadian oncologists have generally similar attitudes regarding the costs and cost effectiveness of cancer medications and related health policies. Indeed, a majority of US and Canadian oncologists favored the use of more cost-effectiveness data in drug coverage decisions and access to effective cancer treatments only if they are cost effective. This may reflect that “American oncologists are beginning to come to terms with the unavoidable reality of resource constraints and may suggest some willingness of American oncologists to accept comparative cost-effectiveness data in drug coverage decisions as is already happening in Canada and other countries.”10(p4152) If that is so, the United States could benefit from lessons learned from studies like this one in countries like Canada, where patients and oncologists are already facing the reality of these restraints.
In summary, limits on funding of new cancer medications because of their high costs have resulted in substantial variation in access to appropriate treatments in a large publically funded health care system. Policymakers need to consider whether their decisions are consistent with the articulated values of their systems and, if not, whether currently planned processes will appropriately address these inconsistencies. Key stakeholders need to consider the advantages and disadvantages of the different means of accessing effective but unfunded cancer drugs so that access to these medications can be appropriately and fairly integrated into publically funded health care systems like that of Canada. Lessons learned from studies like this in publically funded systems might inform policymakers in multipayer systems like that of the United States if limiting access to effective cancer drugs to cope with the rising costs of cancer care is required in the future.
Supplementary Material
Acknowledgment
We thank Ms Liying Zhang for statistical analysis and Ms Charlene Wainwright for assistance in preparing this article. Supported in part by the Canadian Association of Medical Oncologists.
C.M.B. is supported by a Canadian Institutes of Health Research and Canadian Patient Safety Institute Chair in Patient Safety and Continuity of Care.
S.R.B., W.K.E., and C.M.B. are members of the pan-Canadian Oncology Drug Review Expert Review Committee; however, the views expressed in this article are those of the authors.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: All authors
Administrative support: Scott R. Berry, Chaim M. Bell
Provision of study materials or patients: Scott R. Berry
Collection and assembly of data: All authors
Data analysis and interpretation: Scott R. Berry, William K. Evans, Chaim M. Bell
Manuscript writing: All authors
Final approval of manuscript: All authors
References
- 1.Schrag D. The price tag on progress: Chemotherapy for colorectal cancer. N Engl J Med. 2004;351:317–319. doi: 10.1056/NEJMp048143. [DOI] [PubMed] [Google Scholar]
- 2.Canada Health Act. RSC. 1985 [Google Scholar]
- 3.Savage C. Report Card on Cancer in Canada. Volume 12. Toronto, Ontario, Canada: Cancer Advocacy Coalition; 2010. From JODR to pCODR; p. 36. [Google Scholar]
- 4.Flood CM, Hardcastle L. Tough choices: Private sale of drugs in public hospitals. CMAJ. 2010;182:374–376. doi: 10.1503/cmaj.081137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chafe R, Dhalla IA, Dobrow M, et al. Accessing unfunded cancer drugs in publicly funded hospitals. Lancet Oncol. 2009;10:306–307. doi: 10.1016/S1470-2045(09)70039-7. [DOI] [PubMed] [Google Scholar]
- 6.Khoo K, Ragaz J, Hryniuk W, et al. Report Card On Cancer in Canada. Volume 8. Toronto, Ontario, Canada: Cancer Advocacy Coalition; 2006. Cancer drug access in Canada; pp. 26–38. [Google Scholar]
- 7.Khoo K, Ragaz J, Hryniuk W, et al. Report Card on Cancer in Canada. Volume 9. Toronto, Ontario, Canada: Cancer Advocacy Coalition; 2007. Cancer drug access in Canada, part two: One year later—Are we making progress? pp. 18–30. [Google Scholar]
- 8.Khoo K, Colucci R, Hryniuk W, et al. Report Card on Cancer in Canada. Volume 10. Toronto, Ontario, Canada: Cancer Advocacy Coalition; 2008. The new wave of cancer drugs; pp. 43–52. [Google Scholar]
- 9.Chan K, Berry SR, Strauss S, et al. Canadian medical oncologists' practice and perception on accessing new drugs for patients with metastatic colorectal cancer: A national survey. J Clin Oncol. 2008;26(suppl):361s. abstr 6600. [Google Scholar]
- 10.Berry SR, Bell CM, Ubel PA, et al. Continental divide? The attitudes of US and Canadian oncologists on the costs, cost-effectiveness, and health policies associated with new cancer drugs. J Clin Oncol. 2010;28:4149–4153. doi: 10.1200/JCO.2010.29.1625. [DOI] [PubMed] [Google Scholar]
- 11.Vogel L. Pan-Canadian review of cancer drugs will not be binding on provinces. CMAJ. 2010;182:887–888. doi: 10.1503/cmaj.109-3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cancer Care Ontario. Toronto, Ontario, Canada: Cancer Care Ontario; 2006. Report of the Provincial Working Group on the Delivery of Oncology Medications for Private Payment in Ontario Hospitals. [Google Scholar]
- 13.Berry SR, Hubay S, Soibelman H, et al. The effect of priority setting decisions for new cancer drugs on medical oncologists' practice in Ontario: A qualitative study. BMC Health Serv Res. 2007;7:193. doi: 10.1186/1472-6963-7-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364:2060–2065. doi: 10.1056/NEJMsb1013826. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.