Abstract
Laparoscopic adrenalectomy has become a gold standard in adrenal gland surgery. More recently, some minimally invasive trials have been conducted on single access surgery on the adrenal gland. In this study, we introduce our first experiences of robot-assisted posterior retroperitoneoscopic adrenalectomy using single-port access and the da Vinci system.
Keywords: Adrenalectomy, Robotics, Retroperitoneal space, Minimally invasive
INTRODUCTION
Recent advances in the technologic and surgical instrument fields have resulted in the developments of several novel surgical techniques, such as, Natural Orifice Transluminal Endoscopic Surgery and Laparoendoscopic Single-site Surgery, which minimize perioperative co-morbidities and increase cosmetic benefits [1]. However, these new techniques have several limitations due to restrictive instrumentation movement because of the small access ports used and relatively low-quality images produced.
In 1992, Gagner et al. [2] first introduced the use of laparoscopic adrenalectomy for the treatment of small adrenal tumors, and since, laparoscopic adrenalectomy has become a gold standard in adrenal gland surgery. More recently, some minimally invasive trials have been conducted on single access surgery on the adrenal gland [3].
In 2001, Horgan and Vanuno [4] described a robot-assisted laparoscopic adrenalectomy technique, and since, several institutions have reported their experiences of this technique using the da Vinci surgical robot system (Intuitive Surgical, Inc., Sunnyvale, CA, USA). The multi-articulated instruments of this robotic system and the 3-D, magnified image provided by its stable camera platform greatly benefit endoscopic adrenalectomy.
In this study, we introduce our first experiences of robot-assisted posterior retroperitoneoscopic adrenalectomy using single-port access and the da Vinci system. To the best our knowledge, this is the first case report issued on robotic single port adrenalectomy using a posterior retroperitoneal approach.
CASE REPORT
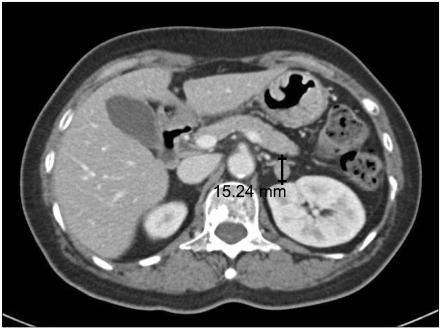
A 56-year-old woman was referred to our endocrine surgery division due to the presence of a 1.5 cm sized mass in her left adrenal gland (Fig. 1), which was incidentally found on an abdominal computed tomography scan during health screening. She had been taking 25 mg atenolol, 4 mg lacidipine, and 80 mg telmisartan daily under a diagnosis of hypertension for 12 years. Her initial blood pressure was 130/80 mmHg, and her routine laboratory tests, which included renal function tests, electrolyte, and 24-hour urinary catecholamines were normal. In the standing position, her morning plasma aldosterone level was 398 pmoL/L (standard range, 38.9 to 306.8 pmoL/L), her concurrently measured plasma renin activity was 0.01 µg/L/hr (standard range, 1.31 to 3.95 µg/L/hr), and her plasma aldosterone to renin activity ratio was 3,980 pmoL/L per µg/L/hr. In view of the hypertension and a raised plasma aldosterone to renin activity ratio, a working diagnosis of hyperaldosteronism-induced hypertension was made. We discussed surgical options with the patient and decided to perform robot-assisted single port retroperitoneoscopic adrenalectomy.
Fig. 1.
Computed tomography scan of the patient showing a 1.5 × 1.1 cm mass in the left adrenal gland.
The route used to approach the adrenal gland was slightly modified version of that described by Walz et al. [5].
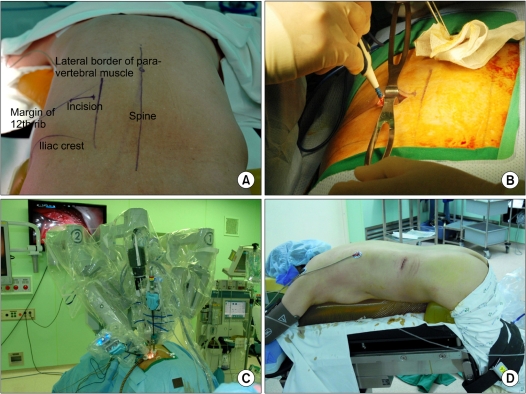
Under general anesthesia, the patient lies in prone, jack-knife position with hip joints bending at a right angle. Soft pillows were applied at the ventral portion of the chest and pelvis (Fig. 2D). Initially, a 3 cm-sized transverse skin incision was made just below the lowest tip of the 12th rib (Fig. 2A, B), and then subcutaneous and muscle layers were split and opened. After exposing the retroperitoneal space, the Glove port (NELIS, Bucheon, Korea) was applied to the skin incision and maintained pneumoretroperitoneum. CO2 was then insufflated to a pressure of 18 mmHg to create adequate working space.
Fig. 2.
Operative views of robotic posterior retroperitoneoscopic adrenalectomy using single access. (A) Anatomic landmark, (B) skin incision, (C) instrumentation of each robotic arms, and (D) operative position and postoperative wound.
A 10 mm robotic camera with 30 degree up view and three 5 mm robotic ports were inserted through 4 port of the Glove port. The camera was located at the center of incision and placed in its most cephalic portion. The Maryland dissector (Intuitive Surgical Inc.) was placed on the lateral side of the incision, and a harmonic curved shears (Intuitive Surgical Inc.) was placed on the medial side of the incision. The assistant port was placed on the most caudal portion and endoscopic metal suction tip (WISAP, Munchen, Germany) was introduced.
Using the Maryland dissector and the harmonic curved shears, retroperitoneal fatty tissue in the vessel free layer was detached from Gerota's fascia and pushed up for the identification of upper margin of the kidney. The adrenal gland and its tumor were then visualized and mobilized. Small vessels around the adrenal gland were then coagulated using the harmonic shears. The adrenal vein was found caudally, medial to the upper kidney pole, and ligated using the harmonic curved shears. The adrenal gland was then fully mobilized, and the adrenal gland and its tumor were delivered using a retrieval bag.
The total operation time was 188 minutes, and the console time was 57 minutes.
On the day of surgery, the patient started taking sips of water after full awakening, and on the 1st postoperative day, the patient gradually took a soft, general diet. Postoperatively, the patient received only an intravenous narcotic agent on the operative day. Analgesics were not required. The patient recovered well uneventfully and was discharged on the 3rd postoperative day. The permanent pathologic diagnosis was of adrenal cortical adenoma. Six month postoperatively, her blood pressure was well controlled without an antihypertensive agent.
DISCUSSION
Laparoscopic adrenalectomy can be performed in four ways, that is, by using transperitoneal approaches in the supine or lateral position or retroperitoneal approaches in the lateral or prone position. Walz et al. [6] demonstrated the feasibility, safety, wide applicability, and speed of the posterior retroperitoneal approaches to the adrenal glands.
In 2001, Horgan and Vanuno [4] reported the first robot-assisted laparoscopic adrenalectomy, and since, more than 100 cases of robotic adrenalectomy using the transperitoneal approaches have been performed. However, no report on robot-assisted posterior retroperitoneoscopic adrenalectomy or on single port robotic adrenalectomy has been issued. Elias and colleagues reviewed the literature on robotic adrenalectomy and comparisons made between laparoscopic and robotic adrenalectomy. Operative times for robotic and laparoscopic cases were 99 to 188 and 82 to 131 minutes, respectively, and times to discharge were 4 to 6.7 and 3.4 to 6.9 days, respectively [7]. Wu et al. [8] demonstrated that robotic adrenalectomy is well tolerated and effective, has short-term outcomes, which are comparable with those of laparoscopic adrenalectomy, and has subjective advantages regarding fine motion, dexterity, and surgeon comfort. As compared with robotic adrenalectomy data previously reported [7], our results indicate that operative time was somewhat longer, which is probably because it was our first experience and more time was required to create an adequate working space and to effectively utilize robotic system instruments via the single access port.
Compared to robot-assisted transperitoneal adrenalectomy, robot-assisted single port retroperitoneoscopic adrenalectomy could not only reduce postoperative ileus, bacterial contamination, and intestinal complications because of not opening the peritoneal cavity, but also reduce postoperative pain because of using minimally invasive single-access approaches.
Our initial experiences of robot-assisted single port retroperitoneoscopic adrenalectomy did much to assure us of its safety and feasibility. We suggest that robot-assisted single port retroperitoneoscopic adrenalectomy be viewed as a useful surgical option for the treatment of adrenal pathologies.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Box G, Averch T, Cadeddu J, Cherullo E, Clayman R, Desai M, et al. Nomenclature of natural orifice translumenal endoscopic surgery (NOTES) and laparoendoscopic single-site surgery (LESS) procedures in urology. J Endourol. 2008;22:2575–2581. doi: 10.1089/end.2008.0471. [DOI] [PubMed] [Google Scholar]
- 2.Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992;327:1033. doi: 10.1056/NEJM199210013271417. [DOI] [PubMed] [Google Scholar]
- 3.Walz MK, Alesina PF. Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery. Langenbecks Arch Surg. 2009;394:447–450. doi: 10.1007/s00423-008-0418-z. [DOI] [PubMed] [Google Scholar]
- 4.Horgan S, Vanuno D. Robots in laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2001;11:415–419. doi: 10.1089/10926420152761950. [DOI] [PubMed] [Google Scholar]
- 5.Walz MK, Peitgen K, Hoermann R, Giebler RM, Mann K, Eigler FW. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg. 1996;20:769–774. doi: 10.1007/s002689900117. [DOI] [PubMed] [Google Scholar]
- 6.Walz MK, Alesina PF, Wenger FA, Deligiannis A, Szuczik E, Petersenn S, et al. Posterior retroperitoneoscopic adrenalectomy--results of 560 procedures in 520 patients. Surgery. 2006;140:943–948. doi: 10.1016/j.surg.2006.07.039. [DOI] [PubMed] [Google Scholar]
- 7.Hyams ES, Stifelman MD. The role of robotics for adrenal pathology. Curr Opin Urol. 2009;19:89–96. doi: 10.1097/MOU.0b013e32831b446c. [DOI] [PubMed] [Google Scholar]
- 8.Wu JC, Wu HS, Lin MS, Chou DA, Huang MH. Comparison of robot-assisted laparoscopic adrenalectomy with traditional laparoscopic adrenalectomy - 1 year follow-up. Surg Endosc. 2008;22:463–466. doi: 10.1007/s00464-007-9488-1. [DOI] [PubMed] [Google Scholar]