Abstract
Objective
To evaluate the association of MRI-based knee cartilage T2 measurements and focal knee lesions with knee pain in knees without radiographic osteoarthritis (OA) among subjects with OA risk factors.
Methods
We studied the right knees of 126 subjects from the Osteoarthritis Initiative database. We randomly selected 42 subjects aged 45–55 years with OA risk factors, right knee pain (WOMAC pain score ≥5), no left knee pain (WOMAC pain score =0) and no radiographic OA (KL-score ≤1) in the right knee. We also selected two comparison groups: 42 subjects without knee pain in either knee and 42 with bilateral knee pain. Both groups were frequency matched to subjects with right knee only pain by gender, age, BMI and KL-score. All subjects underwent 3T MRI of the right knee. Focal knee lesions were assessed and cartilage T2 measurements were performed.
Results
Prevalence of meniscal, bone marrow and ligamentous lesions and joint effusion were not significantly different between the groups (p>0.05), while cartilage lesions were more frequent in subjects with right only knee pain compared to subjects without knee pain (p<0.05). T2 values averaged over all compartments were similar in subjects with right only knee pain (34.4±1.8ms) and with bilateral knee pain (34.7±4.7ms), but significantly higher compared to subjects without knee pain (32.4±1.8ms) (p<0.05).
Conclusion
These results suggest that elevated cartilage T2 values are associated with findings of pain in the early phase of OA, while among morphological knee abnormalities only knee cartilage lesions are significantly associated with knee pain status.
Keywords: Osteoarthritis, WOMAC, MRI, T2 relaxation time, WORMS
Introduction
Osteoarthritis (OA) affects nearly 27 million people in the United States [1]. The most commonly affected joint is the knee and the predominant clinical symptom in most OA patients is pain [2]. The Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index is a reliable and frequently used tool to evaluate clinical symptoms of knee OA including presence and grade of pain during different activities [3;4]. OA is characterized by the progressive loss of hyaline articular cartilage, which can be evaluated by using magnetic resonance imaging (MRI) [5;6]. Previous studies reported an inverse relationship between MRI-based cartilage volume measurements and knee pain assessed by using the WOMAC pain score [7;8]. Furthermore knee pain appears to be associated with prevalent bone marrow edema pattern, synovitis, joint effusion, meniscal tears and denuded subchondral bone [9–14]. While most of these studies were performed in subjects with radiographic evidence of OA, little is known about these associations in subjects in the early phase of OA, who have knee pain, but no radiographic evidence of OA. Such individuals are of particular interest, since they may most benefit from treatment or behavioural interventions.
The early phase of OA is characterized by biochemical changes of the cartilage including proteoglycan loss, increased water content and deterioration of the collagen network [15]. These changes can be non-invasively detected by quantitative MRI measurements such as T2 relaxation time mapping [16;17]. Therefore it could be interesting to analyze the association of knee pain not only with focal knee lesions such as cartilage and meniscal abnormalities, but also with knee cartilage T2 measurements in subjects in the early phase of knee OA.
The NIH launched the Osteoarthritis Initiative (OAI), a longitudinal, observational multi-center study with 4,796 participants, to better understand the natural evolution of OA (http://www.oai.ucsf.edu/). The OAI database contains radiographs and MR images as well as clinical data including the WOMAC pain score [18]. The OAI progression cohort consists of subjects with radiographic tibiofemoral knee OA (defined as a definite tibiofemoral osteophyte) and frequent knee symptoms (“pain, aching, or stiffness in or around the knee” on most days for at least one month in the past 12 months) at baseline. Subjects in the OAI incidence cohort did not fulfil these criteria at baseline, but had OA risk factors such as overweight or obesity, history of knee injury, history of knee surgery and knee symptoms (“pain, aching, or stiffness in or around the knee” in the past 12 months for at least one month but not on most days).
The purpose of this study was to analyze whether MRI-based knee cartilage T2 measurements as well as prevalence of focal knee lesions in subjects from the OAI incidence cohort (no radiographic or clinical evidence of OA) are associated with knee pain as quantified with the WOMAC pain score.
Materials and Methods
Subjects
Data used in the preparation of this article were obtained from the Osteoarthritis Initiative (OAI) database, which is available for public access at http://www.oai.ucsf.edu/. Specific OAI datasets used were baseline clinical dataset 0.2.2 and baseline imaging datasets 0.E.1 and 0.C.2.
We selected 126 subjects from the OAI incidence cohort for this study. Subjects from the OAI incidence cohort did not have symptomatic knee OA, defined as frequent symptoms and radiographic OA in the same knee, in either knee at baseline, but had at least one of the following OA risk factors at baseline: knee symptoms (“pain, aching, or stiffness in or around the knee” in the past 12 months for at least one month but not on most days), overweight or obesity, history of knee injury, history of knee surgery, family history of total knee replacement or Heberden nodes.
Forty-two subjects (21 males, 21 females) aged 45–55 years with right knee pain (Western Ontario and McMaster University (WOMAC) pain score ≥5), no left knee pain (WOMAC pain score of zero) and Kellgren-Lawrence (KL)-score ≤1 (i.e. no osteophytes or minimal osteophytes, and a joint space narrowing score of zero) in the right knee were randomly selected from the OAI incidence cohort. The sample was designed to have an equal number of men and women and an equal number of KL = 0 and KL = 1 knees. The age range of 45–55 years was used to focus on younger subjects who may most benefit from treatment or behavioural interventions. A WOMAC threshold of 5 was used based on a previous study, which used WOMAC pain scores to study eligibility for individuals to be included in an OA knee trial [19]. There was no specific inclusion criteria based on body mass index (BMI).
In addition, gender-, age-, BMI- and KL-frequency matched control groups were identified: 42 subjects without knee pain (WOMAC pain score of zero in either knee) and 42 subjects with bilateral knee pain (WOMAC pain score ≥5 in both knees) from the OAI incidence cohort were also included in this study.
All subjects included in this study provided informed consent. The study protocol, amendments and informed consent documentation were reviewed and approved by the local institutional review boards.
WOMAC Questionnaire
The Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index is a well-established tool to evaluate clinical symptoms of OA in the knee, including pain, stiffness, and physical function over the last seven days [3;4]. All subjects completed the WOMAC questionnaire for the right and left knee on the day knee radiographs and MR images were acquired. They were asked five activity questions and had to provide a pain score for each activity (0 = none; 1 = mild; 2 = moderate; 3 = severe; 4 = extreme pain). Using this grading system, summed scores ranged from 0 to 20 for each knee. The recruited subjects with WOMAC pain scores ≥5 had at least one activity, where they had moderate amounts of pain. Based on the WOMAC pain scores of both knees, subjects were stratified into three groups with (a) no knee pain, (b) right knee pain, and (c) bilateral knee pain.
Imaging
Bilateral standing posterior-anterior fixed flexion knee radiographs were acquired. Knees were positioned in a plexiglas frame (SynaFlexer, CCBR-Synarc, San Francisco, CA, USA) with 20°–30° flexion and 10° internal rotation of the feet. Right knee radiographs were graded by two radiologists (L.N. with 4 years of experience and W.V. with 7 years of experience) in consensus by using the Kellgren-Lawrence (KL) scoring system [20].
All subjects underwent 3T MRI (Trio, Siemens, Erlangen, Germany) of the right knee. The following five sequences were used in this study as described in the OAI MRI protocol [18]:
a sagittal three-dimensional dual-echo steady-state (DESS) sequence with water excitation and coronal and axial reformations (TE / TR = 4.7 / 16.3 ms, field of view (FOV) = 14 cm, slice thickness = 0.7 mm, in-plane spatial resolution = 0.365 × 0.456 mm2, flip angle = 25, bandwidth = 185 Hz / pixel),
a sagittal two-dimensional intermediate-weighted turbo spin echo (TSE) sequence with fat suppression (TE / TR = 30 / 3200 ms, field of view (FOV) = 16 cm, slice thickness = 3 mm, in-plane spatial resolution = 0.357 × 0.511 mm2, flip angle = 180, bandwidth = 248 Hz / pixel),
a coronal two-dimensional intermediate-weighted turbo spin-echo (TSE) sequence (TE / TR = 29 / 3850 ms, field of view (FOV) = 14 cm, slice thickness = 3 mm, in-plane spatial resolution = 0.365 × 0.456 mm2, flip angle = 180, bandwidth = 352 Hz / pixel),
a coronal three-dimensional T1-weighted fast low-angle shot (FLASH) sequence with water excitation (TE / TR = 7.57 / 20 ms, field of view (FOV) = 16 cm, slice thickness = 1.5 mm, in-plane spatial resolution = 0.313 × 0.313 mm2, flip angle = 12, bandwidth = 130 Hz / pixel), and
a sagittal two-dimensional multislice multiecho (MSME) spin echo sequence for T2 mapping (TR = 2700 ms, seven TEs = 10 ms, 20 ms, 30 ms, 40 ms, 50 ms, 60 ms, 70 ms, field of view (FOV) = 12 cm, slice thickness = 3 mm with 0.5mm gap, in-plane spatial resolution = 0.313 × 0.446 mm2, bandwidth = 250 Hz / pixel).
WORMS Grading
MR images of the right knee were transferred to picture archiving communication system (PACS) workstations (Agfa, Ridgefield Park, NJ, USA) and assessed for the presence and grade of meniscal, cartilage, and ligamentous lesions as well as bone marrow edema pattern (BMEP) and joint effusion using a modified whole organ MRI score (WORMS) as previously described [21–23]. Three radiologists (L.N. with 4 years, W.V. with 7 years and T.M.L. with 22 years of experience) analyzed 16 MRI studies in consensus to calibrate thresholds for grading abnormalities. The remaining 110 MRI studies were read by two radiologists (L.N. and W.V.) independently. In case of disagreement, consensus reading was performed with the third, most experienced radiologist (T.M.L.). The radiologists were blinded to the WOMAC pain scores of the subjects.
Meniscal lesions were graded separately in 6 regions (medial/lateral and anterior/body/posterior) using the following 4-point scale: 0 = normal; 1 = intra-substance abnormal signal; 2 = non-displaced tear; 3 = displaced or complex tear; 4 = complete destruction/maceration. Compared to the original WORMS system, grade 1 was added to better reflect presence of early degenerative meniscal disease.
ACL (anterior cruciate ligament), PCL (posterior cruciate ligament), MCL (medial collateral ligament), LCL (lateral collateral ligament), patellar tendon and popliteal tendon were evaluated using a 4-point scale (0 = no lesion; 1 = signal changes around the ligament; 2 = partial tear; 3 = complete tear).
Joint effusion was graded using a 4-point scale (0 = normal; 1 = <33% of maximum potential distention; 2 = 33–66% of maximum potential distention; 3 = >66% of maximum potential distention).
Cartilage lesions and BMEP were not assessed by using the original 15 regions, but six condensed regions (patella, trochlea, medial/lateral femur and medial/lateral tibia).
BMEP were defined as poorly marginated areas of increased T2 signal intensity and graded using a four-point scale: 0 = none; 1= diameter of <5mm; 2= diameter of 5−20mm; 3 = diameter of >20mm.
Cartilage lesions were graded using an 8-point scale: 0 = normal thickness and signal intensity; 1 = normal thickness or swelling with abnormal signal on fluid sensitive sequences; 2 = partial-thickness focal defect <1 cm in greatest width; 2.5 = full-thickness focal defect <1 cm in greatest width; 3 = multiple areas of partial thickness (grade 2) defects intermixed with areas of normal thickness, or a grade 2 defect wider than 1 cm but <75% of the region; 4 = diffuse (>75% of the region) partial-thickness loss; 5 = multiple areas of full-thickness loss (grade 2.5) or a grade 2.5 lesion wider than 1 cm but <75% of the region; 6 = diffuse (>75% of the region) full-thickness loss. Condensing the anatomical regions from 15 to 6 would have potentially affected the frequency of grade 4 and 6 lesions. However, grade 4 lesions are very rare and usually if there is >75% partial thickness cartilage loss, full thickness lesions are present and grade 6 lesions are not expected in this cohort with KL-scores ≤1.
Similar to previous studies [21–23], a WORMS maximum score (WORMS Max) was assigned to each knee by the greatest WORMS score in any compartment. WORMS Max >0 in any joint structure was taken as an indication of a lesion. A meniscal WORMS Max >1 indicated a non-displaced tear or worse, while a cartilage WORMS Max >1 identified subjects with at least one partial thickness defect. Cartilage WORMS Max >1 was also used to exclude lesions characterized only by signal abnormalities, i.e. grade 1 lesions.
T2 Measurements
The MSME spin echo sequences were transferred to a SUN workstation (Sun Microsystems, Mountain View, CA, USA). Studies have suggested that excluding the first echo from a multiecho Carr-Purcell-Meiboom-Gill sequence minimizes error from stimulated echoes in calculated T2 values for cartilage [24;25]. Raya et al. showed that a fit to a noise-corrected exponential improves the accuracy and precision of cartilage T2 measurements [26]. Therefore T2 maps were calculated with custom-built software on a pixel-by-pixel basis skipping the first echo and using a noise-corrected exponential fitting as previously described [27]. Five distinct compartments (patella, medial/lateral femur and medial/lateral tibia) were segmented using in-house software based on IDL (Interactive Data Language, Research Systems, Boulder, CO, USA) directly in the T2 maps. In order to exclude both fluid and chemical shift artifacts from the region of interest, a technique was used that allowed adjustment of the region of interest simultaneously in the T2 map and first echo of the multiecho sequence by opening separate image panels at the same time with synchronized cursor, slice number and zoom. This segmentation procedure has been applied in previous studies [21;23;27]. T2 maps were segmented by one operator (A.A.) and supervised by a radiologist (T.B.). Mean T2 values for each compartment were calculated after completed segmentation. Segmentation of the trochlea compartment was not performed due to flow artifacts from the popliteal artery.
Statistical Analysis
The statistical analyses were performed with SPSS (SPSS Inc., Chicago, IL, USA) using a two-sided 0.05 level of significance. Pearson χ2 test and t-test were used to compare frequencies of OA risk factors and WOMAC pain score between subjects with no knee pain and right knee pain, respectively subjects with right knee pain and bilateral knee pain. Multivariate linear and logistic regression models were used to compare T2 measurements as well as the prevalence of focal knee lesions between subjects with no knee pain and right knee pain, respectively subjects with right knee pain and bilateral knee pain, adjusting for gender, age, KL-score, BMI and other OA risk factors. In addition, odds ratios with 95% confidence intervals were calculated for the association between subject groups and prevalence of cartilage lesions.
Reproducibility
To assess intra- and inter-reader reproducibility of the WORMS grading, 13 subjects were randomly selected and WORMS grading was performed two times by two readers (L.N. and W.V.) independently. Intra-class correlation coefficients (ICC) were calculated to compare the exact WORMS score for meniscal and cartilage lesions and BMEP in each compartment [28]. Reproducibility for ligamentous lesions and joint effusion was not performed due to their low prevalence in the study population.
The intra-reader (inter-reader) reproducibility of the two radiologists for meniscal WORMS grading was 0.93 and 0.94 (0.94), for cartilage WORMS grading 0.92 and 0.93 (0.92) and for BMEP WORMS grading 0.98 and 0.99 (0.98).
The intra-reader reproducibility for T2 measurements was determined in 13 randomly selected subjects in each cartilage compartment. T2 maps of each subject were segmented three times by one operator (A.A.). Reproducibility errors for each compartment were calculated in absolute numbers as root mean square average of the errors for each knee and on percentage basis as the root mean square average of the single coefficients of variation per knee, according to Gluer et al.[29].
Intra-reader reproducibility for T2 measurements of the compartments ranged from 0.82% to 3.43% (mean: 1.76%), respectively 0.30ms to 0.98ms (mean: 0.56ms). Highest reproducibility errors were observed in the patella, lowest reproducibility errors in the medial femur.
Results
Subject Characteristics
Mean ± standard deviation of age, BMI and WOMAC pain scores as well as frequencies of gender, KL-score and OA risk factors are listed in Table 1. The WOMAC pain score of the right knee was significantly different between subjects with right and bilateral knee pain (7.0±2.0 vs. 8.4±2.4; p=0.008). Differences in WOMAC pain scores of the right and left knee in subjects with bilateral knee pain were not significant (p=0.120; Table 1). The OA risk factor “knee symptoms in the past 12 months” was prevalent in 85.7% of the subjects without knee pain, although these subjects had a WOMAC pain score of zero in either knee. That is explained by the definition of the WOMAC pain score focusing on the previous seven days. All subjects with right and bilateral knee pain had knee symptoms in the past 12 months (Table 1).
Table 1.
Characteristics of subjects without knee pain (A), with right knee pain (B) and with bilateral knee pain (C). Frequencies of gender, KL-score and OA risk factors are listed in absolute numbers and on percentage basis. Age, BMI and WOMAC pain scores are displayed as mean ± standard deviation.
| A: Subjects without knee pain (n=42) |
B: Subjects with right knee pain (n=42) |
C: Subjects with bilateral knee pain (n=42) |
|
|---|---|---|---|
| male | 21 (50.0%) | 21 (50.0%) | 21 (50.0%) |
| KL-score = 0 | 21 (50.0%) | 21 (50.0%) | 21 (50.0%) |
| KL-score = 1 | 21 (50.0%) | 21 (50.0%) | 21 (50.0%) |
| knee symptoms in the past 12 months | 36 (85.7%)* | 42 (100.0%)* | 42 (100.0%) |
| history of knee injury | 24 (57.1%) | 24 (57.1%) | 20 (47.6%) |
| history of knee surgery | 7 (16.7%) | 12 (28.6%) | 10 (23.8%) |
| family history of knee replacement surgery | 6 (14.3%) | 12 (28.6%)~ | 3 (7.1%)~ |
| Heberden nodes | 9 (21.4%) | 6 (14.3%) | 7 (16.7%) |
| age [years] | 50.4±2.7 | 50.0±3.0 | 50.6±2.9 |
| BMI [kg/m2] | 28.3±3.6 | 28.3±4.6 | 27.6±4.4 |
| WOMAC pain score right knee | 0.0±0.0* | 7.0±2.0*,~ | 8.4±2.4~ |
| WOMAC pain score left knee | 0.0±0.0 | 0.0±0.0~ | 7.7±2.6~ |
statistically significant differences (p<0.05) between group A and B.
statistically significant differences (p<0.05) between group B and C.
Focal Knee Lesions
A significantly higher prevalence of meniscal lesions (WORMS >0) in the medial posterior horn was observed in all three subject groups, compared to the five other compartments (p<0.05; Table 2). Seven subjects without knee pain (16.7%), 9 subjects with right knee pain (21.4%), and 3 subjects with bilateral knee pain (7.1%) had a meniscal tear in the medial posterior horn (WORMS >1). Differences between the groups were not statistically significant (p>0.05). The prevalence of meniscal lesions (WORMS Max >0) was not significantly different between subject groups (p>0.05; Table 3). Similarly, subject groups showed no significant difference in the prevalence of meniscal tears (WORMS Max >1) as shown in Table 3 (p>0.05).
Table 2.
Prevalence of meniscal, cartilage and ligamentous lesions (WORMS >0) in the right knee of subjects without knee pain (A), with right knee pain (B), and with bilateral knee pain (C) in absolute numbers and on percentage basis for each compartment.
| A: Subjects without knee pain (n=42) |
B: Subjects with right knee pain (n=42) |
C: Subjects with bilateral knee pain (n=42) |
||
|---|---|---|---|---|
| Meniscus: | ||||
| Medial Anterior WORMS >0 | 1 (2.4%) | 0 (0.0%) | 1 (2.4%) | |
| Medial Body WORMS >0 | 9 (21.4%) | 8 (19.0%) | 4 (9.5%) | |
| Medial Posterior WORMS >0 | 24 (57.1%) | 25 (59.5%) | 12 (28.6%) | |
| Lateral Anterior WORMS >0 | 2 (4.8%) | 4 (9.5%) | 1 (2.4%) | |
| Lateral Body WORMS >0 | 5 (11.9%) | 5 (11.9%) | 5 (11.9%) | |
| Lateral Posterior WORMS >0 | 8 (19.0%) | 7 (16.7%) | 5 (11.9%) | |
| Cartilage: | ||||
| Patella WORMS >0 | 23 (54.8%) | 26 (61.9%) | 29 (69.0%) | |
| Trochlea WORMS >0 | 17 (40.5%) | 20 (47.6%) | 19 (45.2%) | |
| Medial Femur WORMS >0 | 7 (16.7%) | 20 (47.6%) | 7 (16.7%) | |
| Lateral Femur WORMS >0 | 5 (11.9%) | 5 (11.9%) | 5 (11.9%) | |
| Medial Tibia WORMS >0 | 3 (7.1%) | 3 (7.1%) | 3 (7.1%) | |
| Lateral Tibia WORMS >0 | 19 (45.2%) | 18 (42.9%) | 17 (40.5%) | |
| Ligaments: | ||||
| ACL WORMS>0 | 2 (4.8%) | 3 (7.1%) | 2 (4.8%) | |
| PCL WORMS>0 | 0 (0.0%) | 1 (2.4%) | 0 (0.0%) | |
| MCL WORMS>0 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| LCL WORMS>0 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Patella Tendon WORMS>0 | 0 (0.0%) | 2 (4.8%) | 1 (2.4%) | |
| Popliteal Tendon WORMS>0 | 0 (0.0%) | 2 (4.8%) | 0. (0.0%) | |
Table 3.
Prevalence of focal knee lesions of subjects without knee pain (A), with right knee pain (B) and with bilateral knee pain (C). WORMS Max >0 in any joint structure indicate a lesion. WORMS Max >1 specifies prevalence of meniscal tear (respectively of grade 2 or higher cartilage lesion).
| A: Subjects without knee pain (n=42) |
B: Subjects with right knee pain (n=42) |
C: Subjects with bilateral knee pain (n=42) |
A vs. B p- value* |
B vs. C p- value* |
|
|---|---|---|---|---|---|
| Meniscus: | |||||
| WORMS Max >0 | 28 (66.7%) | 28 (66.7%) | 20 (47.6%) | 0.771 | 0.101 |
| WORMS Max >1 | 14 (33.3%) | 15 (35.7%) | 9 (21.4%) | 0.910 | 0.272 |
| Cartilage: | |||||
| WORMS Max >0 | 32 (76.2%) | 36 (85.7%) | 37 (88.1%) | 0.193 | 0.513 |
| WORMS Max >1 | 20 (47.6%) | 28 (66.7%) | 26 (61.9%) | 0.016 | 0.379 |
| Ligaments: | |||||
| WORMS Max >0 | 2 (4.8%) | 6 (14.3%) | 3 (7.1%) | 0.080 | 0.526 |
| Bone Marrow Edema Pattern: | |||||
| WORMS Max >0 | 17 (40.5%) | 16 (38.1%) | 14 (33.3%) | 0.959 | 0.388 |
| Joint Effusion: | |||||
| WORMS Max >0 | 0 (0.0%) | 3 (7.1%) | 4 (9.5%) | 0.997 | 0.502 |
Adjusted for gender, age, KL-score, BMI and other OA risk factors.
P-values indicating statistical significance (p<0.05) are printed in bold.
Cartilage lesions (WORMS >0) were most frequent in the patella and trochlea compartment in all three subject groups (Table 2). A higher prevalence of cartilage lesions (WORMS Max >0) was observed in subjects with right (85.7%) and bilateral knee pain (88.1%), compared to subjects without knee pain (76.2%; Table 3). However, differences were not statistically significant between subjects with no knee pain and right knee pain, respectively subjects with right knee pain and bilateral knee pain (p>0.05; Table 3). Prevalence of grade 2 or higher cartilage lesions (WORMS Max >1) were significantly higher in subjects with right knee pain, compared to subjects without knee pain (p=0.016; Table 3). An odds ratio (95% confidence interval) of 3.52 (1.26–9.80) was calculated for the association between subjects with right knee pain / subjects without knee pain and prevalence of WORMS Max>1 cartilage lesions. There were no differences between subjects with right and bilateral knee pain (p>0.05; Table 3).
Ligamentous lesions were prevalent in 4.8%, 14.3% and 7.1% of the subjects with no, right, and bilateral knee pain, respectively (p>0.05; Table 2 and 3). Prevalence of BMEP and joint effusion were not significantly different between the subject groups as shown in Table 3 (p>0.05).
T2 Measurements
There were no significant differences of cartilage T2 measurements between subjects with right compared to those with bilateral knee pain in any compartment (p>0.05; Table 4). However, subjects with right knee pain showed significantly elevated T2 values in the medial femur, medial tibia and lateral tibia compartments compared to the subjects without knee pain (p<0.05; Table 4). Averaged over all five compartments, T2 values were similar in subjects with right knee pain (34.4±1.8ms) and with bilateral knee pain (34.7±4.7ms), but significantly higher compared to subjects without knee pain (32.4±1.8ms) (p<0.05; Table 4).
Table 4.
Mean T2 values (mean±SD) of the five segmented compartments and averaged over the five compartments in subjects without knee pain (A), with right knee pain (B) and with bilateral knee pain (C).
| A: Subjects without knee pain (n=42) |
B: Subjects with right knee pain (n=42) |
C: Subjects with bilateral knee pain (n=42) |
A vs. B p- value* |
B vs. C p- value* |
|
|---|---|---|---|---|---|
| Patella mean T2 [ms] | 31.4±2.3 | 30.7±1.9 | 31.3±4.9 | 0.138 | 0.495 |
| Medial Femur mean T2 [ms] | 35.9±2.5 | 38.3±2.5 | 38.2±5.0 | <0.001 | 0.880 |
| Medial Tibia mean T2 [ms] | 31.3±2.5 | 34.4±2.6 | 34.5±5.6 | <0.001 | 0.919 |
| Lateral Femur mean T2 [ms] | 33.2±2.4 | 34.2±2.2 | 34.8±4.6 | 0.080 | 0.589 |
| Lateral Tibia mean T2 [ms] | 30.4±2.8 | 34.2±2.8 | 34.5±5.0 | <0.001 | 0.927 |
| mean T2 averaged over all five compartments [ms] | 32.4±1.8 | 34.4±1.8 | 34.7±4.7 | <0.001 | 0.770 |
Adjusted for gender, age, KL-score, BMI and other OA risk factors.
P-values indicating statistical significance (p<0.05) are printed in bold.
Independent of group, subjects with a meniscal tear in the medial posterior horn (WORMS >1) showed no significantly elevated cartilage T2 values in any compartment, compared to subjects with medial posterior horn WORMS scores of 0 or 1 (p>0.05).
Discussion
This study demonstrated that cartilage T2 values in subjects without radiographic OA, but with OA risk factors were significantly elevated in those with knee pain, compared to those without knee pain. The prevalence of cartilage lesions were related with knee pain. However, other focal knee lesions such as meniscal abnormalities and BMEP were not associated with knee pain in this study population.
The pathogenesis of OA related knee pain is clinically relevant and therefore an important research topic. Subchondral bone and synovium may be responsible for nociceptive stimuli in OA and not the cartilage itself, since it does not contain nerve fibers and therefore cannot directly generate pain [30]. These facts suggest that cartilage lesions are not a major determinant of knee pain. However, the results of the present study demonstrated a relationship between cartilage lesions and knee pain. Increased prevalence of cartilage lesions in subjects with knee pain were observed compared to subjects without knee pain. These results are consistent with previous studies, which reported an association of cartilage loss with knee pain [7;8]. One likely possibility for the association of cartilage lesions with pain is that the biomechanical load is altered by the cartilage lesions, placing greater deforming stress upon the underlying subchondral bone [2;30].
BMEP and joint effusion could be responsible for knee pain. However, we observed a low prevalence of joint effusion, thus limiting the statistical analysis. We found that the prevalence of BMEP in subjects with and without knee pain in this study was no significantly different. In contrast to these findings, previous studies reported associations of knee pain with BMEP and joint effusion [9;11;13]. While these studies included subjects with symptomatic and radiographic OA, we focused on subjects, who had knee pain, but no radiographic OA. The varied subject selection between the studies may explain why no associations of pain with BMEP and joint effusion were found in our study.
A degenerative meniscal tear suggests early stage knee OA and a recent study reported elevated articular cartilage T2 values in subjects with prevalent meniscal tears of the medial posterior horn [31;32]. Interestingly, we observed no association between the prevalence of meniscal tears of the medial posterior horn and cartilage T2 values. Furthermore meniscal and ligamentous lesions were not associated with pain in this study population, which is consistent with previous studies [9;14]. Therefore cartilage seems to be the most appropriate joint structure reflecting a morphological correlate of knee pain prevalence in subjects in the early phase of OA.
In addition to higher prevalence of cartilage lesions, significantly elevated cartilage T2 values were found in subjects with knee pain, compared to subjects without knee pain. Since increased T2 relaxation times are based on biochemical changes of the cartilage such as proteoglycan loss and increased water content, these results suggest that deterioration of cartilage quality is associated with findings of pain in the early phase of OA. While previous studies reported a significant correlation between WOMAC pain sore and cartilage T2 measurements in subjects with radiographic OA [33;34], our study demonstrated that cartilage T2 measurements may also be a sensitive assessment tool for early cartilage degeneration and related knee pain as found in subjects with no radiographic OA, but OA risk factors. This finding is in particular important, since these subjects may most benefit from treatment or behavioural interventions. These results underline once more the potential of cartilage T2 measurements to detect early cartilage degeneration in subjects with OA risk factors [21;23;35].
This study had several limitations. Firstly, subjects were included in this study based on their self-reported, subjective pain perception. We used the WOMAC pain score, which is a reliable tool to evaluate OA related knee pain [3;4]. However, the WOMAC questionnaire focuses on the last seven days and is not a long-term evaluation tool, which may be a limitation of this study. Since the WOMAC questionnaire is well-established and has been used in previous studies with similar purposes [7–10;12;13], we based our inclusion criteria regarding knee pain on this questionnaire. Secondly, malalignment is a known OA risk factor [36;37]. We did not adjust for malalignment in the statistical analysis, because the baseline data collected by the OAI only included goniometer alignment readings, which have been found to be inaccurate [38]. Thirdly, increased cartilage volume (cartilage softening) is observed in the diseased compartments in the early phase of knee OA [39]. We did not investigate whether higher T2 values are associated with increased cartilage volume (cartilage softening), since cartilage segmentation was directly performed in the T2 maps, which are not suited for cartilage volume measurements because of a slice thickness of 3mm and 0.5mm gap. An additional segmentation of the cartilage compartments in the DESS images is necessary to investigate possible associations of cartilage T2 and cartilage volume. This is very time-consuming and was beyond the scope of this study. Future studies have to shed light on this issue. Lastly, reproducibility of cartilage T2 measurements and WORMS grading is critical and may be also a limitation. However, we found acceptable reproducibility errors in this study and the OAI established quality assurance methods to achieve high quality of cartilage T2 measurements [40].
In conclusion, the prevalence of cartilage lesions as well as cartilage T2 measurements were related with knee pain in subjects without radiographic OA, but with OA risk factors using the WOMAC questionnaire. This study suggests that cartilage T2 measurements may be a quantitatively measurable biomarker for knee pain in the early phase of OA but larger scale studies are required to better assess the full significance of these findings.
Significance and Innovations.
Among morphological knee abnormalities only knee cartilage lesions are significantly associated with knee pain status in subjects without radiographic osteoarthritis (OA), but with OA risk factors.
Elevated cartilage T2 values are associated with findings of pain in the early phase of OA.
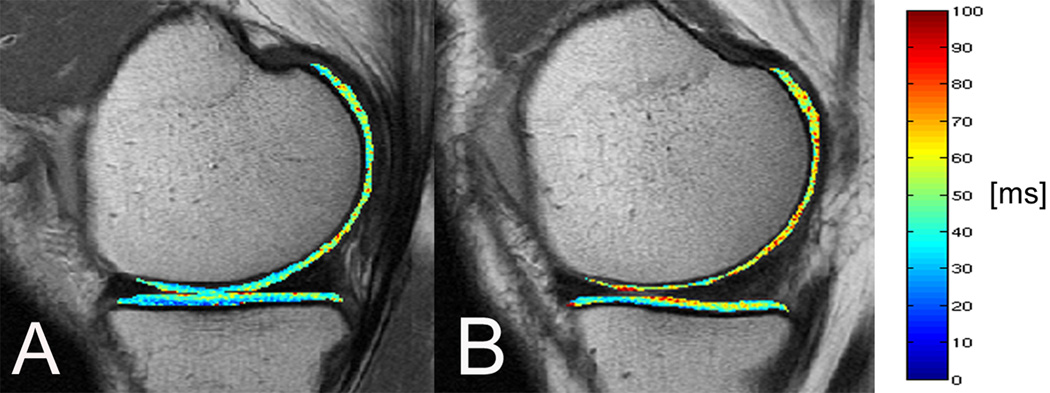
Figure 1.
T2 color maps of the medial femur and medial tibia compartments of the right knee overlaid with the first-echo images of the MSME sequence. (A) Representative subject without knee pain and (B) representative subject with right knee pain. Blue color indicates low, red color high cartilage T2 values. The subject with right knee pain showed elevated T2 values compared to the subject without knee pain (41.6ms in the medial femur, respectively 35.7ms in the medial tibia versus 35.3ms in the medial femur, respectively 33.9ms in the medial tibia).
Acknowledgement
Grant support: This study was supported by NIH U01AR059507-01 and NIH F32AR059478-01. The Osteoarthritis Initiative is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Pfizer, Inc.; Novartis Pharmaceuticals Corporation; Merck Research Laboratories; and GlaxoSmithKline. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health.
This manuscript has received the approval of the OAI Publications Committee based on a review of its scientific content and data interpretation.
Footnotes
Financial interests / Conflict of interest: The authors have no financial interests and no conflict of interest with regard to the work.
Reference List
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008;34(3):623–643. doi: 10.1016/j.rdc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 4.Bellamy N. The WOMAC Knee and Hip Osteoarthritis Indices: development, validation, globalization and influence on the development of the AUSCAN Hand Osteoarthritis Indices. Clin Exp Rheumatol. 2005;23(5 Suppl 39):S148–S153. [PubMed] [Google Scholar]
- 5.Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, Majumdar S. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226(2):373–381. doi: 10.1148/radiol.2262012190. [DOI] [PubMed] [Google Scholar]
- 6.Roemer FW, Eckstein F, Guermazi A. Magnetic resonance imaging-based semiquantitative and quantitative assessment in osteoarthritis. Rheum Dis Clin North Am. 2009;35(3):521–555. doi: 10.1016/j.rdc.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 7.Hunter DJ, March L, Sambrook PN. The association of cartilage volume with knee pain. Osteoarthritis Cartilage. 2003;11(10):725–729. doi: 10.1016/s1063-4584(03)00160-2. [DOI] [PubMed] [Google Scholar]
- 8.Wluka AE, Wolfe R, Stuckey S, Cicuttini FM. How does tibial cartilage volume relate to symptoms in subjects with knee osteoarthritis? Ann Rheum Dis. 2004;63(3):264–268. doi: 10.1136/ard/2003.007666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torres L, Dunlop DD, Peterfy C, Guermazi A, Prasad P, Hayes KW, Song J, Cahue S, Chang A, Marshall M, Sharma L. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006;14(10):1033–1040. doi: 10.1016/j.joca.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Baker K, Grainger A, Niu J, Clancy M, Guermazi A, Crema M, Hughes L, Buckwalter J, Wooley A, Nevitt M, Felson DT. Relation of synovitis to knee pain using contrast-enhanced MRIs. Ann Rheum Dis. 2010;69(10):1779–1783. doi: 10.1136/ard.2009.121426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hill CL, Gale DG, Chaisson CE, Skinner K, Kazis L, Gale ME, Felson DT. Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis. J Rheumatol. 2001;28(6):1330–1337. [PubMed] [Google Scholar]
- 12.Moisio K, Eckstein F, Chmiel JS, Guermazi A, Prasad P, Almagor O, Song J, Dunlop D, Hudelmaier M, Kothari A, Sharma L. Denuded subchondral bone and knee pain in persons with knee osteoarthritis. Arthritis Rheum. 2009;60(12):3703–3710. doi: 10.1002/art.25014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo GH, McAlindon TE, Niu J, Zhang Y, Beals C, Dabrowski C, Le Graverand MP, Hunter DJ. Bone marrow lesions and joint effusion are strongly and independently associated with weight-bearing pain in knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2009;17(12):1562–1569. doi: 10.1016/j.joca.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kornaat PR, Bloem JL, Ceulemans RY, Riyazi N, Rosendaal FR, Nelissen RG, Carter WO, Hellio Le Graverand MP, Kloppenburg M. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology. 2006;239(3):811–817. doi: 10.1148/radiol.2393050253. [DOI] [PubMed] [Google Scholar]
- 15.Blumenkrantz G, Majumdar S. Quantitative magnetic resonance imaging of articular cartilage in osteoarthritis. Eur Cell Mater. 2007;13:76–86. doi: 10.22203/ecm.v013a08. [DOI] [PubMed] [Google Scholar]
- 16.Burstein D, Gray M, Mosher T, Dardzinski B. Measures of molecular composition and structure in osteoarthritis. Radiol Clin North Am. 2009;47(4):675–686. doi: 10.1016/j.rcl.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Liess C, Lusse S, Karger N, Heller M, Gluer CC. Detection of changes in cartilage water content using MRI T2-mapping in vivo. Osteoarthritis Cartilage. 2002;10(12):907–913. doi: 10.1053/joca.2002.0847. [DOI] [PubMed] [Google Scholar]
- 18.Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage. 2008;16(12):1433–1441. doi: 10.1016/j.joca.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goggins J, Baker K, Felson D. What WOMAC pain score should make a patient eligible for a trial in knee osteoarthritis? J Rheumatol. 2005;32(3):540–542. [PubMed] [Google Scholar]
- 20.Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan J, Stehling C, Muller-Hocker C, Schwaiger BJ, Lynch J, McCulloch CE, Nevitt MC, Link TM. Vastus lateralis/vastus medialis cross-sectional area ratio impacts presence and degree of knee joint abnormalities and cartilage T2 determined with 3T. Osteoarthritis Cartilage. 2011;19(1):65–73. doi: 10.1016/j.joca.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stehling C, Lane NE, Nevitt MC, Lynch J, McCulloch CE, Link TM. Subjects with higher physical activity levels have more severe focal knee lesions diagnosed with 3T MRI: analysis of a non-symptomatic cohort of the osteoarthritis initiative. Osteoarthritis Cartilage. 2010;18(6):776–786. doi: 10.1016/j.joca.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stehling C, Liebl H, Krug R, Lane NE, Nevitt MC, Lynch J, McCulloch CE, Link TM. Patellar cartilage: T2 values and morphologic abnormalities at 3.0-T MR imaging in relation to physical activity in asymptomatic subjects from the osteoarthritis initiative. Radiology. 2010;254(2):509–520. doi: 10.1148/radiol.09090596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maier CF, Tan SG, Hariharan H, Potter HG. T2 quantitation of articular cartilage at 1.5 T. J Magn Reson Imaging. 2003;17(3):358–364. doi: 10.1002/jmri.10263. [DOI] [PubMed] [Google Scholar]
- 25.Smith HE, Mosher TJ, Dardzinski BJ, Collins BG, Collins CM, Yang QX, Schmithorst VJ, Smith MB. Spatial variation in cartilage T2 of the knee. J Magn Reson Imaging. 2001;14(1):50–55. doi: 10.1002/jmri.1150. [DOI] [PubMed] [Google Scholar]
- 26.Raya JG, Dietrich O, Horng A, Weber J, Reiser MF, Glaser C. T2 measurement in articular cartilage: impact of the fitting method on accuracy and precision at low SNR. Magn Reson Med. 2010;63(1):181–193. doi: 10.1002/mrm.22178. [DOI] [PubMed] [Google Scholar]
- 27.Stehling C, Baum T, Mueller-Hoecker C, Liebl H, Carballido-Gamio J, Joseph GB, Majumdar S, Link TM. A novel fast knee cartilage segmentation technique for T(2) measurements at MR imaging - data from the Osteoarthritis Initiative. Osteoarthritis and Cartilage. 2011;19(8):984–989. doi: 10.1016/j.joca.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 29.Gluer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK. Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int. 1995;5(4):262–270. doi: 10.1007/BF01774016. [DOI] [PubMed] [Google Scholar]
- 30.Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365(9463):965–973. doi: 10.1016/S0140-6736(05)71086-2. [DOI] [PubMed] [Google Scholar]
- 31.Englund M, Guermazi A, Lohmander SL. The Role of the Meniscus in Knee Osteoarthritis: a Cause or Consequence? Radiologic Clinics of North America. 2009;47(4) doi: 10.1016/j.rcl.2009.03.003. 703-+ [DOI] [PubMed] [Google Scholar]
- 32.Zarins ZA, Bolbos RI, Pialat JB, Link TM, Li X, Souza RB, Majumdar S. Cartilage and meniscus assessment using T1rho and T2 measurements in healthy subjects and patients with osteoarthritis. Osteoarthritis Cartilage. 2010 doi: 10.1016/j.joca.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bolbos RI, Zuo J, Banerjee S, Link TM, Ma CB, Li X, Majumdar S. Relationship between trabecular bone structure and articular cartilage morphology and relaxation times in early OA of the knee joint using parallel MRI at 3 T. Osteoarthritis Cartilage. 2008;16(10):1150–1159. doi: 10.1016/j.joca.2008.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232(2):592–598. doi: 10.1148/radiol.2322030976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hovis KK, Stehling C, Souza RB, Haughom BD, Baum T, Nevitt M, McCulloch C, Lynch JA, Link TM. Physical Activity Is Associated With Magnetic Resonance Imaging-Based Knee Cartilage T2 Measurements in Asymptomatic Subjects With and Those Without Osteoarthritis Risk Factors. Arthritis and Rheumatism. 2011;63(8):2248–2256. doi: 10.1002/art.30419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hunter DJ, Sharma L, Skaife T. Alignment and Osteoarthritis of the Knee. Journal of Bone and Joint Surgery-American Volume. 2009;91A:85–89. doi: 10.2106/JBJS.H.01409. [DOI] [PubMed] [Google Scholar]
- 37.Friedrich KM, Shepard T, Chang G, Wang L, Babb JS, Schweitzer M, Regatte R. Does joint alignment affect the T2 values of cartilage in patients with knee osteoarthritis? Eur Radiol. 2010;20(6):1532–1538. doi: 10.1007/s00330-009-1689-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis & Rheumatism-Arthritis Care & Research. 2006;55(2):306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- 39.Kleemann RU, Krocker D, Cedraro A, Tuischer J, Duda GN. Altered cartilage mechanics and histology in knee osteoarthritis: relation to clinical assessment (ICRS Grade) Osteoarthritis and Cartilage. 2005;13(11):958–963. doi: 10.1016/j.joca.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 40.Schneider E, NessAiver M, White D, Purdy D, Martin L, Fanella L, Davis D, Vignone M, Wu G, Gullapalli R. The osteoarthritis initiative (OAI) magnetic resonance imaging quality assurance methods and results. Osteoarthritis Cartilage. 2008;16(9):994–1004. doi: 10.1016/j.joca.2008.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]