Abstract
Imiquimod is a TLR agonist that is used as an antitumor agent, mainly against skin tumors. Its clinical benefits are well described in several studies; however, the mechanisms behind its antitumor effects are not completely understood. In this issue of the JCI, Drobits and colleagues demonstrate that topical application of imiquimod suppresses cutaneous melanoma by TLR7-dependent recruitment and transformation of plasmacytoid dendritic cells into killer cells; this occurs independently of conventional adaptive immune mechanisms.
Imiquimod is a synthetic imidazoquinoline with demonstrable antiviral and antitumor properties. It is formulated as a 5% cream and has been approved to treat certain types of actinic keratoses, which are premalignant, flat, scaly growths on the skin caused by too much sun exposure; some primary skin malignancies, including basal cell carcinoma (BCC) and squamous cell carcinoma (1); and external genital warts. The efficacy of imiquimod as a treatment for BCC is impressive: complete histological clearance is achieved in almost 80% of the cases (2). Imiquimod has also been used off-label to treat cutaneous melanoma and locally recurrent mucosal melanoma (3), although it is a less effective treatment for this primary skin malignancy than it is for BCC (4).
Imiquimod modulates diverse immune responses through TLR7 ligation
The antitumor effect of imiquimod is multifactorial. It has direct antiangiogenic (5) and caspase-mediated proapoptotic activity (6). However, it also acts as an “immune response modifier,” modulating the function of immune cells, especially antigen-presenting cells such as conventional dendritic cells (cDCs), plasmacytoid dendritic cells (pDCs), monocytes, and macrophages. The effects of imiquimod on immune cells are mediated via activating signals initiated by its binding to TLR7 and, in some instances, to TLR8 (4).
TLRs comprise a family of conserved, germ-line–encoded pattern recognition receptors that recognize diverse molecules from pathogens and are essential for host defense (7). Upon ligand binding, TLRs recruit an adaptor molecule, most frequently MyD88, and promote activation of signaling molecules and pathways (including the NF-κB and MAPK pathways) that lead to the production of proinflammatory cytokines (e.g., TNF and IL-12). In pDCs, activation of the transcription factor IRF7 after TLR7 ligation leads to MyD88-dependent production of type I IFNs and upregulation of TNF-related apoptosis-inducing ligand (TRAIL) and granzyme B (7), which confer on the pDCs a death-inducing effector function. IL-1β and IL-18 are also released through TLR-independent inflammasome activation (7). Imiquimod can directly (via a TLR) or indirectly (via the type I IFNs derived from imiquimod-stimulated pDCs) stimulate NK cells, CD8+ T cells, CD4+ T cells, and B cells. Agonists of TLRs, including imiquimod, can also reverse CD4+ Treg function in a TLR8 signaling–dependent, DC-independent manner (8).
As a result of their multifactorial antitumor effects, TLR agonists such as imiquimod are being widely tested as adjuvant therapies in cancer patients. Their administration has been associated with intratumoral infiltration of multiple subsets of DCs, and, when delivered in combination with tumor-associated antigens in humans, they have resulted in delayed time to tumor recurrence (4). However, TLR-activated cDCs and pDCs can also induce and/or recruit immune suppressive Tregs in vitro and in vivo, and high levels of pDCs in the tumor microenvironment are associated with poor prognosis (9), indicating that we are far from understanding how TLR agonists such as imiquimod modulate immune cell function and how to appropriately utilize them for the treatment of cancer.
In this issue of the JCI, Drobits and colleagues shed some light on these matters by examining the consequences of topical imiquimod application in an orthotopic mouse model of melanoma (10). The data generated identify pDCs as leaders of the antitumor response initiated by imiquimod.
Imiquimod clears melanoma through pDC-dependent innate immune mechanisms
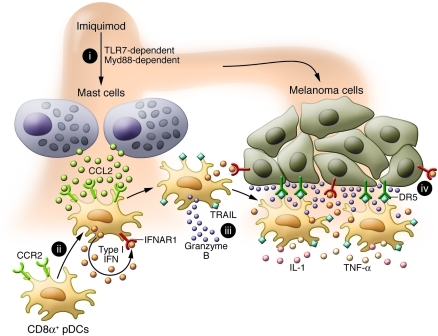
Drobits and colleagues found that imiquimod rapidly stimulated resident dermal mast cells to produce the chemokine CCL2 and that this promoted the migration of imiquimod-activated pDCs expressing CCR2, the CCL2 receptor, into the skin (ref. 10 and Figure 1). Importantly, the recruited pDCs were fully equipped to produce type I IFNs, which matured the pDCs into cytolytic cells and triggered the upregulation of specific receptors on melanoma cells that made them susceptible to the cytolytic effects of pDCs. Most significantly, the authors showed that imiquimod-mediated suppression of tumor growth was a direct consequence of the IFN-dependent cytolytic function of pDCs rather than direct apoptotic effects of type I IFNs and that it was independent of other innate or adaptive immune responses.
Figure 1. Mechanism of imiquimod-mediated tumor cell killing by pDCs.
(i) Skin application of imiquimod acts on mast cells through TLR7, inducing the secretion of CCL2. (ii) CD8α+ pDCs migrate to the skin toward CCL2 while at the same time being exposed to imiquimod. Imiquimod-stimulated pDCs produce high levels of type I IFNs, which have several effects. First (iii), in a paracrine loop, type I IFNs induce pDCs to kill tumor cells through upregulation of expression and/or secretion of cytolytic molecules such as TRAIL and granzyme B. Second (iv), type I IFNs induce on melanoma cells the expression of the receptor for TRAIL (DR5), which makes them susceptible to killing by TRAIL-expressing pDCs.
CCL2, is it bad or is it good?
The critical role played by dermal mast cells in the imiquimod-induced antitumor response defined by Drobits et al. (10) is novel. Mast cells, predominantly localized in the skin and mucosal surfaces, are known effectors of innate immunity, able to induce inflammatory reactions within minutes. They express TLR7 and release proinflammatory cytokines upon its ligation (11). Using Ccl2–/– mice, Drobits et al. showed that mast cell–associated CCL2 production was required for recruitment of pDCs into cutaneous tumors (10). Interestingly, the CCL2-mediated antitumor effects were due to its capacity to “condition” type I IFN–producing pDCs to migrate to inflamed skin and execute their killing function. Tumor cells have been shown to produce CCL2 (a capacity not evaluated in the present study), and this has not always been linked with a favorable outcome (12). Indeed, CCL2 produced by tumor cells or tumor stroma has been associated with tumor progression in mice as a result of its ability to recruit inflammatory CCR2-expressing monocytes that enhance the subsequent extravasation of the tumor cells through effects on endothelial cells (12). These mouse data, together with an observed clinical association between CCL2 overexpression in human cancers and poor prognosis (12), and the fact that CCL2-specific neutralizing antibodies inhibit human melanoma xenograft progression (13) have instead supported the development of therapeutic approaches that neutralize CCL2 activity. It seems, therefore, that the stimulus, source, and mechanisms of CCL2 action might be pivotal in the final outcome of an antitumor response.
Imiquimod’s dual role: controlling “attraction” and “activation”
The pattern of pDC migration reflects a complex interchange between chemokine receptor expression by pDCs and chemokine secretion in lymph nodes and inflamed tissues (14). In blood, pDCs, either constitutively or following activation, express CCR7 and respond to CCL21 in high endothelial venules, allowing them to home to lymph nodes. They may then traffic to peripheral sites such as inflamed skin by acquiring the ability to respond to CCL2 and other locally produced chemokines. This pattern of pDC migration is consistent with the concept that pDCs become activated in a sequential fashion. Besides CCL2, imiquimod induces the production of the chemokine ligands for CXCR3 (15) and the skin-homing chemokine CCL20 (14). A recent study suggested that upregulation of CCR6 and CCR10 (the receptors for CCL20 and CCL27/28) on pDCs is crucial for imiquimod-dependent pDC migration to the skin (14), although the relevance of CCL20 and whether CCR6-expressing pDCs acquire a killer phenotype was not investigated in the model studied by Drobits et al. Tumors including melanomas also produce chemokines that attract pDCs (16), but these may not activate their antitumor potential. The data generated by Drobits and colleagues (10), however, indicates for the first time that imiquimod has the dual advantage of conditioning skin resident and attracting migrating pDCs to produce type I IFNs and cytolytic molecules while at the same time regulating the production of chemokine gradients in the skin that control pDC trafficking.
The work of Drobits et al. showing that pDCs recruited into imiquimod-treated skin acquire cytolytic capacity against tumor cells (10) is in line with other reports suggesting an emerging role for pDCs as antitumor effector cells (15, 17, 18). Chaperot et al. first showed that pDCs could directly kill melanoma cell lines in a TLR7-dependent manner (17). This effect was later described in HIV infection, where TLR7-activated pDCs were found to kill virus-exposed CD4+ T cells (19). In skin tumors such as BCC there is evidence of pDC activation, local secretion of IFN-α (18), and pDC expression of TRAIL at the imiquimod-treated site (15). Drobits et al. reaffirmed the imiquimod-derived pDC killer phenotype (10) and demonstrated, using knockout mice, that it is dependent on TLR7, MyD88, and the receptor for type I IFN (IFNAR1). It was previously described how type I IFNs are essential for upregulation of the cytolytic molecules TRAIL and granzyme B on pDCs and the TRAIL receptor DR5 on tumor cells (7). Furthermore, Drobits and colleagues demonstrated that type I IFNs also control the initial production of CCL2 after imiquimod application, as Ifnar1–/– mice failed to produce CCL2 or to recruit pDCs into the dermis, suggesting that type I IFNs produced by the few resident dermal pDCs may be required to initiate the CCL2 gradient in the dermis.
Is tumor clearance reliant on pDCs alone?
Together, the data generated by Drobits et al. (10) led them to envision a two-phase response during imiquimod therapy that begins with fully competent pDC recruitment to the tumor area within 3 days, followed by a cascade of type I IFN–dependent mechanisms that contribute to enhancing the antitumor effect (Figure 1). This sustained antitumor effect was shown to occur without the contribution of other immune cells, as early depletion of NK or T cells did not affect tumor regression, giving pDCs a unique and individual role as tumor-killing cells at this stage. However, we believe that it is unlikely that pDCs alone maintain melanoma cells in “equilibrium” in the long term. Although the role of other immune cells was not tested at later time points, it is known that tumor-derived chemokines, in particular CCL2, can attract T cells, while type I IFNs can recruit T cells, B cells, and CD8α+ DCs into the tumor (20). Along those lines, imiquimod-treated skin lesions and tumors show a prominent inflammatory cell infiltrate (including CD8+ T cells, NK cells, and B cells; refs. 15, 21) that is sometimes associated with tumor regression. Moreover, direct injection of TLR9 agonists into melanomas has resulted in pDC-mediated NK cell activation and NK cell–mediated tumor cell death, resulting in cross-presentation of tumor antigens to T cells (22). Imiquimod-treated tumors also contain a decreased percentage of Tregs, both those that express Foxp3+ and those that produce IL-10 and TGF-β (23). In fact, Drobits et al. found that when CD4+ T cells were depleted in their model, tumor growth decreased (10), and this could perhaps be explained by a loss of Tregs. Together, these studies suggest that strong adaptive immune responses will ultimately be necessary to contain local tumor growth, metastatic disease, and local recurrences, and thus far, imiquimod treatment has resulted only in limited regression or stabilization of cutaneous melanoma metastasis (24).
Final remarks
In summary, TLR agonists such as imiquimod possess important properties that can be exploited for immunotherapy against tumors such as melanoma. As vaccine adjuvants, they are showing promise in the clinic against various cancers (4), even when injected directly into the tumor (25). However, further studies, especially those examining their effects in combination with radiation, chemotherapy, new biologics (e.g., antibodies specific for CTLA-4 or PD-1), and/or signaling pathway inhibitors (e.g., inhibitors of BRAF or MEK), are necessary in order to determine the most effective ways to improve their antitumor activity. Moreover, we cannot forget that some tumor cells express TLRs and this may eventually modulate the outcome of the antitumor response elicited by TLR agonists such as imiquimod (4). Finally, considering the new data generated by Drobits and colleagues, attention needs to be given to how efficiently chemokines, which attract or recruit multiple types of antitumor cells into tumors, are elicited to optimize the outcome of TLR agonist therapy. Addition of chemokines and/or application of combinations of TLR agonists that elicit relevant chemokines directly into tumors may improve the fight against resistant skin tumors.
Acknowledgments
The authors acknowledge support in part from the Melanoma Research Alliance and the following NIH awards: R01AI081848 and R37AI044628.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2012;122(2):481–484. doi:10.1172/JCI61345
See the related article beginning on page 575.
References
- 1.Stanley MA. Imiquimod and the imidazoquinolones: mechanism of action and therapeutic potential. Clin Exp Dermatol. 2002;27(7):571–577. doi: 10.1046/j.1365-2230.2002.01151.x. [DOI] [PubMed] [Google Scholar]
- 2.Geisse J, Caro I, Lindholm J, Golitz L, Stampone P, Owens M. Imiquimod 5% cream for the treatment of superficial basal cell carcinoma: results from two phase III, randomized, vehicle-controlled studies. . J Am Acad Dermatol. 2004;50(5):722–733. doi: 10.1016/j.jaad.2003.11.066. [DOI] [PubMed] [Google Scholar]
- 3.Smyth EC, et al. Treatment of locally recurrent mucosal melanoma with topical imiquimod. J Clin Oncol. 2011;29(33):e809–e811. doi: 10.1200/JCO.2011.36.8829. [DOI] [PubMed] [Google Scholar]
- 4.Gnjatic S, Sawhney NB, Bhardwaj N. Toll-like receptor agonists: are they good adjuvants? Cancer J. 2010;16(4):382–391. doi: 10.1097/PPO.0b013e3181eaca65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li VW, Li WW, Talcott KE, Zhai AW. Imiquimod as an antiangiogenic agent. J Drugs Dermatol. 2005;4(6):708–717. [PubMed] [Google Scholar]
- 6.Meyer T, Nindl I, Schmook T, Ulrich C, Sterry W, Stockfleth E. Induction of apoptosis by Toll-like receptor-7 agonist in tissue cultures. Br J Dermatol. 2003;149(suppl 66):9–14. doi: 10.1046/j.0366-077x.2003.05632.x. [DOI] [PubMed] [Google Scholar]
- 7.Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011;34(5):637–650. doi: 10.1016/j.immuni.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Peng G, et al. Toll-like receptor 8-mediated reversal of CD4+ regulatory T cell function. Science. 2005;309(5739):1380–1384. doi: 10.1126/science.1113401. [DOI] [PubMed] [Google Scholar]
- 9.Wei S, et al. Plasmacytoid dendritic cells induce CD8+ regulatory T cells in human ovarian carcinoma. Cancer Res. 2005;65(12):5020–5026. doi: 10.1158/0008-5472.CAN-04-4043. [DOI] [PubMed] [Google Scholar]
- 10.Drobits B, et al. Imiquimod clears tumors in mice independent of adaptive immunity by converting pDCs into tumor-killing effector cells. J Clin Invest. 2012;122(2):575–585. doi: 10.1172/JCI61034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heib V, et al. Mast cells are crucial for early inflammation, migration of Langerhans cells, and CTL responses following topical application of TLR7 ligand in mice. Blood. 2007;110(3):946–953. doi: 10.1182/blood-2006-07-036889. [DOI] [PubMed] [Google Scholar]
- 12.Qian BZ, et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475(7355):222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gazzaniga S, et al. Targeting tumor-associated macrophages and inhibition of MCP-1 reduce angiogenesis and tumor growth in a human melanoma xenograft. J Invest Dermatol. 2007;127(8):2031–2041. doi: 10.1038/sj.jid.5700827. [DOI] [PubMed] [Google Scholar]
- 14.Sisirak V, et al. CCR6/CCR10-mediated plasmacytoid dendritic cells recruitment to inflamed epithelia following instruction in lymphoid tissues. Blood. 2011;118(19):5130–5140. doi: 10.1182/blood-2010-07-295626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stary G, Bangert C, Tauber M, Strohal R, Kopp T, Stingl G. Tumoricidal activity of TLR7/8-activated inflammatory dendritic cells. J Exp Med. 2007;204(6):1441–1451. doi: 10.1084/jem.20070021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sozzani S, Vermi W, Del Prete A, Facchetti F. Trafficking properties of plasmacytoid dendritic cells in health and disease. Trends Immunol. 2010;31(7):270–277. doi: 10.1016/j.it.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Chaperot L, et al. Virus or TLR agonists induce TRAIL-mediated cytotoxic activity of plasmacytoid dendritic cells. J Immunol. 2006;176(1):248–255. doi: 10.4049/jimmunol.176.1.248. [DOI] [PubMed] [Google Scholar]
- 18.Urosevic M, et al. Disease-independent skin recruitment and activation of plasmacytoid predendritic cells following imiquimod treatment. J Natl Cancer Inst. 2005;97(15):1143–1153. doi: 10.1093/jnci/dji207. [DOI] [PubMed] [Google Scholar]
- 19.Hardy AW, Graham DR, Shearer GM, Herbeuval JP. HIV turns plasmacytoid dendritic cells (pDC) into TRAIL-expressing killer pDC and down-regulates HIV coreceptors by Toll-like receptor 7-induced IFN-alpha. Proc Natl Acad Sci U S A. 2007;104(44):17453–17458. doi: 10.1073/pnas.0707244104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuertes MB, et al. Host type I IFN signals are required for antitumor CD8+ T cell responses through CD8{alpha}+ dendritic cells. J Exp Med. 2011;208(10):2005–2016. doi: 10.1084/jem.20101159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adams S, et al. Immunization of malignant melanoma patients with full-length NY-ESO-1 protein using TLR7 agonist imiquimod as vaccine adjuvant. J. Immunol. 2008;181(1):776–784. doi: 10.4049/jimmunol.181.1.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu C, et al. Plasmacytoid dendritic cells induce NK cell-dependent, tumor antigen-specific T cell cross-priming and tumor regression in mice. J Clin Invest. 2008;118(3):1165–1175. doi: 10.1172/JCI33583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark RA, et al. Human squamous cell carcinomas evade the immune response by down-regulation of vascular E-selectin and recruitment of regulatory T cells. J Exp Med. 2008;205(10):2221–2234. doi: 10.1084/jem.20071190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolf IH, Smolle J, Binder B, Cerroni L, Richtig E, Kerl H. Topical imiquimod in the treatment of metastatic melanoma to skin. Arch Dermatol. 2003;139(3):273–276. doi: 10.1001/archderm.139.3.273. [DOI] [PubMed] [Google Scholar]
- 25.Brody JD, et al. In situ vaccination with a TLR9 agonist induces systemic lymphoma regression: a phase I/II study. J Clin Oncol. 2010;28(28):4324–4332. doi: 10.1200/JCO.2010.28.9793. [DOI] [PMC free article] [PubMed] [Google Scholar]