Abstract
Objectives. We examined the associations of oral health literacy (OHL) with oral health status (OHS) and dental neglect (DN), and we explored whether self-efficacy mediated or modified these associations.
Methods. We used interview data collected from 1280 female clients of the Special Supplemental Nutrition Program for Women, Infants and Children from 2007 to 2009 as part of the Carolina Oral Health Literacy Project. We measured OHL with a validated word recognition test (REALD-30), and we measured OHS with the self-reported National Health and Nutrition Examination Survey item. Analyses used descriptive, bivariate, and multivariate methods.
Results. Less than one third of participants rated their OHS as very good or excellent. Higher OHL was associated with better OHS (for a 10-unit REALD increase: multivariate prevalence ratio = 1.29; 95% confidence interval = 1.08, 1.54). OHL was not correlated with DN, but self-efficacy showed a strong negative correlation with DN. Self-efficacy remained significantly associated with DN in a fully adjusted model that included OHL.
Conclusions. Increased OHL was associated with better OHS but not with DN. Self-efficacy was a strong correlate of DN and may mediate the effects of literacy on OHS.
According to the most recent National Assessment of Adult Literacy Survey, nearly half (43%) of adults in the United States are at risk for low literacy.1 Consumer health information is frequently written at or above the 10th-grade reading level, meaning that approximately 90 million adult Americans with low health literacy skills struggle to understand fundamental health information such as consent forms, instructions, and drug labels.2
“Health literacy” refers to the ability to perform basic reading and numerical tasks necessary to navigate the health care environment and act on health care information.3 Healthy People 2010 defines health literacy as
[t]he degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.4(pp11–15)
Individuals with low health literacy skills often have poorer health knowledge and health status, unhealthy behaviors, less utilization of preventive services, higher rates of hospitalizations, increased health care costs, and ultimately poorer health outcomes than do those with higher literacy levels.5–11 Health literacy has been shown to function as a mediator between socioeconomic factors, such as race and education, and health behaviors and health outcomes,12–14 partly explaining health disparities.15,16 Paasche-Orlow and Wolf proposed a conceptual model of causal pathways between health literacy and health outcomes in which the effect of literacy on health outcomes is mediated by patient-level and extrinsic factors grouped as (1) access to and utilization of health care, (2) provider–patient interaction, and (3) self-care.17 Although these pathways have yet to be validated, a recent report by Osborn et al.18 suggested that self-efficacy, which refers to a person's belief in their own competence, and self-care do indeed mediate the effect of health literacy on health status. Previous investigations had not found any association between health literacy and self-efficacy.19,20
The body of literature linking literacy to overall health continues to grow, but studies linking literacy to dental health are relatively new. Oral health literacy (OHL) has been defined as the degree to which individuals have the capacity to obtain, process, and understand basic oral health information and services needed to make appropriate health decisions and act on them.21
The network of proximal and distal factors affecting oral health is complex and is not understood completely. These factors include genetic and environmental factors,22 sociodemographics,23–25 and personality.26–28 Although OHL represents one's ability to understand and process relevant health information, other characteristics may modify one's resulting decisions or actions. In this context, recent attention has focused on the role of oral health behaviors29,30 because, unlike most other factors affecting oral health, behaviors are readily amenable to change.31 The construct of self-efficacy beliefs is considered to represent an important link between health knowledge, health behaviors, and health outcomes,32 and it correlates well with other personality characteristics related to health behaviors.33 Because self-efficacy is a significant determinant of health-related actions initiated or avoided by individuals, its consideration in the oral health context has been advocated.31,34
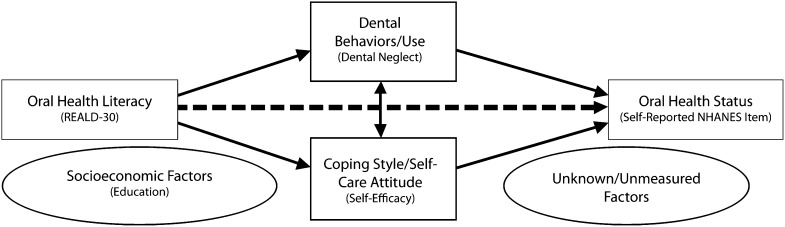
Although conceptual frameworks illustrating possible pathways linking health literacy to health outcomes or health status have been developed in medicine,12,14,17 little progress has been made in developing such pathways between OHL and oral health status (OHS). Macek et al.35 recently proposed a conceptual model linking word recognition and conceptual knowledge, decision-making, and communication skills with oral health outcomes. Although this model is not exhaustive, we theorize that OHL likely exerts effects on avoidance of care (i.e., dental neglect [DN]; Figure 1), which may or may not be mediated or modified by individual or systemic characteristics along the lines of the Paasche-Orlow and Wolf model.17
FIGURE 1—
Conceptual model of the association of self-reported OHS with OHL, self-efficacy, and dental neglect among female WIC participants (n = 1280): Carolina Oral Health Literacy study, North Carolina, 2007–2009.
Note. NHANES = National Health and Nutrition Examination Survey; OHL = oral health literacy; OHS = oral health status; REALD = Rapid Estimate of Adult Literacy in Dentistry; WIC = Supplemental Nutrition Program for Women, Infants and Children. Dashed arrow represents effects of OHL on OHS. Solid arrows represent pathways explored and hypothesized to mediate the effect of OHL on OHS. Education and other socioeconomic and unknown or unmeasured factors are also believed to confound or mediate this association (arrows omitted for parsimony).
To the best of our knowledge, no previous investigation has examined the links of OHL with OHS and DN, so we sought to establish these links. Because of the absence of any data linking self-efficacy with OHL, we also sought to examine this association and to empirically investigate the role of self-efficacy as a mediator or modifier36 of the association between OHL and DN and OHS, without conducting any comprehensive pathway analyses.
METHODS
The Carolina Oral Health Literacy (COHL) Project collected interview data from 1405 participants from 2007 to 2009.37 The main goal of the COHL was to examine OHL and its relationship to health behaviors and health outcomes among caregivers, infants, and children enrolled in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) in North Carolina. A prospective cohort study design was developed to determine OHL levels in a population attending WIC clinics that were selected because of the large number and diverse backgrounds of low-income clients attending those clinics. Nine sites in 7 counties were selected. For the present analysis, we excluded men (n = 49; 3.5% of total), Asians (n = 12; 0.9%), and those who did not have English as their primary language (n = 79; 5.6%).
Measures
The major explanatory variable was OHL, measured using a validated word recognition test called the Rapid Estimate of Adult Literacy in Dentistry (REALD-30).38 The REALD-30 scale score ranges from 0 (lowest literacy) to 30 (highest literacy). Our major outcome variables were DN and self-reported OHS.
We used a modified version of the previously validated Dental Neglect Scale (DNS) to evaluate DN.39–41 Participants were asked to report their agreement with 6 items describing their dental behaviors, with responses ranging from “definitely not” to “definitely yes” on a 4-point Likert scale. These items were: “I keep my dental care at home”; “I receive the dental care I should”; “I need dental care, but I put it off”; “I brush as well as I should”; “I control snacking between meals as well as I should”; and “I consider my dental health to be important.” We computed a cumulative score ranging from 6 (least DN) to 24 (most DN) and estimated Cronbach α as a measure of internal consistency and reliability. A recent investigation42 suggested that 2 factors may be distinguishable within the DNS (“dental neglect” and “avoidance of care”), so we conducted factor analysis (retaining eigenvalue > 1) to determine whether this was the case in our study sample.
We assessed OHS using the National Health and Nutrition Examination Survey item “How would you describe the condition of your mouth and teeth?” with possible responses of “excellent,” “very good,” “good,” “fair,” or “poor.” We evaluated self-efficacy as a potential effect mediator or modifier,43 and we measured it using the 10-item General Self-Efficacy Scale (GSES).44 Items in the GSES are related to one's ability to cope with general life demands (e.g., “I can always manage to solve difficult problems if I try hard enough” and “I can remain calm when facing difficulties because I can rely on my coping abilities”). The construct of self-efficacy refers to one's coping ability across a wide range of demanding situations,44 and the GSES has been shown to have good psychometric properties across diverse populations.45 The scale's scores range from 10 (lowest self-efficacy) to 40 (highest self-efficacy). We obtained Cronbach α for the GSES to determine its reliability in the context of our study.
We evaluated demographic characteristics and dental use as potential confounders. We collected demographic information for age, race, and educational attainment. Age was measured in years and was coded as a quintile-categorical indicator variable. Race was coded as an indicator variable with terms for White, African American, and American Indian/Alaskan Native. Education was coded as a 4-level categorical variable (1 = did not finish high school, 2 = high school diploma or GED, 3 = some technical education or some college, and 4 = ≥ college education). Dental use referred to the time since the last dental visit and was coded as a 4-level categorical variable (4 = < 12 months, 3 = 12–23 months, 2 = 2–5 years, 1 = > 5 years).
Statistical Analyses
We generated descriptive statistics of OHL and DN sorted by demographic characteristics, dental use, and OHS. We tested the normality assumption for DN, OHL, and self-efficacy scores by means of a combined skewness and kurtosis evaluation test46 and a P < .05 criterion. To examine the association of self-efficacy scores with OHL and DN, we used graphical methods that were based on local polynomial smoothing functions to illustrate the bivariate associations and corresponding 95% confidence intervals (CIs). To further quantify these associations we computed Spearman's correlation coefficients (ρ) for their pairwise combinations and 95% CIs using bootstrapping (1000 repetitions). For all analyses we used the computed OHL, DN, and self-efficacy scores with no standardization, as in previous investigations.34,35,37–41
We used multivariate modeling based on log binomial regression to obtain prevalence ratios (PRs) and 95% CIs for the association of OHL with OHS (excellent/very good vs good/fair/poor). We chose log binomial regression instead of traditional logistic regression because odds ratios tend to overestimate the PR when the outcome is common (> 20%).47 Moreover, PR estimates obtained from log binomial models have a more straightforward interpretation in cross-sectional study designs.48
We considered race, age, education, and dental use to be a priori confounders of the association among OHL, DN, and health status; therefore, we included them in the minimal model (model A) and all subsequent analytical models. We empirically examined self-efficacy as an effect mediator in the association between OHL and health status by adding this variable (model B) and computing a “percentage change in estimate” using model A as the referent. This approach is analogous to a confounding evaluation. We evaluated effect measure modification by self-efficacy in the context of statistical interaction and a P < .1 criterion for the coefficient of an interaction term between self-efficacy and OHL. Its inclusion (model C) was also assessed with a change-in-estimate criterion of greater than or equal to 10% as follows: change = [ln(PRfull) – ln(PRreduced) / ln(PRreduced)] × 100.
The addition of the interaction term between OHL and self-efficacy was also evaluated with a likelihood ratio test (LRT χ2), comparing the full model (model C) and nested model (model B) and using a P < .1 criterion. We also employed a second multivariate model based on linear regression to obtain adjusted DN score differences and 95% CIs for the impact of literacy and self-efficacy on DN. We used Stata version 11.1 (StataCorp LP, College Station, TX) to conduct all analyses.
RESULTS
The demographic characteristics, dental use, and OHS of our analytical sample (n = 1280), along with the corresponding REALD-30 scores and DNS distribution characteristics, are presented in Table 1. The racial representation for Whites, African Americans, and American Indians/Alaska Natives was 2:2:1, and their mean age was 26.6 years (SD = 6.9). Two thirds of participants had a high school education or less, and less than one third rated their oral health as very good or excellent.
TABLE 1—
Distribution of REALD-30 and DNS Scores by Demographic Characteristics, Dental Use, and Oral Health Status Among Female WIC Participants: Carolina Oral Health Literacy Study, North Carolina, 2007–2009
| REALD-30b |
DNSc |
|||||
| Characteristic | No. a | % or Mean (SD) | Mean (SD) | Median | Mean (SD) | Median |
| All | 1280 | 100 | 15.8 (5.3) | 16 | 11.9 (3.2) | 12 |
| Race | ||||||
| White | 503 | 39.3 | 17.4 (4.9) | 17 | 12.0 (3.2) | 12 |
| African American | 522 | 40.8 | 15.3 (5.1) | 15 | 11.9 (3.2) | 12 |
| American Indian/Alaska Native | 255 | 19.9 | 13.7 (5.3) | 14 | 11.5 (3.3) | 12 |
| Education | ||||||
| Did not finish high school | 306 | 23.9 | 13.0 (4.8) | 13 | 11.1 (3.6) | 12 |
| High school diploma or GED | 479 | 37.4 | 15.0 (4.9) | 15 | 11.9 (3.1) | 12 |
| Some technical or college training | 430 | 33.6 | 18.0 (4.7) | 18 | 11.8 (3.1) | 12 |
| College degree or higher | 65 | 5.1 | 20.7 (4.8) | 21 | 11.0 (3.2) | 11 |
| Age, y, quintiles | ||||||
| Q1 (range: 17.2–20.9) | 256 | 19.5 (0.8) | 14.2 (4.8) | 15 | 11.4 (3.4) | 11 |
| Q2 (range: 20.9–23.4) | 256 | 22.1 (0.7) | 15.5 (5.2) | 15 | 12.1 (3.2) | 12 |
| Q3 (range: 23.4–26.5) | 256 | 24.8 (0.9) | 16.5 (5.0) | 16 | 11.6 (3.1) | 12 |
| Q4 (range: 26.5–30.9) | 256 | 28.6 (1.3) | 16.3 (4.8) | 16 | 12.1 (3.2) | 12 |
| Q5 (range: 30.9–65.6) | 256 | 37.7 (6.1) | 16.6 (6.0) | 17 | 12.0 (3.2) | 12 |
| Dental use (time since last dental visit) | ||||||
| < 12 mo | 727 | 57.1 | 15.8 (5.2) | 16 | 10.9 (3.2) | 11 |
| 12–23 mo | 218 | 17.1 | 16.1 (5.5) | 16 | 12.5 (3.0) | 12 |
| 2–5 y | 177 | 13.9 | 15.8 (5.6) | 16 | 13.3 (2.6) | 13 |
| > 5 y | 151 | 11.9 | 15.4 (4.7) | 15 | 13.9 (2.6) | 14 |
| “How would you describe the condition of your mouth and teeth?” | ||||||
| Excellent | 118 | 9.3 | 16.1 (5.6) | 17 | 9.0 (2.5) | 9 |
| Very good | 258 | 20.2 | 16.8 (5.3) | 17 | 10.3 (2.7) | 10 |
| Good | 481 | 37.7 | 15.6 (5.1) | 16 | 11.7 (2.8) | 12 |
| Fair | 287 | 22.5 | 15.5 (5.1) | 15 | 13.5 (2.8) | 13 |
| Poor | 131 | 10.3 | 15.4 (5.6) | 15 | 14.7 (3.1) | 15 |
Note. DNS = Dental Neglect Scale; REALD-30 = Rapid Estimate of Adult Literacy in Dentistry; WIC = Supplemental Nutrition Program for Women, Infants, and Children. The sample size was n = 1280.
Column figures may not add up to total because of missing values.
The REALD-30 is a validated word recognition test in which scale score ranges from 0 (lowest literacy) to 30 (highest literacy).
The DNS asks participants to report their agreement with 6 items describing their dental behaviors, with responses ranging from “definitely not” to “definitely yes” on a 4-point Likert scale (6 = least dental neglect; 24 = most dental neglect). These items are: “I keep my dental care at home”; “I receive the dental care I should”; “I need dental care, but I put it off”; “I brush as well as I should”; “I control snacking between meals as well as I should”; and “I consider my dental health to be important.”
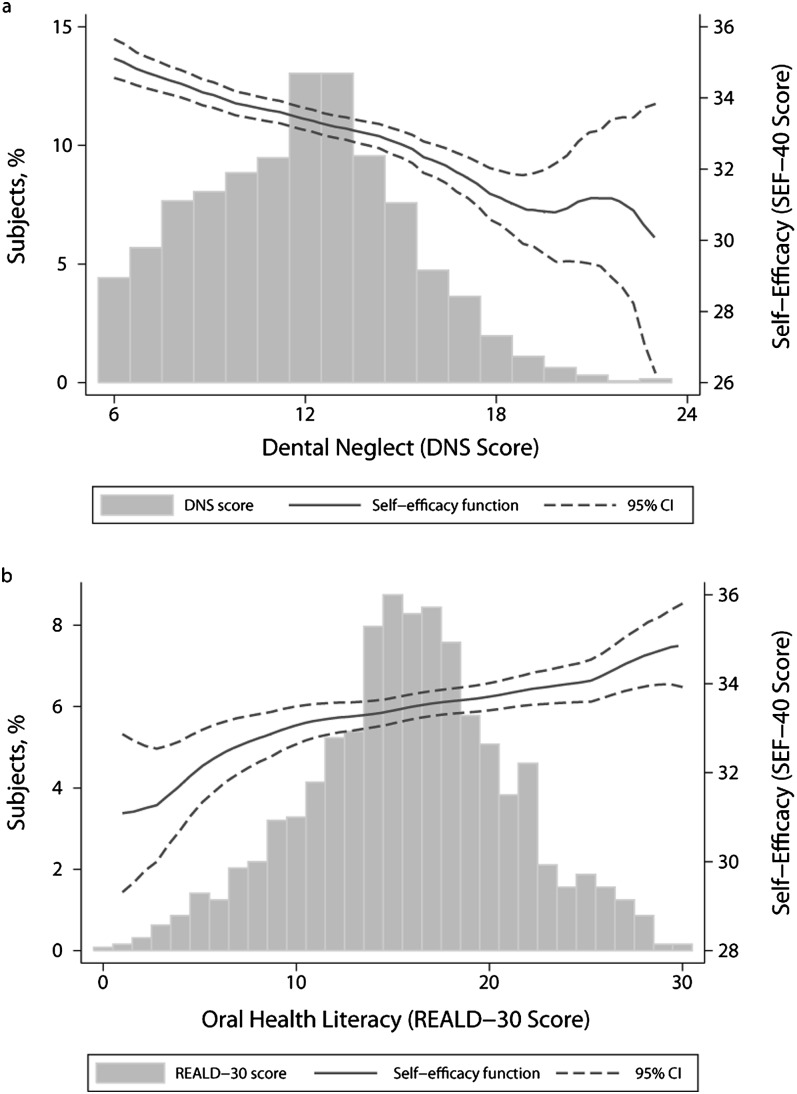
The overall distribution of REALD-30 and DNS scores is illustrated in Figure 2. OHL scores were normally distributed (χ2 = 1.53; df = 2; P > .05), with a mean of 15.8 (SD = 5.3) and a range of 0 to 30. DN scores were positively skewed, with a mean of 11.9 (SD = 3.2) and a range of 6 to 23. Self-efficacy scores were negatively skewed, with a mean of 33.4 (SD = 4.1) and a range of 15 to 40. Self-efficacy scores were positively correlated with DN and did not show any important pattern of association with OHL. Factor analysis confirmed that DN items loaded on 1 principal factor (eigenvalue = 1.5). Cronbach α for DN and self-efficacy was 0.62 and 0.81, respectively. Figure 2 also illustrates the bivariate relationships of self-efficacy with OHL and DN, and includes 2 histograms that illustrate the univariate distribution of OHL and DN. Pairwise Spearman's correlation coefficients among GSES score, OHL, and DN were ρDNS,GSES = −0.26 (95% CI = −0.31, −0.20); ρREALD-30,GSES = 0.10 (95% CI = 0.04, 0.15); and ρREALD-30,DNS = −0.02 (95% CI = −0.08, 0.04).
FIGURE 2—
Univariate distributions of (a) dental neglect scores and (b) oral health literacy overlaid by polynomial fit functions with self-efficacy among female WIC participants (n = 1280): Carolina Oral Health Literacy study, North Carolina, 2007–2009.
Note. CI = confidence interval; DNS = Dental Neglect Scale; REALD = Rapid Estimate of Adult Literacy in Dentistry; SEF = Self-Efficacy Scale; WIC = Supplemental Nutrition Program for Women, Infants and Children.
Higher DN scores were associated with worse OHS. We noted marked differences in OHL levels between education levels, ages, and racial groups (Table 1). Independent of race, age, education, and dental use, higher OHL was associated with better OHS (PR = 1.03; 95% CI = 1.01, 1.04), an estimate that corresponded to a 29% (95% CI = 8%, 54%) increase in prevalence of excellent/very good versus good/fair/poor oral health for a 10-point increase in OHL (Table 2, model A). Inclusion of self-efficacy in the model resulted in an 11% reduction in the measure of association between OHL and OHS (Table 2, model B). Furthermore, the interaction term between OHL and self-efficacy was retained in model C (P < .1), and its inclusion improved the model fit significantly (χ2 = 4.7; df = 1; P < .1).
TABLE 2—
Associations With Self-Reported Oral Health Status (Excellent/very good vs Good/fair/poor) Among Female WIC Participants: Carolina Oral Health Literacy Study, North Carolina, 2007–2009
| Model A, PR (95% CI) | Model B, PR (95% CI) | Model C, PR (95% CI) | |
| REALD-30 (OHL) scoreab | 1.03 (1.01, 1.04) | 1.02** (1.00, 1.04) | 0.88 (0.78, 1.00) |
| GSES scorebc | — | 1.05 (1.03, 1.08) | 0.98 (0.93, 1.05) |
| Interaction (self-efficacy × OHL) | — | — | 1.00* (1.00, 1.01) |
| Race | |||
| White (Ref) | 1.00 | 1.00 | 1.00 |
| African American | 0.96 (0.79, 1.16) | 0.89 (0.73, 1.07) | 0.88 (0.72, 1.06) |
| American Indian/Alaska Native | 1.22 (0.98, 1.52) | 1.18 (0.95, 1.47) | 1.18 (0.95, 1.47) |
| Age (quintiles) | 0.91 (0.85, 0.97) | 0.92 (0.86, 0.98) | 0.91 (0.86, 0.97) |
| Education level | 1.17 (1.06, 1.31) | 1.14 (1.03, 1.27) | 1.15 (1.03, 1.27) |
| Dental use | 0.77 (0.69, 0.84) | 0.78 (0.70, 0.85) | 0.77 (0.70, 0.85) |
Note. CI = confidence interval; GSES = General Self-Efficacy Scale; OHL = oral health literacy; PR = prevalence ratio; REALD-30 = Rapid Estimate of Adult Literacy in Dentistry; WIC = Supplemental Nutrition Program for Women, Infants, and Children. Estimates calculated by multivariate log binomial regression modeling. The sample size was n = 1280.
The REALD-30 is a validated word recognition test in which scale score ranges from 0 (lowest literacy) to 30 (highest literacy).
Estimates correspond to a 1-unit increase.
The GSES is a 10-item scale that is used to measure the construct of self-efficacy, which refers to one's coping ability across a wide range of demanding situations. The scale's scores range from 10 (lowest self-efficacy) to 40 (highest self-efficacy).
*P = .02; **P = .01.
The final model to determine the impact of OHL and self-efficacy on DN is presented in Table 3. When OHL and self-efficacy were jointly considered with regard to DN and independently of race, age, and education, self-efficacy and dental use were associated with significant decreases in DN scores, whereas OHL showed no pattern of association. Dental use could be considered as a “downstream” event of OHS in a hypothetical model, with worse dental condition leading to more dental visits, so we performed an iteration of our multivariate model that removed this variable. Exclusion of dental use from the multivariate model resulted in no change in the estimate of OHL (data not shown).
TABLE 3—
Associations With Dental Neglect Among Female WIC Participants: Carolina Oral Health Literacy Study, North Carolina, 2007–2009
| B (95% CI) | |
| REALD-30 (OHL) scoreab | 0.01 (−0.02, 0.05) |
| Race | |
| White (Ref) | 1.00 |
| African American | 0.25 (−0.12, 0.62) |
| American Indian/Alaska Native | −0.39 (−0.85, 0.07) |
| Age quintiles | 0.14 (0.02, 0.26) |
| Education level | −0.16 (−0.38, 0.05) |
| Dental use | −1.05 (−1.20, −0.90) |
| GSES scorebc | −0.18 (−0.22, −0.14) |
Note. CI = confidence interval; GSES = General Self-Efficacy Scale; OHL = oral health literacy; REALD-30 = Rapid Estimate of Adult Literacy in Dentistry; WIC = Supplemental Nutrition Program for Women, Infants, and Children. Estimates calculated by multivariate linear regression modeling. The sample size was n = 1280.
The REALD-30 is a validated word recognition test in which scale score ranges from 0 (lowest literacy) to 30 (highest literacy).
Estimate corresponds to a 1-unit increase.
The GSES is a 10-item scale that is used to measure the construct of self-efficacy, which refers to one's coping ability across a wide range of demanding situations. The scale's scores range from 10 (lowest self-efficacy) to 40 (highest self-efficacy).
DISCUSSION
Our investigation is the first to our knowledge to examine and report on the association of OHL with self-reported OHS and DN. We found that WIC clients with higher OHL were more likely to report excellent/very good OHS than good/fair/poor OHS. There was a poor correlation between OHL and DN. However, we found that lower self-efficacy was strongly correlated with DN, and this association persisted after adjustment for age, race, education, dental use, and OHL. Literacy, on the other hand, demonstrated a modest association with OHS after adjustment for age, race, education, and dental use.
The important role of self-efficacy in OHS provides support to conceptual models that place appropriate decision-making between conceptual knowledge and oral health outcomes.35,43 Increased self-efficacy may be a factor that enables individuals to engage in positive dental behaviors, which is consistent with theories of planned behavior,26 locus of control theory,24 and the social cognitive theory.32 As illustrated in our conceptual model (Figure 1), it is likely that personal characteristics such as self-efficacy mediate or modify the impact of literacy on oral health behaviors. We used the general self-efficacy measure instead of one specific to oral health. Although instruments that could capture dental care–specific dimensions have been developed and validated in dentistry,49–51 they have not been widely tested. By contrast, the role of general self-efficacy as a determinant, modifier, or moderator of health behavior change or maintenance is well-supported.33,34,52–55
Our data revealed a poor correlation between OHL and DN. Thomson and Locker41 defined the construct of DN as “failure to take precautions to maintain oral health, failure to obtain needed dental care, and physical neglect of the oral cavity.” This construct may be too narrow to encompass the entire spectrum of self-care, preventive attitudes, and dental attendance all together. Further work is warranted to identify these pathways that could be potential targets for oral health interventions.
Although the effect estimates for the association of OHL and self-efficacy with OHS are small (PR = 1.02 and 1.05, respectively, in model B), they correspond to 1-point changes in these variables. On the basis of these multivariate model–derived coefficients for the association of literacy and self-efficacy with OHS, we estimate that a 10-unit increase in REALD-30 scores corresponds to a PR of 1.25 (95% CI = 1.05, 1.49), and a 10-unit increase in GSES scores corresponds to a PR of 1.64 (95% CI = 1.31, 2.06). Moreover, the synergistic interaction between literacy and self-efficacy in model C, although small in magnitude, indicated that the effect of literacy was more pronounced among individuals with higher self-efficacy and that the effect of self-efficacy was more pronounced among individuals with higher literacy.
The rationale for considering both effect mediation and effect measure modification is supported by the fact that the determination of a variable as a mediator is context-specific and requires previous knowledge of underlying theory stating that the variable of interest is on a causal pathway between exposure and outcome.36 Previous studies examining health behaviors have indeed considered self-efficacy both as a mediator and as a modifier (moderator).56 In the context of OHL, no previous studies have examined the relationship between literacy and self-efficacy. Although some previous studies in medicine did not find an association between health literacy and self-efficacy,19,20 evidence from 2 recent investigations supports the link.18,57 Self-efficacy was also found to be a strong correlate of oral hygiene behaviors among Australian dental patients.49
Although we did not conduct formal pathway analyses to support the proposed conceptual model, we did find a marked effect attenuation of the OHL–OHS association when self-efficacy was entered into the model (contrast of models A and B). This finding indicates that OHL may confer its effect on OHS via self-efficacy, as has been suggested for health literacy and health status.17,52 This finding should be interpreted with caution until future studies formally investigate these pathways. Similarly, when DN was examined as the analytical endpoint, self-efficacy was significantly inversely correlated with neglect, but OHL did not show any material association.
Our finding of an interaction between literacy and self-efficacy constitutes evidence of effect measure modification that underscores the importance of considering both dental-specific factors and personality measures as correlates or antecedents of oral health behaviors and outcomes.31 Evidence indicates that self-efficacy may be improved via knowledge enhancement.58,59 Thus, providing individuals with the necessarily skills to obtain, understand, and act on dental-related information may increase their ability to cope with the demands of oral health maintenance and may ultimately lead to improved oral health outcomes.
Along these lines, Bandura60 suggested that “belief in one's efficacy to exercise control is a common pathway through which psychosocial influences affect health functioning.” If this paradigm were used when planning interventions, a determination could be made that certain individuals may benefit more from the use of visual materials to communicate key information, depending on literacy or self-efficacy criteria. Conversely, others may benefit from behavior reinforcement and motivational interviewing,61 a patient-centered, directive therapeutic technique designed to enhance readiness for change by helping individuals explore and resolve ambivalence59 and potentially increase their coping skills.61 Motivational interviewing has been used successfully for the treatment of health behavior–based problems,62 and it has been recently tested in the dental arena as a strategy for caregivers to use in prevention of early childhood caries.63 Stewart et al.59 and other recent reports64–66 described effective applications of such approaches in improving dental patients’ knowledge, self-efficacy, and behaviors.
These results should be considered in light of the study's limitations. The data were collected from a nonprobability convenience sample of clients from North Carolina WIC clinics. Our sample characteristics prevent generalization of results beyond females enrolled in WIC and attending the specific clinics in North Carolina during the time of this study. Future research should draw from a population-based probability sample. REALD-30 has been validated in English only, so our recruitment was limited to English-speaking patients. Also, our measurement of OHL is based on a word recognition test.37 Although word recognition instruments measure only selected aspects of literacy skills and are not comprehensive, comparable word recognition instruments have been used with success in medicine, and they are correlated strongly with reading fluency. Our initial investigations compared the REALD-30 to a dental functional health literacy test and found a high correlation between them.67 More recent reports comparing functional literacy estimates with word recognition and numeracy assessments have also confirmed the high correlation between these measures.68
Although our participants were recruited from a nonprobability convenience sample of WIC clients in a single US state and thus may have limited external validity, we feel that this population is an important one to examine. WIC was established by the Food and Nutrition Service of the US Department of Agriculture to target low-income women, infants, and children who are at risk nutritionally. WIC's goal is to improve the health outcomes of its clients by providing nutritious foods, nutritional education, counseling, and medical or dental referrals to facilitate good health care during pregnancy, the postpartum period, infancy, and early childhood. WIC has a huge reach, serving more than 9.1 million individuals annually and more than one third of all infants born in the United States.69 WIC is often the first contact that poor people have with the health care system. Because of its repeated contact with vulnerable populations, WIC is uniquely positioned to identify families with low health literacy.
To date, research in OHL has been based on only a few studies of care-seeking participants. This investigation is the first to our knowledge to report on the relationships among OHL, self-efficacy, DN, and self-reported OHS in a cohort of participants in a large public health program. On the basis of our findings, we advocate for the consideration of personality traits, such as self-efficacy, along with OHL as risk factors or screeners for poorer oral health outcomes and as important factors to consider when planning oral health intervention programs.
Acknowledgments
This research was supported by the National Institute of Dental and Craniofacial Research (grant RO1DE018045).
Note. The views expressed in the article are those of the authors and do not necessarily reflect the views of the National Institute of Dental and Craniofacial Research.
Human Participant Protection
This study protocol was approved by the biomedical institutional review board at the University of North Carolina at Chapel Hill.
References
- 1.Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education; 2006 [Google Scholar]
- 2.Kircsh I, Jungeblut A, Jenkins L, Kolstad A. Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey. Washington, DC: US Dept of Education; 1993 [Google Scholar]
- 3.Institute of Medicine Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004 [PubMed] [Google Scholar]
- 4.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Department of Health and Human Services; 2000 [Google Scholar]
- 5.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13(12):791–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–172 [DOI] [PubMed] [Google Scholar]
- 7.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87(6):1027–1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parker RM, Williams MV, Baker DW, Nurss JR. Literacy and contraception: exploring the link. Obstet Gynecol. 1996;88(suppl 3):72S–77S [DOI] [PubMed] [Google Scholar]
- 9.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–541 [DOI] [PubMed] [Google Scholar]
- 10.Williams MV, Parker RM, Baker DWet al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274(21):1677–1682 [PubMed] [Google Scholar]
- 11.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7(3):204–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33(5):374–378 [DOI] [PubMed] [Google Scholar]
- 14.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121(3):245–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paasche-Orlow MK, Wolf MS. Promoting health literacy research to reduce health disparities. J Health Commun. 2010;15(suppl 2):34–41 [DOI] [PubMed] [Google Scholar]
- 16.Volandes AE, Paasche-Orlow MK. Health literacy, health inequality and a just healthcare system. Am J Bioeth. 2007;7(11):5–10 [DOI] [PubMed] [Google Scholar]
- 17.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(suppl 1):S19–S26 [DOI] [PubMed] [Google Scholar]
- 18.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35(1):118–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision-making. Am J Health Behav. 2007;31(suppl 1):S27–S35 [DOI] [PubMed] [Google Scholar]
- 20.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829 [DOI] [PubMed] [Google Scholar]
- 21.National Institute of Dental and Craniofacial Research, National Institutes of Health, US Public Health Service, US Dept of Health and Human Services. The invisible barrier: literacy and its relationship with oral health. A report of a workgroup sponsored by the National Institute of Dental and Craniofacial Research, National Institutes of Health, US Public Health Service, US Dept of Health and Human Services. J Public Health Dent. 2005;65(3):174–182 [DOI] [PubMed] [Google Scholar]
- 22.Mucci LA, Björkman L, Douglass CW, Pedersen NL. Environmental and heritable factors in the etiology of oral diseases—a population-based study of Swedish twins. J Dent Res. 2005;84(9):800–805 [DOI] [PubMed] [Google Scholar]
- 23.Astrom AN, Ekback G, Ordell S, Unell L. Socio-behavioral predictors of changes in dentition status: a prospective analysis of the 1942 Swedish birth cohort. Community Dent Oral Epidemiol. 2011;39(4):300–310 [DOI] [PubMed] [Google Scholar]
- 24.Peker K, Bermek G. Oral health: locus of control, health behavior, self-rated oral health and socio-demographic factors in Istanbul adults. Acta Odontol Scand. 2011;69(1):54–64 [DOI] [PubMed] [Google Scholar]
- 25.Lindmark U, Hakeberg M, Hugoson A. Sense of coherence and oral health status in an adult Swedish population. Acta Odontol Scand. 2011;69(1):12–20 [DOI] [PubMed] [Google Scholar]
- 26.Buunk-Werkhoven YA, Dijkstra A, van der Schans CP. Determinants of oral hygiene behavior: a study based on the theory of planned behavior. Community Dent Oral Epidemiol. 2010;39(3):250–259 [DOI] [PubMed] [Google Scholar]
- 27.Stenström U, Einarson S, Jacobsson B, Lindmark U, Wenander A, Hugoson A. The importance of psychological factors in the maintenance of oral health: a study of Swedish university students. Oral Health Prev Dent. 2009;7(3):225–233 [PubMed] [Google Scholar]
- 28.Wolfe GR, Stewart JE, Hartz GW. Relationship of dental coping beliefs and oral hygiene. Community Dent Oral Epidemiol. 1991;19(2):112–115 [DOI] [PubMed] [Google Scholar]
- 29.Schou L. The relevance of behavioural sciences in dental practice. Int Dent J. 2000;50(6):324–332 [DOI] [PubMed] [Google Scholar]
- 30.Hollister MC, Anema MG. Health behavior models and oral health: a review. J Dent Hyg. 2004;78(3):6. [PubMed] [Google Scholar]
- 31.Yevlahova D, Satur J. Models for individual oral health promotion and their effectiveness: a systematic review. Aust Dent J. 2009;54(3):190–197 [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997 [Google Scholar]
- 33.Waller KV, Bates RC. Health locus of control and self-efficacy beliefs in a healthy elderly sample. Am J Health Promot. 1992;6(4):302–309 [DOI] [PubMed] [Google Scholar]
- 34.Syrjälä AM, Knuuttila ML, Syrjälä LK. Self-efficacy perceptions in oral health behavior. Acta Odontol Scand. 2001;59(1):1–6 [DOI] [PubMed] [Google Scholar]
- 35.Macek MD, Haynes D, Wells W, Bauer-Leffler S, Cotten PA, Parker RM. Measuring conceptual health knowledge in the context of oral health literacy: preliminary results. J Public Health Dent. 2010;70(3):197–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(suppl 2):5–14 [DOI] [PubMed] [Google Scholar]
- 37.Lee JY, Divaris K, Baker D, Rozier RG, Lee SY, Vann WF., Jr Oral health literacy levels among a low-income WIC population. J Public Health Dent. 2011;71(2):152–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30—a brief communication. J Public Health Dent. 2007;67(2):94–98 [DOI] [PubMed] [Google Scholar]
- 39.Jamieson LM, Thomson M. Dental health, dental neglect, and use of services in an adult Dunedin population sample. N Z Dent J. 2002;98(431):4–8 [PubMed] [Google Scholar]
- 40.Jamieson LM, Thomson WM. The dental neglect and dental indifference scales compared. Community Dent Oral Epidemiol. 2002;30(3):168–175 [DOI] [PubMed] [Google Scholar]
- 41.Thomson WM, Locker D. Dental neglect and dental health among 26-year-olds in the Dunedin Multidisciplinary Health and Development Study. Community Dent Oral Epidemiol. 2000;28(6):414–418 [DOI] [PubMed] [Google Scholar]
- 42.Coolidge T, Heima M, Johnson EK, Weinstein P. The Dental Neglect Scale in adolescents. BMC Oral Health. 2009;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacKinnon DP, Luecken L. Statistical analysis for identifying mediating variables in public health dentistry interventions. J Public Health Dent. 2011;71(suppl 1):S37–S46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. : Weinman J, Wright S, Johnston M, Measures in Health Psychology: A User's Portfolio. Causal and Control Beliefs. Windsor, UK: NFER-NELSON; 1995:35–37 [Google Scholar]
- 45.Scholz U, Gutiérrez-Doña B, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess. 2002;18(3):242–251 [Google Scholar]
- 46.D'Agostino RB, Balanger A, D'Agostino RB., Jr A suggestion for using powerful and informative tests of normality. Am Stat. 1990;44(4):316–321 [Google Scholar]
- 47.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Skov T, Deddens J, Petersen MR, Endahl L. Prevalence proportion ratios: estimation and hypothesis testing. Int J Epidemiol. 1998;27(1):91–95 [DOI] [PubMed] [Google Scholar]
- 49.Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: testing an extended Health Belief Model. Patient Educ Couns. 2010;78(2):269–272 [DOI] [PubMed] [Google Scholar]
- 50.Kakudate N, Morita M, Sugai Met al. Development of the self-efficacy scale for maternal oral care. Pediatr Dent. 2010;32(4):310–315 [PubMed] [Google Scholar]
- 51.Syrjälä A-MH, Kneckt MC, Knuuttila MLE. Dental self-efficacy as a determinant to oral health behaviour, oral hygiene and HbA1c level among diabetic patients. J Clin Periodontol. 1999;26(9):616–621 [DOI] [PubMed] [Google Scholar]
- 52.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15(suppl 2):146–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986;13(1):73–92 [DOI] [PubMed] [Google Scholar]
- 54.Skaret E, Kvale G, Raadal M. General self-efficacy, dental anxiety and multiple fears among 20-year-olds in Norway. Scand J Psychol. 2003;44(4):331–337 [DOI] [PubMed] [Google Scholar]
- 55.McCaul KD, O'Neill HK, Glasgow RE. Predicting the performance of dental hygiene behaviors: an examination of the Fishbein and Ajzen model and self-efficacy expectations. J Appl Soc Psychol. 1988;18(2):114–128 [Google Scholar]
- 56.Latka MH, Hagan H, Kapadia Fet al. A randomized intervention trial to reduce the lending of used injection equipment among injection drug users infected with hepatitis C. Am J Public Health. 2008;98(5):853–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolf MS, Davis TC, Osborn CY, Skripkauskas S, Bennett CL, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns. 2007;65(2):253–260 [DOI] [PubMed] [Google Scholar]
- 58.Renz AN, Newton JT. Changing the behavior of patients with periodontitis. Periodontol 2000 2009;51:252–268 [DOI] [PubMed] [Google Scholar]
- 59.Stewart JE, Wolfe GR, Maeder L, Hartz GW. Changes in dental knowledge and self-efficacy scores following interventions to change oral hygiene behavior. Patient Educ Couns. 1996;27(3):269–277 [DOI] [PubMed] [Google Scholar]
- 60.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164 [DOI] [PubMed] [Google Scholar]
- 61.Miller WSR. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford; 2002 [Google Scholar]
- 62.Hettema J, Steele J, Miller WR. A meta-analysis of research on motivational interviewing treatment effectiveness. Annu Rev Clin Psychol. 2005;1:91–111 [DOI] [PubMed] [Google Scholar]
- 63.Harrison R, Veronneau J, Leroux B. Design and implementation of a dental caries prevention trial in remote Canadian Aboriginal communities. Trials. 2010;11:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Buunk-Werkhoven YA, Dijkstra A, van der Wal Het al. Promoting oral hygiene behavior in recruits in the Dutch Army. Mil Med. 2009;174(9):971–976 [DOI] [PubMed] [Google Scholar]
- 65.Kakudate N, Morita M, Sugai M, Kawanami M. Systematic cognitive behavioral approach for oral hygiene instruction: a short-term study. Patient Educ Couns. 2009;74(2):191–196 [DOI] [PubMed] [Google Scholar]
- 66.Weyant R. Interventions based on psychological principles improve adherence to oral hygiene instructions. J Evid Based Dent Pract. 2009;9(1):9–10 [DOI] [PubMed] [Google Scholar]
- 67.Gong DA, Lee JY, Rozier RG, Pahel BT, Richman JA, Vann WF., Jr Development and testing of the Test of Functional Health Literacy in Dentistry (TOFHLiD). J Public Health Dent. 2007;67(2):105–112 [DOI] [PubMed] [Google Scholar]
- 68.Sabbahi DA, Lawrence HP, Limeback H, Rootman I. Development and evaluation of an oral health literacy instrument for adults. Community Dent Oral Epidemiol. 2009;37(5):451–462 [DOI] [PubMed] [Google Scholar]
- 69.US Dept of Agriculture, Food and Nutrition Service. WIC program participation and costs. Available at: http://www.fns.usda.gov/pd/wisummary.htm. Accessed March 21, 2011