Abstract
Cystadenoma of the liver is a rare neoplasm. Although many cystadenomas are asymptomatic, symptoms can include abdominal pain, postprandial epigastric discomfort, and nausea. Dramatic changes in hepatic imaging techniques have been helpful for diagnosing cystic lesions of the liver, such as simple cyst, hydatid cyst, cystadenoma, cystadenocarcinoma, and metastatic neuroendocrine tumors. However, it remains difficult to differentiate cystadenoma from cystadenocarcinoma for multiseptated cystic hepatic lesions with papillary projection on computed tomography (CT) and magnetic resonance imaging (MRI). Here we report the case of a 47-year-old woman with several months of postprandial discomfort and abdominal fullness. CT and MRI revealed multiseptated cystic lesions with papillary excrescences. A left hemihepatectomy was performed. Histology showed a benign mucinous cystic tumor with ovarian-like stroma.
Keywords: Liver, Papillary cystadenoma, Ovarian-like stroma
INTRODUCTION
Biliary cystadenoma and cystadenocarcinoma constitute less than 5% of intrahepatic cysts originating from the bile duct [1]. Hepatobiliary cystadenoma is considered a premalignant lesion, and the presence of ovarian stroma, regardless of the features of the epithelium, is a favorable prognostic sign [2,3]. Recent, dramatic changes in imaging techniques may be helpful for differentiating cystadenoma from cystadenocarcinoma. However, surgeons should be very cautious in their decisions about appropriate treatment for well-demarcated cystic lesions with internal septation on computed tomography (CT). Internal septation and polypoid protrusions or wall excrescences on CT should raise concern for cystadenocarcinoma [4]. Internal nodularity and septation, wall hemorrhage, and hemorrhagic internal fluid are all suggestive of biliary cystadenocarcinoma. There are various Korean medical reports about biliary cystadenoma and cystadenocarcinoma with good results after complete excision of lesions [5,6]. Due to the malignant potential of cystadenoma, complete resection is necessary.
CASE REPORT
A 47-year-old woman was admitted to the hospital with a several-month history of postprandial discomfort and abdominal bloating. The patient had been well until five months prior to presentation, when she began to have epigastric distension. The patient had no history of endoscopic evaluation or previous abdominal surgery. She had not taken oral contraceptives for approximately 20 years. On physical examination, a palpable mass was found in the right upper quadrant and epigastric area. Three years earlier she had undergone an abdominal ultrasound (US) at another hospital for general weakness. The US demonstrated a 4 × 5.5 cm well-defined cyst that was considered a simple hepatic cyst. She did well until June 2007, at which time she presented with symptoms. An ultrasound revealed a multiseptated 10 × 20 cm hepatic cyst. Biochemical tests were unremarkable, except for a preoperative carbohydrate antigen (CA) 19-9 level of 61.35 U/mL. Contrast-enhanced CT scan of the abdomen demonstrated a 20 × 15 × 12 cm cyst localized in hepatic segments II and III, with several smaller cysts inside (Fig. 1). Following that exam, the patient underwent magnetic resonance imaging, which was diagnostic for hepatic cystadenoma (Fig. 2). The cystadenoma compressed the inferior vena cava and the right and medial hepatic veins. The wall of the cyst was detached from the hepatic parenchyma due to hemorrhagic leak. Posterior to the hepatic peduncle, the wall of the cyst emerged at the liver surface, just underneath Glisson's capsule. The patient was brought to the operating room in an elective setting. A midline incision was performed. Intraoperative liver ultrasound was employed. A large, well-demarcated, round mass occupied nearly the entire left lobe. There were no other cystic lesions in the right hepatic lobe. The right lobe seemed to be smaller due to this huge mass. The gallbladder was shifted to the right but appeared normal, and no bile duct dilatation was seen. We proceeded with a left hemihepatectomy considering the malignant potential. The cut section of the specimen revealed a large cystic mass filled with gray-brown mucinous fluid and multiple communicating loculations of different sizes (Figs. 3, 4). The loculations were lined by columnar, cuboidal, or even flattened epithelium, which was surrounded by a layer of highly cellular mesenchymal tissue that resembled ovarian stroma (Fig. 5). Cystic fluid analysis showed normal levels of CA 19-9. The postoperative course was uneventful, and the patient was discharged on postoperative day 14. Histology confirmed the diagnosis of mucinous biliary cystadenoma with ovarian-like stroma.
Fig. 1.
Contrast-enhanced computed tomography showing a cystic lesion in liver segments II and III.
Fig. 2.
Magnetic resonance imaging showing a cystic lesion in liver segments II and III with papillary projections.
Fig. 3.
Gross photograph of a typical formalin-fixed resected specimen of a biliary cystadenoma, showing a trabecular, multilocular cystic lesion with a thickened wall.
Fig. 4.
Cut section of the specimen revealing a large cystic mass filled with gray-brown mucinous fluid and multiple communicating loculations of different sizes.
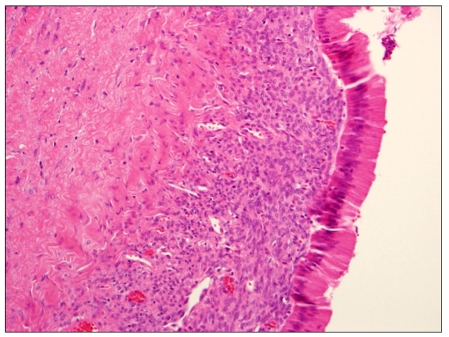
Fig. 5.
The loculations were lined by columnar, cuboidal, or even flattened epithelium, which was surrounded by a layer of highly cellular, mesenchymal tissue that resembled ovarian stroma (H&E, ×400).
DISCUSSION
Primary biliary cystadenoma and cystadenocarcinoma of the intrahepatic biliary systems are rare tumors [1]. Biliary cystadenomas mainly affect women, and this is a different gender preponderance than is seen for biliary cystadenocarcinoma [2]. These tumors are usually large, multilocular, and cystic in appearance [3]. Biliary cystadenomas are multiloculated cysts with an epithelial lining composed of biliary-type cuboidal or nonciliated columnar cells and are surrounded by a stroma that mimics ovarian stroma in 85 to 90% of cases [3]. Typical presenting symptoms are abdominal pain and jaundice, and signs of cholangitis may be present in the setting of significant biliary obstruction [7]. Radiologic studies, such as sonography and CT, may reveal cystadenoma. Occasionally imaging reveals internal septations or papillary infoldings of the cyst itself. A significant solid component in the cyst suggests malignancy. Biliary cystadenoma is considered a premalignant condition, and only microscopic investigations can reliably differentiate it from its malignant counterpart, cystadenocarcinoma. Of special interest in their report, the demonstration of benign epithelium in majority of the cystadenocarcinomas makes it highly probable that they arose in previously benign cystadenomas. The presence of benign epithelium in most cystadenocarcinomas supports their origin from cystadenoma [8]. Suh et al. [5] also reports there are foci of benign epithelium in biliary cystadenocarcinoma and all of the biliary cystadenoma cases had mesenchymal stroma resembling ovarian stroma. Recently, both cystadenomas and cystadenocarcinomas have been divided into those with ovarian-like stroma, implying a good prognosis, and those without ovarian-like stroma, implying a poor prognosis [3]. Although neoplasms with ovarian-like stroma are predominantly seen in women, those without ovarian stroma are evenly dispersed between both sexes. Laboratory tests of liver function are usually normal unless the biliary tree is compressed, which results in elevation of alkaline phosphatase and perhaps bilirubin. CA 19-9 may be elevated, but carcinoembryonic antigen and alpha-fetoprotein are usually normal. Cystadenomas require complete excision. Partial excision results in persistence or recurrence of the cyst and associated symptoms [6,9]. Although rare, transformation into a cystadenocarcinoma has been reported [10]. Excision of cystadenomas can be accomplished by either liver resection or enucleation. Reports supporting resection cite the low associated mortality of the procedure and the permanent relief of symptoms [9].
In conclusion, biliary cystadenoma should be considered when radiologic imaging reveals a multilocular cystic hepatic lesion with papillary excrescences. Treatment requires complete resection because of the malignant potential. Hepatic resection may be necessary to achieve complete excision of the cyst. Complete surgical resection yields excellent results.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Thomas KT, Welch D, Trueblood A, Sulur P, Wise P, Gorden DL, et al. Effective treatment of biliary cystadenoma. Ann Surg. 2005;241:769–773. doi: 10.1097/01.sla.0000161982.57360.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wheeler DA, Edmondson HA. Cystadenoma with mesenchymal stroma (CMS) in the liver and bile ducts. A clinicopathologic study of 17 cases, 4 with malignant change. Cancer. 1985;56:1434–1445. doi: 10.1002/1097-0142(19850915)56:6<1434::aid-cncr2820560635>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 3.Devaney K, Goodman ZD, Ishak KG. Hepatobiliary cystadenoma and cystadenocarcinoma. A light microscopic and immunohistochemical study of 70 patients. Am J Surg Pathol. 1994;18:1078–1091. [PubMed] [Google Scholar]
- 4.Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001;21:895–910. doi: 10.1148/radiographics.21.4.g01jl16895. [DOI] [PubMed] [Google Scholar]
- 5.Suh KS, Ahn SM, Kim SW, Lee KU, Park YH, Kim ST. Biliary cystadenoma and cystadenocarcinoma. J Korean Surg Soc. 1996;50:410–416. [Google Scholar]
- 6.Park SJ, Lee HY, Joo SH, Kim YW, Lee SM, Hong SW. Biliary cystadenoma and cystadenocarcinoma. J Korean Surg Soc. 2007;73:77–82. [Google Scholar]
- 7.Sato M, Watanabe Y, Tokui K, Kohtani T, Nakata Y, Chen Y, et al. Hepatobiliary cystadenocarcinoma connected to the hepatic duct: a case report and review of the literature. Hepatogastroenterology. 2003;50:1621–1624. [PubMed] [Google Scholar]
- 8.Ishak KG, Willis GW, Cummins SD, Bullock AA. Biliary cystadenoma and cystadenocarcinoma: report of 14 cases and review of the literature. Cancer. 1977;39:322–338. doi: 10.1002/1097-0142(197701)39:1<322::aid-cncr2820390149>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 9.Regev A, Reddy KR, Berho M, Sleeman D, Levi JU, Livingstone AS, et al. Large cystic lesions of the liver in adults: a 15-year experience in a tertiary center. J Am Coll Surg. 2001;193:36–45. doi: 10.1016/s1072-7515(01)00865-1. [DOI] [PubMed] [Google Scholar]
- 10.Akwari OE, Tucker A, Seigler HF, Itani KM. Hepatobiliary cystadenoma with mesenchymal stroma. Ann Surg. 1990;211:18–27. doi: 10.1097/00000658-199001000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]