Abstract
INTRODUCTION
Most leg ulcers are vascular based. Only if vascular therapy fails other causes are considered. We report the case of a female with incapacitating leg ulcers caused by a rare condition which was only diagnosed after failing treatment.
PRESENTATION OF CASE
The female had an extensive previous history including diabetes, renal insufficiency and cardiovascular disease and presented with three large and painful ulcers on her left lower leg. Standard treatment with antibiotics, wound excision and additional treatment with hyperbaric oxygen were ineffective. One month post hospital-admission calciphylaxis cutis caused by renal failure induced secondary hyperparathyroidism was diagnosed. Surgical treatment by a parathyroidectomy induced rapid regeneration of the ulcers.
DISCUSSION
Our patient's vast comorbidity and previous history had expanded differential considerations causing a delay in diagnosis. Our patient's previous history led us to believe her ulcers were vascular based, however her chronic renal failure appeared responsible for her condition.
CONCLUSION
Although less probable than venous insufficiency and concomittant leg ulcers or other differential considerations, calciphylaxis cutis should be part of the differential diagnosis in any end stage renal disease-patient with unexplained ulcers as an effective therapy is readily available.
Keywords: Calciphylaxis, Secondary hyperparathyroidism, Parathyroidectomy, End stage renal disease, Calcific uraemic arteriolopathy, Ulcer
1. Introduction
Most leg ulcers are vascular based. Only when vascular therapy fails other causes are considered. We describe the case of a 55-year-old woman with multiple excruciatingly painful ulcers on her left lower leg who had a different cause of her ulcers than expected and therefore experienced a delay in treatment. After diagnosis, appropriate therapy resulted in rapid improvement of the ulcers.
2. Presentation of case
A 55-year-old woman with an extensive medical history including severe hypertension (HT), idiopathic pancreatitis, aortic valve replacement, dysplastic thyroid nodules, gout and an impressive viral history was seen at our hospital. Her pancreatitis was causative for diabetes mellitus type 2 (DM2) and her HT complicated by retinopathy, cardiomegaly and dialysis dependent end stage renal disease (ESRD) for which she had recceived a post-mortal kidney transplant 10 years earlier. The kidney transplant was stable but only moderately functioning. She additionally suffered from hirsutism, hyperlipidaemia and a benign multinodular struma.
The patient was referred to the surgical department at our hospital with three excruciatingly painful, pussing and necrotic ulcers on her left lower leg. The ulcers were up to six centimetres with bullae and erythema and had been present for 2–3 weeks. Amoxicillin started by the general practitioner had been without effect.
On admittance neither signs of infection of the leg were found nor were there any other findings on physical examination, especially no fever. Cultures were negative. Her previous history led us to believe the ulcers were of vascular origin, which was supported by laboratory and vascular investigations. The ulcers were attributed to be complications of her diabetes and initial wound treatment consisted of dressings, painkillers and additional wound debridement as the ulcers were demarquating and necrotic.
Our patient remained troubled by pain and the ulcers were not improving after one week as is shown in Fig. 1a.I. The ulcers were now diagnosed as diabetic ulcers not responding to treatment and she was started on hyperbaric oxygen treatment. Additional wound-biopsy and leg-angiography were nonconclusive.
Fig. 1.

Aspect of the ulcers. (a.I) Three months prior to surgery. (a.II) Two months post-surgery. (a.III) Two years post-surgery.
One month after admission our patient was still not improving and impatient while a clear cause of the ulcers remained absent. Differential considerations were as shown in Table 1. Cryoglobulinemia, lupus anticoagulans and antiphospholipid syndrome were excluded by laboratory investigations. Sickle cell anaemia had been excluded prior to our patient's kidney transplant. Chalk deposits which had remained unexplained in aforementioned biopsy (Fig. 2), could be explanatory for calciphylaxis cutis and therefore an X-ray was performed to search for chalk desposits and additionally exclude osteomyelitis.
Table 1.
Differential considerations.
| Cause | Disorder |
|---|---|
| Microangiopathy | DM, necrobiosis lipoidica |
| Metabolic | Gout, calciphylaxis cutis, pyoderma gangrenosum |
| Vasculitis | PAN, Wegener's granulomatosis, cryoglobulinaemia, SLE |
| Haematologic | Sickle cell anaemia, thalassemia |
| Other | Impetigo bullosa, erysipelas, osteomyelitis, antiphospholipid syndrome, lupus anticoagulans |
DM, diabetes mellitus; PAN, polyarteriitis nodosa; SLE, systemic lupus erythematosus.
Fig. 2.
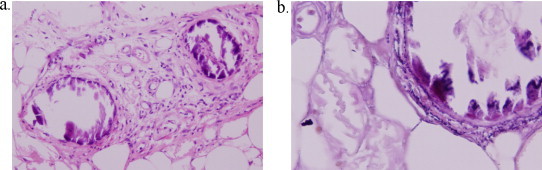
Microscopy view of ulcer border biopsies. (a) Vascular deposits, neovascularisation and fat degeneration due to necrosis (160× magnification, H&E stain). (b) Intravascular calcification on detailed recording (400× magnification, elastica-Von Gieson stain).
Surprisingly, the X-ray demonstrated marked calcifications of smaller blood vessels in the entire lower left leg and in combination with our patient's ESRD raised our suspicion of a secondary hyperparathyroidism (2HPT) and associated calcifying laesions. Parathyroid hormone (PTH) levels were 110.1 pmol/L (reference values 2–7 pmol/L) and the diagnosis calciphylaxis cutis caused by renal failure induced 2HPT was made.
Initial treatment consisted of a calcimimetic medical treatment and partial necrotectomy and punch graft biopsies. Unfortunately this resulted in a paradoxical spread of necrosis one month later and also a novel necrotic lesion formed at the punch graft upper leg donor site. Her PTH levels were rising (66.3 and 82.4 pmol/L one month and two months after initiation of medical therapy, respectively) and a multidisciplinary decision was made to perform parathyroidectomy. Our patient underwent a subtotal parathyroidectomy. Rapid wound regeneration was observed after parathyroidectomy as is demonstrated in Fig. 1a.II. Our patient felt reborn. Two years after surgery, our patient had no residual complaints regarding her leg ulcers, and wound healing was near complete as shown in Fig. 1a.III. Fig. 1 illustrates the drastic wound improvement as observed after parathyroidectomy.
3. Discussion
We report the case of a female with incapacitating leg ulcers caused by a rare condition which was only diagnosed after failing treatment. Our patient's previous history led us to believe her ulcers were vascular based, however her chronic renal failure appeared responsible. Manipulation of our patient's wounds resulted in a spread of necrosis. Indeed, iatrogenic skin trauma may predispose to calciphylactic lesions.1,2 Our patient experienced great benefit from parathyroidectomy.
Most leg ulcers are vascular based. Only if vascular therapy fails other causes are considered, as happened in our patient. Calciphylaxis cutis has been reported to occur in 0.1% of patients with an ulcus cruris.3 Most patients will therefore be diagnosed late. It is a rare but serious disorder with mortality rates reported up to 80%.4
Calciphylaxis cutis occurs in 1–4% of patients with ESRD or up to 5% of the dialysis population. Gold standard diagnostic strategy is pathological analysis, revealing intimal hyperplasia and medial calcification of small dermal and subcutaneous arterioles and arteries.4,5 A pathogenesis remains speculative but is probably multifactorial.6,7 Chronic renal failure, hypercalcaemia, hyperphophataemia, an elevated calcium-phosphate product and 2HPT all increase the risk of calciphylaxis cutis.8 Recent findings suggest a more complex pathogenesis due to the occurrence of calciphylaxis cutis in patients with normal and low parathyroid levels.5 Treatment is predominantly medical including calcimimetics and bisphosphonates to correct for hypercalcaemia and hyperphosphataemia.4
Another approach to correct the metabolic disturbances found in calciphylaxis is a parathyroidectomy. About 1–2% of patients with 2HPT receive a parathyroidectomy each year, 4% of these patients due to life threatening calciphylaxis.9 Parathyroidectomies have been described to enhance wound healing, prolong survival and additionally reduce pain, narcotic use and the number of amputations required.10,11 A meta-analysis conducted in 2001 reported a 65% survival rate for patients receiving parathyroidectomy compared to a 35% survival rate for patients not receiving surgery.6 These findings are in line with our own literature research describing case reports (January 2000–May 2011) for patients receiving a parathyroidectomy for calciphylaxis cutis caused by renal failure induced secondary hyperparathyroidism conducted with the help of a clinical librarian. We found a 57.8% improvement rate and 25.0% non-improvement rate (n = 64) after parathyroidectomy as is shown in Table 2.
Table 2.
Literature search of case reports describing outcome after parathyroidectomy for secondary hyperparathyroidism induced calciphylaxis cutis.
| Reference | No.a | Procedure | Improved | Not improved |
|---|---|---|---|---|
| Yip12 | 1 | 1 NOS | 1 | |
| Sulkova13 | 1 | 1 subtotal | 1 | |
| Wahab14 | 1 | 1 total & autoTx | 1 | |
| Couto15 | 1 | 1 total | 1 | |
| Acher-Chenebaux16 | 1 | 1 subtotal | 1 | |
| Duffy17 | 6 | 4 subtotal 2 total | 6 | |
| Paskalev18 | 1 | 1 subtotal | 1 | |
| Bardsley19 | 3 | 3 subtotal | 2 | 1 |
| Matsuoka20 | 6 | 6 total & autoTx | 3 | 3b |
| Galimberti21 | 3 | 3 subtotal | 1 | 2 |
| Oikawa22 | 1 | Parathyroidectomy NOS | 1 | |
| Arch-Ferrer23 | 23 | 12 total & autoTx 11 subtotal |
11 | 2c |
| Bahar G24 | 1 | 1 subtotal | 1 | |
| Sefer S25 | 1 | 1 total | 1 | |
| Girotto10 | 6 | 6 subtotal | 6 | |
| Kang26 | 7 | 5 subtotal 2 total & autoTx |
6 1 NOS |
|
| Patetsios27 | 1 | 1 total & autoTx | 1 | |
| TOTAL | 64 | 36 subtotal (56.3%) 22 total & autoTx (34.4%) 4 total (6.3%) 2 NOS (3.1%) |
37 improved (57.8%) 16 not improved (25.0%) 11 other (17.2%) |
|
Pubmed search terms: (secondary hyperparathyroidism) AND (calcification OR calciphylaxis OR calcinosis) AND (cutis OR dermis OR skin OR dermal OR dermopathy OR dermatological OR cutaneous). Limits: English, 2000–May 2011
Number of patients receiving surgical treatment. NOS, not otherwise specified.
One improved patient, and one non-improved patient required amputation.
Seven patients died of unrelated causes. Three patients were lost to follow up.
4. Conclusion
Calciphylaxis cutis caused by renal failure induced 2HPT is a rare but serious condition and should be integrated in a differential diagnosis in any patient with renal failure and unexplained leg ulcers not improving after vascular interventions as an effective therapy is readily available.
Consent
Vocal consent was acquired from the patient prior to writing this case report. Unfortunately, upon submission of this case report the patient had died. We were therefore unable to obtain written consent.
Conflict of interest statement
None of the authors has any financial arrangements or potential conflicts of interest related to this article.
Funding
None.
Ethical approval
Studies on patients or volunteers require ethics committee approval and fully informed written consent which should be documented in the paper.
Author contributions
L.B. van Rijssen—data acquisition and analysis, article drafting, article revision.
Dr. E.E.A. Brenninkmeijer—data acquisition, article revision.
Dr. E.J.M. Nieveen van Dijkum—interpretation of data, article drafting, article revision and final approval.
References
- 1.Meissner M., Gille J., Kaufmann R. Calciphylaxis: no therapeutic concepts for a poorly understood syndrome? J Dtsch Dermatol Ges. 2006;4:1037–1044. doi: 10.1111/j.1610-0387.2006.06127.x. [DOI] [PubMed] [Google Scholar]
- 2.Raymond C.B., Wazny L.D. Sodium thiosulfate, bisphosphonates, and cinacalcet for treatment of calciphylaxis. Am J Health Syst Pharm. 2008;65:1419–1429. doi: 10.2146/ajhp070546. [DOI] [PubMed] [Google Scholar]
- 3.Sick I., Ruzicka T. The many faces of chronic leg ulcers. Dtsch Med Wochenschr. 2010;135:1440–1445. doi: 10.1055/s-0030-1262431. [DOI] [PubMed] [Google Scholar]
- 4.Rogers N.M., Coates P.T. Calcific uraemic arteriolopathy: an update. Curr Opin Nephrol Hypertens. 2008;17:629–634. doi: 10.1097/MNH.0b013e32830f4566. [DOI] [PubMed] [Google Scholar]
- 5.Cordova K.B., Oberg T.J., Malik M., Robinson-Bostom L. Dermatologic conditions seen in end-stage renal disease. Semin Dial. 2009;22:45–55. doi: 10.1111/j.1525-139X.2008.00534.x. [DOI] [PubMed] [Google Scholar]
- 6.Hafner J., Keusch G., Wahl C., Sauter B., Hü rlimann A., von Weizsäcker F. Uremic small-artery disease with medial calcification and intimal hyperplasia (so-called calciphylaxis): a complication of chronic renal failure and benefit from parathyroidectomy. J Am Acad Dermatol. 1995;33:954–962. doi: 10.1016/0190-9622(95)90286-4. [DOI] [PubMed] [Google Scholar]
- 7.Mathur R.V., Shortland J.R., el-Nahas A.M. Calciphylaxis. Postgrad Med J. 2001;77:557–561. doi: 10.1136/pmj.77.911.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hussein M.R., Ali H.O., Abdulwahed S.R., Argoby Y., Tobeigei F.H. Calciphylaxis cutis: a case report and review of literature. Exp Mol Pathol. 2009;86:134–135. doi: 10.1016/j.yexmp.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Pitt S.C., Sippel R.S., Chen H. Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am. 2009;89:1227–1239. doi: 10.1016/j.suc.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girotto J.A., Harmon J.W., Ratner L.E., Nicol T.L., Wong L., Chen H. Parathyroidectomy promotes wound healing and prolongs survival in patients with calciphylaxis from secondary hyperparathyroidism. Surgery. 2001;130:645–650. doi: 10.1067/msy.2001.117101. [DOI] [PubMed] [Google Scholar]
- 11.Milas M., Weber C.J. Near-total parathyroidectomy is beneficial for patients with secondary and tertiary hyperparathyroidism. Surgery. 2004;136:1252–1260. doi: 10.1016/j.surg.2004.06.055. [DOI] [PubMed] [Google Scholar]
- 12.Yip S.L., Koo S.C., Yen C.H., Mak K.H. Calcinosis cutis of the hand in a renal failure patient: a case report. J Orthop Surg (Hong Kong) 2011;19:113–115. doi: 10.1177/230949901101900126. [DOI] [PubMed] [Google Scholar]
- 13.Sulkova S.D., Valek M. Skin wounds associated with calciphylaxis in end-stage renal disease patients on dialysis. Nutrition. 2010;26:910–914. doi: 10.1016/j.nut.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Wahab M.A., Al K.F. Calciphylaxis after parathyroidectomy in chronic renal failure. Saudi J Kidney Dis Transpl. 2008;19:854–860. [PubMed] [Google Scholar]
- 15.Couto F.M., Chen H., Blank R.D., Drezner M.K. Calciphylaxis in the absence of end-stage renal disease. Endocr Pract. 2006;12:406–410. doi: 10.4158/EP.12.4.406. [DOI] [PubMed] [Google Scholar]
- 16.Acher-Chenebaux A., Maillard H., Potier A., Nzeyimana H., Cazals F., Celerier P. Cutaneous calciphylaxis treated by autologous keratinocytes graft and subtotal parathyroidectomy. Ann Dermatol Venereol. 2006;133:260–263. doi: 10.1016/s0151-9638(06)70893-6. [DOI] [PubMed] [Google Scholar]
- 17.Duffy A., Schurr M., Warner T., Chen H. Long-term outcomes in patients with calciphylaxis from hyperparathyroidism. Ann Surg Oncol. 2006;13:96–102. doi: 10.1245/ASO.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 18.Paskalev D., Kircheva A. Cutaneous calciphylaxis in a haemodialysis patient. J Wound Care. 2005;14:312. doi: 10.12968/jowc.2005.14.7.26806. [DOI] [PubMed] [Google Scholar]
- 19.Bardsley S., Coutts R., Wilson C. Calciphylaxis and its surgical significance. ANZ J Surg. 2005;75:356–359. doi: 10.1111/j.1445-2197.2005.03354.x. [DOI] [PubMed] [Google Scholar]
- 20.Matsuoka S., Tominaga Y., Uno N., Goto N., Sato T., Katayama A. Calciphylaxis: a rare complication of patients who required parathyroidectomy for advanced renal hyperparathyroidism. World J Surg. 2005;29:632–635. doi: 10.1007/s00268-005-7514-9. [DOI] [PubMed] [Google Scholar]
- 21.Galimberti R.L., Farias E.R., Parra I.H., Algranati L., Kowalczuk A., Imperiali N. Cutaneous necrosis by calcific uremic arteriolopathy. Int J Dermatol. 2005;44:101–106. doi: 10.1111/j.1365-4632.2005.02169.x. [DOI] [PubMed] [Google Scholar]
- 22.Oikawa S., Osajima A., Tamura M., Murata K., Yasuda H., Anai H. Development of proximal calciphylaxis with penile involvement after parathyroidectomy in a patient on hemodialysis. Intern Med. 2004;43:63–68. doi: 10.2169/internalmedicine.43.63. [DOI] [PubMed] [Google Scholar]
- 23.Arch-Ferrer J.E., Beenken S.W., Rue L.W., Bland K.I., Diethelm A.G. Therapy for calciphylaxis: an outcome analysis. Surgery. 2003;134:941–944. doi: 10.1016/j.surg.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Bahar G., Mimouni D., Feinmesser M., David M., Popovzer A., Feinmesser R. Subtotal parathyroidectomy: a possible treatment for calciphylaxis. Ear Nose Throat J. 2003;82:390–393. [PubMed] [Google Scholar]
- 25.Sefer S., Trotic R., Degoricija V., Vrsalovic M., Ratkovic-Gusic I., Kes P. Healing of skin necrosis and regression of anticardiolipin antibodies achieved by parathyroidectomy in a dialyzed woman with calcific uremic arteriolopathy. Croat Med J. 2001;42:679–682. [PubMed] [Google Scholar]
- 26.Kang A.S., McCarthy J.T., Rowland C., Farley D.R., van Heerden J.A. Is calciphylaxis best treated surgically or medically? Surgery. 2000;128:967–971. doi: 10.1067/msy.2000.110429. [DOI] [PubMed] [Google Scholar]
- 27.Patetsios P., Bernstein M., Kim S., Mushnick R., Alfonso A. Severe necrotizing mastopathy caused by calciphylaxis alleviated by total parathyroidectomy. Am Surg. 2000;66:1056–1058. [PubMed] [Google Scholar]


