Abstract
INTRODUCTION
Low back ache is a common complaint in the elderly and in the absence of red flag symptoms can be easily dismissed as benign. Pheochromocytoma presenting as back pain is unusual and to our knowledge, only two previous cases have been reported in the literature with back pain as the ‘only’ presenting symptom.
CASE PRESENTATION
We illustrate the case of an 85 year-old woman who presented with a 6 month history of back pain due to a very large Pheochromocytoma. This was incidentally picked up during a routine Lumbar spine plain radiograph and was noted to be a large Pheochromocytoma occupying the whole of the left abdomen. She required an open adrenalectomy to remove the large left adrenal tumour weighing 2.3 kg.
CONCLUSION
Pheochromocytoma can present as a mimic of musculoskeletal conditions and hence due care should be exercised in assessing such presentations both in the young and elderly patients. Our patient is different from the other reported cases, as she is an 85 year-old and ‘back pain’ can be easily dismissed without investigating in such age groups, thereby missing serious conditions.
Keywords: Pheochromocytoma, Laparotomy, MIBG (iodine-131-meta-iodobenzylguanidine), CT (computed tomography), MRI (magnetic resonance imaging), Catecholamine, MEN (multiple endocrine neoplasia) II syndrome, Guanethidine
1. Introduction
Pheochromocytomas are rare catecholamine secreting tumours derived from the chromaffin cells and usually present in young or middle-aged adults. They produce diverse clinical effects due to hormone secretion and local effects. They are seen in 0.1–0.9% of hypertensive individuals.1 The typical presenting symptoms in more than 90% of cases with Pheochromocytoma are headache, palpitation, perspiration or paroxysmal hypertension. The clinically silent tumours are assumed to produce little or no catecholamines and tend to be larger. These are usually picked up incidentally during imaging done for other reasons.
Pheochromocytomas produce effects due to the catecholamines secreted and can cause life threatening hypertensive crises. A minimum of 3 timed urinary samples may be required to make the diagnosis as secretion of hormones can be intermittent and may be missed. Larger tumours with necrosis may also not produce hormones as seen in our case. The tumour has diverse radiological appearances and range from small solid tumours to large cystic, haemorrhagic and calcified tumours.
2. Case presentation
An 85 year-old woman with a 6 month history of low back pain was referred to our department following the detection of a large abdominal mass. The general practitioner had initially referred her for a plain radiograph of the Lumbar spine to evaluate the back pain. She did not have any abdominal pain, spinal cord compression symptoms or radicular pain. Her BP was 200/90 mmHg during her initial presentation to the General practitioner's surgery.
The Lumbar spine plain film showed a large partially calcified lesion on the left side of the abdomen extending posteriorly (Fig. 1). An ultrasound scan suggested the possibility of an enlarged spleen. CT scan confirmed the presence of a large cystic tumour with extensive calcifications arising from the left adrenal gland and pushing the spleen anteriorly and left kidney inferiorly. MRI scan of the adrenals confirmed the CT scan findings and suggested a possible Pheochromocytoma (Fig. 2). An MIBG scan showed a large photopenic area localised to the left adrenal mass (Fig. 3) and areas of increased tracer activity in the periphery of this mass suggestive of Guanethidine positive receptors, thereby predicting the lesion as a probable Pheochromocytoma. 24-h urine collections for catecholamine metabolites and cortisol were normal.
Fig. 1.

Plain Lumbar spine film showing calcified lesion on the left side of the abdomen.
Fig. 2.
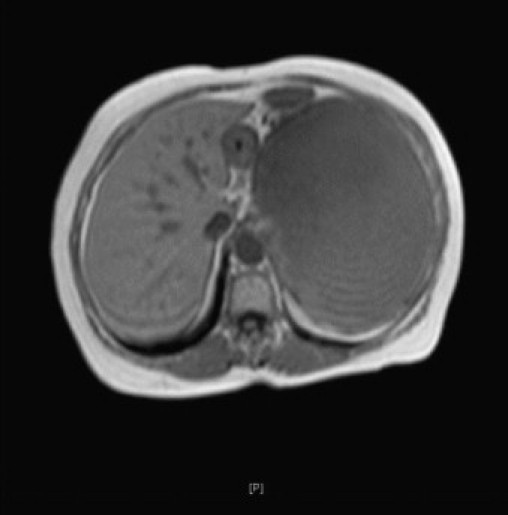
MRI scan showing the left adrenal mass occupying whole of the left abdomen, pushing spleen antero-medially and left kidney antero-inferiorly.
Fig. 3.
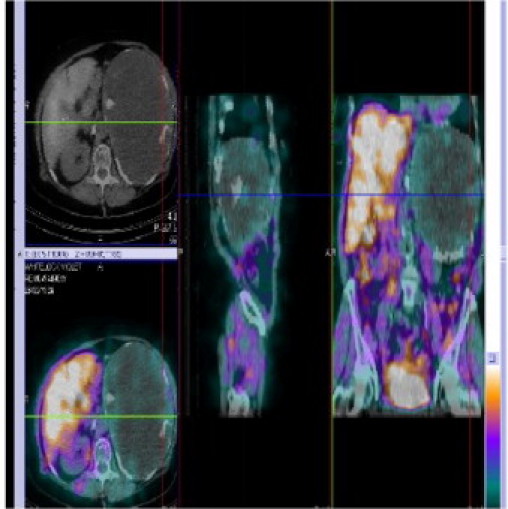
MIBG scan showing areas of increased tracer activity in the periphery of this mass suggestive of Guanethidine positive receptors in a Pheochromocytoma.
She was treated with alpha receptor blocking drugs prior to surgery. A very large tumour of size 28 × 16 × 13 cm was excised at laparotomy weighing 2.3 kg (Fig. 4). The tumour was cystic and nodular containing necrotic areas with haemorrhage and calcified material. The largest nodule measured 6.7 × 5 × 5 cm. Histopathology confirmed Pheochromocytoma. She made an uneventful recovery with normalisation of blood pressure and was discharged 13 days post-operatively.
Fig. 4.

Large tumour of size 28 × 16 × 13 cm was excised, weighing 2.3 kg.
3. Discussion
Pheochromocytoma presenting as back pain is unusual and to our knowledge, only a few cases have been reported in the literature with back pain as the ‘only’ presenting symptom.2, 3, 4 They can present with other associated symptoms due to high catecholamine levels like watery diarrhoea and abdominal pain.5 There has been another report from Japan of a patient with ruptured Pheochromocytoma presenting with back pain6 but with unruptured cases, it is very rare.
Rarely these Pheochromocytomas can occur extra-adrenally in the organs of Zuckerkandl and can present as back pain or can lead to sudden death as a result of hypertensive crises.7 These reports were from patients with in age group 20s–60s.2, 3, 4, 5, 6, 7
Our patient had a very large tumour without catecholamine secretion, possibly due to large areas of necrosis and/or intermittent nature of secretion of catecholamines, but conclusively proven to have Guanethidine receptors and presented with non-specific lumbago symptoms picked up on routine plain radiograph. Furthermore, her blood pressure did normalise post-operatively. The size with accompanying pressure effect had caused low back ache in our patient. The elderly patients with low back ache without neurological and ‘red flag’ symptoms most often have a benign cause for this, but occasionally a rare and significant cause is identified.
4. Conclusion
This case alerts us to the fact that Pheochromocytoma and other retroperitoneal tumours can mimic musculoskeletal conditions and therefore patients with new spinal pain warrant a routine radiological examination. Clinicians should be aware of rare presentations and mimicry of serious conditions.
Competing interests
The authors declare that they have no competing interests.
Funding
No source of funding.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors’ contributions
RK and JRN went through the patient notes, lab reports and made the initial draft. AH made the necessary corrections, checked the references and made the final draft. RH went through the manuscript making relevant corrections and finalising images. All authors read and approved the final manuscript.
References
- 1.Sweeney Ann T. Pheochromocytoma. eMedicine. 2009 Jul 31. [Google Scholar]
- 2.Davis M., Bove G. A case of pheochromocytoma presenting as low back pain. J Manipulative Physiol Ther. 2007;30(8):598–601. doi: 10.1016/j.jmpt.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Hamdan A., Hirsch D., Green P., Neumann A., Drozd T., Molad Y. Pheochromocytoma: unusual presentation of a rare disease. Isr Med Assoc J. 2002;4:827–828. [PubMed] [Google Scholar]
- 4.Arcos C.T., Luque V.R., Luque J.A., Garcia P.M., Jimenez A.B., Munoz M.M. Malignant giant pheochromocytoma: a case report and review of the literature. Can Urol Assoc J. 2009;3(6):E89–E91. doi: 10.5489/cuaj.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salmi J., Pelto-Huikko M., Auvinen O., Karvonen A.L., Saaristo J., Paronen I., et al. Adrenal pheochromocytoma-ganglioneuroma producing catecholamines and various neuropeptides. Acta Med Scand. 1988;224:403–408. doi: 10.1111/j.0954-6820.1988.tb19603.x. [DOI] [PubMed] [Google Scholar]
- 6.Mayumi M., Haruhiro S., Mitsunori Y., Sunao S.H., Toshiro T., Robert Y.O. Spontaneous rupture of pheochromocytoma and its clinical features: a case report. Tokai J Exp Clin Med. 2008;33(3):110–115. [PubMed] [Google Scholar]
- 7.Sperry K., Smialek J.E. Sudden death due to a paraganglioma of the organs of Zuckerkandl. Am J Forensic Med Pathol. 1986;7:23–29. doi: 10.1097/00000433-198603000-00005. [DOI] [PubMed] [Google Scholar]


