Abstract
Background
Associations between modifiable health risk factors during middle age with disability and mortality in later life are critical to maximizing longevity while preserving function. Positive health effects of maintaining normal weight, routine exercise, and non-smoking are known for the short and intermediate term. We studied the effects of these risk factors into advanced age.
Methods
A cohort of 2,327 college alumnae ≥60 years was followed annually (1986–2005) by questionnaires addressing health risk factors, history, and Health Assessment Questionnaire disability (HAQ-DI). Mortality data were ascertained from the National Death Index. Low, medium, and high risk groups were created based upon the number (0, 1, ≥2) of health risk factors (overweight, smoking, inactivity) at baseline. Disability and mortality for each group were estimated from unadjusted data and regression analyses. Multivariable survival analyses estimated time to disability or death.
Results
Medium and high-risk groups had higher disability than the low risk group throughout the study (p<0.001). Low-risk subjects had onset of moderate disability delayed 8.3 years compared with high-risk. Mortality rates were higher in the high risk group (384 versus 247 per 10,000 person-years). Multivariable survival analyses showed the number of risk factors to be associated with cumulative disability and increased mortality.
Conclusions
Seniors with fewer behavioral risk factors during middle age have lower disability and improved survival. These data document that the associations of lifestyle risk factors upon health continue into the ninth decade.
Keywords: disability, aging, mortality, exercise, smoking, weight, longitudinal study
Introduction
Improvement in health in the United States has resulted in greater longevity, raising concerns about increased frailty and disability in an increasingly aging population1,2. Potential consequences of increasing age-related disability include higher health costs and decreased quality of life. Alternatively, if reduction in health risks postpones disability to a greater degree than it extends life, health burdens of age may decrease3. We sought to examine the hypothesis that health gains associated with fewer health risks would continue through the ninth decade of life.
Behavioral risk factor reduction is a potentially cost-effective means to improve long-term health outcomes. Most studies have evaluated risk factors individually rather than as a summation4–7. Few have followed subjects into advanced age, essential for estimation of cumulative lifetime health.
In 1998, we reported our eight-year experience on the relationship of health-related risk factors to cumulative disability in a cohort of University of Pennsylvania alumni from 1939–1940. We found that fewer health-related risks (smoking, overweight, and inactivity) led to increased survival and decreased disability11. The relative improvements in death rates and disability incidence could not be reliably estimated given relatively few deaths and young age of 68 among survivors. Here, we examine the long-term associations of cumulative risk factors upon disability and mortality to an average age of 85 years with nearly 50% mortality.
Methods
In 1986, we initiated a longitudinal study of risk factors for progressive disability and mortality in a previously identified cohort of college alumni12, inviting individuals from University of Pennsylvania alumni records in 1939 and 1940. Respondents (n=2843) were followed annually with mailed self-administered questionnaires11.
Participants
Participants averaged 68-years of age at baseline and had completed at least two consecutive questionnaires between 1986–2005 (n=2,327). The observation period for each participant was time from baseline questionnaire through death, last completed questionnaire, or end of the observation period, December 2005.
Variables
Self-reported data were collected on demographics, physical function, and selected risk factors. We chose body mass index (BMI), cigarette smoking, and physical inactivity as modifiable risk factors frequently associated with impaired functional status and premature mortality13–15. Health risk factors were defined at initial survey: (1) being above or below a normal weight range (abnormal BMI), defined by National Heart Lung and Blood Institute (NHLBI) guidelines16, as a BMI > 25 or < 18.5 kg/m2; (2) current cigarette smoking; and (3) inactivity, defined as absence of vigorous physical activity that works up a sweat (including jogging, cycling, brisk walking, swimming and other sports). Questionnaires captured data on the prevalence of comorbid conditions including hypertension, diabetes, arthritis, stroke, cancer, depression, cardiovascular, pulmonary, neurologic and gastrointestinal diseases. Subjects estimated walking pace using an ordinal scale: 1=casual or strolling (less than 2 mph); 2=average or normal (2 mph); 3=fairly briskly (3 mph); 4=brisk or striding (4 mph or faster).
Group assignment
Participants were placed into three risk groups based upon the number of baseline risk factors: low (no risk factors), medium (one risk factor), and high (≥ two risk factors). Primary outcomes were time to disability and death.
Disability Assessment
Disability was assessed by the Health Assessment Questionnaire Disability Index (HAQ-DI), a validated measure widely used in clinical studies17,18. It assesses functional ability in eight categories: rising, dressing and grooming, hygiene, eating, walking, reach, grip, and routine household activities18. Each is scored from 0 (no difficulty) to 3 (unable to do) after accounting for assistive devices or help of another person. The disability index averages the individual category scores, yielding a score from 0 to 3. For reference, a HAQ–DI of 0.25 is roughly equivalent to mild disability in 1–2 functional categories; 0.5 to moderate disability in two categories. Disability scores of 0.75 to 1.0 are typical of subjects with rheumatoid arthritis and osteoarthritis19–21.
We examined three disability endpoints: (1) HAQ-DI for each calendar year of observation; (2) cumulative disability over the period of observation (sum of annual HAQ-DI scores); and (3) time to development of moderate disability (HAQ-DI=1).
Mortality Assessment
Mortality data for all study participants through 2005 was ascertained using the National Death Index22.
Statistical Methods
Baseline characteristics were compared using means and proportions. Because some comorbidities are singular events (stroke, myocardial infarction) and may not be reported on subsequent questionnaires, baseline and cumulative prevalence was tabulated. Unadjusted mean baseline HAQ-DI scores were compared by study group. Similarly, annual and cumulative disability scores in low-risk subjects were compared to medium- and high-risk groups using Student t-tests. Kaplan-Meier curves were used to compare time to first HAQ-DI=1.0 (moderate disability) and mortality between groups. Multivariable Cox proportional hazard models were created for the development of moderate disability and time to death to control for variables known to affect outcomes (age, gender, baseline disability, walking pace23, and comorbidities). Time to moderate disability and to mortality was estimated both from the unadjusted data and from linear regression of all data points.
To understand the relative roles of each risk factor (overweight, smoking, and inactivity), we constructed multivariable Cox proportional hazard models using each separate risk factor as covariates. Given that higher baseline HAQ-DI scores are strongly correlated with both future disability and mortality24,25, we performed these analyses on the subset of participants with zero baseline disability (n=1,736, 75% of subjects). Models were adjusted for age, gender, walking pace, and comorbidities.
Population attributable risk (PAR) for mortality and for moderate disability (HAQ-DI=1) was calculated for each individual risk factor as well as for individuals with ≥ 1 risk factor. PAR were calculated separately for the entire cohort, subjects with baseline HAQ-DI=0, and for survivors with baseline HAQ-DI=0. Analyses were performed with SAS [Carey NC]; a two-sided test with p<0.05 was considered statistically significant. This study received IRB approval and all participants provided written informed consent.
Results
At baseline, participants had a mean age of 68 years and were predominately Caucasian and male as expected from university alumnae in 1939–1940. Mean BMI was 24.7kg/m2; 41% (n=985) had a BMI>25kg/m2 and 1.3% (n=31) <18.5kg/m2. Eight percent (n=190) smoked; 52% (n=1,213) were inactive. Pair-wise correlations between overweight and inactivity were −0.07 (p=0.34) among smokers and −0.06 (p=0.006) among nonsmokers.
Risk groups were composed as follows: Low (n=605, 25.9%); Medium (n=1,073; 46.1%); High (n=649; 27.9%). Cohort characteristics by risk group at baseline and last follow-up are shown in Table 1. Risk groups were comparable in gender, ethnicity, baseline age and years of education.
Table 1.
Demographic, Risk Factors, and Outcomes by Risk Group
| Low Risk (0 Risk Factors) |
Medium Risk (1 Risk Factor) |
High Risk (2–3 Risk Factors) |
||||
|---|---|---|---|---|---|---|
| Baseline | Last | Baseline | Last | Baseline | Last | |
| Number of Subjects | 605 | 1073 | 649 | |||
| Men (%) | 76.5 | 77.1 | 78.0 | |||
| Education (years, SD) | 17.5 (1.7) | 17.5 (1.8) | 17.4 (1.8) | |||
| At Baseline and At Last Observation | ||||||
| Age (years, SD) | 67.8 (3.3) | 84.9 (2.3) | 68.1 (3.7) | 85.0 (2.4) | 68.1 (3.8) | 85.4 (3.0) |
| Smokers (%) | 0 | 1.0 | 4.4 *** | 1.6 | 22.0 *** | 11.2 *** |
| BMI§, kg/m2 | 22.9 (1.4) | 22.9(2.4) | 24.5 (3.0)*** | 24.2 (3.4) *** | 26.7 (3.4)*** | 25.8 (4.0) *** |
| BMI§ <18.5 or >=25 (%) | 0 | 21.2 | 40.9 *** | 40.9 *** | 88.9 *** | 66.6 *** |
| Vigorous Exercise min/week (SD) | 189 (187) | 236 (329) | 79 (138)*** | 185 (290) ** | 4 (26)*** | 116 (232) *** |
| Exercise Minutes=0 (%) | 0 | 25.6 | 54.7 *** | 38.7 *** | 96.5 *** | 55.6 *** |
| HAQ-DI* (range 0–3.0) (SD) | 0.04 (0.11) | 0.38 (0.59) | 0.07 (0.19)*** | 0.50 (0.67)*** | 0.11 (0.22)*** | 0.55 (0.69)*** |
| HAQ-DI* =0 (%) | 80.7 | 48.3 | 75 ** | 40.4 ** | 66.7 *** | 36.7 *** |
| Walk pace (SD) | 2.6 (0.9) | 2.1 (0.9) | 2.2 (0.9) *** | 1.8(0.9)*** | 1.8(1.0)*** | 1.5 (0.9) *** |
| Number of Cormorbid conditions (SD) | 1.0 (1.0) | 1.5 (1.3) | 1.2 (1.1) * | 1.5(1.4) | 1.4(1.1) *** | 1.6(1.4) |
| At Last Observation | ||||||
| Years observed (1986–2005) (SD) | 16.4(4.3) | 15.7(4.8) ** | 14.8(5.2) *** | |||
| Lost to follow-up (%) | 20.2 | 17.9 | 16.0 | |||
| Died by 2005 (%) | 40.5 | 46.8* | 56.9*** | |||
| Age at Death (years) (SD) | 81.5 (5.7) | 81.2 (6.1) | 80.3 (6.2)* | |||
| Mortality Rate (Per 10,000 Person-years,95% CI) (range) # | 248 (219–281) | 298 (273 326) * | 384 (347–425) *** | |||
| Mortality Rate, Men (Per 10,000 Person-years, 95% CI) (Range) | 275 (240–316) | 319 (290–352) | 392 (350–440) *** | |||
| Mortality Rate, Women (Per 10,000 Person-years, 95% CI) (Range) | 165 (122–224) | 233 (191–285) | 354 (282–444) *** | |||
P-values compared to Low Risk:
<0.05,
<0.01,
<0.001
BMI=body mass index (kg/m2)
HAQ-DI = Health Assessment Questionnaire Disability Index
The incidence rates are compared using Fisher's exact test
By definition, low-risk participants met healthy BMI, smoking, and physical activity criteria at baseline. Medium-risk participants had a very low smoking rate (<5%); 41% had an abnormal BMI; and 55% did not exercise routinely. In contrast, 22% of high-risk subjects smoked, 89% had abnormal BMI, and only 3.5% exercised routinely. Walking pace was slower in the medium and high-risk groups when compared to the low-risk group. Baseline rates of hypertension, pulmonary disease, gastrointestinal disorders, arthritis and diabetes were higher in the high-risk compared to low-risk group. Prevalence of comorbidities was similar between groups.
Baseline HAQ-DI scores were low for all groups, although medium- and high-risk groups had higher scores than the low-risk group. The majority (75%) of participants had no disability. By the last observation, risk factor differences between groups had attenuated; although all comparisons remained significantly different between risk groups. Walking pace decreased and cumulative prevalence of comorbidies increased for all groups. With the exception of higher rates of hypertension and diabetes among high-risk participants, the cumulative prevalence of comorbidies did not differ significantly between risk groups.
Participants were observed for an average of 15.6 years. Age of survivors in 2005 was similar for all groups (85 years). Last observed HAQ-DI scores were significantly lower for the low-risk group compared to medium- and high-risk groups. Forty-eight percent of all study participants had died by 2005. Although age at death was similar, mortality rates were nearly 50% higher for high- compared to low-risk participants (384 vs. 248 per 10,000 person-years, p<0.001). Approximately 1% of participants, excluding decedents, were lost to follow-up each year. Those participants were 6 months younger with similar lower baseline HAQ-DI Scores.
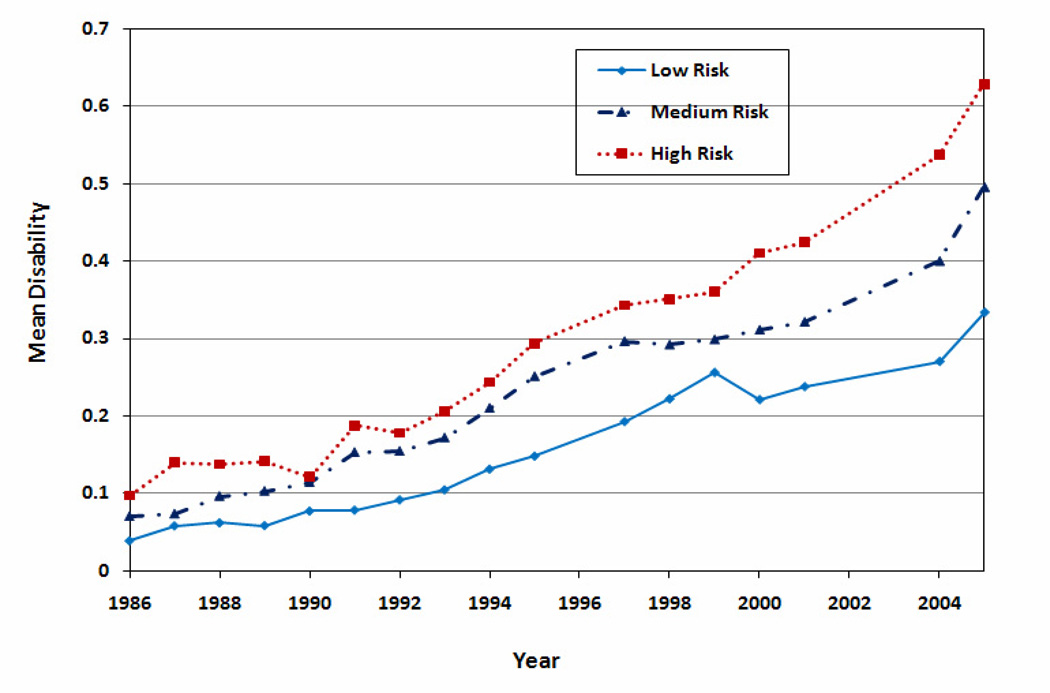
Figure 1 displays yearly HAQ-DI scores by risk group. Disability increased each year in all groups. Participants without risk factors had the lowest HAQ-DI at each time point, followed by those with one risk factor. Differences were most pronounced at the later time points.
Figure 1.
Unadjusted mean annual HAQ-DI disability scores by group. Diamond shape represents the low risk group (zero risk factors), triangle for medium risk group (one risk factor), and square for high risk group (two or three risk factors).
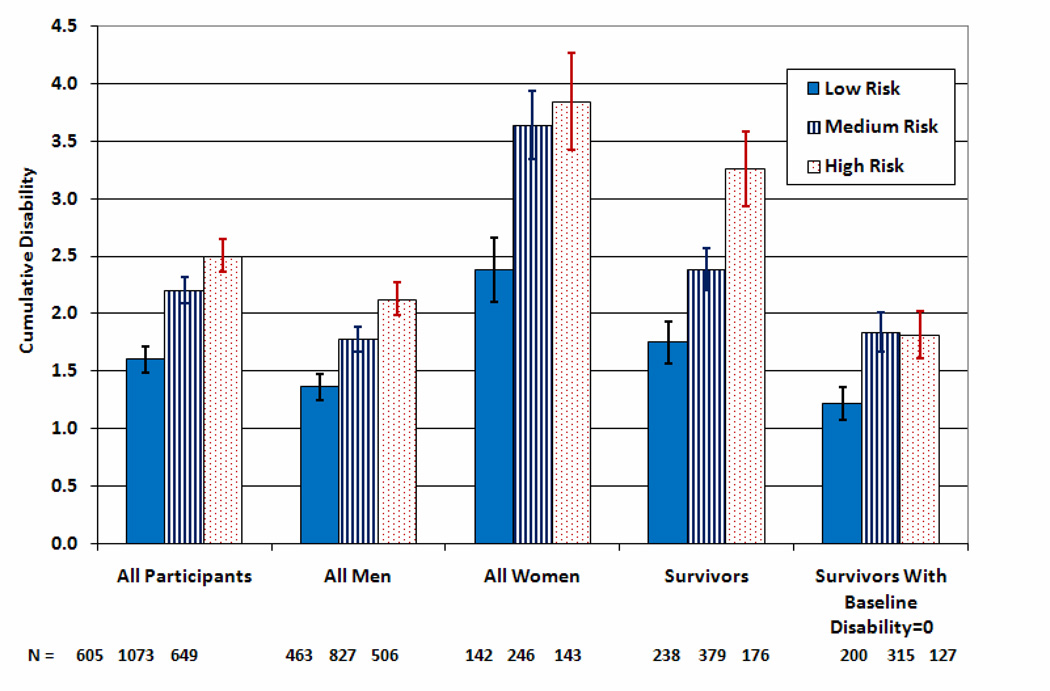
Figure 2 shows the dose-response relationship among groups in cumulative disability when comparing all participants, survivors, survivors without baseline disability, and by gender. Differences are most pronounced when comparing high- to low-risk participants. Cumulative disability, a surrogate for total lifetime disability, contains a bias in favor of the high risk group because of the shorter period during which disability accumulates. Similar results were seen when average disability was compared. Decedents had the highest average disability scores at all time points.
Figure 2.
Cumulative disability (sum of annual HAQ-DI disability scores by risk group).
We compared Kaplan-Meier curves for the time for each group to attain a HAQ-DI of 1.0 (moderate disability) and death. The median time to develop moderate disability was approximately 8.0 years longer in the low-risk than the high-risk group (log-rank test p<0.0001).
Cox proportional hazard models adjusted for age, sex, and baseline disability yielded nearly identical findings. Compared to low-risk, the high-risk group had nearly a two-fold increased risk for the development of moderate disability (HAQ-DI=1) (HR 1.91, 95%CI 1.50–2.42), while medium risk participants had a 60% increased risk (HR 1.61, 95%CI 1.29–2.01). Age (HR 1.11, 95%CI 1.08–1.13) and higher baseline disability (HR 49.5, 95%CI 37–66) were also associated with disability.
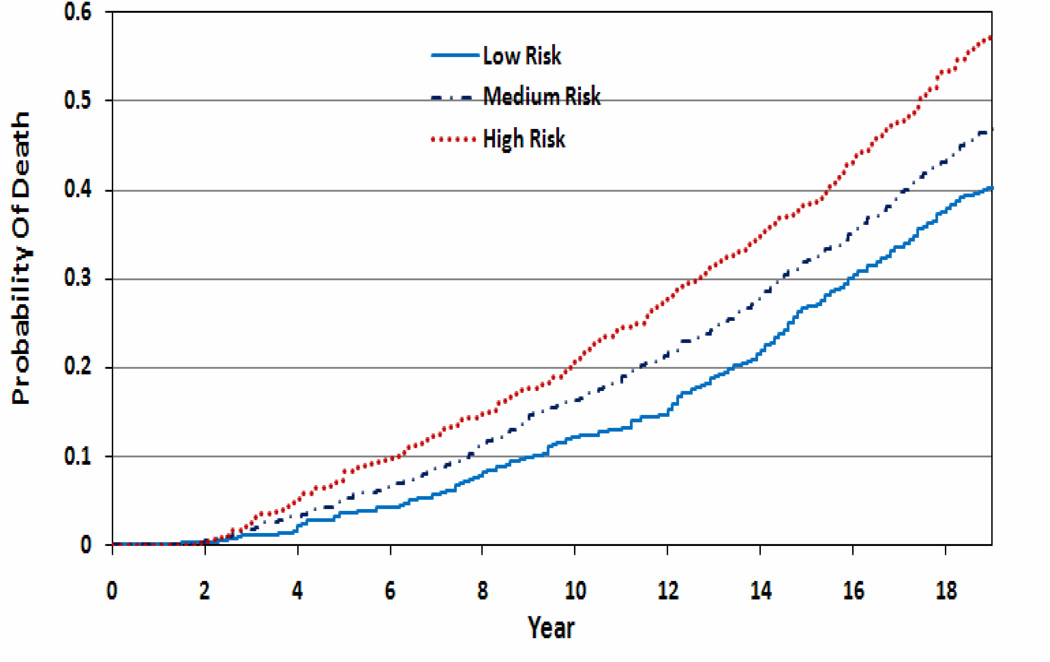
The unadjusted probability of survival was significantly higher for low- compared to medium-and high-risk groups (Figure 3). Curves separated early in the period of observation and continued to diverge over time. Sixty percent of the low-risk group was alive at 19 years compared to 53% and 43% in medium- and high-risk groups. The time to 20% mortality in each group was postponed by 3.6 years in low- versus high-risk participants; the postponement was 3.9 years to 40% mortality. Similar results were found when analyses were restricted to participants without baseline disability. Using survival analysis, medium- and high- risk participants had increased adjusted risks of mortality compared to low-risk (HR 1.18, 95%CI 1.01–1.37 and HR 1.47, 95%CI 1.25–1.73) although the differences were less marked compared with disability differences.
Figure 3.
Kaplan-meier curve of probability of death by risk group
Multivariable Cox proportional hazards models were used to examine the relative role of each individual risk factor (abnormal BMI, smoking, and inactivity) as well as baseline walking pace and individual comorbidities upon moderate disability and mortality. Because the baseline HAQ-DI is among the strongest predictors of future disability and mortality, these analyses were restricted to the subset of participants (n=1,736) with baseline HAQ-DI=0 (Table 3). Males had an increased hazard of death (HR 1.47, 95%CI 1.18–1.81) but a reduced risk of disability (HR 0.52,95%CI 0.40–0.68). Among the three risk factors, smoking was associated with a two-fold increased risk of moderate disability (HR 2.02, 95%CI 1.32–3.08) and an even higher risk of death (HR 2.32, 95%CI 1.83–2.94). Faster walking pace was associated with a decrease in both morbidity and mortality. The presence of hypertension, diabetes, cardiovascular, pulmonary disease, stroke, or cancer at the baseline was associated with higher mortality; whereas only arthritis and stroke were associated with disability.
Table 3.
Association of Individual Risk Factors with Disability and Mortality (Participation with Zero Baseline Disability)
| Moderate Disability (HAQ-DI=1) (all subjects n=1726) |
Moderate Disability (HAQ-DI=1) non- smokers (n=1595) |
|||
|---|---|---|---|---|
| Variable | HR | 95% CI | HR | 95% CI |
| Age (year) | 1.11 | 1.07 – 1.16 | 1.12 | 1.08 – 1.17 |
| Male | 0.52 | 0.40 – 0.68 | 0.52 | 0.39 – 0.70 |
| No Exercise | 1.14 | 0.88 – 1.47 | 1.13 | 0.86 – 1.48 |
| Abnormal BMI* | 1.26 | 0.98 – 1.61 | 1.23 | 0.95 – 1.59 |
| Smoking | 2.02 | 1.32 – 3.08 | ||
| Walking pace | 0.84 | 0.74 – 0.96 | 0.85 | 0.73 – 0.97 |
| Diabetes | 3.26 | 2.06 – 5.17 | 3.45 | 2.17 – 5.49 |
| Arthritis | 1.66 | 1.27 – 2.16 | 1.64 | 1.25 – 2.17 |
| Cardiac Disease | 1.44 | 0.99 – 2.07 | 1.48 | 1.02 – 2.16 |
| stroke | 2.95 | 1.49 – 5.83 | 2.86 | 1.32 – 6.20 |
| Cancer | 1.84 | 0.97 – 3.50 | 1.9 | 1.00 – 3.63 |
| Depression | 1.36 | 0.80 – 2.30 | 1.37 | 0.79 – 2.37 |
|
Mortality (all subjects n=1726) |
Mortality non-smokers (n=1595) |
|||
| Variable | HR | 95% CI | HR | 95% CI |
| Age (year) | 1.12 | 1.1 – 1.14 | 1.13 | 1.1 – 1.15 |
| Male | 1.47 | 1.19 – 1.81 | 1.55 | 1.23 – 1.95 |
| No Exercise | 1.08 | 0.92 – 1.27 | 1.06 | 0.89 – 1.25 |
| Abnormal BMI | 1.08 | 0.93 – 1.26 | 1.08 | 0.92 – 1.27 |
| Smoking | 2.32 | 1.83 – 2.94 | ||
| Walking pace | 0.90 | 0.83 – 0.98 | 0.9 | 0.82 – 0.98 |
| Hypertension | 1.20 | 1.03 – 1.41 | 1.25 | 1.05 – 1.48 |
| Diabetes | 1.95 | 1.44 – 2.62 | 1.87 | 1.37 – 2.55 |
| Cardiac Disease | 1.57 | 1.27 – 1.93 | 1.6 | 1.29 – 1.99 |
| Stroke | 1.75 | 1.07 – 2.87 | 2.11 | 1.24 – 3.57 |
| Cancer | 1.65 | 1.11 – 2.44 | 1.51 | 1 – 2.28 |
| Pulmonary Disease | 1.61 | 1.15 – 2.26 | 1.51 | 1.03 – 2.21 |
| Depression | 1.06 | 0.74 – 1.53 | 0.96 | 0.63 – 1.46 |
BMI= body mass index (kg/m2)
Since smoking as associated with the greatest risk for disability and mortality, we repeated the analysis on non-smokers (n=1,595). Neither having an abnormal BMI nor inactivity was significantly associated with disability or mortality in this smaller subset. Comorbid conditions and walking pace had similar effects upon disability and mortality in non-smokers.
Because of the possibility that death may be related to disability, and as such could present informational censoring over time26, we repeated multi-variable proportional hazards modeling for disability among the 960 survivors. The magnitude of hazard ratios for covariates including individual risk factors, walking pace, and comorbidities was not substantially different than when decedents were include in the analysis (data not shown).
Population attributable risk for mortality and for moderate disability (HAQ-DI=1) were calculated for each risk factor and for individuals with ≥ 1 lifestyle risk factor (Table 4). Excess risk was seen for all risk groups for both mortality and moderate disability. Similar to the survival analysis, the highest attributable risk was seen with smoking.
Table 4.
Measures of Attributable Risk in the Population
| Mortality all subjects (N=2327) | |||||
|---|---|---|---|---|---|
| n | Deaths | Population Incidence Rate per 100 |
Exposed | PAR § | |
| Population | 2327 | 1116 | 47.96 | ||
| Smokers | 190 | 130 | 68.42 | 20.46 | |
| BMI risk | 1016 | 521 | 51.28 | 3.32 | |
| Inactive | 1213 | 624 | 51.44 | 3.48 | |
| ≥ 1 risk factor | 1722 | 871 | 50.58 | 2.62 | |
|
Mortality With Zero Disability (HAQ-DI=0#) at baseline (n=1726) | |||||
| n | Deaths |
Population Incidence Rate per 100 |
Exposed | PAR | |
| Population | 1726 | 766 | 44.38 | ||
| Smokers | 131 | 87 | 66.41 | 22.03 | |
| Abnormal BMI* | 715 | 337 | 47.13 | 2.75 | |
| Inactive | 861 | 412 | 47.85 | 3.47 | |
| ≥ 1 risk factor | 1238 | 577 | 46.61 | 2.23 | |
| Moderate Disability: HAQ-DI=1. Subjects with baseline HAQ-DI=0 (n=1726) | |||||
| n | HAQ-DI=1 |
Population Incidence Rate per 100 |
Exposed | PAR | |
| Population | 1726 | 290 | 16.80 | ||
| Smokers | 131 | 28 | 21.37 | 4.57 | |
| Abnormal BMI | 715 | 137 | 19.16 | 2.36 | |
| Inactive | 861 | 156 | 18.12 | 1.32 | |
| ≥ 1 risk factor | 1238 | 229 | 18.50 | 1.70 | |
| Moderate Disability: HAQ-DI=1. Surviving subjects with baseline HAQ-DI=0, (n=960) | |||||
| n | HAQ-DI=1 |
Population Incidence Rate per 100 |
Exposed | PAR | |
| Population | 960 | 151 | 15.73 | ||
| Smokers | 44 | 11 | 25.00 | 9.27 | |
| Abnormal BMI | 378 | 74 | 19.58 | 3.85 | |
| Inactive | 449 | 76 | 16.93 | 1.20 | |
| ≥ 1 risk factor | 661 | 117 | 17.70 | 1.97 | |
PAR=Population Attributable Risk
BMI= body mass index (kg/m2)
HAQ-DI=health assessment questionnaire disability index
Discussion
This longitudinal study of 2,327 college-educated older adults shows that maintaining normal weight, not smoking, and regular physical activity are persistently associated with slower development of disability and reduction in mortality. Results are consistent across different subgroups of the cohort: men, women, those with and without initial disability, decedents, and survivors; and across analytic methods. The differences among subjects with zero, one, and ≥ two risk factors appeared early and were constant or diverged further as participants approached an average age of 85. Results did not differ substantially with subgroup analyses. As individual behavioral risk factors, only smoking appeared to have a statistically significant association with both disability and mortality after controlling for the prevalence of comorbid conditions at enrollment. The postponement of mortality was 3.6 to 3.9 years, similar to the roughly four years expected from the Gompertz function for an increase of 50% in mortality rates27.
Our findings support previous studies of aging in older adults and provide a longitudinal context, a longer period of observation with extension into the ninth decade, essential for estimation of cumulative lifetime morbidity. Several studies have documented independent effects of lack of physical activity and weight above the normal range as risk factors for increased disability and mortality in older adults28–31. Although the role of cigarette smoking on increased mortality is well established, there are fewer data regarding cigarette smoking and physical disability7,32. A systematic review of behavioral determinants of healthy aging identified not-smoking, ongoing physical activity, and maintaining normal weight as key elements leading to improved outcomes in aging individuals33. Indeed, population-based studies of the United Kingdom found that smoking was directly attributable to 19% of all deaths and 12% of disability adjusted life years (DALY) lost34. Similarly, physical inactivity was found to be responsible for 3.1%35 and overweight contributed to 7.3%36 of morbidity and mortality in the UK. Because of differences in populations between studies, direct comparisons to results seen in this cohort (college-educated older adults) to the UK population is difficult, although results are similar with respect to smoking contributing to the highest risk for both death and disability.
Our study was not designed to address the mechanisms underlying associations between behavioral risk factors and disability and mortality. We can speculate that such mechanisms include accrual of comorbid conditions such as cardio-pulmonary disease and diabetes as described in other studies of similar populations34–36. Although our study did not find striking differences in the cumulative prevalence of comorbid conditions between risk groups as subjects entered advance old age, it is possible that the severity of these conditions, earlier age of onset, as well as differences in cardio-respiratory reserve explain our findings.
The strengths of this study include the large cohort followed annually for nearly two decades into their mid 80s. This cohort had little to no baseline disability in their seventh decade of life, allowing cumulative disability to be estimated.
Several limitations need to be considered. With the exception of death, data were acquired from self-report. However, we have documented in similar populations a strong correlation between HAQ-DI scores and observed performance37.
Loss to follow-up is to be expected in studies of long duration, but has the potential to introduce bias if living participants who are lost-to-follow up are substantially different from completers. We had a low rate of loss (<1% per year), but with slightly higher rates of drop-out among low-risk participants. Completers were similar, if not slightly older, than survivor lost-to-follow-up. Mortality data were ascertained irrespective of completer status.
We approached the issue of informational censoring of death in this study by several means. First, we analyzed determinants of death and disability separately among all participants. When analyzing disability outcomes, for which death may be associated with disability, cumulative disability among all participants and compared that to the subset of surviving participants. Similar approaches were employed when analyzing risk factors for the development of disability.
This study was initiated as a test of the Compression of Morbidity hypothesis3, where fewer health risks would postpone both morbidity and death, but morbidity more so than mortality. Data presented here are consistent with that hypothesis, with mortality postponed nearly four years and disability to the 0.3 level (the highest with complete data) postponed by 8.2 years. There are, however, several challenges in making direct comparisons of morbidity and mortality. Disability is a subset of morbidity and the degree to which it is a valid surrogate for morbidity might be challenged. Second, these data, even after two decades, only contain the first one-half of deaths and much of the morbidity will come after age 85. It may be speculated that differences between risk groups will narrow in the future, though at this point differences continue to diverge. Direct comparisons, therefore, should be made with caution.
Study of disability trajectories in the last months of life suggests little relation between specific disease diagnostic categories or counts of co-morbid diseases and disability levels, implying that population movement toward trajectories with later onset of disability, irrespective of diagnoses, could improve senior health38. Our findings that health risk factors in the seventh decade of life continue to predict disability and mortality in the eighth and ninth decades suggest that maintenance of healthy lifestyle behaviors may help compress morbidity far into the lifespan. This study provides support for health policy approaches that postpone morbidity through lifestyle risk reduction.
Table 2.
Prevalence of Comorbid Conditions by Risk Group
| Condition | Low Risk | Medium Risk | High Risk | |||
|---|---|---|---|---|---|---|
| Baseline | Cumulative | Baseline | Cumulative | Baseline | Cumulative | |
| Hypertension | 164 (27.1) | 281 (46.4) | 335 (31.2) | 550 (51.3) | 246 (37.9) *** | 349 (53.8) * |
| Diabetes | 20 (3.3) | 49 (8.1) | 48 (4.5) | 119 (11.1) | 50 (7.7) *** | 112 (17.3) *** |
| Arthritis | 161 (26.6) | 395 (65.3) | 315 (29.4) | 684 (63.7) | 219 (33.7)* | 406 (62.6) |
| Cardiovascular disease | 71 (11.7) | 262 (43.3) | 151 (14.1) | 497 (46.3) | 81 (12.5) | 274 (42.2) |
| Stroke | 8 (1.3) | 71 (11.7) | 33 (3.1)* | 128 (11.9) | 16 (2.5) | 71 (11.1) |
| Cancer | 16 (2.6) | 211 (34.9) | 27 (2.5) | 369 (34.4) | 16 (2.5) | 218 (33.6) |
| Pulmonary | 19 (3.1) | 109 (18.0) | 60 (5.6) * | 207 (19.3) | 47 (7.2)* | 137 (21.1) |
| Neurologic | 32 (5.3) | 182 (30.1) | 52 (4.8) | 289 (26.9) | 42 (6.5) | 173 (26.7) |
| Depression | 30 (5.0) | 75 (12.4) | 48 (4.5) | 123 (11.5) | 35 (5.4) | 74 (11.4) |
| Gastrointestinal disorders | 127 (21) | 252 (41.7) | 231 (21.5) | 458 (42.7) | 171 (26.3)* | 307 (47.3) |
P-values compared to Low Risk:
<0.05,
<0.01,
<0.001
Acknowledgments
Funding Source: This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (AR43584)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
All authors had full access to the data, and each contributed substantially to writing and revising the manuscript
References
- 1.Olshansky SJ, Goldman DP, Zheng Y, Rowe JW. Aging in America in the twenty-first century: demographic forecasts from the MacArthur Foundation Research Network on an aging society. Milbank Q. 2009;87:842–862. doi: 10.1111/j.1468-0009.2009.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374(9696):1196–1208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 4.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168:1638–1646. doi: 10.1001/archinte.168.15.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its condequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 7.Reuser M, Bonneux LG, Willekens FJ. Smoking kills, obesity disables: a multistate approach of the US Health and Retirement Survey. Obesity. 2009;17:783–789. doi: 10.1038/oby.2008.640. [DOI] [PubMed] [Google Scholar]
- 8.Kuller LH, Ockene JK, Meilahn E, et al. Cigarette smoking and mortality. MRFIT Research Group. Prev Med. 1991;20:638–654. doi: 10.1016/0091-7435(91)90060-h. [DOI] [PubMed] [Google Scholar]
- 9.Leon AS, Connett J. Physical activity and 10.5 year mortality in the Multiple Risk Factor Intervention Trial (MRFIT) Int J Epidemiol. 1991;20:690–697. doi: 10.1093/ije/20.3.690. [DOI] [PubMed] [Google Scholar]
- 10.Gazino JM. Fifth phase of the epidemiologic transition: the age of obesity and inactivity. JAMA. 2010;303:275–276. doi: 10.1001/jama.2009.2025. [DOI] [PubMed] [Google Scholar]
- 11.Vita AJ, Terry RB, Hubert HB, Fries JF. Aging, health risks, and cumulative disability. New Engl J Med. 1998;338:1035–1041. doi: 10.1056/NEJM199804093381506. [DOI] [PubMed] [Google Scholar]
- 12.Paffenbarger Rs, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J. Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 13.Kannel WB, Belanger A, D'Agostino R, Israel I. Physical activity and physical demand on the job and risk of cardiovascular disease and death: the Framingham Study. Am Heart J. 1986 Oct;112(4):820–825. doi: 10.1016/0002-8703(86)90480-1. [DOI] [PubMed] [Google Scholar]
- 14.Harris T, Cook EF, Garrison R, et al. Body mass index and mortality among nonsmoking older persons. The Framingham Heart Study. JAMA. 1988 Mar 11;259(10):1520–1524. [PubMed] [Google Scholar]
- 15.Relationship between baseline risk factors and coronary heart disease and total mortality in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Prev Med. 1986;15:254–273. doi: 10.1016/0091-7435(86)90045-9. [DOI] [PubMed] [Google Scholar]
- 16.National Institutes of Health, Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Obes Res. 1998;6 Suppl 2:51S–209S. [PubMed] [Google Scholar]
- 17.Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol. 1982;9:789–793. [PubMed] [Google Scholar]
- 18.Bruce B, Fries JF. The Health Assessment Questionairre (HAQ) Clin Exp Rheumatol. 2005;23 Suppl 39:S14–S16. [PubMed] [Google Scholar]
- 19.Krishnan E, Tugwell P, Fries JF. Percentile benchmarks in patients with rheumatoid arthritis: Health Assessment Questionnaire as a quality indicator (QI) Arthritis Res Ther. 2004;6:R505–R513. doi: 10.1186/ar1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sokka T, Kautiainen H, Hannonen P, Pincus T. Changes in Health Assessment Questionnaire disability scores over five years in patients with rheumatoid arthritis compared with the general population. Arthritis Rheum. 2006;54:3113–3118. doi: 10.1002/art.22130. [DOI] [PubMed] [Google Scholar]
- 21.Bruce B, Fries J. Longitudinal comparison of the Health Assessment Questionnaire (HAQ) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Arthritis Rheum. 2004;51:730–737. doi: 10.1002/art.20695. [DOI] [PubMed] [Google Scholar]
- 22.Doody MM, Hayes HM, Bilgrad R. Comparability of National Death Index Plus and standard procedures for determining causes of death in epidemiologic studies. Ann Epidemiol. 2001;11(1):46–50. doi: 10.1016/s1047-2797(00)00177-0. [DOI] [PubMed] [Google Scholar]
- 23.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bijnen FC, Feskens EJ, Caspersen CJ, et al. Baseline and previous physical activity in relation to mortality in elderly men: the Zutphen Elderly Study. Am J Epidemiol. 1999;150:1289–1296. doi: 10.1093/oxfordjournals.aje.a009960. [DOI] [PubMed] [Google Scholar]
- 25.Hubert HB, Fries JF. Predictors of physical disability after age 50: six year longitudinal study in a runners club and university population. Ann Epidemiol. 1994;4:285–294. doi: 10.1016/1047-2797(94)90084-1. [DOI] [PubMed] [Google Scholar]
- 26.Murphy TE, Han L, Allore HG, et al. Treatment of death in the analysis of longitudinal studies of gerontological outcomes. J Gerontol A Biol Sci Med Sci. 2011;66:109–114. doi: 10.1093/gerona/glq188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fries JF, Crapo LM. Vitality and Aging. San Francisco, California: W.H. Freeman Company; 1981. [Google Scholar]
- 28.Lang IA, Guralnik JM, Melzer D. Physical activity in middle-aged adults reduces risk of functional impairment independent of its effect on weight. J Am Geriatr Soc. 2007;55:1841–1841. doi: 10.1111/j.1532-5415.2007.01426.x. [DOI] [PubMed] [Google Scholar]
- 29.Riebe D, Blissmer Bj, Greaney ML, et al. The relationship between obesity, physical activity, and physical function in older adults. J Aging Health. 2009;21:1159–1178. doi: 10.1177/0898264309350076. [DOI] [PubMed] [Google Scholar]
- 30.Taylor DH, Ostbye T. The Effect of middle- and old- age body mass index on short-term mortality in older people. J Am Geriatr Soc. 2001;49:1319–1326. doi: 10.1046/j.1532-5415.2001.49259.x. [DOI] [PubMed] [Google Scholar]
- 31.Ford ES, Bergmann MM, Kroger J, et al. Healthy living is the best revenge: findings from the European Prospective Investigation into Cancer and Nutrition-Potsdam Study. Arch Int Med. 2009;169:1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 32.Strandbert AY, Strandbert TE, Pitkala K, et al. The effect of smoking in midlife on health-related quality of life in old age. Arch Int Med. 2008;168:1968–1974. doi: 10.1001/archinte.168.18.1968. [DOI] [PubMed] [Google Scholar]
- 33.Peel NM, McClure RJ, Bartlett HP. Behavorial determinants of healthy aging. Am J Prev Med. 2005;28:298–304. doi: 10.1016/j.amepre.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Allender S, Balakrishnan R, Scarborough P, Webster P, Rayner M. The burden of smoking-related ill health in the UK. Tobacco Control. 2009;18:262–267. doi: 10.1136/tc.2008.026294. [DOI] [PubMed] [Google Scholar]
- 35.Allender S, Foster C, Scarborough P, Rayner M. The burden of physical activity-related ill health in the UK. J Epidemiol Community Health. 2007;61:344–348. doi: 10.1136/jech.2006.050807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Allender S, Rayner M. The burden of overweight and obesity-related ill health in the UK. Obesity reviews. 2007;8:467–473. doi: 10.1111/j.1467-789X.2007.00394.x. [DOI] [PubMed] [Google Scholar]
- 37.Lane NE, Bloch DA, Wood PD, Fries JF. Aging, long-distance running, and the development of musculoskeletal disability. Am J Med. 1987;82:772–780. doi: 10.1016/0002-9343(87)90014-3. [DOI] [PubMed] [Google Scholar]
- 38.Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010;362:1173–1180. doi: 10.1056/NEJMoa0909087. [DOI] [PMC free article] [PubMed] [Google Scholar]