Abstract
Background:
There are only a few effective treatment options currently available for treatment-refractory obsessive compulsive disorder (OCD). The supplementary motor area (SMA) has been reported to play an important role in the pathophysiology of OCD. Functional neuroimaging studies indicate that OCD is associated with increased activity in the SMA, caudate nucleus, and anterior cingulate gyrus. Novel treatment strategies like repetitive transcranial magnetic stimulation (rTMS) have been proposed for OCD refractory to standard treatments. These clinic-based data report on the efficacy of rTMS in medication-resistant OCD.
Materials and Methods:
Twelve right-handed persons with medication-resistant OCD were administered rTMS as an add-on treatment. Stimulation was given at 1 Hz for 10 seconds followed by 15 seconds pause and 100 trains of stimulus over the SMA per session for 5 days in a week. Assessments were done on yale brown obsessive compulsive scale (Y-BOCS) at baseline and at the end of rTMS intervention.
Results:
The subjects had a mean age of 33.17±12.74 years. Mean scores on Y-BOCS were 26.17 at baseline and 17.17 at the end of treatment, reflecting significant improvement. The subjects did not report any significant side effects except one person with known bipolar illness, who developed manic symptoms after the 3rd session of the rTMS.
Conclusions:
Low-frequency rTMS over the SMA appears a promising treatment strategy as an add-on treatment in treatment-refractory patients of OCD.
Keywords: Obsessive compulsive disorder, repetitive transcranial magnetic stimulation, supplementary motor area
INTRODUCTION
Obsessive compulsive disorder (OCD) is a debilitating condition with a prevalence of 2–3%.[1,2] Even with recent advancements in psychopharmacology, 40–60% of the patients with OCD do not show satisfactory response to the standard treatments. Even if the response occurs, it is often delayed by 4–8 weeks.[3] Low rate of response to medication has led to several pharmacological and non-pharmacological treatment strategies to augment the standard treatment. These include using another anti-obsessional agent, cognitive–behavioral therapy, lithium carbonate, buspirone, low doses of atypical antipsychotics, psychosurgery repetitive transcranial magnetic stimulation (rTMS) and deep brain stimulation.[4,5]
rTMS is a non-invasive technique that delivers magnetic pulses to the underlying cortex by stimulating coil applied directly to the scalp. The potential of rTMS to influence subcortical neurons has been well established by imaging studies.[6] The pulse produces an intense magnetic field that causes depolarization of neurons underlying the magnetic coil. The depolarization of neurons cascades a series of neurophysiological changes.
There have been some studies on the use of rTMS in resistant OCD with varying outcomes depending on the site of cortical stimulation.[7–16] However, because of variability in the stimulation site, limited number of studies and different parameters used for rTMS stimulations, it is difficult to draw definitive conclusions about its clinical efficacy and site of stimulations. Hence, we need more clinical and research data to draw some conclusion about the site of stimulation for rTMS treatment in persons suffering from OCD.
Neurobiological and neurophysiological models of OCD have linked obsessive and compulsive symptoms to deficits of response control and inhibition.[17,18] Although the neural basis of inhibitory control deficits in OCD remains largely unknown, functional magnetic resonance imaging (fMRI) and magnetic resonance spectroscopy (MRS) studies on OCD patients have reported hyperactivation of the medial frontal cortex (MFC) and supplementary motor area (SMA).[19] Available data show positive effects after stimulation of the right and left prefrontal cortex and of the SMA, with response rates ranging from 25 to 60% in treatment-refractory OCD patients.[7,10–12,16]
This paper reports on the efficacy of rTMS as an add-on treatment in treatment-refractory patients with OCD.
MATERIALS AND METHODS
The Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, is equipped with rTMS service for clinical and research purpose, where patients for various psychiatric disorders are given rTMS, 5 days a week. These clinic-based data reflect the results of rTMS given to a group of patients with treatment-resistant OCD, who received treatment in the rTMS room during the period October 2009 to April 2010. Diagnoses of OCD were made as per International Classification of Disease-10 criteria. Drug resistance was defined as nonresponse to two anti-obsessional drugs for 6–8 weeks with adequate dose. Informed consent is taken as a routine procedure before the treatment is administered. Thumb movement visualization method was used to determine the resting motor threshold by stimulating the left primary motor cortex. Determination of motor threshold required 5–10 minutes at the first treatment session and lesser time on subsequent days because the location had been measured and marked. The subjects were administered low-frequency (1 Hz) rTMS over SMA corresponding with Fz (SMA) of International 10–20 EEG System. rTMS was administered using a Magstim Rapid[2] Brain Stimulator (Magstim Company Ltd, Whiteland, London) with a focal 70-mm figure 8-shaped coil. All rTMS stimulations were administered in the specially designed rTMS room with electronically adjusted chair. Patients were laid supine with the head elevated on a head rest. rTMS sessions were given for five consecutive days in a week for two consecutive weeks. rTMS protocol for each patient consisted of 15 treatment sessions of 1 Hz repetitive stimulus over the SMA with 100% of active motor threshold. The stimulus was given for 10 seconds followed by 15 seconds pause. One hundred trains of stimulus were given per session. One thousand pulses were given in each session. Subjects continued on their medications which were not changed during the period they were receiving rTMS. All patients were evaluated by yale brown obsessive compulsive scale (Y-BOCS) at baseline and at the end of 15th session by the psychiatrist. In accordance with the safety criteria for rTMS, subjects with a history of seizure or bearing pacemakers, metal implants, implanted medical pumps, metal clips inside the skull and pregnant women are not given rTMS.
RESULTS
These clinical data report on 12 patients (5 males and 7 females) with resistant OCD who received rTMS treatment during the period October 2009 to April 2010. Mean age of the subjects was 33.17±12.74 (range 18–55) years. A significant decline was observed in the mean Y-BOCS scores from 26.17 to 17.17 after rTMS treatment for 2 weeks [Table 1]. Comparison of obsessional subtotal and compulsion subtotal scores before and after the rTMS intervention also reflected statistically significant difference in the mean value [Figure 1]. During the rTMS intervention, one subject developed manic symptoms after 3rd rTMS session and was excluded from the sample. The patient who developed manic symptoms had history suggestive of bipolar illness and was maintaining well on lithium as mood stabilizer. No troublesome side effects were reported with rTMS intervention during and after the treatment. Two patients reported moderate pain and feeling of discomfort at the stimulation site.
Table 1.
Important clinical characteristics of sample
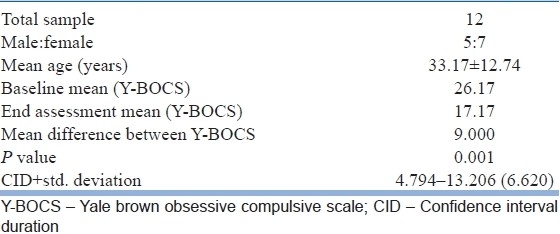
Figure 1.
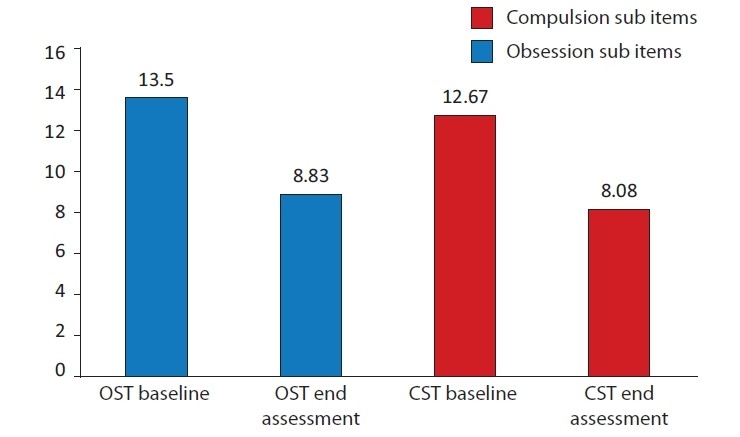
Comparison of obsession subtotals (OST) score and compulsion subtotals (CST) score before and after rTMS with Y-BOCS
DISCUSSION
There is no standardized area of stimulation identified for rTMS intervention in patients suffering from OCD.
There have been few studies of rTMS intervention in OCD.[7–12,13–15] The results were promising but inconclusive for several reasons. There was a lack of uniformity in the studies related to the site of stimulation, stimulation parameters and treatment duration. Till date, no uniform target area has been identified for rTMS stimulation in OCD, as in depression, where left prefrontal cortex is considered a standard site for rTMS as approved by the food and drug administration. Some workers have reported improvement in symptomatology, when orbitofrontal cortex (OFC) and SMA were the targets.[15,16] Stimulation in both right as well as left prefrontal cortex has also not shown positive results.[9–11,13,14] In the present study, we stimulated the SMA because of imaging evidence reflecting hyperactivation of the MFC and SMA in patients suffering from OCD.[19]
In a recent study, Mantovani et al. in 2010 have reported a response rate of 67% in OCD by rTMS stimulation in the SMA. Improvement seen in our OCD patients with rTMS stimulation in the SMA is comparable with this study.
These clinical data might be contributory for determining the area of stimulation in persons suffering from OCD. The sample of our data is well characterized and drug resistant with stable therapy, and no drug treatment was changed during the study period. We observed clinically significant improvement in OCD symptoms in our patients, with benefits lasting up to 4 weeks after the end of rTMS treatment in 11 patients and approximately 5 months in one patient.
However, there are several limitations of this report. Being a clinic-based study drawing sample from the clinic population, the study was open in nature with no control group. Sample size was also small. We could not also be very confident about the exact site of stimulation because no neuronavigation methods were used.
Controlled studies are required with larger sample size using neuronavigation techniques to confirm the efficacy of rTMS in patients with OCD.
CONCLUSION
This clinical data reflect that low-frequency rTMS over SMA appears to be useful for persons suffering from treatment-resistant OCD. All subjects tolerated rTMS intervention without any marked side effects. Approximately 50% persons with resistant OCD had shown statistically significant decrease of the Y-BOCS scores after the rTMS intervention. The report supports further investigation into the potential therapeutic applications of rTMS in resistant OCD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Karno M, Golding JM, Sorenson SB, Burnam MA. The epidemiology of obsessive compulsive disorder in five US communities. Arch Gen Psychiatry. 1988;45:1094–9. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- 2.Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, et al. The cross national epidemiology of obsessive compulsive disorder. J Clin Psychiatry. 1994;55(suppl):5–10. [PubMed] [Google Scholar]
- 3.Pallanti S, Hollander E, Bienstock C, Koran L, Leckman J, Marazziti D, et al. Treatment non-response in OCD: Methodological issues and operational definitions. Int J Neuropsychopharmacol. 2002;5:181–91. doi: 10.1017/S1461145702002900. [DOI] [PubMed] [Google Scholar]
- 4.Albert U, Bergesio C, Pessina E, Maina G, Bogetto F. Management of treatmentresistant obsessive-compulsive disorder: Algorithms for pharmacotherapy. Panminerva Med. 2002;44:83–91. [PubMed] [Google Scholar]
- 5.Ipser JC, Carey P, Dhansay Y, Fakier N, Seedat S, Stein DJ. Pharmacotherapy augmentationstrategies in treatment-resistant anxiety disorders. Cochrane Database Syst Rev. 2006;4:CD005473. doi: 10.1002/14651858.CD005473.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Husain FT, Nandipati G, Braun AR. Stimulating transcranial magnetic stimulation during PET with a large-scale neural network model of the prefrontal cortex and the visual system. Neuroimage. 2002;15:58–73. doi: 10.1006/nimg.2001.0966. [DOI] [PubMed] [Google Scholar]
- 7.Mantovani A, Lisanby SH, Pieraccini F, Ulivelli M, Castrogiovanni P, Rossi S. Repetitive Transcranial magnetic stimulation (rTMS) in the treatment of obsessive compulsive disorder (OCD) and Tourette's syndrome (TS) Int J Neuropsychopharmacol. 2006;9:95–100. doi: 10.1017/S1461145705005729. [DOI] [PubMed] [Google Scholar]
- 8.Martin JL, Barbanoj MJ, Pérez V, Sacristán M. Transcranial magnetic stimulation for treatment of obsessive-compulsive disorder. Cochrane Database Syst Rev. 2003;3:CD003387. doi: 10.1002/14651858.CD003387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg BD, George MS, Martin JD, Benjamin J, Schlaepfer TE, Altemus M, et al. Effect of prefrontal transcranial magnetic stimulation in obsessive-compulsive disorder: A preliminary study. Am J Psychiatry. 1997;154:867–9. doi: 10.1176/ajp.154.6.867. [DOI] [PubMed] [Google Scholar]
- 10.Alonso P, Pujol J, Cardoner N, Benlloch L, Deus J, Menchón JM, et al. Right prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: A double blind, placebo-controlled study. Am J Psychiatry. 2001;158:1143–5. doi: 10.1176/appi.ajp.158.7.1143. [DOI] [PubMed] [Google Scholar]
- 11.Sachdev PS, McBride R, Loo CK, Mitchell PB, Malhi GS, Croker VM. Right versus left prefrontal transcranial stimulation for obsessive-compulsive disorder: A preliminary investigation. J Clin Psychiatry. 2001;62:981–4. doi: 10.4088/jcp.v62n1211. [DOI] [PubMed] [Google Scholar]
- 12.Prasko J, Pasková B, Záleský R, Novák T, Kopecek M, Bares M, et al. The effect of repetitive transcranial magnetic stimulation (rTMS) on symptoms in obsessive compulsive disorder: A randomized, double-bind, sham-controlled study. Neuroendocrinol Lett. 2006;27:327–32. [PubMed] [Google Scholar]
- 13.Sachdev PS, Loo CK, Mitchell PB, McFarquhar TF, Malhi GS. Repetitive Transcranial magnetic stimulation for the treatment of obsessive-compulsive disorder: A double-blind controlled investigation. Psychol Med. 2007;37:1645–9. doi: 10.1017/S0033291707001092. [DOI] [PubMed] [Google Scholar]
- 14.Sarkhel S, Sinha VK, Praharaj SK. Adjunctive high-frequency right prefrontal repetitive transcranial magnetic stimulation (rTMS) was not effective in obsessive-compulsive disorder but improved secondary depression. J Anxiety Disord. 2010;24:535–9. doi: 10.1016/j.janxdis.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Mantovani A, Simpson HB, Fallon BA, Rossi S, Lisanby SH. Randomized sham-controlled trial of repetitive transcranial magnetic stimulation in treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2010;13:217–27. doi: 10.1017/S1461145709990435. [DOI] [PubMed] [Google Scholar]
- 16.Ruffini C, Locatelli M, Lucca A, Benedetti F, Insacco C, Smeraldi E. Augmentation effect of repetitive transcranial magnetic stimulation over the orbitofrontal cortex in drug-resistant obsessive-compulsive disorder patients: A controlled investigation. Prim Care Companion J Clin Psychiatry. 2009;11:226–30. doi: 10.4088/PCC.08m00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bannon S, Gonsalvez CJ, Croft RJ, Boyce PM. Response inhibition deficits in obsessive-compulsive disorder. Psychiatry Res. 2002;110:165–74. doi: 10.1016/s0165-1781(02)00104-x. [DOI] [PubMed] [Google Scholar]
- 18.Muller J, Roberts JE. Memory and attention in obsessive-compulsive disorder: A review. J Anxiety Disord. 2005;19:1–28. doi: 10.1016/j.janxdis.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Yucel M, Harrison BJ, Wood SJ, Fornito A, Wellard RM, Pujol J, et al. Functional and biochemical alterations of the medial frontal cortex in obsessive-compulsive disorder. Arch Gen Psychiatry. 2007;64:946–55. doi: 10.1001/archpsyc.64.8.946. [DOI] [PubMed] [Google Scholar]


