Abstract
Introduction
A rarely reported entity, Waugh's syndrome is the association between intestinal malrotation and intussusception. We present a case of Waugh's syndrome encountered during a medical mission to a resource poor country.
Presentation of case
A 3-month-old female presented with septic shock and acute bowel obstruction secondary to intussusception and malrotation. She required aggressive resuscitation and emergent laparotomy, bowel resection, Ladd procedure and temporary ileostomy.
Discussion
First described in 1911, Waugh's syndrome has been rarely reported in the literature. We summarize a total of 54 cases of Waugh's syndrome that are reported in the literature to date.
The complicated but successful care of this patient reflects the severe outcome of any inadequate treatment of Waugh's syndrome and illustrates the importance of medical volunteers in developing countries.
Conclusion
As the relationship between malrotation and intussusception may be more frequent than recorded, surgeons must be aware that non-operative management of intussusception may be inadequate therapy.
Keywords: Waugh, Intussusception, Malrotation, Haiti, Ladd, Pediatric
1. Introduction
A rarely reported entity, Waugh's syndrome is the association between intestinal malrotation and intussusception. The only prospective study of Waugh's syndrome reports the association in 18 of 49 or 40% of patients with intussusception,1 implicating increased bowel mobility with increased potential for telescoping. Other authors contend that the association may be more common and unrecognized in patients who have had non-operative management of intussusception.2
We describe a case of Waugh's syndrome encountered during a medical mission to a resource poor country. Our patient presented with dehydration, ruptured colon, purulent peritonitis and septic shock, reflecting the potential severe outcome when Waugh's syndrome is inadequately treated, secondary to long-segment intussusception and bowel necrosis. We then discuss recent reports of the disease.
2. Presentation of case
A 3-month-old, 5.5 kg female developed acute abdominal distension, bilious vomiting, bloody diarrhea and fever. Her mother reported no prenatal care and normal spontaneous vaginal delivery at approximately full-term. The child had known allergies or prior illnesses.
After four days of intermittent intravenous hydration at a public hospital, she was transferred to a volunteer-run hospital for operative intervention. Pre-operatively, she appeared severely dehydrated with a sunken fontanelle and altered mental status. She had a severely distended abdomen with rebound tenderness but no palpable mass. An abdominal X-ray revealed distended small bowel and air-fluid levels. Because of limited resources, no further studies could be performed.
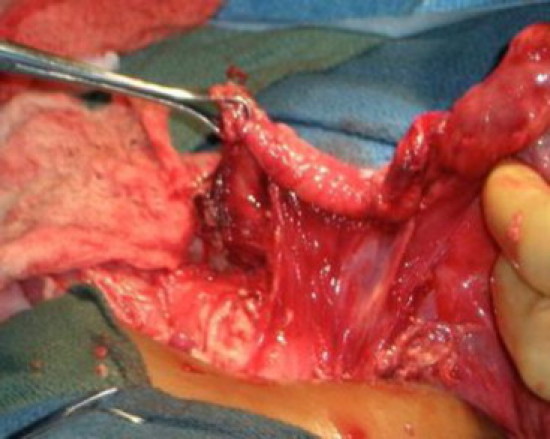
After aggressive hydration, broad-spectrum intravenous antibiotics and pressor support, the patient underwent midline laparotomy. Decompression by enterotomy was performed, and purulent contamination was noted. Ladd's bands were present as was a duodenojejunal flexure to the right of the superior mesenteric artery. The ileocecum had extensively telescoped into the descending colon, and manual reduction of the intussusception was performed. The cecum and right colon had no attachments to the posterior abdominal wall and were necrotic and ruptured. The distal ileum was also noted to be ischemic.
Ladd procedure, right hemicolectomy and extended distal ileal resection were performed. The remaining transverse colon was then secured to the posterior abdominal wall. After washout with normal saline, a diverting ileostomy was created (Fig. 1, Fig. 2).
Fig. 1.
Ladd's bands and a right-sided duodenojejunal junction, revealing the malrotation component of Waugh's syndrome.
Fig. 2.

Manual reduction of intussusception in a patient with Waugh's syndrome.
The patient recovered uneventfully. She remained healthy for four weeks, after which an ileo-colic anastomosis was created without complications.
3. Discussion
Waugh first described the association between intestinal malrotation and intussusception in 1911.3 In the only prospective study of the syndrome, Brereton et al. reported the association in 40% of 49 infants and established the eponym.1
In 2000, Breckon and Hadley described six infants with Waugh's syndrome and listed 39 cases documented in the literature before 1999.2 We identified two additional reports from the Osteopathic and Indian literature from 1971 and 1995, respectively.4, 5 Since 1999, five studies reported an additional six cases of infantile Waugh's syndrome (Table 1), and we present yet another incident.6, 7, 8, 9, 10 A total of 54 cases of infantile Waugh's syndrome have been reported in the literature to date.
Table 1.
Additional patients with infantile Waugh's syndrome documented in the literature. An addendum to cases previously reported by Breckon and Hadley.2
| Author | Journal | Year | Number of cases in report |
|---|---|---|---|
| Tabibi et al.4 | Journal of the AOA | 1971 | 1 |
| Sarin and Singh5 | Indian Pediatrics | 1995 | 1 |
| Inan et al.6 | Journal of Pediatric Surgery | 2004 | 2 |
| Rao and Kumar7 | Indian Journal of Pediatrics | 2005 | 1 |
| Lukong et al.8 | South Africa Journal of Surgery | 2007 | 1 |
| Al-Jahdali et al.9 | Journal of Pediatric Surgery | 2009 | 1 |
| Hardy et al.11 | The American Surgeon | 2011 | 1 |
Although discussed most often as a pediatric disease, Waugh's syndrome has also been reported in adults. Hsieh et al. described a 56-year old male with bowel obstruction and Waugh's syndrome.10 Interestingly, in this case, the obstructive symptoms were preceded by lifelong intermittent abdominal pain and vomiting, suggesting recurrent intussusception potentiated by increased bowel mobility.
For the majority of reported cases, Ladd procedure and manual reduction of the intussusception have been the treatments of choice. A laparoscopic approach to Waugh's syndrome has also recently been described.11 Because of prolonged illness, scant resources and limited access to surgeons, our patient presented in extremis and required aggressive resuscitation, bowel decompression, bowel resection and washout in addition to typical operative management. Also, the gross contamination of the peritoneum necessitated a temporary diverting ileostomy.
Many authors feel Waugh's syndrome may be more common but unrecognized since treatment by enema is often sufficient for reduction, and operative exploration is not performed.2 Our case provides further evidence of an association between malrotation and intussusception and the potential for severe illness if treatment is insufficient or delayed.
The successful treatment of this patient also illustrates the benefit of medical volunteers in developing countries. Without access to operative intervention at the public hospital, our patient's illness severely worsened. Volunteer opportunities including short-term options are widely available in numerous countries.
4. Conclusion
The relationship between intestinal malrotation and intussusception has been rarely reported in the literature. As the relationship may be more frequent than is recorded, surgeons must be aware that non-operative management of intussusception may be inadequate if a malrotation component is present.
The case presented demonstrates the intestinal necrosis and severe inflammatory response that may result from inadequately managed Waugh's syndrome. The case also reflects the benefit of volunteers in developing countries who may provide more prompt access to operative intervention.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient's mother for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Gerard Baltazar, D.O.—Primary contact, writer and analyzer.
Cyril Sahyoun, M.D.—Secondary contact, primary editor.
Jacklin Sime, M.S.-3—Assistant with writing, editing.
Marlon Bitar, M.D. and Jerry Bitar, M.D.—Directors at Hospital Bernard Mevs, Port-au-Prince, Haiti; secondary editors.
A.C. Rao, M.D.—Chairman of Surgery at Wyckoff Heights Medical Center, Brooklyn, NY, USA; secondary editor.
Acknowledgements
We express our sincere thanks to Hospital Bernard Mevs and Project Medishare for allowing the infrastructure of a humanitarian mission. Thanks to Dr. Thomas Anzelmo for his excellent anesthesia. Thanks also to Dr. Akella Chendrasekhar and Dr. Maria Lopez for their editorial input.
References
- 1.Brereton R.J., Taylor B., Hall C.M. Intussusception and malrotation in infants: Waugh's syndrome. British Journal of Surgery. 1986;73:55–57. doi: 10.1002/bjs.1800730123. [DOI] [PubMed] [Google Scholar]
- 2.Breckon V.M., Hadley G.P. Waugh's syndrome: a report of six patients. Pediatric Surgery International. 2000;16:370–373. doi: 10.1007/s003830000349. [DOI] [PubMed] [Google Scholar]
- 3.Waugh G.E. Referred penile pain in intussusception with notes of three cases. The Lancet. 1911;I:1492–1494. [Google Scholar]
- 4.Tabibi M., Thompson R.B., Gipe J.F., Dailey W.P. Malrotation syndrome with secondary intussusception: report of a case. Journal of the American Osteopathic Association. 1971;70:686–691. [PubMed] [Google Scholar]
- 5.Sarin Y.K., Singh V.P. Waugh's syndrome. Indian Pediatrics. 1995;32:108–109. [PubMed] [Google Scholar]
- 6.Inan M., Basaran U.N., Ayvaz S., Pul M. Waugh's syndrome: report of two cases. Journal of Pediatric Surgery. 2004;39:110–111. doi: 10.1016/j.jpedsurg.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 7.Rao P.L.N.G., Kumar V. Waugh's syndrome. Indian Journal of Pediatrics. 2005;72:E21–E22. doi: 10.1007/BF02760597. [DOI] [PubMed] [Google Scholar]
- 8.Lukong C.S., Maitama M.I., Aminu B., Mshelbwala P.M., Ameh E.A. Intestinal malrotation and midgut volvulus coexisting with intussusception. South African Journal of Surgery. 2007;45:30. [PubMed] [Google Scholar]
- 9.Al-Jahdali A., Lees G.M., Gay D.P., Al-Sairafi Colocolic intussusception in a preterm infant with intestinal malrotation. Journal of Pediatric Surgery. 2009;44:E17–E18. doi: 10.1016/j.jpedsurg.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Hsieh T.M., Sheen-Chen S.M., Lin C.C. Combination of adult intussusception and intestinal malrotation: an unusual presentation. Digestive Diseases and Sciences. 2008;53:3037–3039. doi: 10.1007/s10620-008-0530-5. [DOI] [PubMed] [Google Scholar]
- 11.Hardy D., Howell C., Hatley R., Pipkin W. Laparoscopic approach to Waugh's Syndrome. The American Surgeon. 2011;77:78–79. [PubMed] [Google Scholar]


