Abstract
A 9-year-old girl presented to the Child Guidance Clinic with clinical features suggestive of depressive episode of 1 week duration. There was history of short febrile illness 3 weeks prior to the onset of the depressive symptoms. MRI scan of brain showed features of acute disseminated encephalomyelitis.
Keywords: Acute disseminated encephalomyelitis, children, depressive episode
INTRODUCTION
Acute disseminated encephalomyelitis (ADEM) is an acute demyelinating disorder of the central nervous system (CNS) which follows an infection or vaccination.[1] The hallmark of ADEM is the rapid development of a focal or multifocal neurological disorder with peak dysfunction occurring in several days.[2–4] The diagnosis is based on the acute onset of neurologic signs and symptoms together with magnetic resonance imaging (MRI) evidence of multifocal, hyper-intense lesions on fluid-attenuated inversion recovery (FLAIR) and T2-weighted images.[2,4]
Even though psychiatric manifestations are known to occur in ADEM, depressive episode as the initial manifestation of ADEM is rare.[5] Severe depression as an initial symptom of acute disseminated encephalomyelitis in an elderly patient was reported in the past.[6] To the best of our knowledge depressive disorder as the initial manifestation in children has not been reported. We report the case of ADEM presenting as depressive episode in a child.
CASE REPORT
A 9-year-old girl was brought to the Child Guidance Clinic at the Department of Pediatrics at Medical College, Calicut, Kerala, with history of acute onset of change in behavior of 1 week duration. She became withdrawn and was not interested in play and other pleasurable activities. She was very irritable getting angry easily. Her speech was markedly reduced and she occasionally cried for no apparent reason. She also had severe loss of appetite and exhibited disturbed sleep. She had a non-specific febrile illness 3 weeks prior to the onset of the behavior change. The fever lasted for 1 week and there was no associated head ache, vomiting, skin rash, or diarrhea. The illness subsided with out-patient treatment. There was no history of any immunizations in the recent past. She was born of non-consanguineous marriage and her developmental mile stones were normal. She was going to school normally and had average academic performance.
On mental status examination, the child was cooperative for interview. Her psychomotor activity was reduced. Her speech was relevant and coherent with prolonged reaction time. Her mood was depressed. There were no delusions or hallucinations. Primary mental functions were intact. On nervous system examination, motor system, sensory system, and reflexes were within normal limits. There were no cerebellar or meningeal signs. A clinical diagnosis of moderate depressive episode (F-32-1) as per ICD 10 diagnostic criteria[7] was made. The child was started on fluoxetine 10 mg per day.
Routine blood and urine examination was normal. CSF study was also normal. EEG showed frontal beta dominance and mild slowing of the background activity. MRI of brain showed hyperintense signals in T2 and FLAIR sequences involving bilateral corona radiata, gangliocapsular midbrain, middle cerebellar peduncle, and medial cerebellar hemispheres. The MR images were consistent with ADEM Figures 1 and 2.
Figure 1.
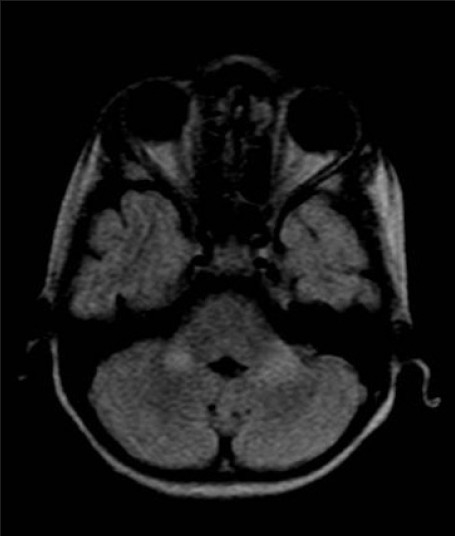
MR image (FLAIR) showing hyper-intense lesions involving bilateral middle cerebellar peduncles
Figure 2.
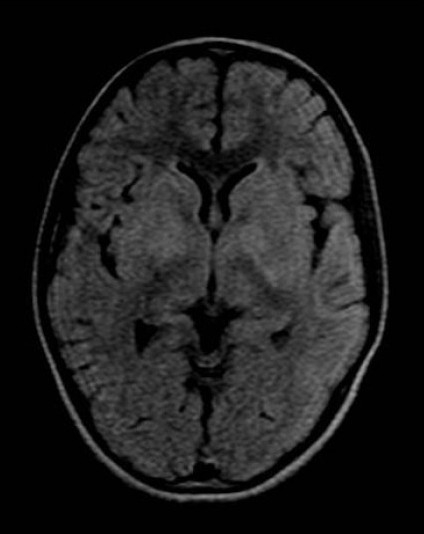
MR image (FLAIR) showing hyperintense lesions involving bilateral caudate and lentiform nuclei and subtle hyperintensity involving left frontal lobe grey matter
After obtaining the MRI report, a diagnosis of moderate depressive episode secondary to acute disseminated encephalomyelitis (ADEM) was made and the child was treated with methyl prednisolone 30 mg/kg per day for 3 days. There was dramatic improvement in symptoms after the treatment with methylprednisolone. She was switched over to oral prednisolone 2 mg/kg/day which was given for 2 weeks and gradually tapered off.
DISCUSSION
The clinical features in this child were consistent with the diagnosis of moderate depressive episode except for the duration criteria.[7] The MRI images were consistent with the diagnosis of ADEM. Non-specific upper respiratory infection or febrile illness most commonly precedes ADEM by an interval of 2 to 28 days.[2,4] In our child there was non-specific febrile illness 3 weeks prior to the onset of the depressive symptoms. There was also dramatic improvement after starting treatment with methylprednisolone. Hence, the diagnosis of ADEM presenting as depressive episode was made in this child.
Neuropsychiatric manifestations are not uncommon in ADEM.[6,8] The neuropsychiatric symptoms described include aggression, agitation, auditory hallucinations, catatonic waxy flexibility, delusions, disorganized behaviour, disorganized thinking, disorientation, inappropriate laughter, hostility, irritability, mania, mood lability, mutism, paranoia, and personality change.[6,9] Acute psychotic disorder occurring in ADEM has been reported in the past.[10] We have reported from the same center two children with ADEM who presented with acute psychotic disorder.[11] Psychiatric symptoms can occur as the initial presentation of ADEM before the occurrence of neurological manifestations or may be associated with neurological manifestations.[5,6] The psychiatric symptoms may persist after subsidence of the neurological symptoms or there can be total recovery after treatment with steroids.[5] In the present case, the child recovered after treatment with methylprednisolone.
The case is reported to emphasize the point that psychotic disorder or depressive disorder occurring in a child for the first time warrants detailed evaluation to rule out organic causes. ADEM is one of the organic disorders that should be considered in such situations especially if the psychotic or depressive symptoms began after an episode of febrile illness.
ACKNOWLEDGMENT
We thank Dr. A. Riyaz, HOD and the staff of the Department of Pediatrics, Medical College, Calicut for their help in case management and preparation of the article.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Murthy JM. Acute disseminated encephalomyelitis. Neurol India. 2002;50:238–43. [PubMed] [Google Scholar]
- 2.Garg RK. Acute disseminated encephalomyelitis. Postgrad Med J. 2003;79:11–7. doi: 10.1136/pmj.79.927.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madan S, Aneja S, Tripathi RP, Batra A, Seth A, Taluja V. Acute Disseminated Encephalomyelitis – A case series. Indian Pediatr. 2005;42:367–71. [PubMed] [Google Scholar]
- 4.Murthy SN, Faden HS, Cohen ME, Bakshi R. Acute disseminated encephalomyelitis in children. Pediatrics. 2002;110:e21. doi: 10.1542/peds.110.2.e21. [DOI] [PubMed] [Google Scholar]
- 5.Patel SP, Friedman RS. Neuropsychiatric features of acute disseminated encephalomyelitis. J Neuropsychiatry Clin Neurosci. 1997;9:534–40. doi: 10.1176/jnp.9.4.534. [DOI] [PubMed] [Google Scholar]
- 6.Matsuda M, Miki J, Tabata K, Ikeda S. Severe depression as an initial symptom in an elderly patient with acute disseminated encephalomyelitis. Intern Med. 2001;40:1149–53. doi: 10.2169/internalmedicine.40.1149. [DOI] [PubMed] [Google Scholar]
- 7.The ICD–10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization (WHO); 1992. World Health Organization. [Google Scholar]
- 8.Habek M, Brinar M, Brinar VV, Poser CM. Psychiatric manifestations of multiple sclerosis and acute disseminated encephalomyelitis. Clin Neurol Neurosurg. 2006;108:290–4. doi: 10.1016/j.clineuro.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 9.Bachmann S, Schröder J. Catatonic syndrome related to acute disseminated encephalomyelitis (ADEM) Schizophr Res. 2006;87:336–7. doi: 10.1016/j.schres.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Krishnakumar P, Jayakrishnan MP, Beegum MN, Riyaz A. Acute disseminated encephalomyelitis presenting as acute psychotic disorder. Indian Pediatr. 2008;45:999–1001. [PubMed] [Google Scholar]
- 11.Nasr JT, Andriola MR, Coyle PK. ADEM: Literature review and case report of acute psychosis presentation. Pediatr Neurol. 2000;22:8–18. doi: 10.1016/s0887-8994(99)00116-2. [DOI] [PubMed] [Google Scholar]


