Abstract
Introduction
Mycotic pseudoaneurysms of native arteries are rare. Treatment involves arterial excision with or without revascularization.
Presentation of case
A 49-year-old diabetic man presented with a 4-month history of progressive left mid-thigh pain, associated with a pulsatile mass and fever. Clinically, he appeared to have a mycotic pseudoaneurysm, which was confirmed by computed tomography. The aneurysm was excluded from the circulation by an extra-anatomical bypass graft using autologous vein.
Conclusion
Native arterial mycotic pseudoaneurysms typically occur in immuno-compromised patients. They may be successfully treated using autologous vein bypass.
Discussion
Arterial infection is associated with immunosuppressive states and Staphylococcus aureus is the most commonly isolated organism in mycotic aneurysms. Also, Escherichia coli, Salmonella sp. and anaerobic species have been identified. Salmonella species are associated with mycotic aneurysms in the abdominal aorta and the use of autogenous vein grafts is the standard treatment for this condition. In lower extremities, autogenous conduits have been already used with good results of patency and freedom from re-infection. Endovascular treatment is a feasible approach in these situations, but there is not reports regarding long term results and this treatment is occasionally associated with prosthesis infection.
Keywords: Pseudoaneurysm, Femoral artery, Salmonella
1. Introduction
Mycotic pseudoaneurysm is a consequence of arterial disruption by bacterial infection.1 Native arterial infection in the absence of previous prostheses is rare. The intra-cranial arteries are the most common site of infection, followed by the aorta.2 Treatment generally involves arterial excision and in situ or extra-anatomical revascularization. The use of lower-extremity deep and superficial veins to perform bypasses is reported, with satisfactory results.3 Alternatively, endovascular stent deployment has low morbidity, but there are concerns regarding prosthesis infection and its consequences (i.e., embolization, hemorrhage, and sepsis).4, 5 We report a case of superficial femoral artery mycotic pseudo-aneurysm treated using extra-anatomical tunneled greater saphenous vein.
2. Case presentation
A 49-year-old diabetic man presented with a 4-month history of progressive left mid-thigh pain, associated with a mass and episodes of fever. He had developed general weakness and weight loss of 10 kg over the previous 6 months. There was no history of lower-extremity trauma or illicit drug use. Physical examination revealed a tender, warm, erythematous pulsatile mass in the medial left thigh. The femoral pulse was normal, but the popliteal, dorsalis pedis, and posterior tibial pulses were diminished. A computerized tomography (CT) angiogram was performed (Fig. 1) which confirmed the clinical impression of a mycotic pseudoaneurysm.
Fig. 1.
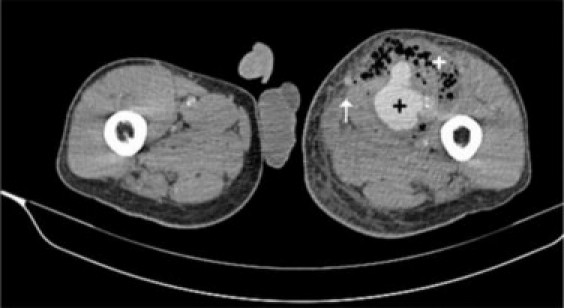
Preoperative CT. Note the large pseudoaneurysm (black cross) and the associated collection (white cross). The white arrow indicates greater saphenous vein.
Echocardiogram identified no cardiac vegetations. Duplex ultrasound examination of the contralateral greater saphenous vein (GSV) demonstrated a venous diameter of 4.0 mm, with no signs of phlebitis. Laboratory exams revealed leukocytosis and hepatitis/HIV serology were negative. Empirical piperacillin–tazobactam and vancomycin therapy was initiated.
Surgery was performed the morning after admission. The procedure was initiated by lateral aspect popliteal artery dissection, followed by common femoral artery isolation. The right GSV was harvested and a subcutaneous lateral thigh tunnel was created. Following systemic heparinisation, the origin of the superficial femoral artery (SFA) was ligated. The GSV was implanted in a non-reversed manner, and the valves were removed using Mills’ valvulotome after proximal anastomosis. Flow rate was estimated as 450 mL/min. The graft was tunneled and after distal anastomosis, another ligature was placed in the popliteal artery. After completing the bypass, the incisions were closed and bandaged. Drainage of the mass through another incision yielded a brownish air–liquid secretion that was sent for culture. During the drainage, SFA disruption was noted and others ligatures were necessary to control retrograde and collaterals hemorrhage, but blood transfusion was not necessary during the surgery or recovery.
The amplitudes of the popliteal and distal pulses were normal after the procedure and the patient reported improvement of the pain. Culture identified Salmonella sp. sensitive to ampicillin, ceftriaxone, and ciprofloxacin. Bypass patency was demonstrated in a control CT angiogram and no collections of pus were detected near the native SFA, which was surgically occluded (Fig. 2).
Fig. 2.

Postoperative CT angiogram (anterior and lateral view). Note the extra-anatomical position of the conduit in the left tight.
The patient was discharged one week postoperatively and was prescribed ciprofloxacin for a further 8 weeks. The patient was well clinically at discharge. There were no signs of infection at the 2-week follow-up visit and incisions appeared satisfactory. At 6 months follow-up, there were no signs of reinfection and a duplex ultrasound revealed that the bypass graft remains patent.
3. Discussion
Iatrogenic and traumatic injuries are the main causes of pseudoaneurysm.2 Mycotic aneurysms are rare, being associated with intimal disruption and bacterial invasion with arterial infection. Therefore, this condition most commonly occurs at sites of atherosclerotic plaques, aneurysms, and arterial bifurcations.6 Arterial infection is associated with immunosuppressive states such as HIV infection, diabetes mellitus and active cancer.7, 8
Staphylococcus aureus is the most commonly isolated organism in mycotic aneurysms, with Salmonella sp., Escherichia coli, and anaerobic species also identified.2 Salmonella sp. are associated with mycotic aneurysms in the thoracic and abdominal aorta, especially in patients with HIV infection. Independent of immunosuppressive disorders, a 6–8-week course of antibiotics is recommended and prophylactic cholecystectomy must be considered.9
Illicit drug use is implicated in the development of mycotic aneurysm. The condition occurs more commonly in the lower extremities if the patient has used their leg veins in an attempt to conceal needle puncture marks, or following previous thrombosis or sclerosis of the arm veins. In these patients, the clinical manifestations range from splinter hemorrhages to ischemic lesions caused by digital emboli.10
In the aorta and iliac arteries, native or prosthetic graft infections are generally treated by arterial or prosthesis excision, followed by revascularization using veins. Clagett et al.11 reported satisfactory results using deep and superficial veins for aortic reconstruction. In this situation, even extra-anatomical tunneled prostheses (e.g., axillo-bifemoral bypass graft) are associated with high rates of re-infection (10–23%) and of failure (35%).12
Superficial veins such as the greater saphenous vein have been used as grafts for treatment of mycotic aneurysm in other arterial segments, including the extra-cranial carotid artery.13 In native common femoral artery (CFA) infections, Klonaris et al.14 reported satisfactory results using the internal iliac artery (IIA). Their patients were intravenous drug users, and high-virulence bacteria were identified (E. coli and S. aureus). Surgical treatment involved dissection and removal of the IIA, which was then used as a patch. Schneider et al.15 described the use of in situ deep-vein grafts to treat superficial femoral artery pseudoaneurysm. Even when autologous vein is used, re-infection must be considered. Ehsan and Gibbons16 advocated the use of per-operative broad-spectrum antibiotics, followed by extensive arterial debridement and creation of another tunnel where possible. Another treatment option involves arterial ligation achieved by resection, but this type of surgery is associated with a 34% incidence of significant ischemia necessitating major amputation.2
Endovascular treatment of aortic mycotic aneurysm has been reported.17 This approach is favored because of the high morbidity and mortality associated with conventional surgical treatment, but stent infection, sepsis, and fatal complications must be considered.18 It is suggested that endograft stenting is safe following a course of antibiotics and negative blood cultures, but current management suggests its use only in high-risk surgical patients.17
In other studies, Klonaris et al.19 reported hybrid, staged management of arterial infections in 6 patients with anastomotic pseudoaneurysm who were treated by endograft placement, followed by secondary arterial debridement and vein-patch arterial closure. Wales et al.20 reported a similar technique for extra-cranial carotid artery pseudoaneurysm, but using an extra-anatomical greater saphenous vein bypass graft.
In summary, we present a case of a mycotic pseudoaneurysm of the superficial femoral artery treated successfully with extra-anatomic bypass using saphenous vein. We believe that the use of autologous vein is the best treatment option for arterial infection, and that creation of an extra-anatomical tunnel is associated with lower re-infection rates.
Conflict of interest
None.
Funding
None.
Ethical approval
Obtained.
Author contributions
M.V.M.C. – Conception and design, writing, final approval of the article and overall responsibility.
M.H.C. – Writing, critical revision of the article and final approval of the article.
D.P.S. – Data collection, critical revision of the article and final approval of the article.
Contributor Information
Marcus Vinícius Martins Cury, Email: mvmcury@hotmail.com.
Maysa Heineck de Campos, Email: maysacam@hotmail.com.
Diogo Pires dos Santos, Email: diogopsantos@gmail.com.
References
- 1.Osler W. The Gulstonian lectures on malignant endocarditis. Br Med J. 1885;1:467. doi: 10.1136/bmj.1.1262.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown S.L., Busuttil R.W., Baker J.D., Machleder H.I., Moore W.S., Barker W.F. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. J Vasc Surg. 1984;1:541–547. [PubMed] [Google Scholar]
- 3.Ehrenfeld W.K., Wilbur B.G., Olcott C.N., Stoney R.J. Autogenous tissue reconstruction in the management of infected prosthetic grafts. Surgery. 1979;85:82–92. [PubMed] [Google Scholar]
- 4.Riga C., Bicknell C., Jindal R., Cheshire N., Hamady M. Endovascular stenting of peripheral infected aneurysms: a temporary measure or definitive solution in high-risk patients. Cardiovasc Intervent Radiol. 2008;31:1228–1235. doi: 10.1007/s00270-008-9372-y. [DOI] [PubMed] [Google Scholar]
- 5.Simmental A., Johnson J.T., Horowitz M. Delayed complications of endovascular stenting for carotid blowout. Am J Otol. 2003;24:417–419. doi: 10.1016/s0196-0709(03)00088-7. [DOI] [PubMed] [Google Scholar]
- 6.Schneider J.A., Rheuban K.S., Crosby I.K. Rupture of postcoarctation mycotic aneurysms of the aorta. Ann Thorac Surg. 1979;27:185–190. doi: 10.1016/s0003-4975(10)63267-5. [DOI] [PubMed] [Google Scholar]
- 7.Botes K., Van Marle J. Surgical intervention for HIV related vascular disease. Eur J Vasc Endovasc Surg. 2007;34:390–396. doi: 10.1016/j.ejvs.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Bowden D.J., Hayes P.D., Sadat U., Choon See T. Mycotic pseudoaneurysm of the superficial femoral artery in a patient with cushing disease: case report and literature review. Vascular. 2009;17:163–167. doi: 10.2310/6670.2008.00060. [DOI] [PubMed] [Google Scholar]
- 9.Nseir B., Cutrona A.F. Salmonella-related mycotic pseudoaneurysm. Cleve Clin J Med. 2009;76:315–316. doi: 10.3949/ccjm.76a.08031. [DOI] [PubMed] [Google Scholar]
- 10.Benitez P.R., Newell M.A. Vascular trauma in drug abuse: patterns of injury. Ann Vasc Surg. 1986;1:175–181. doi: 10.1016/S0890-5096(06)61977-8. [DOI] [PubMed] [Google Scholar]
- 11.Clagett G.P., Bowers B.L., Lopez-Viego M.A., Rossi M.B., Valentine R.J., Myers S.I., et al. Creation of a neo-aortoiliac system from lower extremity deep and superficial veins. Ann Surg. 1993;218:239–249. doi: 10.1097/00000658-199309000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seeger J.M., Pretus H.A., Welborn M.B., Ozaki C.K., Flynn T.C., Huber T.S. Long-term outcome after treatment of aortic graft infection with staged extra-anatomic bypass grafting and aortic graft removal. J Vasc Surg. 2000;32:451–461. doi: 10.1067/mva.2000.109471. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Q., Duan Z.Q., Xin S.J., Wang X.W., Dong Y.T. Management of extracranial carotid artery aneurysms: 17 years’ experience. Eur J Vasc Endovasc Surg. 1999;18:162–165. doi: 10.1053/ejvs.1999.0876. [DOI] [PubMed] [Google Scholar]
- 14.Klonaris C., Katsargyris A., Papapetrou A., Vourliotakis G., Tsiodras S., Georgopoulos S., et al. Infected femoral artery pseudoaneurysm in drug addicts: the beneficial use of the internal iliac artery for arterial reconstruction. J Vasc Surg. 2007;45:498–504. doi: 10.1016/j.jvs.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Schneider J.R., Oskin S.I., Verta M.J., Jr. Superficial femoral vein graft interposition in situ repair for femoral mycotic aneurysm. Ann Vasc Surg. 2009;23(January–February (1)):147–149. doi: 10.1016/j.avsg.2007.12.023. [Epub 2008 May 27] [DOI] [PubMed] [Google Scholar]
- 16.Ehsan O., Gibbons C.P. A 10-year experience of using femoro-popliteal vein for revascularisation in graft and arterial infections. Eur J Vasc Endovasc Surg. 2009;38:172–179. doi: 10.1016/j.ejvs.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Kan C.D., Lee H.L., Yang Y.J. Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: a systematic review. J Vasc Surg. 2007;46:906–912. doi: 10.1016/j.jvs.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Therasse E., Soulez G., Cartier P., Passerini L., Roy P., Bruneau L., et al. Infection with fatal outcome after endovascular metallic stent placement. Radiology. 1994;192:363–365. doi: 10.1148/radiology.192.2.8029398. [DOI] [PubMed] [Google Scholar]
- 19.Klonaris C., Katsargyris A., Vasileiou I., Markatis F., Liapis C.D., Bastounis E. Hybrid repair of ruptured infected anastomotic femoral pseudoaneurysms: emergent stent-graft implantation and secondary surgical debridement. J Vasc Surg. 2009;49:938–945. doi: 10.1016/j.jvs.2008.10.063. [DOI] [PubMed] [Google Scholar]
- 20.Wales L., Kruger A.J., Jenkins J.S., Mitchell K., Boyne N.S., Walker PJ Mycotic carotid pseudoaneurysm: staged endovascular and surgical repair. Eur J Vasc Endovasc Surg. 2010;39(January):23–25. doi: 10.1016/j.ejvs.2009.10.012. [DOI] [PubMed] [Google Scholar]


