Abstract
INTRODUCTION
Infectious mononucleosis is common among young adults and teenagers. However, spontaneous rupture of spleen secondary to IM is rare and it is the most frequent cause of death in infectious mononucleosis.
PRESENTATION OF CASE
A previously healthy 16-year-old girl presented with a one-week history of sore throat, non-productive cough, fever, malaise and a positive Monospot test. Prior to transfer to the hospital, she had two syncopal episodes and a complaint of abdominal pain at home. Clinical examination revealed that she was febrile and mildly tachycardic with an evidence of localised peritonism on her left upper quadrant. Urgent abdominal ultrasound and computed tomography scan showed subcapsular haematoma with a significant amount of complex fluid within the abdominal cavity, especially the left flank. Emergency laparotomy was performed and a moderate amount of haemoperitoneum was evacuated. The spleen was found grossly enlarged with a haematoma identified on the ruptured capsule. Splenectomy was performed and peritoneal cavity was washed out meticulously prior to the closure of the abdominal wall.
DISCUSSION
Despite the fact that infectious mononucleosis is a self-limiting disease, it may cause serious and lethal complications. The best treatment of splenic rupture secondary to infectious mononucleosis has been controversial but it is mainly based on the haemodynamical status of the patient and the experience of the treating surgeon.
CONCLUSION
Spontaneous rupture of spleen secondary to IM can be lethal in those patients with high possibility of deterioration with conservative management, thus timely surgical intervention is required.
Keywords: Spleen, Splenic rupture, Splenectomy, Infectious mononucleosis, Kissing disease
1. Introduction
Infectious mononucleosis is common among young adults and teenagers with an incidence of 345–671 cases per 100,000 population per year.1 It is caused by an infection with the Epstein Barr virus with a triad of fever, sore throat and cervical lymphadenopathy. Majority of patients will have asymptomatic splenomegaly. Splenomegaly is caused by the proliferation of mononuclear cells in the spleen as reaction from Epstein Barr virus infection. However, spontaneous rupture or atraumatic rupture of spleen secondary to infectious mononucleosis is rare with an estimation of 0.06%2 to 0.5%3 and it is the most frequent cause of death in infectious mononucleosis.
2. Presentation of case
A previously healthy 16-year-old girl presented to the emergency department (ED) of a hospital in Southern Sydney. She had had a one-week history of sore throat, non-productive cough, fever and malaise. No history of trauma was reported. A course of oral antibiotic was prescribed by her local doctor the week prior to her ED presentation and ceased because of a positive Monospot test. At her home, she complained of an overnight history of chest and abdominal tenderness. In the morning, she was found lying on the floor of the toilet after a bang heard and loss of consciousness for approximately 10 s. She had a second syncopal episode a while later but regained consciousness quickly. Her parents called the ambulance and she was found with a systolic blood pressure of 80 mmHg at scene and intravenous resuscitation was commenced during transfer to the emergency department. At the hospital, she was alert and orientated. On admission, she was haemodynamically stable with evidence of postural hypotension and mildly tachycardic. Tympanic temperature of 38° was recorded. On examination, her abdomen was tender on palpation and left upper quadrant was involuntarily guarded. Spleen was not palpable due to guarding and severe tenderness. Tonsillitis was seen but no cervical lymph nodes were palpable. Laboratory tests found her haemoglobin to be low (89 g/L) and leucocyte count normal. Surgical consultation was immediately arranged and spontaneous rupture of the spleen was the primary diagnosis. Urgent abdominal ultrasound (Fig. 1) and computed tomography scan (Fig. 2) showed subcapsular haematoma with a significant amount of complex fluid within the abdominal cavity, especially the left flank. Emergency laparotomy was performed and a moderate amount of haemoperitoneum was evacuated. The spleen was found grossly enlarged with a haematoma identified on the ruptured capsule (Fig. 3). Splenectomy was performed and peritoneal cavity was washed out meticulously prior to the closure of the abdominal wall. Post-operatively she was recovering in intensive care unit with no blood transfusion required. She was transferred from intensive care unit to ward on day 4 post-operatively. Prior to discharge home on day 8, she was vaccinated for meningococcus, pneumococcus, and Haemophilius influenza.
Fig. 1.
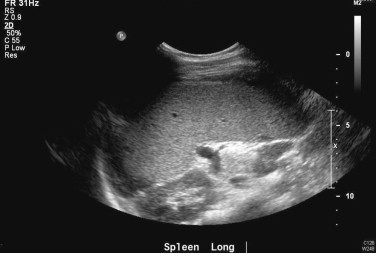
Urgent abdominal ultrasound showed subcapsular haematoma with a significant amount of complex fluid within the abdominal cavity.
Fig. 2.

Computed tomography scan showed subcapsular haematoma with a significant amount of complex fluid within the abdominal cavity, especially the left flank.
Fig. 3.
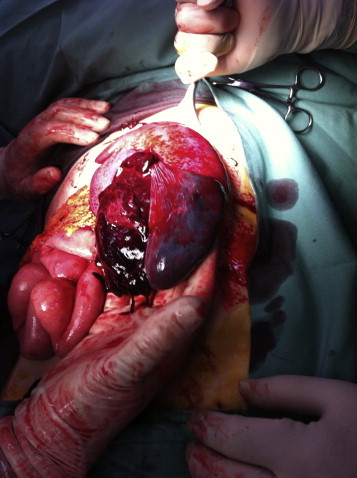
The spleen was found grossly enlarged with a haematoma identified on the ruptured capsule.
3. Discussion
Despite the fact that infectious mononucleosis is a self-limiting disease, it may cause serious and lethal complications. The mechanism of splenic rupture secondary to infectious mononucleosis has been controversial. It is commonly believed that it is caused by an increase in intra-abdominal pressure or contraction of the diaphragm with vigorous cough, vomiting and defecation, leading to a compression of the spleen.4 However, Patel et al. argue that it is primarily the result of an expanding subcapsular haematoma which subsequently tears the capsule and leads to haemoperitoneum.5 Traditionally, rupture of spleen is treated by splenectomy. The rationale is to prevent the chance of sudden death as an early complication of splenic rupture and the risk from blood transfusion. Primary repair was considered, but the difficulties in technique due to the enlargement and friability of the diseased spleen and high chance of rebleed made it less favoured.6,7 Based on the immunologic role of spleen and post-splenectomy infection (OPSI), there has been a trend on conservative management for splenic rupture on those patients with haemodyanamically stability.8 The survival rate of splenectomy in those patients is close to 100% in the literature.9,10 With potential death from rupture of spleen in infectious mononucleosis, the survival benefit outweighs the risks of sepsis from post-splenectomy infection.
4. Conclusion
Spontaneous rupture or atraumatic rupture of spleen secondary to infectious mononucleosis is rare but lethal. Timely surgical intervention is required in those patients with high possibility of deterioration with conservative management.
Author contributions
Dr Andy C.M. Won participated in medical record review, writing, imaging, review. Dr Anthony Ethell participated in review.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Obtained.
References
- 1.Bailey R.E. Diagnosis and treatment of infectious mononucleosis. Am Fam Physician. 1994;49:879–888. [PubMed] [Google Scholar]
- 2.Farley D.R., Zietlow S.P., Bannon M.P., Farnell M.B. Spontaneous rupture of the spleen due to infectious mononucleosis. Mayo Clin Proc. 1992;67:846–853. doi: 10.1016/s0025-6196(12)60822-2. [DOI] [PubMed] [Google Scholar]
- 3.Lai P.K. Infectious mononucleosis: recognition and management. Hosp Pract. 1977;8:47–52. doi: 10.1080/21548331.1977.11707175. [DOI] [PubMed] [Google Scholar]
- 4.Rawsthorne G.B., Cole T.P., Kyle J. Spontaneous rupture of the spleen in infectious mononucleosis. Br J Surg. 1970;57:396–398. doi: 10.1002/bjs.1800570517. [DOI] [PubMed] [Google Scholar]
- 5.Patel J.M., Rizzolo E., Hinshaw J.R. Spontaneous subcapsular splenic hematomas as the only clinical manifestation of infection mononucleosis. JAMA. 1982;247:3243–3244. [PubMed] [Google Scholar]
- 6.Safran D., Bloom G.P. Spontaneous splenic rupture following infectious mononucleosis. Am Surg. 1990;56:601–605. [PubMed] [Google Scholar]
- 7.Konvolinka C.W., Wyatt D.B. Splenic rupture and infectious mononucleosis. J Emerg Med. 1989;7:471–475. doi: 10.1016/0736-4679(89)90148-0. [DOI] [PubMed] [Google Scholar]
- 8.Lambotte O., Debord T., Plotton N., Roue R. Splenic hematoma during infectious mononucleosis: non-operative treatment. Presse Med. 1998;27:209. [PubMed] [Google Scholar]
- 9.Rutkow I. Rupture of the spleen in infectious mononucleosis. Arch Surg. 1978;113:718–720. doi: 10.1001/archsurg.1978.01370180060007. [DOI] [PubMed] [Google Scholar]
- 10.Stockinger Z.T. Infectious mononucleosis presenting as spontaneous splenic rupture without other symptoms. Mil Med. 2003;168(9):722–724. [PubMed] [Google Scholar]


