Abstract
In patients presenting with a neck adenopathy from a clinically unknown primary, efforts should be made to localize the primary tumour, as this allows a more focused therapy. Imaging is helpful in identifying suspicious mucosal sites that should be further investigated endoscopically, including biopsy. In case no primary tumour is detected in the head and neck, a positron emission tomography (PET) study can be considered to search for an infraclavicular primary tumour. This article reviews the diagnostic value of computed tomography (CT), magnetic resonance imaging, PET and PET/CT in this clinical context.
Keywords: Clinically unknown primary, head and neck cancer, computed tomography, magnetic resonance imaging, positron emission tomography
Introduction
The condition of an unknown primary in the neck can be defined as a patient presenting with metastasis of a carcinoma in the neck lymph nodes, without prior history of malignancy, and without the primary tumour being found. The term clinically unknown primary (CUP) is most often used in the context of squamous cell cancer.
The treatment of such a patient is (chemo)radiotherapy with or without neck dissection, including irradiation of all potential mucosal disease sites, causing substantial morbidity. Although this treatment has been effective, significant side effects occur, such as xerostomia and dysphagia[1]. In such a situation, efforts should be made to find the primary tumour, as this allows a more focused therapy, with less morbidity and possibly a better outcome.
In most cases, the CUP is a subtle tumour, situated in the palatine tonsil, tongue base or pyriform sinus; the nasopharynx should also be scrutinized, especially in regions where nasopharyngeal cancer is endemic.
Imaging is rarely firmly diagnostic for a purely mucosal primary cancer. In most cases, the contribution of imaging is to identify one or more suspicious sites that should be further investigated during endoscopic examination; in addition, imaging provides important information about the metastatic neck mass.
Invasive diagnostic procedures are best performed after imaging, as biopsy and tonsillectomy cause tissue changes that may be misinterpreted as evidence of tumour on imaging studies. On the other hand, if such procedures are performed first, the primary may be detected, and hence the lesion is no longer an unknown tumour.
It is noteworthy that the reported incidence of CUP is very divergent. In two recent publications, both on the impact of positron emission tomography (PET) imaging on the management of head and neck cancer, the incidence varied from 0.8% to 21%[2,3]. This variability may be related to differences in patient population, but also to a different definition of a CUP. Often, it is not clear whether the primary tumour was called unknown after a routine head and neck physical examination, or after invasive diagnostic screening. Such differences in definition clearly influence the potential impact of imaging studies on identifying a CUP. In this regard, it is not surprising that in the study with the higher incidence[3], the impact of PET in finding the CUP was far greater than in the study with the lower incidence[2].
Several imaging techniques are available to search for a CUP tumour, including ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI) and metabolic imaging. Ultrasonography is mainly of use when the primary tumour is suspected to be of thyroid gland origin.
A basic requisite for the detection of a subtle lesion is an adequate technical execution of the imaging technique applied[1].
Computed tomography
CT may point the clinician to a suspicious region, possibly corresponding to the primary tumour, by showing areas of subtle soft tissue thickening or a subtle asymmetric appearance of the pharyngeal or laryngeal structures (Fig. 1). Also the appearance of the nodal disease carries important information. The anatomical localization of the adenopathies gives an indication where the primary tumour may be situated. The nodal architecture may suggest the localization of the primary, as may be the case in thyroid cancer (Fig. 2). Imaging is also important in determining the presence and extent of extracapsular tumour spread, as involvement of critical structures, such as the carotid artery, influences the decision to perform a neck dissection or not. The presence of extracapsular spread on imaging also indicates a higher chance of metastatic spread, and screening for distant disease should then be intensified, including chest CT or whole body PET imaging.
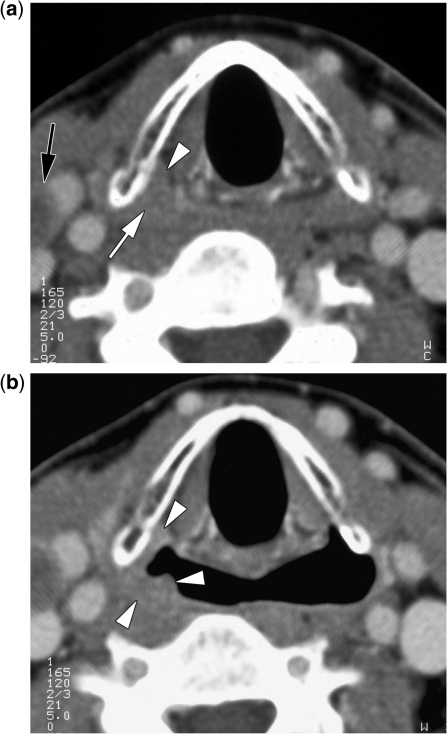
Figure 1.
Contrast-enhanced CT images in a patient presenting with a right-sided level III adenopathy (partially visible in (a), black arrow); fine-needle aspiration cytology showed squamous cell cancer; clinically no primary tumour could be identified. The axial image during quiet breathing (a) shows subtle soft tissue thickening in the apex of the right pyriform sinus (white arrow; compare with opposite side). There is subtle infiltration or displacement of the paraglottic space fat (arrowhead). Axial image obtained during modified Valsalva manoeuvre (b) shows somewhat less expansion of the right pyriform sinus compared with the opposite side; the soft tissue irregularity is now more visible (arrowheads). These findings are highly suspect for being the primary tumor, which was confirmed by biopsy.
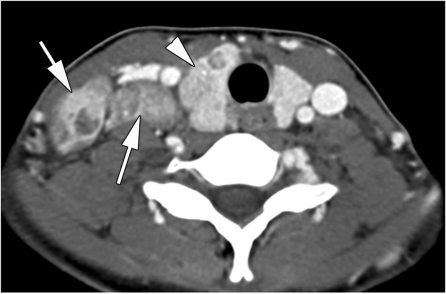
Figure 2.
Contrast-enhanced CT image in a 20-year-old female patient presenting with a right lower neck swelling. Several adenopathies, appearing partially cystic, are seen in the base of the neck (arrows). The location and appearance of these adenopathies are suggestive for papillary thyroid cancer. The right thyroid lobe is slightly enlarged and appears heterogeneous (arrowhead), an aspecific finding in itself, but in this context suspicious for cancer. After resection, the entire gland turned out to be diffusely involved by tumour.
CT was reported to be able to detect the primary site in 30% of patients presenting with neck nodal metastasis of squamous cell cancer [5]. However, although CT has been widely used in this situation, few scientific studies have been published on its actual value in this particular clinical situation.
Recently, in a large retrospective study[6] the role of imaging in the detection of CUP was thoroughly examined. In this study, all patients (n = 236) presented with nodal metastases from a cancer that was not obvious at conventional work-up, including a head and neck examination by multiple examiners. Eventually, the primary tumour was detected in 53% of patients. The chance of detecting the primary tumour was significantly higher in those patients in whom the physical and radiologic investigation did show a suspicious finding. Suspicious findings during the physical examination and on the CT study were the only variables independently correlated with the discovery of the primary tumour. Among other variables, positive findings on nuclear imaging studies were not independently correlated with the discovery of the primary in this study.
Magnetic resonance imaging
The search for the primary tumour can also been done using MRI. Conventional spin echo sequences show anatomical disturbances, similar to CT. The advantage of MRI is its higher contrast resolution, but the technique also has several disadvantages, such as a higher risk of motion-induced artefacts, technical difficulties in covering the entire head and neck region, a long examination time and higher costs compared with CT. A difference in diagnostic accuracy in detecting clinically occult tumours in the head and neck, compared with CT, has not yet been proven scientifically.
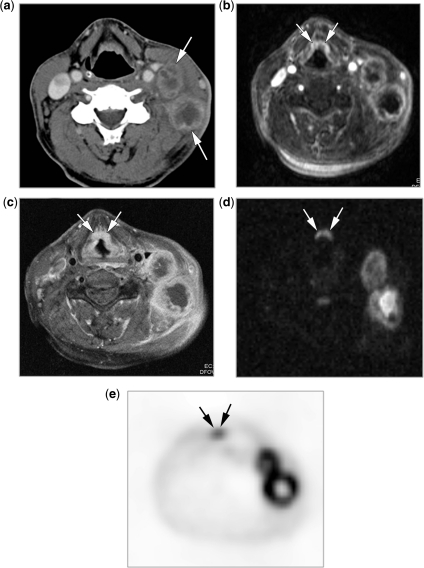
Newer functional MR-techniques may be helpful in finding the clinically occult lesion, for example by showing small mucosal foci of increased perfusion or restricted diffusion (Fig. 3). Further study is still required to determine the complementary value of these sequences in this context.
Figure 3.
Patient presenting with left-sided neck adenopathies, without clinically apparent primary tumour. (a) Contrast-enhanced CT image shows large, centrally necrotic adenopathies at level III on the left side (arrows). No primary tumour was detected in this study. (b) Frame of a dynamic T1-weighted MR sequence, acquired during and immediately after bolus injection of gadolinium. Apart from the viable border of the adenopathies, the epiglottis (arrows) also shows somewhat increased and heterogeneous uptake of contrast agent. (c) Contrast-enhanced T1-weighted spin echo image (obtained after (b)) shows a slightly thickened epiglottis (arrows). (d) B1000 diffusion-weighted image. Apart from the adenopathies, also diffusion restriction is seen at the epiglottic level (arrows). (e) A PET scan was also obtained in this patient, and this also confirms, apart from the adenopathies, that an epiglottic lesion is present (arrows). Retrospectively, the epiglottis also looks a bit thicker than normal on the initial CT study. Histology revealed epiglottic squamous cell cancer.
Metabolic imaging
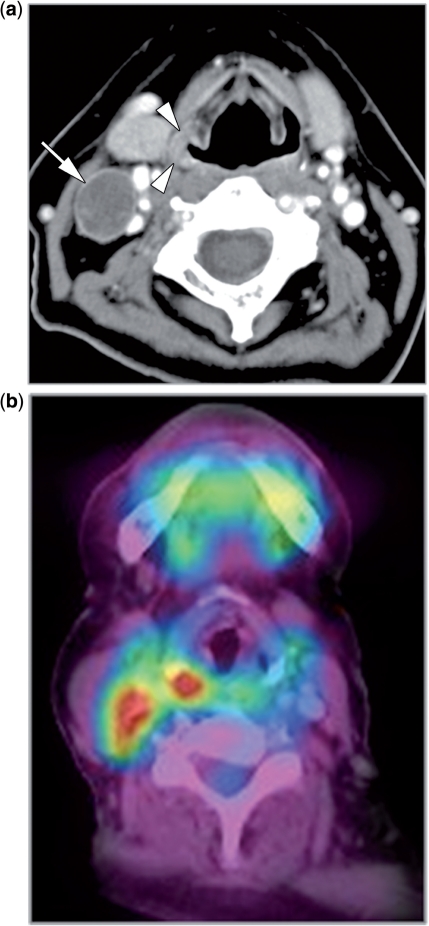
As in disease processes metabolic changes occur before anatomical disturbances become visible, PET may become positive before anatomical imaging, and thus be able to spot a CUP more readily than CT or MRI. Also, PET is characterized by a high lesion-to-background contrast, making subtle abnormalities more easy to spot than on a CT or MR study (Fig. 4).
Figure 4.
Patient presenting with an adenopathy in the right neck; fine-needle aspiration cytology showed SCC. No primary tumour could be found clinically. (a) Contrast-enhanced CT image confirms the presence of a necrotic adenopathy (arrow). The right pyriform sinus shows focally a slightly thickened wall (arrowheads). (b) PET/CT shows two hot spots, corresponding to the adenopathy and the wall thickening in the pyriform sinus; endoscopic biopsy confirmed squamous cell cancer in the pyriform sinus.
On the other hand, small lesions may not be large enough to accumulate sufficient tracer to become visible. Furthermore, some tissues show physiological tracer uptake, such as the salivary glands, lymphoid tissue, brain tissue, and also muscles may show uptake when activated. Also inflammatory processes may accumulate tracer. This may lead to false-positive results, but also to false-negative results, as pathologic uptake may become wrongly classified as physiologic.
Several studies have evaluated the use of PET to detect a CUP. In the study from Johansen et al.[7], 60 patients with a CUP were enrolled, and 19 were examined before and 41 after panendoscopy. In this study, most patients underwent PET; a minority had PET/CT. The detection rate of a primary tumour was somewhat higher in the pre- than in the postendoscopy group; although this difference was not statistically significant, possibly a number of tumours were detected by endoscopy in this group, resulting in a lower detection rate when PET was performed. The overall sensitivity was 86%, as a number of tumours were not seen on PET, but were detected after biopsies or after tonsillectomy. The false-negative rate is difficult to determine exactly in this context, as one can expect that a number of subclinical primaries will be eradicated by radiotherapy, and therefore will never be recognized. The specificity in this study was 69%. False-positive results using PET were not infrequent (up to 40% in the tongue base and tonsils), and were more frequent after panendoscopy. For this reason, these authors recommend obtaining a PET scan at an early stage; the disadvantage is that a number of patients will undergo this examination unnecessarily, as the tumour would have been detected during panendoscopy.
In the study reported by Roh et al.[8], PET/CT examinations were performed. The detection rate of the primary tumours was similar to Johansen’s study, but the specificity was substantially better (82%). This can be explained by a reduction in false-positive PET results by coregistration with CT, thus providing both physiologic and anatomic imaging capabilities.
The results reported by Cianchetti et al.[6], in which the patient population underwent a mix of PET and PET/CT, are clearly different. The detection rate using PET was only 14%. Furthermore, none of these tumours was detected based solely on PET, as in all these patients the physical examination and/or the results of the radiologic examination were suspicious (but not definitely positive), and these sites would have been biopsied in any case. Their conclusion was that the incremental benefit of PET over the physical examination and CT/MRI is limited.
Second primary tumours
Smoking and alcohol abuse irritate the entire mucosa of the respiratory tract, inducing premalignant and malignant lesions. This has led to the concept of field cancerization or condemned mucosa, initially published concerning the oral region, but this can be generalized for the entire head and neck mucosa. The reported frequency of a synchronous second malignant tumour (at the same time or within 6 months after identification of the index tumour) ranges from 2 to 20%.
Such a second malignant mucosal tumour may be discovered during the diagnostic work-up (or follow-up) of the first carcinoma in the respiratory tract. Sometimes, these second primary tumours are not detected or overlooked clinically, but may be discovered during the radiologic evaluation of the index tumour (Fig. 5).
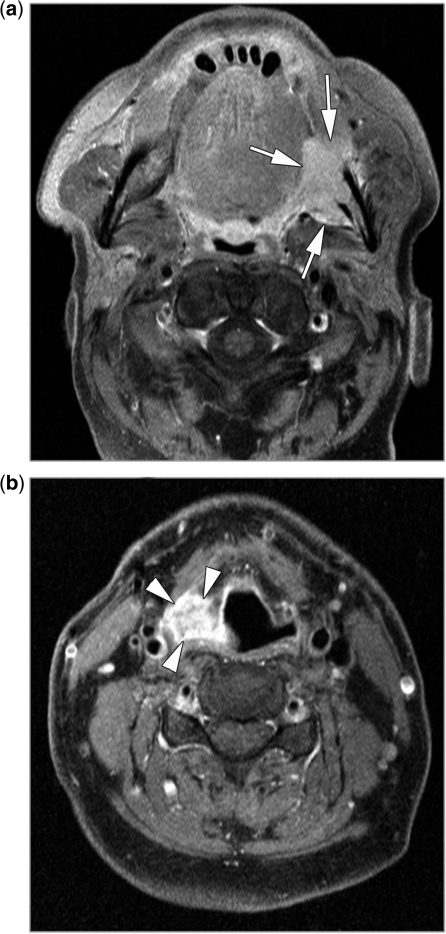
Figure 5.
(a,b) Contrast-enhanced T1-weighted spin echo images in a patient investigated for a cancer in the left retromolar trigone, invading the mandible (a, arrows). During this examination, a synchronous tumour is seen in the right pyriform sinus (b, arrowheads), which went undetected during the preceding physical examination of the head and neck. This was also a squamous cell cancer.
Whole body imaging in CUP
A clear advantage of PET and PET/CT is that these techniques allow nearly the entire body to be evaluated, as the primary tumour presenting with a neck adenopathy may be localized below the clavicles. The incidence of an infraclavicular primary tumour varies between 24% and 45%[6,9,10]. However, as such infraclavicular primaries are most commonly localized in the lungs or oesophagus, a chest CT could be considered as an alternative to PET; endoscopic examination of the oesophagus is done in the routine work-up of these patients.
The incidence of distant metastasis from a CUP is estimated to be between 3 and 14%[6,7], and most of these metastases also occur in the lungs.
In patients with head and neck cancer, the incidence of metachronous second primary tumours is between 6 and 9%; for this reason, some authors advocate an annual PET study in these patients as a screening modality[11], but such a follow-up strategy is not widely accepted. Whole body MRI may become an alternative to PET/CT in the future.
Conclusion
If a patient presents with a neck lump, without clinical evidence of a mucosal primary and without risk factors for developing squamous cell carcinoma, the first radiologic examination can be an ultrasound study. This non-invasive and cheap examination is helpful in differentiating between a benign (often cystic) lesion and neck nodal disease. Some tumours produce neck adenopathies displaying quite typical ultrasound features, such as papillary thyroid cancer, and during the same session a detailed evaluation of the thyroid gland can be performed.
If the patient is known to have a nodal metastasis from a squamous cell cancer, or has clear risk factors for such a neoplasm, the first radiologic examination can be a CT or MRI study of the neck. In a number of patients, the primary tumour will be found, and in some other patients, one or more suspicious areas can be identified that need to be scrutinized during an endoscopic examination including biopsies. Furthermore, CT or MRI provide useful information about the extent of nodal disease, and the possible presence of macroscopic extranodal tumour spread.
Conventional MRI has a comparable accuracy with CT for detecting a CUP, but further technical developments may improve the diagnostic yield of MRI. PET, and better PET/CT, is indicated if CT or MRI do not show the primary tumour, and also if there is an increased risk of distant metastases.
References
- 1.Erkal HS, Mendenhall WM, Amdur RJ, Villaret DB, Stringer SP. Squamous cell carcinomas metastatic to cervical lymph nodes from an unknown head-and-neck mucosal site treated with radiation therapy alone or in combination with neck dissection. Int J Radiat Oncol Biol Phys. 2001;50:55–63. doi: 10.1016/s0360-3016(00)01554-6. [DOI] [PubMed] [Google Scholar]
- 2.Lonneux M, Hamoir M, Reychler, et al. Positron emission tomography with [18F]fluorodeoxyglucose improves staging and patient management in patients with head and neck squamous cell carcinoma: a multicenter prospective study. J Clin Oncol. 2010;28:1190–5. doi: 10.1200/JCO.2009.24.6298. [DOI] [PubMed] [Google Scholar]
- 3.Scott AM, Gunawardana DH, Bartholomeusz D, Ramshaw JE, Lin P. PET changes management and improves prognostic stratification in patients with head and neck cancer: results of a multicenter prospective study. J Nucl Med. 2008;49:1593–600. doi: 10.2967/jnumed.108.053660. [DOI] [PubMed] [Google Scholar]
- 4.Hermans R, De Keyzer F, Vandecaveye V. Imaging techniques. In: Hermans R, editor. Head and neck cancer imaging. Berlin: Springer; 2006. p. 31. [Google Scholar]
- 5.Muraki AS, Mancuso AA, Harnsberger HR. Metastatic cervical adenopathy from tumors of unknown origin: the role of CT. Radiology. 1984;152:749–53. doi: 10.1148/radiology.152.3.6463256. [DOI] [PubMed] [Google Scholar]
- 6.Cianchetti M, Mancuso AA, Amdur RJ, et al. Diagnostic evalution of squamous cell carcinoma metastatic to cervical lymph nodes from an unknown head and neck primary site. Laryngoscope. 2009;119:2348–54. doi: 10.1002/lary.20638. [DOI] [PubMed] [Google Scholar]
- 7.Johansen J, Buus S, Loft A, et al. Prospective study of 18FDG-PET in the detection and management of patients with lymph node metastases to the neck from an unknown primary tumor. Results from the DAHANCA-13 study. Head Neck. 2008;30:471–8. doi: 10.1002/hed.20734. [DOI] [PubMed] [Google Scholar]
- 8.Roh JL, Kim JS, Lee JH, et al. Utility of combined (18)F-fluorodeoxyglucose-positron emission tomography and computed tomography in patients with cervical metastases from unknown primary tumors. Oral Oncol. 2009;45:218–24. doi: 10.1016/j.oraloncology.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Grau C, Johansen LV, Jakobsen J, Geertsen P, Andersen E, Jensen BB. Cervical lymph node metastases from unknown primary tumors. Results from a national survey by the Danish Society for Head and Neck Oncology. Radiother Oncol. 2000;55:121–9. doi: 10.1016/S0167-8140(00)00172-9. [DOI] [PubMed] [Google Scholar]
- 10.Rusthoven KE, Koshy M, Paulino AC. The role of fluorodeoxyglucose positron emission tomography in cervical lymph node metastases from an unknown primary tumor. Cancer. 2004;101:2641–9. doi: 10.1002/cncr.20687. [DOI] [PubMed] [Google Scholar]
- 11.Bradley PH, Bradley PT. Searching for metachronous tumours in patients with head and neck cancer: the ideal protocol. Curr Opin Otolaryngol Head Neck Surg. 2010;18:124–33. doi: 10.1097/MOO.0b013e3283374ccf. [DOI] [PubMed] [Google Scholar]