Abstract
Objectives
1) to compare the effect of functional electrical stimulation (FES) to that of hinged ankle-foot orthosis (AFO) on assisting foot clearance, gait speed and endurance and 2) to determine whether there is added benefit in using the FES in conjunction with the hinged AFO in individuals with incomplete spinal cord injury (ISCI).
Design
Within-subject comparison of walking under 4 conditions: 1) AFO, 2) FES, 3) AFO and FES, and 4) no orthosis. A plastic hinged AFO was used for all AFO conditions.
Setting
Tertiary rehabilitation centre.
Participants
19 individuals with ISCI.
Main Outcome Measures
The self-selected gait speed, six-minute walk distance, and foot clearance values were compared between conditions.
Results
Gait speed increased with FES (p < .05) and with AFO (p = .06). Six-minute walk distance also increased with AFO (P < .05). No difference was seen between the two forms of orthoses in both gait speed and endurance. The greatest increase in gait speed and endurance from the ‘no orthosis’ condition was measured with the ‘AFO and FES’ combined condition. Foot clearance improved with FES but not with AFO. Subjects that showed increase in gait speed with FES demonstrated weaker hip flexors, knee flexors, and ankle dorsiflexors than those that did not benefit from FES.
Conclusions
Both the FES and the hinged AFO promote walking and FES is only superior to AFO in increasing foot clearance values. When looking at the combination of results, the hinged AFO and FES together may offer advantages over either device alone.
Keywords: Spinal Cord Injuries, Walking, Electric stimulation, Orthotic devices
Individuals with incomplete spinal cord injury (ISCI) often retain or regain the ability to walk. However, walking may not be their selected method of mobility due to their limited speed and endurance which is frequently well below that required for community activities.1,2 Inefficient limb clearance due to reduced hip, knee, and ankle excursions during the swing phase of the gait cycle is a common contribution to the pathology of gait after ISCI.
The traditional approach to assist foot clearance during swing is the use of an ankle foot orthosis (AFO) which maintains the foot in a dorsiflexed position throughout the gait cycle. However, an AFO offers poor cosmesis, bulkier footwear, and restriction of ankle movement which may hinder other tasks such as transfers. An alternative approach to aid foot clearance is to electrically stimulate the common peroneal nerve to produce ankle dorsiflexion during swing. Stimulation of the peroneal nerve may also trigger reflex synergistic flexion enhancing hip and knee flexion during the swing phase of gait. 3,4
The first application of electrical stimulation to prevent foot drop during the swing phase of gait was by Liberson et al.,5 who stimulated the peroneal nerve in persons with hemiparesis. Twelve years later, Kralj & Grobelnik6 proposed the use of functional electrical stimulation (FES) for restoring walking in persons with spinal cord injury. Since then, many investigators have studied the benefits of several types of FES systems in this population and there has been considerable development in the technology of FES systems. Reported benefits of FES include reduction of tone,7,8 spasms,7,8 and oxygen consumption/energy cost,8–10 increase independence in activities of daily living,11 and improvement in gait performance.8,10,12–15
In spite of the extensive literature on the benefits of FES, studies on the effects of simple single-channel FES systems (e.g., peroneal nerve stimulators) on walking parameters in persons with ISCI are scarce. Given the recent advances in the technology of such devices, it would be beneficial to determine whether these simple systems can improve gait performance and whether the improvements are superior to those attained with devices such as an AFO which is often considered the standard of care. Stein et al.12 and later Wieler et al.15 studied such FES systems and found increases in gait speed when participants walked with the use of FES as opposed to no FES. To date, no study has compared the benefits of FES with those of AFO in individuals with ISCI. This information would allow clinicians to make better recommendations regarding technical aids. In addition, identifying characteristics of those individuals that most benefit from FES would provide further guidance in determining the proper device for individual clients.
The purpose of this study was: 1) to compare the effect of FES to that of AFO on assisting foot clearance, improving gait speed and endurance (as measured by the six-minute walk test), 2) to determine whether there is added benefit in using the FES in conjunction with AFO, and 3) to identify motor characteristics of those that benefit from the use of FES in individuals with ISCI.
METHODS
Participants
Nineteen participants with ISCI were recruited on a volunteer basis. Criteria for inclusion in the study were as follows: 1) present with foot-drop as a result of a chronic (at least 1 year post event) ISCI and 2) able to walk independently or with supervision for at least six minutes (with rest intervals) with or without mobility aids/orthoses. Persons who had orthopaedic or neurological conditions in addition to the spinal cord injury were excluded from the study. Ethics approval was obtained from the local university and hospital ethics committees. Each participant was informed of the study procedures before giving their consent to participate in the study.
Participant characteristics are summarized in Table 1. Neurological levels and impairment scales were determined according to the American Spinal Injury Association (ASIA) standards.16 Ambulation was categorized by the physical therapist (based on an interview and assessment) into 6 categories as described by Perry et al.:17 physiological walker, limited household walker, unlimited household walker, most-limited community walker, least-limited community walker, and community walker.
Table 1.
Participant characteristics (N=19)
| Variable | Mean | Standard Deviation |
|---|---|---|
| Age (years) | 42.7 | 13.6 |
| Time since injury (years) | 11.9 | 11.3 |
| Height (m) | 1.72 | 0.09 |
| Leg length (m) | 0.83 | 0.05 |
| Weight (kg) | 74.9 | 13.3 |
|
| ||
| Neurological level (paraplegia/tetraplegia) | 8/11 | |
| Sex (M/F) | 13/6 | |
| More affected side (R/L) | 12/7 | |
| ASIA Impairment Scale (C/D) | 5/14 | |
| Ambulation Status (Pw/LHw/UHw/MLCw/LLCw/Cw) | 2/2/3/4/3/5 | |
Abbreviations: Male (M), Female (F), Right (R), Left (L), Physiological walker (Pw), Limited Household walker (LHw), Unlimited Household walker (UHw), Most Limited Community walker (MLCw), Least Limited Community walker (LLCw), Community walker (Cw).
FES system
The FES system used in this study was the WalkAide system which features an inbuilt sensor that measures the tilt of the shank with respect to gravity18 (Figure 1). The WalkAide was attached to the participant’s lower leg on the more affected side, just below the knee with the electrodes over the common peroneal nerve. The tilt sensor was set up to trigger the stimulation of the nerve during the swing phase of gait (i.e., from end of stance phase when the lower leg is tilted back to the beginning of the next stance phase when the lower leg is tilted forward in front of the body). Prior to testing, stimulation levels were adjusted for optimal walking performance and comfort by a physical therapist and each participant. All participants had at least one practice session prior to the testing day.
Figure 1.

Illustration of the FES system and typical hinged AFOs used in this study.
Procedures
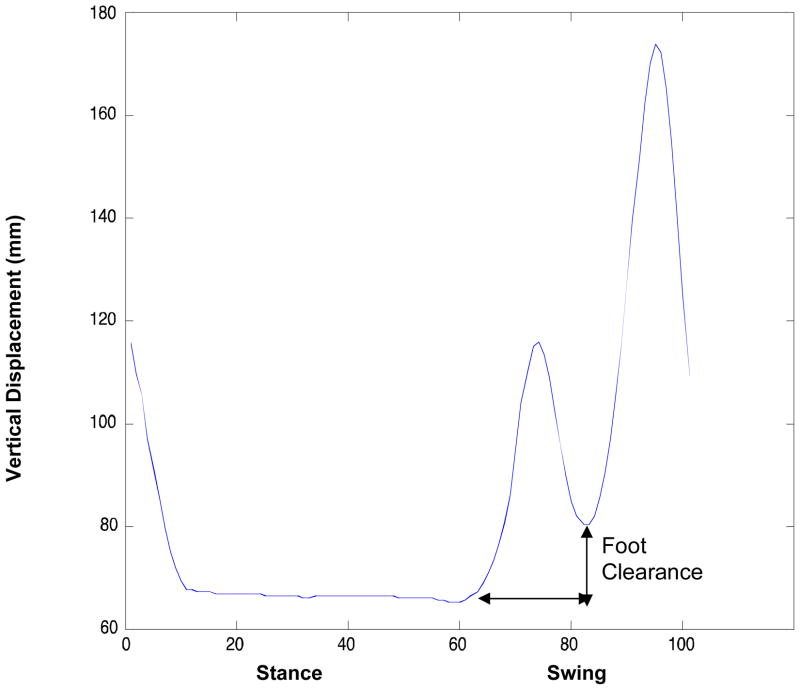
Participants were asked to walk with their usual mobility aid at their “most comfortable speed” (i.e. self-selected speed) along an 8-meter walkway for three trials each under four conditions: 1) with AFO, 2) with FES, 3) with AFO and FES, and 4) with no orthosis. The order of the condition in which the test was performed was randomly selected. To minimize bias, instructions provided by the investigators were consistent and no encouragement was given for any of the testing conditions. When necessary, rest breaks were taken between trials to ensure that participants were not fatigued and the trial reflected their true self-selected speed. A rest session and then a practice walking trial were implemented between each condition to minimize possibility of carryover between conditions. Nine of the 19 subjects had some previous exposure to the FES system (two had purchased one over 6 months prior and seven others had been introduced to it during rehabilitation). For the AFO conditions, a plastic hinged AFO was used (Figure 1) to allow for movement at the ankle when the stimulator was on during the swing phase of gait. This type of AFO stops ankle plantarflexion while it allows free dorsiflexion in both the stance and swing phases of gait. The AFO was custom fitted as recommended by the physical therapist for each participant. An optoelectronic sensor (Nothern Digital, Waterloo, Canada) was used to track infrared emitting diodes (IREDs) attached to the participants’ lateral malleoli and fifth metatarsal-phalangeal joints (MT). In this camera set-up, the error of locating the coordinates of an IRED in space was 0.9 mm in the anterior/posterior direction and 0.45 mm in the up/down direction.19 Data was collected at 60Hz. Gait speed was calculated using cumulative consecutive stride lengths (forward distance covered by the lateral malleolus marker from initial contact to the next initial contact of the same leg) in the middle 4-meter section (i.e., representative window of constant gait speed) of the 8-meter walkway and the corresponding elapsed time. The MT marker was used to calculate foot clearance (i.e., toe clearance). The minimum vertical displacement of the MT marker during stance was set at “zero”. For each gait cycle, foot clearance was defined as the difference in vertical height between “zero” and the vertical displacement when the MT marker drops to minimum clearance in mid-swing after the initial rise in early swing (Figure 2). The mean of at least five gait cycles from the three walking trials was calculated.
Figure 2.
Illustration of “foot clearance” using vertical displacement measures of the MT marker.
Following the gait assessment, participants returned to our centre to perform the six-minute walk tests as a measure of gait endurance under the four conditions. The four six-minute walk tests were performed on two separate days to minimize fatigue. For subjects with very low activity tolerance, the tests were performed on four separate days. Participants were instructed to walk for six minutes, covering as much ground as possible, on a flat surface around two marked lines that were 18.5 meters apart without stopping unless they needed to.20 No verbal feedback or phrases of encouragement were provided except one minute before the end of the test, at which point they were informed of the elapsed time.
For measures of muscle strength, a physical therapist performed the manual muscle test on each participant for eight lower limb muscle groups (hip flexors/extensors/abductors, knee flexors/extensors, ankle dorsiflexors/plantarflexors, and toe extensors) in standardized positions.21 Muscle strength was graded on a ten-grade scale (0–5) as per Herbison et al.22. We have previously evaluated the test-retest reliability (separate days) for manual muscle testing in a small group (N = 8) of individuals with spinal cord injury and found the intraclass correlation to be 0.82–0.99 for the eight lower limb muscle groups. Others22–24 have also reported high reliability for upper and lower limb manual muscle testing in persons with spinal cord injury.
Data analysis
Descriptive statistics were performed for all variables measured. Univariate analysis of variance blocked for subject was used to compare differences in outcome measures (gait speed, six-minute walk distance, and foot clearance) across the four conditions: 1) AFO, 2) FES, 3) AFO and FES, and 4) no orthosis. Post-hoc tests were performed using Duncan’s test. In addition, to determine the strength characteristics of the participants that showed improvement in gait speed with the use of FES when compared to the ‘no orthosis’ condition, secondary analyses were performed. Participants were divided into 2 groups: ‘improved’ (i.e., speed increased by > 5%) and ‘not improved’ groups. Mann-Whitney U tests were used to compare the strength of each of the eight muscle groups of the more affected and less affected sides between the two groups. We used parametric tests for the functional measures as the data showed or approached normal distribution. However, nonparametric tests were used for the muscle grades as most of these measures displayed non-normal distribution (Shapiro-Wilks Test). A significant level of p < .05 (2-tailed) was selected for all statistical tests. All statistical analyses were performed with SPSS 9.0 software.
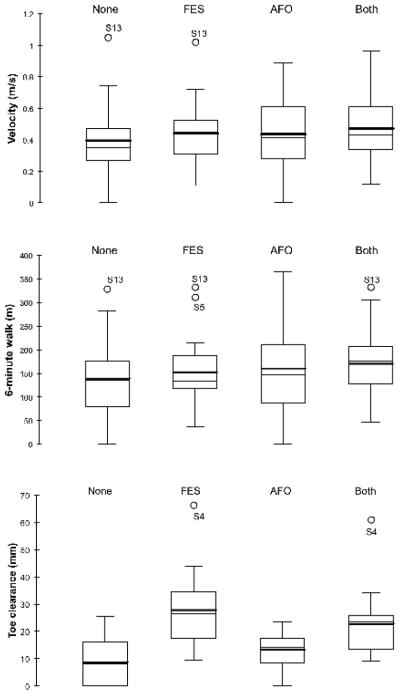
RESULTS
All but one participant had bilateral weakness with one side more affected than the other. The weakest muscle groups were the more affected ankle dorsiflexors and hip extensors which ranged from grades 0 to 3 (Table 2). Gait speed was low with a mean of 0.47 m/s or less for all conditions (Table 3, Figure 3). Consequently, the six-minute-walk distance was also low with as many as six participants covering less than 100 m during the allotted six minutes. One participant was unable to walk without the use of FES; therefore, his speed, six-minute walk distance, and foot clearance were entered as zero for the ‘no orthosis’ and ‘AFO’ conditions. One participant did not return after the first session to perform the six-minute-walk tests and two other participants did not complete all four six-minute walk tests, therefore N < 19 (N = 18 for ‘AFO’ and ‘AFO and FES’, N = 17 for ‘no orthosis’ and ‘FES’) for the six-minute walk distance analyses. All but one participant used a mobility aid (cane = 8, 2-canes = 1, 1-crutch = 1, 2-crutches = 5, walker = 3) and three participants customarily used an AFO for household/community mobility.
Table 2.
Muscle strength (manual muscle test) of participants (N=19) and muscle strength comparisons between the ‘improved’ (N=10) and the ‘not improved’ (N=9) groups.
| Muscle group | Side | Mean ± SD (N=19) | Improved (N=10) | Not improved (N=9) | p |
|---|---|---|---|---|---|
| Hip Flexors | More affected | 2.13 ± 0.76 | 1.75 | 2.55 | 0.02* |
| Less affected | 3.50 ± 0.76 | 3.30 | 3.72 | 0.42 | |
| Hip Extensors | More affected | 1.82 ± 1.04 | 1.40 | 2.28 | 0.02* |
| Less affected | 3.02 ± 1.24 | 2.80 | 3.28 | 0.51 | |
| Hip Abductors | More affected | 2.02 ± 1.37 | 1.70 | 2.39 | 0.41 |
| Less affected | 3.32 ± 1.02 | 3.00 | 3.67 | 0.17 | |
| Knee Flexors | More affected | 2.45 ± 1.22 | 1.95 | 3.00 | 0.02* |
| Less affected | 4.08 ± 0.75 | 3.95 | 4.22 | 0.55 | |
| Knee Extensors | More affected | 3.37 ± 0.96 | 3.00 | 3.78 | 0.10 |
| Less affected | 4.34 ± 0.62 | 3.95 | 4.78 | 0.00* | |
| Ankle Dorsiflexors | More affected | 1.39 ± 1.16 | 0.85 | 2.00 | 0.02* |
| Less affected | 3.87 ± 1.10 | 4.00 | 3.72 | 0.67 | |
| Ankle Plantarflexors | More affected | 2.00 ± 1.11 | 1.60 | 2.44 | 0.13 |
| Less affected | 3.39 ± 1.01 | 3.20 | 3.61 | 0.55 | |
| Great toe Extensors | More affected | 2.97 ± 1.51 | 2.45 | 3.56 | 0.13 |
| Less affected | 4.29 ± 1.07 | 4.25 | 4.33 | 0.81 |
Significant at p < .05. p was calculated using Mann-Whitney U tests.
Participants were categorized as ‘improved’ if their gait speed improved by at least 5% with the use of FES as compared to ‘no orthosis’.
Table 3.
Gait speed (m/s), six-minute walk distance (m), and foot clearance values (mm) for each of the four conditions
| Variable | No orthosis | AFO | FES | AFO and FES |
|---|---|---|---|---|
| Gait speed | 0.40 (0.23) | 0.43 (0.22) * | 0.44 (0.22) † | 0.47 (0.22) †‡ |
| Six-minute walk distance | 138.52 (80.49) | 160.87 (90.59) † | 152.37 (78.39) | 170.55 (76.39) †|| |
| Foot clearance | 8.78 (8.16) | 13.25 (5.85) ¶ | 27.88 (13.48) †**†† | 22.81 (11.59) †** |
p = 0.06 from ‘no orthosis’ condition
p < 0.05 from ‘no orthosis’ condition
p = 0.05 from ‘AFO’ condition
p < 0.05 from ‘FES’ condition
p = 0.09 from ‘no orthosis’ condition
p < 0.05 from ‘AFO’ condition
p = 0.06 from ‘AFO and FES’ condition
Figure 3.
Graphical representation of means (thick lines) and medians (thin lines) of the three main outcome variables (gait speed, six-minute walk distance, and foot clearance) with outliers labeled.
There was a significant increase in gait speed when participants used the FES compared to ‘no orthosis’ (average increase of 10%), though the greatest increase was shown when FES was used in conjunction with a hinged AFO (18% increase) (Table 3). Although values did not reach statistical significance, there was a trend towards an increase in gait speed when using the hinged AFO compared to ‘no orthosis’ (p = 0.06). The distance walked in six minutes was also improved when participants walked with the hinged AFO, either alone or with FES from ‘no orthosis’. In addition, the six-minute-walk distance for the ‘AFO and FES’ condition was significantly higher than for the ‘FES’ condition. No difference was seen between the two forms of orthoses when used alone for either of the two walking measures. As expected, foot clearance improved with the use of FES, whether used alone or in conjunction with the hinged AFO both from ‘no orthosis’ and ‘AFO’ conditions. Foot clearance with and without AFO was not significantly different from each other.
In an attempt to determine the strength characteristics of the individuals with ISCI who most benefit from the use of FES, participants were divided into ‘improved’ (N = 10) and ‘not improved’ (N = 9) groups based on their gait speed improvement (an increase of at least 5%) from the ‘no orthosis’ condition to the ‘FES’ condition. Results of the Mann-Whitney U tests revealed a significant difference between the two groups for the more affected hip flexor/extensor, knee flexor and ankle dorsiflexor strength as well as for the less affected knee extensor strength. In all three cases, the ‘improved’ group demonstrated reduced strength compared to the ‘not improved’ group (Table 2).
DISCUSSION
The main purpose of this study was to determine whether gait speed and endurance of persons with ISCI who present with foot drop can be improved with the use of devices such as AFOs and simple FES systems and whether additional benefits exist when these two devices are used jointly. The FES system used in this study was the WalkAide system which is a simple non-invasive 1-channel stimulator designed to stimulate the common peroneal nerve and assist with foot clearance during swing and thus improve walking.
Both the FES and the hinged AFO demonstrated some walking benefits when used either alone or in combination and no difference in walking measures was evident between these two forms of orthoses. Previous studies12,15 have also reported moderate improvements in gait speed (20–28%) with FES-assisted walking in persons with ISCI consistent with findings in the present study. However, Ladouceur & Barbeau25,26 found that spatio-temporal parameters of gait were similar with and without FES and only improved with long-term use of FES. One reason for this discrepancy in results may be the difference in the subject population studied. As many as 4/14 participants in the study by Ladouceur & Barbeau25,26 walked at a speed > 1m/s, whereas only one participant in the present study was able to walk at such speed. It has been reported that there is an effect of speed on the degree of improvements in gait speed during FES assisted walking. For example, Wieler et al.15 found that simple FES systems were of most benefit to subjects who walked very slowly. Likewise, Ladouceur & Barbeau25 also found a negative correlation between gait speed and orthotic effect of FES, i.e., the greater the speed, the less the effect of FES. In fact, when we compared the speeds of our ‘improved’ (mean speed 0.29 m/s) and ‘not improved’ (mean speed 0.52 m/s) groups, the same trend was seen. Participants covered a greater distance when using the hinged AFO as opposed to ‘no orthosis’ indicating that the support provided by the AFO allowed them to walk further. Although the use of FES and hinged AFO had different effects on walking (one promoted speed while the other promoted endurance), differences between the two devices were not significant for functional measures.
Foot clearance was greatest when walking with FES and it was the only measure that resulted in significant differences between the two types of orthoses. Thus, the FES was effective in preventing foot drop during swing possibly due to increased flexion angles at the hip, knee and ankle as a result of the flexion withdrawal response evoked by the FES as suggested by others4. Ladouceur & Barbeau26 found that hip angular excursion and ankle dorsiflexion angle were increased during swing with FES-assisted walking in persons with chronic ISCI. Further inspection of the data is necessary to confirm whether this is also true in our subject group. In spite of the significant increase in foot clearance with FES-assisted walking compared with AFO-assisted walking, no difference was seen in walking measures between these two devices. That is, the increase in foot clearance provided by the FES over the hinged AFO did not translate into additional benefits in walking. The foot clearance provided by the AFO (13.25 ± 5.85), although not statistically significant (p = 0.09), may be enough to show improvements in walking and a further increase in limb clearance does not grant cumulative benefit. In fact, foot clearance as defined by the vertical displacement of the MT joint in healthy adults has been reported to be as low as 16mm.27 Thus, the required amount of foot clearance for an efficient gait is minimal.
The overall results suggest that the hinged AFO and FES combination offers advantages over either device alone. It is possible that the added stability provided by the AFO combined with the increase in foot clearance aided by the FES during swing helped to generate additional improvement in walking. Thus, our results indicate that one type of orthosis is not superior to the other and suggest that they complement each other in promoting gait performance, the FES assisting during swing and the AFO during stance. It has been suggested that AFOs may improve the ability to support body weight during initial stance,28 improve progression of foot contact during stance,29 and improve the ability to generate push-off in late stance.28,30 Ladouceur & Barbeau25 reported that FES is useful when used as a training tool rather than as an orthosis. In the present study, the FES had an orthotic effect especially when used in conjunction with AFO as evidenced by the significant, although moderate, increase in gait speed. The long-term benefits of such combined systems need to be explored in controlled clinical trials.
Among participants in this study, the ones that did benefit from FES alone (i.e., showed an increase in gait speed by > 5%) demonstrated weaker hip flexors/extensors, knee flexors and ankle dorsiflexors on their more affected side (the side where FES was applied) and weaker knee extensors on their less affected side compared to those that did not benefit from FES. Closer inspection of our data suggests that individuals with no active movement against gravity (i.e., grade < 2.5) in the hip flexors, knee flexors, and ankle dorsiflexors of their more affected side benefit from the use of FES. That is, for these individuals, the FES may play a role in substituting for the weakness in these muscle groups. This concurs with the role of FES in triggering a flexion response which results in hip, knee, and ankle flexion during swing thereby improving limb clearance.4 Biomechanical analyses would be beneficial to confirm these hypotheses.
One limitation of this study is the small sample size. A post-hoc analysis found, however, that the power of tests were satisfactory (> 0.90 for each of the three main outcome variables of gait speed, six-minute walk distance and foot clearance). Future investigations with a larger sample would increase the generalizability of the findings from this study. In addition, though our results indicate statistical significant improvements in function, the clinical relevance of an increase in speed of 0.04 – 0.07 m/s is debatable. These increases in speed, although small, corresponded to 10–18% improvements, which could have a meaningful effect, particularly for an individual with a slow gait speed. Nine of the 19 subjects had had some previous experience with the FES system prior to the study which might have affected performance. However, a post-hoc sub-analyses did not show that these individuals had any greater improvements than the other subjects. Finally, participants and investigators were not blinded from the conditions tested which may have affected the performance of the participants. Participant blinding was not possible and investigator blinding was difficult was the AFO cannot be hidden from view when in use. In an effort to minimize this bias, investigators’ involvement (e.g., instructions, encouragement, etc) was kept consistent during data collection and conditions were blinded when processing data.
CONCLUSION
This study compared the effects of FES and/or hinged AFO on gait performance of individuals with ISCI. The results indicated that although the use of either type of orthosis promoted walking, the ‘AFO and FES’ combination provided greater benefit than either device alone in overall gait function as measured by gait speed and six-minute walk distance. The FES was only superior to the hinged AFO in improving limb clearance during swing; however, this increase in foot clearance did not translate into a further increase in function when the two types of devices were compared. In general, individuals who presented with lower leg muscle strength appeared to benefit more from the FES system than those with stronger leg muscles.
Acknowledgments
We would like to acknowledge grants from the Paralyzed Veterans of America Spinal Cord Research Foundation and the BC Neurotrauma Fund and salary support (career scientist award) to JJE from the Canadian Institute of Health Research (MSH-63617) and Michael Smith Foundation for Health Research.
Footnotes
Suppliers
NeuroMotion, Suite 401, 11044 82nd Avenue, Edmonton, AB, Canada T6G 0T2.
Northern Digital, 103 Randall Dr., Waterloo, ON, Canada, N2V 1C5
SPSS Inc., 233 S. Wacker Dr., Chicago, IL, 60606
References
- 1.Waters RL, Yakura JS, Adkins RH. Gait performance after spinal cord injury. Clin Orthop. 1993;288:87–96. [PubMed] [Google Scholar]
- 2.Krawetz P, Nance P. Gait analysis of spinal cord injured subjects: effects of injury level and spasticity. Arch Phys Med Rehabil. 1996;77:635–8. doi: 10.1016/s0003-9993(96)90000-3. [DOI] [PubMed] [Google Scholar]
- 3.Kralj A, Bajd T, Turk R. Enhancement of gait restoration in spinal injured patients by functional electrical stimulation. Clin Orthop Rel Res. 1988;233:34–43. [PubMed] [Google Scholar]
- 4.Bajd T, Kralj A, Stefancic M, Lavrac N. Use of electrical stimulation in the lower extremities of incomplete spinal cord injured patients. Artificial Organs. 1999;23:403–9. doi: 10.1046/j.1525-1594.1999.06360.x. [DOI] [PubMed] [Google Scholar]
- 5.Liberson WT, Holmquest HJ, Scot D, Dow M. Functional electrotherapy, stimulation of the peroneal nerve synchronized with the swing phase of the gait of hemiplegic subjects. Arch Phys Med Rehabil. 1961;42:101–5. [PubMed] [Google Scholar]
- 6.Kralj A, Grobelnik S. Functional electrical stimulation- A new hope for paraplegic patients? Bulletin of Prosthetic Research. 1973;10:75–102. [Google Scholar]
- 7.Bajd T, Kralj A, Turk R, Benko H, Sega J. Use of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injuries. J Biomed Eng. 1989;11:96–102. doi: 10.1016/0141-5425(89)90115-5. [DOI] [PubMed] [Google Scholar]
- 8.Granat MH, Ferguson ACB, Andrews BJ, Delargy M. The role of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injury- observed benefits during gait studies. Paraplegia. 1993;31:207–15. doi: 10.1038/sc.1993.39. [DOI] [PubMed] [Google Scholar]
- 9.Isakov E, Douglas R, Berns P. Ambulation using the reciprocating gait orthosis and functional electrical stimulation. Paraplegia. 1992;30:239–45. doi: 10.1038/sc.1992.62. [DOI] [PubMed] [Google Scholar]
- 10.Winchester P, Carollo JJ, Habasevich R. Physiologic costs of reciprocal gait in FES assisted walking. Paraplegia. 1994;32:680–6. doi: 10.1038/sc.1994.110. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson ACB, Granat MH. Evaluation of functional electrical stimulation for an incomplete spinal cord injured patient. Physiotherapy. 1992;78:253–6. [Google Scholar]
- 12.Stein RB, Belanger M, Wheeler G, Wieler M, Popovic DB, Prochazka A, Davis LA. Electrical systems for improving locomotion after incomplete spinal cord injury: an assessment. Arch Phys Med Rehabil. 1993;74:954–9. [PubMed] [Google Scholar]
- 13.Gallien P, Brissot R, Eysette M, Tell L, Barat M, Wiart L, Petit H. Restoration of gait by functional electrical stimulation for spinal cord injured patients. Paraplegia. 1995;33:660–4. doi: 10.1038/sc.1995.138. [DOI] [PubMed] [Google Scholar]
- 14.Bajd T, Stefancic M, Matjacic Z, Kralj A, Savrin R, Benko H, et al. Improvement in step clearance via calf muscle stimulation. Medical & Biological Engineering & Computing. 1997;35:113–6. doi: 10.1007/BF02534140. [DOI] [PubMed] [Google Scholar]
- 15.Wieler M, Stein RB, Ladouceur M, Whittaker M, Smith AW, Naaman S, Barbeau H, Bugaresti J, Aimone E. Multicenter evaluation of electrical stimulation systems for walking. Arch Phys Med Rehabil. 1999;80:495–500. doi: 10.1016/s0003-9993(99)90188-0. [DOI] [PubMed] [Google Scholar]
- 16.Maynard FM, Jr, Bracken MB, Creasy G, Ditunno JF, Jr, Donovan WH, Ducker TB, Garber SL, Marino RJ, Stover SL, Tator CH, Waters RL, Wilberger JE, Young W. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. 1997;35:266–74. doi: 10.1038/sj.sc.3100432. [DOI] [PubMed] [Google Scholar]
- 17.Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the stroke population. Stroke. 1995;26:982–9. doi: 10.1161/01.str.26.6.982. [DOI] [PubMed] [Google Scholar]
- 18.Dai RC, Stein RB, Andrews BJ, James KB, Wieler M. Application of tilt sensors in functional electrical stimulation. IEEE Trans Rehabil Eng. 1996;4:63–72. doi: 10.1109/86.506403. [DOI] [PubMed] [Google Scholar]
- 19.Northern Digital. Optotrak Guide. Version 1.0.1. Waterloo (Ontario): 1995. [Google Scholar]
- 20.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–23. [PMC free article] [PubMed] [Google Scholar]
- 21.Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4. Baltimore: Lippincott Williams & Wilkins; 1993. [Google Scholar]
- 22.Herbison GJ, Isaac Z, Cohen ME, Ditunno JF., Jr Strength post-spinal cord injury: myometer vs manual muscle test. Spinal Cord. 1996;34:543–8. doi: 10.1038/sc.1996.98. [DOI] [PubMed] [Google Scholar]
- 23.Frese E, Brown M, Norton BJ. Clinical reliability of manual muscle testing: middle trapezius and gluteus medius muscles. Phys Ther. 1987;67:1072–6. doi: 10.1093/ptj/67.7.1072. [DOI] [PubMed] [Google Scholar]
- 24.Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther. 1987;67:1342–7. doi: 10.1093/ptj/67.9.1342. [DOI] [PubMed] [Google Scholar]
- 25.Ladouceur M, Barbeau H. Functional electrical stimulation-assisted walking for persons with incomplete spinal injuries: longitudinal changes in maximal overground walking speed. Scand J Rehab Med. 2000;32:28–36. doi: 10.1080/003655000750045712. [DOI] [PubMed] [Google Scholar]
- 26.Ladouceur M, Barbeau H. Functional electrical stimulation-assisted walking for persons with incomplete spinal injuries: changes in the kinematics and physiological cost of overground walking. Scand J Rehab Med. 2000;32:72–9. doi: 10.1080/003655000750045587. [DOI] [PubMed] [Google Scholar]
- 27.Winter DA. The biomechanics and motor control of human gait: normal, elderly and pathological. Waterloo (Ontario): University of Waterloo press; 1991. [Google Scholar]
- 28.Lehmann JF, Condon SM, de Lateur BJ, Price R. Gait abnormalities in peroneal nerve paralysis and their corrections by orthosesL biomechanical study. Arch Phys Med Rehabil. 1986;67:380–6. [PubMed] [Google Scholar]
- 29.Abel MF, Juhl GA, Vaughan CL, Damiano DL. Gait assessment of fixed ankle-foot orthoses in children with spastic diplegia. Arch Phys Med Rehabil. 1998;79:126–33. doi: 10.1016/s0003-9993(98)90288-x. [DOI] [PubMed] [Google Scholar]
- 30.Lehmann JF, Esselman PC, Ko MJ, Smith JC, deLateur BJ, Dralle AJ. Plastic ankle-foot orthoses: evaluation of function. Arch Phys Med Rehabil. 1983;64:402–7. [PubMed] [Google Scholar]