Abstract
Objective
This study tested a model for explaining how stress is associated with depressive symptoms in a sample of spouse caregivers of patients with Alzheimer’s disease. It was hypothesized that more depressive symptoms would be significantly correlated with both “primary” caregiver stressors (i.e., care recipient problem behaviors) and “secondary” stress (i.e., role overload), but that this relationship would be significantly mediated by 4 variables: a) personal mastery, b) coping self-efficacy, c) activity restriction, and d) avoidance coping.
Method
We used an asymptotic and resampling strategy for simultaneously testing multiple mediators of the stress-to-depressive symptoms pathway.
Results
Greater stress was significantly related to more depressive symptoms. Increased stress was also associated with reduced personal mastery and self-efficacy, as well as increased activity restriction and avoidance coping. Finally, these four mediators accounted for a significant amount of the relationship between stress and depressive symptoms.
Discussion
These results suggest multiple pathways by which both primary and secondary caregiver stresses may be associated with increased depressive symptoms, and may argue for multiple treatment targets for caregiver interventions.
Keywords: Alzheimer’s Disease, Depression, Coping, Behavioral Activation, Self Efficacy, Stress-Process
INTRODUCTION
Stress Process and Caregiving
Stress process models (Lazarus & Folkman, 1984; Pearlin, Lieberman, Menaghan, & Mullan, 1981) propose that stressful life events act to erode personal resources (e.g., positive coping) or enhance maladaptive responses (e.g., negative coping), which in turn produce negative outcomes (e.g., depression). That is, stress process models suggest that life stresses alone cannot explain the intensity of one’s negative psychiatric outcomes, but rather that certain coping or behavioral factors mediate, or explain the relationship between life stress and negative outcomes.
Alzheimer’s caregiving is one common model for studying stress impact, particularly the impact of stress on depressive symptoms, a finding that has been consistently demonstrated in the literature (Cohen et al., 1990; Gallagher, Rose, Rivera, Lovett, & et al., 1989; Mahoney, Regan, Katona, & Livingston, 2005; Ory, Hoffman, Yee, Tennstedt, & Schulz, 1999; Williamson & Schulz, 1993). Within the context of caregiving, a number of life changes occur over an extended period of time, such as changes to their loved one’s cognitive and behavioral functioning. Two reviews in the literature have reported on the many aspects of caregiving that are linked with psychiatric morbidity in the caregiver, many of which require constant adaptation on the part of the caregiver (Schulz, O’Brien, Bookwala, & Fleissner, 1995; Schulz & Sherwood, 2008). Indeed, in these reviews and elsewhere (Burns, 1996; Schulz et al., 1995; Schulz & Sherwood, 2008; Teri et al., 1992), memory and behavior problems exhibited by Alzheimer’s disease (AD) patients are particularly deleterious to the caregiver in terms of psychiatric well-being.
Pearlin and colleagues (1990) laid out a stress process model of caregiving that identified how caregiving stresses produce negative outcomes such as depression. In this model, “primary” stress indicators, such as a care recipient’s problematic behavior, as well as “secondary” indicators (i.e., feeling overwhelmed by caregiving) are believed to result in intrapsychic strains. These intrapsychic strains then mediate the relations between caregiving stress and negative outcomes such as depression. Within this model, intrapsychic strains included both global and situational strains. One example of a global strain was a reduced sense of personal mastery, or the belief that in general life circumstances are under one’s control. A situational strain of note is confidence in one’s ability to engage in situation-specific strategies for coping with stress (i.e., self-efficacy for coping). While both constructs appear related, personal mastery is differentiated from self-efficacy in that mastery relates to one’s belief that life circumstances are controllable, whereas self-efficacy is conceptualized as confidence in the ability to perform specific actions that result in a desired outcome (Bandura, 1977). Both self-efficacy and personal mastery are believed to impact depression via motivational processes, such that individuals who do not believe they have the ability to impact stressful circumstances are believed to exert less effort toward coping processes thought to help reduce depressive symptoms (Bandura, 1997).
Empirical examination has validated the role of reduced personal mastery in depression. Bookwala and Schulz (1998) studied 300 spousal caregivers and found that behavioral and functional impairment on the part of the care recipient was associated with reduced personal mastery, which in turn was associated with increased caregiver depression, although the authors did not formally test for mediation in this study. Three other studies demonstrated direct relationships between mastery and depressive symptoms but also did not test for mediation. Yates and colleagues (1999) reported that in caregivers of disabled elders, reduced personal mastery was associated with increased report of depressive symptoms. Li et al. (1999) conducted an 18-month longitudinal study of daughter caregivers of an aging parent and found that lower levels of personal mastery were associated with increased levels of depression. Another study of adult daughter caregivers of an impaired parent found that personal mastery was negatively associated with both depressive symptoms and life satisfaction (Christensen, Stephens, & Townsend, 1998). Finally, Sherwood and colleagues (2007) demonstrated that more care recipient problem behaviors were associated with reduced personal mastery, which was associated with greater experience of depressive symptoms in a sample of caregivers of patients with primary malignant brain tumor (PMBT). Further, this study demonstrated that personal mastery partially mediated the stress to depressive symptoms pathway.
Studies examining the role of reduced self-efficacy in caregiver depression also exist. For example, Fortinsky, Kercher, and Burant (2002) found that greater self-efficacy for managing care recipient symptoms was associated with reduced depression in Alzheimer’s caregivers. Gilliam and Steffen (2006) found that reduced caregiving self-efficacy was directly related to greater depressive symptoms in dementia caregivers. A third study found that problem-solving self-efficacy was directly and negatively related to distress in caregivers of frail elders (Zeiss, Gallagher-Thompson, Lovett, Rose, & McKibbin, 1999). Finally, Steffen and colleagues (2002) found that three different types of caregiving self-efficacy (i.e., obtaining respite, responding to patient disruptive behaviors, and controlling upsetting thoughts) were all negatively correlated with depressive symptoms in family caregivers of cognitively impaired older adults. However, with the exception of Zeiss and colleagues, none of these studies examined self-efficacy for problem-focused coping, and none examined the mediating role of self-efficacy on the stress to depression path. Thus, the current study expands on the previous literature by studying the mediating role of self-efficacy for problem-focused coping on the stress-to-depression path.
Coping in the Stress Process
Stresses may also result in activation or erosion of coping responses. One coping response theoretically important in the development and maintenance of depression is restriction of social and recreational activity. Indeed, the “Activity Restriction” model (Williamson & Shaffer, 2000) of depression proposes that life stresses result in restriction of social and recreational activities thought to provide a natural reinforcement to the individual. In the “absence” of these reinforcing activities, increases in depressive symptoms occur. Confirmation of the activity restriction model has been demonstrated in pain patients (Williamson & Schulz, 1995), women with stage 1, stage 2, or stage 3 breast cancer (Williamson, 2000), and Alzheimer’s caregivers (Mausbach, Patterson, & Grant, 2008).
Another coping process that may be activated by caregiving stress is avoidance coping. Sometimes called “escape-avoidance” coping (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986), this type of coping is characterized by attempts to avoid or escape stresses, or to avoid having to deal with the stresses. Escape-avoidance can be cognitive in nature (e.g., “tried to forget the whole thing”; “refused to believe it had happened”) and/or behavioral (“avoided being with people in general”; “went on as if nothing had happened”). In operant conditioning theory, escape-avoidance coping behaviors (i.e., avoiding negative stimuli) are conceptualized to produce short-term relief from life stresses, thus serving a reinforcing role in perpetuating escape-avoidance behaviors. However, ultimately a great amount of effort may be expended engaging in avoidance behaviors. Further, because negative stimuli are not completely avoidable, long-term effects of avoidance coping may actually be detrimental to the individual. Use of avoidance coping has been repeatedly associated with negative psychiatric outcomes (Penley, Tomaka, & Wiebe, 2002), including among caregivers (Garity, 1997; Wright, Lund, Caserta, & Pratt, 1991). Among caregivers, avoidance appears to be more strongly linked with depressive symptoms than other forms of coping (Powers, Gallagher-Thompson, & Kraemer, 2002). One study showed that caregiving stresses are indeed associated with increased use of avoidance coping, which in turn was associated with increased depression, and that avoidance coping partially mediated the relationship between care recipient problem behaviors and depressive symptoms (Mausbach et al., 2006).
The Current Study
When looking at the literature, it appears there is strong support for individual constructs within various stress models, including in caregiving samples. Specifically, previous studies have demonstrated that at least two general intrapersonal constructs are linked to depressive symptoms in caregivers: a) “intrapsychic” strains such as reduced personal mastery (Bookwala & Schulz, 1998) and self-efficacy (Steffen et al., 2002), and b) negative coping styles such as avoidance coping (Mausbach et al., 2006) and activity restriction (Mausbach et al., 2008). While Pearlin’s stress-process model (1990) conceptualizes these constructs as potential buffers of the relationship of stress to depression, caregiver stress has also been theoretically and/or empirically linked directly to reduced personal mastery (Sherwood et al., 2007) and self efficacy (Pearlin et al., 1990), as well as increased avoidance coping (Mausbach et al., 2006) and activity restriction (Mausbach et al., 2008). In turn, these intermediate outcomes are believed (and have been shown) to at least partially mediate the stress-depression pathway. For example, Williamson has conceptualized activity restriction as a mediator of the relationship between life strains and depressive symptoms, which has been demonstrated with various populations (Williamson, 2000; Williamson & Schulz, 1992; Williamson & Shaffer, 2000). Further, avoidance coping has been found to partially mediate, rather than moderate, the stress-depression pathway among AD caregivers (Mausbach et al., 2006), suggesting some forms of coping may have different roles in the development and maintenance of depressive symptoms.
However, perhaps due to methodological limitations, the empirical literature examining the mediating role of these variables appears a) lacking, as with the case of self-efficacy, or b) emphasizes single stress measurements and/or single intermediate variables, whereby only one measure of caregiving stress (e.g., care recipient problem behaviors) and one mediating factor (e.g., avoidance coping) is examined (Mausbach et al., 2006; Sherwood et al., 2007). However, the stress process likely (and theoretically) involves several intermediate pathways in response to multiple stresses, and what appears overlooked in the literature is the role of multiple mediators of the stress to depressive symptoms pathway in caregivers.
The current study seeks to remedy these previous limitations by examining the mediating role of 4 specific variables in the stress-depressive symptoms pathway. Specifically, we examined a multiple mediator model for which we hypothesized that caregiving stress would be significantly associated with decreased personal mastery and self-efficacy, and increased avoidance coping and activity restriction, and that these intermediate variables would all significantly mediate the relationship between caregiver stress and increased depressive symptoms. Also, to demonstrate robustness of the model we sought to empirically test this model using two measures of caregiver stress. Consistent with Pearlin’s model (1990), the first is a primary measure of caregiver stress (i.e., care recipient problem behaviors) and the second is a secondary measure (i.e., role overload). We hypothesized that our 4 variables (i.e., personal mastery, self-efficacy, activity restriction, and avoidance coping) would significantly mediate the relationship between stress and depressive symptoms.
METHODS
Participants
The study population consisted of 126 men and women who were married to a spouse diagnosed with probable AD. All were enrolled in the Alzheimer’s Caregiver Project at the University of California San Diego, which was designed to study psychobiological consequences of caregiving-related stress. To be eligible, participants must have been married to a spouse with a diagnosis of probable AD, be at least 55 years of age, and providing in-home care for their spouse (i.e., the demented spouse could not be living separately from the participant). Participants were excluded if they suffered from a serious physical or mental health condition (e.g., cancer requiring chemotherapy; schizophrenia), if they had severe hypertension defined as blood pressure of 200/120 mmHg, or if they were taking anti-coagulant medication. The latter 2 criteria were included to prevent confounds related to the biological aspects of the project. Participants were primarily recruited by referral from the UCSD Alzheimer’s Disease Research Center (ADRC), through local caregiver support groups, by referral from other participants, and via staff presentation(s) at local health fairs. The protocol was approved by the University’s Institutional Review Board (IRB) and all participants provided written, informed consent prior to participation.
Measures
Demographics and Caregiving Duties
Participants provided demographic information including age, gender, and educational attainment. In addition, caregivers responded to questions related to the number of years they had been providing care for their spouses and the average number of hours per day they provided care for their spouses.
Depressive Symptoms
Participants completed the short form of the Center for Epidemiologic Studies Depression scale (CESD-10) (Andresen, Malmgren, Carter, & Patrick, 1994). This scale contains 10 items assessing their experience of depressive symptoms during the past week, with response options ranging from 0 = “none of the time” to 3 = “most of the time”. Two of the items are reversed scored (i.e., “you felt hopeful about the future”; “you were happy”), and the 10 items are summed to create an overall score reflecting depressive symptoms. For the current study, coefficient alpha was .77.
Caregiver Stress
Participants completed two measures assessing their experience of stress. The first, which assessed primary caregiving stresses, was the Revised Memory and Behavior Problems Checklist (RMBPC) (Teri et al., 1992). This scale consists of 24 items assessing the extent to which care recipients displayed several memory and behavior problems over the past week (e.g., asked the same question over and over; became aggressive to others verbally; cried or became tearful). Caregivers responded to each item by indicating how often each behavior occurred using a 4-point Likert scale whereby 0 = “never”, 1 = “1–2 times”, 2 = “3–6 times”, and 3 = “daily or more often”. Responses to the 24 items were summed to create an overall score ranging from 0–72. Coefficient alpha for the current study was .81.
The second stress measure, reflecting the participant’s “secondary” experience of stress, was the Role Overload scale (Pearlin et al., 1990). For this scale, participants were asked to rate the extent to which 4 statements described them (e.g., “you are exhausted when you go to bed at night”). Responses were given on a 4-point Likert scale ranging from 0 = “not at all” to 3 = “completely”. The 4 items were summed to create a total “role overload” score. The coefficient alpha for this scale was .76.
Global Perceived Control
The Personal Mastery scale (Pearlin et al., 1981; Pearlin & Schooler, 1978) was used to assess caregivers’ sense of global control. For this scale, participants were asked to rate the extent to which they agreed or disagreed with 7 statements (e.g., “there is really no way you can solve some of the problems you have”). Responses were on a Likert scale with 0 = “strongly disagree”, 1 = “disagree”, 2 = “agree”, and 3 = “strongly agree”. Two items were reverse scored (i.e., “you can do just about anything you really set your mind to do”; “what happens to you in the future mostly depends on you”), and the 7 items were summed to create an overall score. In the current study coefficient alpha was .75.
Efficacy Beliefs
Caregivers completed the Coping Self-Efficacy scale (Chesney, Neilands, Chambers, Taylor, & Folkman, 2006), which assessed their level of confidence in performing specific actions to cope with stress. The scale consisted of 13 items assessing confidence in 3 domains: a) self-efficacy for using problem-focused coping (6 items; “make a plan of action and follow it when confronted with a problem”; “think about one part of the problem at a time”), b) self-efficacy for stopping unpleasant thoughts (4 items; “make unpleasant thoughts go away”), and c) self-efficacy for getting support (3 items; “get emotional support from friends and family”). Caregivers indicated how certain they believed they could perform each action on a scale from 0–10, with 0 = “cannot do at all”, 5 = “moderately certain can do”, and 10 = “certain can do”. Self-efficacy for each domain was the sum of the items in that domain. For the present study, the self-efficacy for using problem-focused coping scale was used. The coefficient alpha for this scale was .87.
Activity Restriction
The Activity Restriction Scale (Williamson & Schulz, 1992) was used to measure the extent to which caregivers felt restricted from engaging in social and recreational activities during the past month. The scale consists of 9 items (e.g., “going shopping”; “visiting friends”) to which participants rated their level of restriction using a 5-point Likert scale (0 = “never or seldom did this” to 4 = “greatly restricted”). The 9 items were summed to create an overall score. The coefficient alpha for this sample was .78.
Avoidance Coping
All participants completed the Revised Ways of Coping Checklist (RWCC)(Vitaliano, Russo, & Carr, 1985), which consists of 42 items assessing their use of various coping strategies to manage stress. For the present study, we utilized the Avoidance Coping subscale of the RWCC, which consists of 10 items (e.g., “went on as if nothing had happened”; “kept your feelings to yourself”). Participants responded by indicating the extent to which they used the following strategy to manage their most stressful stress during the past month. Response options were 0 = “never used”, 1 = “used somewhat”, 2 = “used quite a bit”, and 3 = “used a great deal”. The 10 items were summed to create an overall score, and Cronbach’s alpha for the Avoidance Coping scale was .62.
Care Recipient’s Cognitive and Functional Disability
Two scales were used to assess care recipient level of cognitive and functional disability. Both scales were administered to caregivers. The first was the Clinical Dementia Rating (CDR) scale (Morris, 1993), which was used to determine the severity of the care recipient’s dementia. Caregivers responded to a series of questions relating to their spouse’s functioning in six domains (e.g., memory, problem-solving). Based on scores in these domains, an overall dementia rating was given ranging from 0 (non-demented) to 3 (severely demented).
The second scale assessed care recipient ability to perform a variety of activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Caregivers were asked to indicate the extent to which their spouses depended on them for help with 15 ADL/IADL (e.g., eating, cooking, taking medications), with response options ranging from 0 = “not at all” to 4 = “completely”. The 15 items were summed to reflect the number of ADL/IADL the care recipient required help with. For the current sample, coefficient alpha was .91.
Data Analysis
We tested two multiple mediation models in which four proposed variables mediated the relationship between caregiving stress and depressive symptoms. Models 1 and 2 differed by the inclusion of a measure of “primary” stress (i.e., care recipient memory and problem behaviors; Problem Behaviors Model) and a measure of “secondary” stress (i.e., role overload; Role Overload Model). Our four proposed mediators were a) personal mastery (i.e., global perceived control), b) self-efficacy for using problem-focused coping (i.e., coping self-efficacy), c) activity restriction, and d) use of avoidance coping.
We used the bias corrected and accelerated bootstrapping method described by Preacher and Hayes (2008) to test the mediating effect of our proposed variables on the relations between stress and depressive symptoms. Specifically, we utilized the SPSS script offered by Preacher and Hayes (2008) to test for multiple mediation. As described previously (Briggs, 2007; Preacher & Hayes, 2008; Williams & MacKinnon, 2008), bootstrapping methods for examining mediating effects are preferred because they offer increased power and reasonable control over the type I error rate, particularly for small samples and when multivariate normality cannot be assumed. To test for mediation, a series of steps was undertaken. First, our 4 proposed mediators were regressed onto our stress measure (e.g., role overload or problem behaviors). Second, our 4 proposed mediators were entered into a regression predicting depressive symptoms (i.e., direct effects of mediators on DV). Third, multiple regression was used to assess the total effect of stress on depressive symptoms. A final analysis included the independent variable and all mediators as predictors of depressive symptoms. Bootstrapping determines the significance of the drop in the total effect when the potential mediators were included in the model and the significance of mediation for each proposed mediator as well as the 4 mediators as a set. For all analyses, a 95% confidence interval (CI) was used. Also, as recommended by Preacher and Hayes (2008), 5000 bootstrapping samples were generated in the current analyses.
RESULTS
Sample Characteristics
Descriptive characteristics of the sample are found in Table 1. Caregivers were primarily elderly, female, well educated, and providing care for individuals in mid-to-late stages of AD. In addition, bivariate correlations between the variables included in our models are presented in Table 2.
Table 1.
Characteristics of the Sample
| Caregiver Characteristics | |
| Age, M (SD) | 74.2 (8.0) |
| Female, n (%) | 89 (70.6) |
| Educational Attainment, n (%) | |
| < High School | 3 (2.4) |
| High School (or equivalent) | 23 (18.2) |
| Some College | 44 (34.9) |
| College Graduate | 21 (16.7) |
| Professional/Graduate Training | 35 (27.8) |
| Years Caregiving, M (SD) | 4.3 (3.4) |
| Hours of Care/Day, M (SD) | 7.6 (5.7) |
| Brief CESD Score, M (SD) | 8.8 (5.8) |
| Role Overload, M (SD) | 5.2 (3.2) |
| Personal Mastery, M (SD) | 11.5 (3.3) |
| SE for Problem-focused Coping, M (SD) | 43.9 (10.1) |
| Activity Restriction, M (SD) | 16.0 (5.7) |
| Care Recipient Characteristics | |
| Care Recipient CDR Score, n (%) | |
| 1.0 | 51 (40.5) |
| 2.0 | 66 (52.4) |
| 3.0 | 9 (7.1) |
| Care Recipient ADL/IADL Total, M (SD) | 35.9 (10.5) |
| Care Recipient Problem Behaviors, M (SD) | 23.7 (9.5) |
Table 2.
Bivariate correlations between model variables.
| Variable | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| 1. CESD | -- | |||||
| 2. Problem Behaviors | .36* | -- | ||||
| 3. Role Overload | .46* | .42* | -- | |||
| 4. Personal Mastery | −.53* | −.33* | −.46* | -- | ||
| 5. Coping Self-efficacy | −.52* | −.28* | −.31* | .35* | -- | |
| 6. Activity Restriction | .41* | .39* | .61* | −.40* | −.21* | -- |
| 7. Avoidance Coping | .53* | .26* | .29* | −.42* | −.29* | .27* |
p < .05
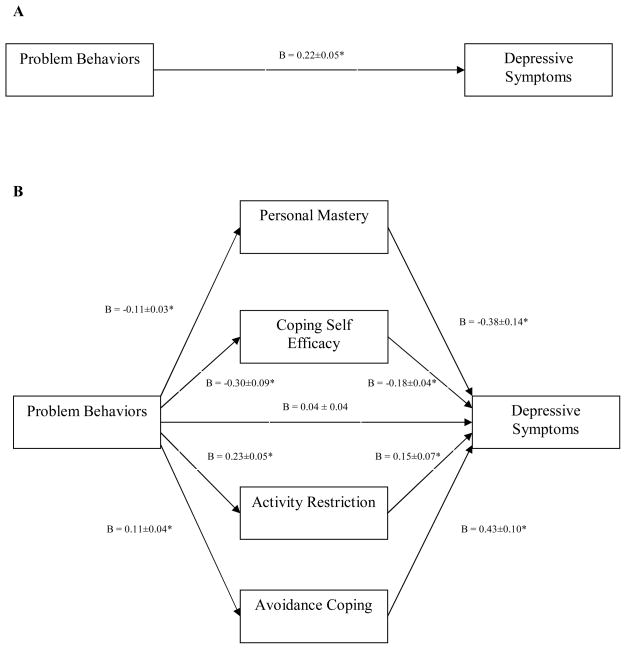
Problem Behaviors Model
Step 1 of our approach was to regress our 4 proposed mediators onto problem behaviors. Results of these analyses indicated that problem behaviors were significantly associated with all four proposed mediators and all were in the theoretically proposed direction. Specifically, greater number of problem behaviors was significantly associated with reduced personal mastery (B = −0.11; t = −3.89, df = 124, p < .001), increased avoidance coping (B = 0.11; t = 3.05, df = 124, p = .003), increased activity restriction (B = 0.23; t = 4.66, df = 124, p < .001), and reduced self-efficacy (B = −0.30; t = −3.22, df = 124, p = .002).
Step 2 examined the association of our 4 proposed mediators with depressive symptoms. Results of this analysis indicated that decreased personal mastery (B = −0.38; t = −2.81, df = 120, p = .006) and self-efficacy (B = −0.18; t = −4.51, df = 120, p < .001) were associated with increased depressive symptoms. In contrast, increased avoidance coping (B = 0.43; t = 4.11, df = 120, p < .001) and activity restriction (B = 0.15; t = 2.08, df = 120, p = .040) were both associated with greater depressive symptoms.
Steps 3 and 4 examined the total and direct effects of problem behaviors on depressive symptoms, respectively. Results of step 3 (total effect) indicated that the greater the number of problem behaviors the greater experience of depressive symptoms (B = 0.22; t = 4.30, df = 124, p < .001). However, in step 4, after controlling for our proposed mediators, the effect of problem behaviors was rendered non-significant (B = 0.04; t = 0.94, df = 120, p = .352). The total amount of variance accounted for by the overall model, which included problem behaviors and our 4 proposed mediators was 51.9% (adjusted R-squared = 50.0%).
Our final analysis examined the multiple mediation effect. Results of this analysis are found in Table 3. In this table, significance of our mediators is determined when the 95% confidence interval does not overlap ‘0’. In brief, our set of 4 proposed mediators significantly mediated the relationship between problem behaviors and depressive symptoms, with all four variables (i.e., avoidance coping, self-efficacy, activity restriction, and personal mastery) reaching statistical significance as mediators of the problem behaviors to depressive symptoms relationship. However, pairwise contrasts indicated that none of the 4 proposed mediators was of significantly greater magnitude than the other three (all p-values > .05). For example, the mediating effect of self-efficacy was not statistically stronger than that of personal mastery. Finally, we calculated the effect size κ2 as the proportion of the maximum possible indirect effect that could have occurred given our design and data (Preacher & Kelley, 2011). For personal mastery, κ2 = .119; for self-efficacy for problem-focused coping, κ2 = .148; for activity restriction κ2 = .058; and for avoidance coping, κ2 = .074. A complete description of these analyses is presented in Figure 1.
Table 3.
Mediation of the Effect of Problem Behaviors on Depressive Symptoms through Personal Mastery, SE for Problem-Focused Coping, Activity Restriction, and Avoidance Coping
| Point Estimate | Product of Coefficients | Bias Corrected and Accelerated CI | |||
|---|---|---|---|---|---|
|
| |||||
| SE | Z | 95% Lower | 95% Upper | ||
| Personal Mastery | .0434 | .0188 | 2.31 | .0138 | .0898 |
| SE for Problem-Focused Coping | .0534 | .0202 | 2.64 | .0216 | .1035 |
| Activity Restriction | .0357 | .0185 | 1.93 | .0029 | .0792 |
| Avoidance Coping | .0477 | .0193 | 2.47 | .0187 | .0921 |
| TOTAL | .1802 | .0396 | 4.54 | .1201 | .2475 |
Note. CI = Confidence Interval; SE = Self-Efficacy.
Figure 1.
Multiple mediation model depicting relations between primary stressors, multiple mediators, and depressive symptoms. Graphic A depicts the total effect of problem behaviors on depressive symptoms. Graphic B depicts the direct effect of problem behaviors on depressive symptoms after including mediators. Note. Values represent unstandardized regression coefficients ± standard error. * p < .05
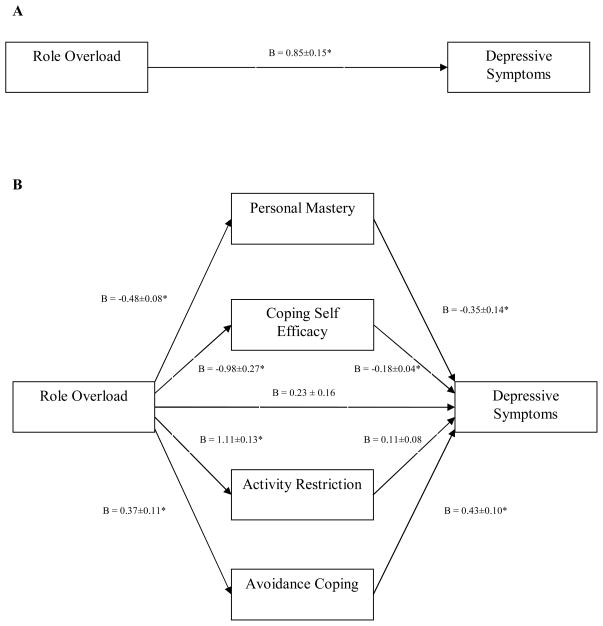
Role Overload Model
As mentioned above, we attempted to replicate (and confirm) our multiple mediation findings from the problem behaviors model using a subjective indicator of stress (i.e., role overload). Step 1 of this model examined the relationship between role overload and each of our 4 proposed mediators. As with our problem behaviors model, greater role overload was significantly associated with decreased personal mastery (B = −0.48; t = −5.72, df = 124, p < .001) and self-efficacy (B = −0.98; t = −3.59, df = 124, p < .001), whereas greater role overload was associated with increased avoidance coping (B = 0.37; t = 3.35, df = 124, p = .001) and activity restriction (B = 1.11; t = 8.64, df = 124, p < .001).
In step 2, decreased personal mastery (B = −0.35; t = −2.56, df = 120, p = .012) and self-efficacy (B = −0.18; t = −4.46, df = 120, p < .001) were significantly associated with increased depressive symptoms even when controlling for role overload. Greater avoidance coping was also significantly associated with more depressive symptoms (B = 0.43; t = 4.18, df = 120, p < .001). However, in this model, activity restriction was not significantly associated with depressive symptoms (B = 0.11; t = 1.32, df = 120, p = .189).
Step 3 indicated support for the relationship between role overload and depressive symptoms (B = 0.85; t = 5.78, df = 124, p < .001), such that higher overload was associated with more depressive symptoms. Step 4, which examined the direct effect of role overload on depressive symptoms after controlling for all 4 mediators, showed a drop in the association between role overload and depressive symptoms (B = 0.23; t = 1.48, df = 120, p = .142). The total amount of variance accounted for in this model was 52.4% (adjusted R-squared = 50.5%).
Consistent with our problem behaviors model, tests of significant mediation confirmed that, as a set, avoidance coping, self-efficacy, activity restriction, and personal mastery significantly mediated the relationship between role overload and depressive symptoms (see Table 4). However, in the role overload model, activity restriction did not reach significance as a mediator of the role overload-to-depressive symptoms relationship. As with our problem behaviors model, pairwise contrasts indicated that none of the 4 proposed mediators was of significantly greater magnitude than the other three (all p-values > .05). Finally, for personal mastery, κ2 = .178; for self-efficacy for problem-focused coping, κ2 = .174; for activity restriction κ2 = .059; and for avoidance coping, κ2 = .092. The overall model is depicted graphically in Figure 2.
Table 4.
Mediation of the Effect of Role Overload on Depressive Symptoms through Personal Mastery, SE for Problem-Focused Coping, Activity Restriction, and Avoidance Coping
| Point Estimate | Product of Coefficients | Bias Corrected and Accelerated CI | |||
|---|---|---|---|---|---|
|
| |||||
| SE | Z | 95% Lower | 95% Upper | ||
| Personal Mastery | .1665 | .0700 | 2.38 | .0488 | .3070 |
| SE for Problem-Focused Coping | .1738 | .0616 | 2.82 | .0753 | .3417 |
| Activity Restriction | .1211 | .0908 | 1.33 | −.0740 | .3248 |
| Avoidance Coping | .1573 | .0595 | 2.64 | .0485 | .3237 |
| TOTAL | .6187 | .1372 | 4.51 | .3523 | .9230 |
Note. CI = Confidence Interval; SE = Self-Efficacy.
Figure 2.
Multiple mediation model depicting relations between secondary stress, multiple mediators, and depressive symptoms. Graphic A depicts the total effect of role overload on depressive symptoms. Graphic B depicts the direct effect of role overload on depressive symptoms after including mediators. Note. Values represent unstandardized regression coefficients ± standard error. * p < .05.
DISCUSSION
The current study examined the evidence for a multiple mediation model of the stress-to-depressive symptoms pathway in elderly spouse caregivers of Alzheimer’s patients. Consistent with predictions, the set of four predicted mediators, namely avoidance coping, self-efficacy for using problem-focused coping, personal mastery, and activity restriction significantly explained the relationship between primary and secondary measures of caregiving stress and depression. Of the four proposed mediators, avoidance coping, self-efficacy, and personal mastery were significant individual mediators of the stress-to-depressive symptoms pathway in both model 1 and model 2. In other words, our data support that intrapsychic strains (i.e., reduced coping self-efficacy and personal mastery) secondary to caregiving stress and increased use of escape-avoidance coping were key variables explaining the pathway between caregiving stress and depression. Further, in model 1, activity restriction served as a significant mediator of the problem behaviors-to-depression pathway. Finally, while we did not present data using two additional self-efficacy subscales (i.e., self-efficacy for stopping unpleasant thoughts and self-efficacy for getting social support), formal tests using these as mediators (in place of self-efficacy for using problem-focused coping) indicated both served as significant mediators of the stress-to-depression pathway with very little impact to the overall model.
These results suggest that stressors associated with the caregiving role cannot entirely explain the severity of negative psychiatric outcomes. Rather, caregiving stress may diminish personal resources and/or enhance maladaptive responses, thereby resulting in consequences such as depression. These findings are also consistent with other caregiving studies examining intrapsychic strain and coping as mediators of adverse psychiatric outcomes (Mausbach et al., 2006; Sherwood et al., 2007). Whereas these previous studies examined single mediators, particularly novel about this study is the examination of multiple mediators using a bias corrected and accelerated bootstrapping method (Preacher & Hayes, 2008). Specifically, by simultaneously examining mediators and also by determining the strength of each mediator in relation to the others, the current multiple mediator test allowed for more complete assessment of the stress process model.
These results have implications for specific treatment targets for psychosocial interventions for Alzheimer’s caregivers. First, to avoid deleterious effects to both intermediate and downstream psychiatric outcomes (i.e., depression), one implication here is to reduce or prevent stress in caregivers. Because care recipient problem behaviors are often the most distressing aspect of caregiving (Burns, 1996; Schulz et al., 1995; Teri et al., 1992), treatments that effectively help caregivers manage this aspect of caregiving may be particularly effective at preventing disruptions to caregivers’ sense of personal mastery and self-efficacy, as well as use of avoidance coping strategies, which in turn may prevent the development of depressive symptoms. Despite the frequent use of antipsychotic medications to treat problem behaviors, these medications appear to have some risk associated with their use (Ray, Chung, Murray, Hall, & Stein, 2009; Ray et al., 2001), even among patients with dementia (Schneider, Dagerman, & Insel, 2005). A recent review of empirically based psychological treatments found two treatment approaches to be efficacious for reducing problem behaviors, namely progressively lowered stress threshold (PLST) and behavior management (Gallagher-Thompson & Coon, 2007). While these interventions directly target problem behaviors, their effects on caregiver outcomes (e.g., depressive symptoms) may be due to changes in mediating outcomes such as presented in our study. Future research should examine whether these treatments produce changes to various coping outcomes (e.g., mastery, self-efficacy, avoidance), and whether these changes mediate the relations between change in problem behaviors and change in depressive symptoms.
In addition to interventions for reducing problem behaviors, other caregiver interventions have demonstrated efficacy for reducing caregiver distress and improving some of the intermediate factors in our model [for review, see (Gallagher-Thompson & Coon, 2007)]. Specifically, Coon and colleagues (2003) found two interventions to be effective for reducing anger and depression as well as increasing self-efficacy in dementia caregivers. The first intervention focused on teaching caregivers cognitive (e.g., generating positive self-talk, monitoring and modifying unhelpful cognitions) and behavioral strategies (e.g., relaxation skills, assertiveness training) for managing frustration in caregivers. The second intervention focused on helping caregivers increase their engagement in pleasant events but did not emphasize cognitive strategies for managing distress. The efficacy of these interventions for increasing self-efficacy and reducing caregiver depression demonstrates how emphasizing the different foci of our multiple mediator model can result in similar treatment outcome. As mentioned above, future trials may consider examining whether interventions producing change in our mediating variables (e.g., self-efficacy, activity restriction) results in change in caregivers’ depressive symptoms.
Besides the use of psychosocial interventions to decrease caregiver stressors and depressive symptoms, it is important to highlight that the role of adult day health care (ADHC) in reducing stress. Utilizing ADCH services has been shown to affect some caregivers’ appraisals of both stressors and psychological well-being. For example, Zarit et al. (1998) showed that a treatment group of dementia caregivers who used adult day care services for 3 months had lower scores on their primary appraisals of overload and strain and reported significantly lower levels of anger and depression compared to a control group of caregivers not using adult day care services. One major benefit of ADHC is that it may provide caregivers relief of some of the negative consequences associated with providing constant care including activity restriction, thus allowing more time for personal, work, and/or other familial obligations.
Interestingly, in this study, activity restriction emerged as a significant mediator of caregiver depression in only the primary caregiving stress model. A previous analysis of dementia caregivers and non-caregiving controls conducted by our team found that activity restriction was a significant mediator of the relation between caregiving status (i.e. caregiver versus control) and depression (Mausbach et al., 2008). However, we found the effect size for the mediating effect of activity restriction to be identical in the problem behaviors and role overload models. Thus, although activity restriction did not meet significance in our role overload model, the effect was equal, suggesting it indeed has a role in the stress-to-depressive symptoms pathway.
This study highlights the different role that mediating variables may play in different points of the caregiving stress process, which is consistent with previous research (Romero-Moreno et al., 2011). Further, although activity restriction was not a significant mediator, it may continue to be a valid treatment target for psychosocial interventions. Indeed, previous studies have shown that purely behavioral interventions, in which participants learn how to increase the number of pleasurable events in their lives, are not only effective for reducing depressive symptoms, but also have positive effects on coping (Coon et al., 2003; Jacobson et al., 1996) and self-efficacy (Coon et al., 2003). To the extent that activity restriction is reduced in these interventions, and that activity restriction is related to the other mediators in our model, it is expected that targeting activity restriction may then result in changes to the other mediators in the model. Furthermore, if behavioral activation can directly increase mastery and self-efficacy, and curb the use of avoidance coping strategies, it would have a moderating effect upon the relationship between patient problem behaviors and development of depression. Further study is needed to directly examine this possibility which would have implications for the development of behavioral activation interventions, and we encourage those conducting intervention studies to examine these relationships.
Although this study had several strengths including its use of both primary and secondary measures of stress and the inclusion of multiple mediating variables, there are some limitations that must be acknowledged. First is the cross-sectional design of the study which precludes making any causal inferences. Therefore, it is impossible to determine the direction or reciprocal nature of the relationships between many of our outcomes (e.g. whether increased caregiver stress resulted in reduced personal mastery and self-efficacy or whether reduced personal mastery and self-efficacy caused increased caregiver stress). Indeed, true tests of mediation imply causality. However, as discussed by Preacher and Hayes (2008), establishing covariation in variables in important since correlation is a necessary, albeit insufficient, condition for establishing mediation. Therefore, in their manuscript, when correlation analyses are used, “causal” ordering of variables should be established on theoretical or procedural grounds, which we believe we have done in this study.
Another limitation of the present study is that our population consisted of exclusively spousal caregivers of patients with AD and therefore our data may not necessarily be representative or generalize to non-spousal caregivers or caregivers caring for persons with other types of illnesses (e.g. patients with cancer, schizophrenia, etc.). Indeed, literature suggests that the experience of depressive symptoms differs by relationship to the care recipient and nature of the disease. For example, Ory et al. (1999) reported that the strains of dementia caregiving were significantly greater than those of nondementia caregiving in terms of hours providing care per week, employment restrictions, leisure time, and spending time with other family members. Dementia caregivers also reported greater emotional and physical suffering as a result of caregiving. Thus, it is possible that some of the relationships between the multiple pathways described in our analysis were strengthened as a result of the distinctive stressors associated with dementia caregivers.
A third limitation is the low internal reliability of our avoidance coping scale (α = .62). We believe this may be due to the brevity of this subscale, which only consisted of 3 items. As a result, caution should be used when interpreting avoidance coping results. While future research should replicate our entire model, this would be particularly true of the mediating role of avoidance coping in the stress-depression relationship.
In sum, we found that avoidance coping, coping self-efficacy, activity restriction, and personal mastery significantly mediated the relationship between caregiving stress and depressive symptoms in a sample of spousal AD caregivers. The proposed pathway is that caregiving stressors (e.g., care recipient problem behaviors) result in increased use of avoidance coping and restriction of social activities, along with a reduced sense of personal mastery and self-efficacy for using problem-focused coping. The intermediate changes then result in increased experience of depressive symptoms. As a set, our two models each explained approximately 50% of the variance in depressive symptoms, suggesting these factors may indeed play an important role in the experience of depression and may be important treatment targets for psychosocial interventions for AD caregivers.
Acknowledgments
Funding for this study was provided by the National Institute on Aging (NIA) through awards R01 AG015301 and R01 AG031090.
References
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- Bookwala J, Schulz R. The role of neuroticism and mastery in spouse caregivers’ assessment of and response to a contextual stressor. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1998;53B:P155–P164. doi: 10.1093/geronb/53b.3.p155. [DOI] [PubMed] [Google Scholar]
- Briggs NE. Estimation of the standard error and confidence interval of the indirect effect in multiple mediator models. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2007;67(8-B):4755. [Google Scholar]
- Burns A. The institute of psychiatry Alzheimer’s disease cohort 1986–1992: Part 1--clinical observations. International Journal of Geriatric Psychiatry. 1996;11:309–320. [Google Scholar]
- Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology. 2006;11:421–437. doi: 10.1348/135910705X53155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen KA, Stephens MA, Townsend AL. Mastery in women’s multiple roles and well-being: adult daughters providing care to impaired parents. Health Psychology. 1998;17:163–171. doi: 10.1037//0278-6133.17.2.163. [DOI] [PubMed] [Google Scholar]
- Cohen D, Luchins D, Eisdorfer C, Paveza GJ, Ashford JW, Gorelick P, et al. Caring for relatives with Alzheimer’s disease: The mental health risks to spouses, adult children, and other family caregivers. Behavior, Health, & Aging. 1990;1:171–182. [Google Scholar]
- Coon DW, Thompson L, Steffen A, Sorocco K, Gallagher-Thompson D. Anger and depression management: Psychoeducational skill training interventions for women caregivers of a relative with dementia. The Gerontologist. 2003;43:678–689. doi: 10.1093/geront/43.5.678. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Kercher K, Burant CJ. Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging & Mental Health. 2002;6:153–160. doi: 10.1080/13607860220126763. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychology and Aging. 2007;22:37–51. doi: 10.1037/0882-7974.22.1.37. [DOI] [PubMed] [Google Scholar]
- Gallagher D, Rose J, Rivera P, Lovett S, et al. Prevalence of depression in family caregivers. The Gerontologist. 1989;29(4):449–456. doi: 10.1093/geront/29.4.449. [Vol 29(3) sic] [DOI] [PubMed] [Google Scholar]
- Garity J. Stress, learning style, resilience factors, and ways of coping in Alzheimer family caregivers. American Journal of Alzheimer’s Disease. 1997;12:171–178. [Google Scholar]
- Gilliam CM, Steffen AM. The relationship between caregiving self-efficacy and depressive symptoms in dementia family caregivers. Aging & Mental Health. 2006;10:79–86. doi: 10.1080/13607860500310658. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Li LW, Seltzer MM, Greenberg JS. Change in depressive symptoms among daughter caregivers: an 18-month longitudinal study. Psychology and Aging. 1999;14:206–219. doi: 10.1037//0882-7974.14.2.206. [DOI] [PubMed] [Google Scholar]
- Mahoney R, Regan C, Katona C, Livingston G. Anxiety and Depression in Family Caregivers of People With Alzheimer Disease: The LASER-AD Study. American Journal of Geriatric Psychiatry. 2005;13:795–801. doi: 10.1176/appi.ajgp.13.9.795. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Aschbacher K, Patterson TL, Ancoli-Israel S, von Känel R, Mills PJ, et al. Avoidant Coping Mediates the Relationship Between Care Recipient Problem Behaviors and Depressive Symptoms in Spousal Alzheimer’s Caregivers. American Journal of Geriatric Psychiatry. 2006;14:299–306. doi: 10.1097/01.JGP.0000192492.88920.08. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Aschbacher K, Patterson TL, Ancoli-Israel S, von Känel R, Mills PJ, et al. Avoidant Coping Partially Mediates the Relationship Between Patient Problem Behaviors and Depressive Symptoms in Spousal Alzheimer Caregivers. American Journal of Geriatric Psychiatry. 2006;14:299–306. doi: 10.1097/01.JGP.0000192492.88920.08. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Aschbacher K, Patterson TL, Ancoti-Israel S, von Känel R, Mills PJ, et al. Avoidant coping partially mediates the relationship between patient problem behaviors and depressive symptoms in spousal Alzheimer caregivers. American Journal of Geriatric Psychiatry. 2006;14:299–306. doi: 10.1097/01.JGP.0000192492.88920.08. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Patterson TL, Grant I. Is depression in Alzheimer’s caregivers really due to activity restriction? A preliminary mediational test of the activity restriction. Journal of Behavior Therapy and Experimental Psychiatry. 2008;39:459–466. doi: 10.1016/j.jbtep.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- Ory MG, Hoffman RR, 3rd, Yee JL, Tennstedt S, Schulz R. Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. The Gerontologist. 1999;39:177–185. doi: 10.1093/geront/39.2.177. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: a meta-analytic review. Journal of Behavioral Medicine. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- Powers DV, Gallagher-Thompson D, Kraemer HC. Coping and depression in Alzheimer’s caregivers: longitudinal evidence of stability. The journals of gerontology Series B, Psychological sciences and social sciences. 2002;57:P205–211. doi: 10.1093/geronb/57.3.p205. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. New England Journal of Medicine. 2009;360:225–235. doi: 10.1056/NEJMoa0806994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray WA, Meredith S, Thapa PB, Meador KG, Hall K, Murray KT. Antipsychotics and the risk of sudden cardiac death. Archives of General Psychiatry. 2001;58:1161–1167. doi: 10.1001/archpsyc.58.12.1161. [DOI] [PubMed] [Google Scholar]
- Romero-Moreno R, Losada A, Mausbach BT, Marquez-Gonzalez M, Patterson TL, Lopez J. Analysis of the moderating effect of self-efficacy domains in different points of the dementia caregiving process. Aging & Mental Health. 2011;15:221–231. doi: 10.1080/13607863.2010.505231. [DOI] [PubMed] [Google Scholar]
- Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934–1943. doi: 10.1001/jama.294.15.1934. [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. American Journal of Nursing. 2008;108:23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, Given CW, Schiffman RF, Murman DL, Von Eye A, et al. The influence of caregiver mastery on depressive symptoms. Journal of Nursing Scholarship. 2007;39:249–255. doi: 10.1111/j.1547-5069.2007.00176.x. [DOI] [PubMed] [Google Scholar]
- Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The Revised Scale for Caregiving Self-Efficacy: Reliability and validity studies. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2002;57B:P74–P86. doi: 10.1093/geronb/57.1.p74. [DOI] [PubMed] [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: the revised memory and behavior problems checklist. Psychology and aging. 1992;7:622–631. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- Vitaliano P, Russo J, Carr JE. The Ways of Coping Checklist: Revision and psychometric properties. Multivariate Behavior Research. 1985;20:3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- Williams J, MacKinnon DP. Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling. 2008;15:23–51. doi: 10.1080/10705510701758166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson GM. Extending the activity restriction model of depressed affect: Evidence from a sample of breast cancer patients. Health Psychology. 2000;19:339–347. [PubMed] [Google Scholar]
- Williamson GM. Extending the activity restriction model of depressed affect: Evidence from a sample of breast cancer patients. Health Psychology. 2000;19:339–347. [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Pain, activity restriction, and symptoms of depression among community-residing elderly adults. Journal of Gerontology. 1992;47:P367–372. doi: 10.1093/geronj/47.6.p367. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Physical illness and symptoms of depression among elderly outpatients. Psychology and Aging. 1992;7:343–351. doi: 10.1037//0882-7974.7.3.343. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Coping with specific stressors in Alzheimer’s disease caregiving. The Gerontologist. 1993;33:747–755. doi: 10.1093/geront/33.6.747. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Activity restriction mediates the association between pain and depressed affect: A study of younger and older adult cancer patients. Psychology and Aging. 1995;10:369–378. doi: 10.1037//0882-7974.10.3.369. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR. Physical illness and depression in older adults: A handbook of theory, research, and practice. Dordrecht, Netherlands: Kluwer Academic Publishers; 2000. The Activity Restriction Model of Depressed Affect: Antecedents and consequences of restricted normal activities; pp. 173–200. [Google Scholar]
- Wright SD, Lund DA, Caserta MS, Pratt C. Coping and caregiver well-being: The impact of maladaptive strategies. Journal of Gerontological Social Work. 1991;17:75–91. [Google Scholar]
- Yates ME, Tennstedt S, Chang BH. Contributors to and mediators of psychological well-being for informal caregivers. Journal of Gerontology, Psychological Science. 1999;54:P12–22. doi: 10.1093/geronb/54b.1.p12. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MA, Townsend A, Greene R. Stress reduction for family caregivers: Effects of adult day care use. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 1998;53:S267–277. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]
- Zeiss A, Gallagher-Thompson D, Lovett S, Rose J, McKibbin C. Self-efficacy as a mediator of caregiver coping: Development and testing of an assessment model. Journal of Clinical Geropsychology. 1999;5:221–230. [Google Scholar]