Abstract
Background:
Purely extradural lumbar schwannomas are rare lesions. Resection traditionally requires an open laminectomy and ipsilateral complete facectomy. Recent reports have demonstrated safety and efficacy of removal of these tumors using mini-open access devices with expandable retractors. We report a case of a giant L3 schwannoma successfully resected through a minimally invasive approach using the non-expandable Spotlight tubular retrator (Depuy Spine).
Case Description:
A 77-year-old woman presented with a history of chronic right leg pain, paresthesias and proximal right leg weakness. Magnetic Resonance imaging (MRI) scan revealed a large dumbbell-shaped extradural foraminal lesion at the L3–L4 level with significant extraforaminal extension. The patient underwent a minimally invasive gross total resection (GTR) of the tumor using an 18-mm Spotlight tubular retractor system. Pathology confirmed the lesion to be a benign schwannoma. Postoperatively, the patient's symptoms resolved and she was discharged from the hospital on the second postoperative day. Postoperative MRI showed no residual tumor. The patient returned to normal activities after 2 weeks and remained asymptomatic with no neurological deficits at final 6 months follow-up.
Conclusion:
Giant lumbar extradural schwannomas can be safely and completely resected using minimally invasive surgery without the need for facectomy or subsequent spinal fusion.
Keywords: Giant schwannoma, minimally invasive surgery, spinal neoplasm
INTRODUCTION
Nerve sheath tumors (NSTs) are the most common form of spinal cord tumor, making up almost one-third of primary spinal neoplasms.[17] These tumors are classified as intradural, combined intradural–extradural (7–24%) and purely extradural (2–31%).[5] Spinal extradural foraminal NSTs are rare primary neoplasms of the spinal cord.[5] Exceptionally, these lesions are found in the lumbar spine. The mainstay of treatment is gross total resection (GTR), classically involving midline incision, bilateral subperiosteal muscle stripping, extensive laminectomy and radical foraminotomy. Fusion is often warranted in order to prevent deformity, pain, and neurological deterioration.[12,13,21] Recent reports have demonstrated safety and efficacy of mini-open removal of these tumors using expandable tubular retractors.[10,13,14] We report a case of minimally invasive removal of a giant L3 schwannoma through an 18-mm Spotlight tubular retractor. The advantages of this approach are discussed.
CASE REPORT
History
A 77-year-old woman presented with a history of chronic right leg pain, paresthesias and proximal right leg weakness. There was no history of bowel/bladder dysfunction. Neurological examination revealed 4/5 strength in the right psoas muscle. There were no other motor or sensory deficits. Magnetic Resonance imaging (MRI) scan revealed a large dumbbell-shaped extradural foraminal lesion at the L3–L4 level with significant extraforaminal extension [Figure 1a and b]. The patient underwent a minimally invasive GTR of the tumor. Pathology confirmed the lesion to be a benign schwannoma. Postoperatively, the patient's symptoms improved and she was discharged from the hospital on the second postoperative day. Postoperative MRI showed no residual tumor [Figure 1c and d]. The patient returned to normal activities after 2 weeks and remained asymptomatic with no neurological deficits at final 6 months follow-up.
Figure 1.
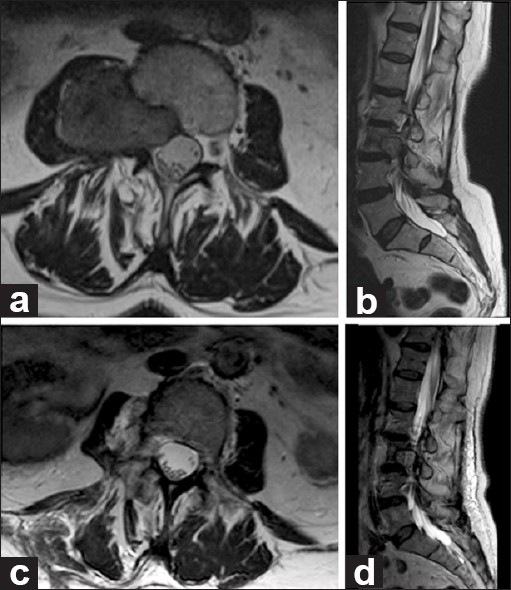
Magnetic resonance images: Preoperative T2-weighted MRI. (a) Axial and (b) sagittal images reveal a right L3-L4 extradural foraminal dumbbell-shaped mass with extraforaminal extension into the right psoas muscle. The patient underwent minimally invasive resection. Postoperative T2-weighted MRI. (c) Axial and (d) sagittal images demonstrate gross total resection and postoperative changes
Operative technique
After sedation and endotracheal intubation, the patient was placed in the prone position on an operating table. Standard sterilization and draping of the lumbosacral area was done. Anteroposterior (AP) and lateral intraoperative fluoroscopy was utilized to localize the L3–L4 level with a k-wire. At this level, a 20-mm-long paramedian skin incision was performed 5 cm from the midline. This paramedian longitudinal incision allowed adequate angle to access the ipsilateral L3–L4 extraforaminal space. The lumbar fascia was incised parallel and slightly medially to the skin incision. A Steinman pin was docked on the right L3–L4 facet complex. A series of dilators were introduced to split the paraspinal muscles. A final 18-mm Spotlight tubular retractor was fixed in place with a table-mounted flexible arm (Depuy Spine, Raynham, MA). The Spotlight was attached to the tube and connected to the light source. Fluoroscopy confirmed the adequate position of the tube retractor in between the right transverse processes of L3 and L4, just lateral to right L3–L4 facet complex [Figure 2]. The surgical microscope was introduced [Video 1]. The fascia and intertransverse membrane were opened allowing access to the tumor capsule. Prior to entry into the tumor capsule, stimulation was performed on the tumor capsule to ensure that there was no nerve root. Standard microsurgical techniques were used. Following coagulation of the tumor capsule, intracapsular debulking was performed using cavitron ultrasonic surgical aspirator (CUSA) [Figure 3]. This allowed us to infold the tumor edges upon themselves and perform extracapsular dissection between the tumor and the psoas muscle. A dissection plane was maintained with paddies. Intraoperative stimulation was performed throughout to ensure that no viable nervous structures were harmed. Following tumor resection, the L3 nerve root was identified and stimulated, confirming its integrity. Hemostasis was performed with standard hemostatic agents and bipolar cautery. The retractor was then removed. The fascia was closed with absorbable sutures and the 20-mm paramedian skin was closed with 2-0 vicryl sutures.
Figure 2.
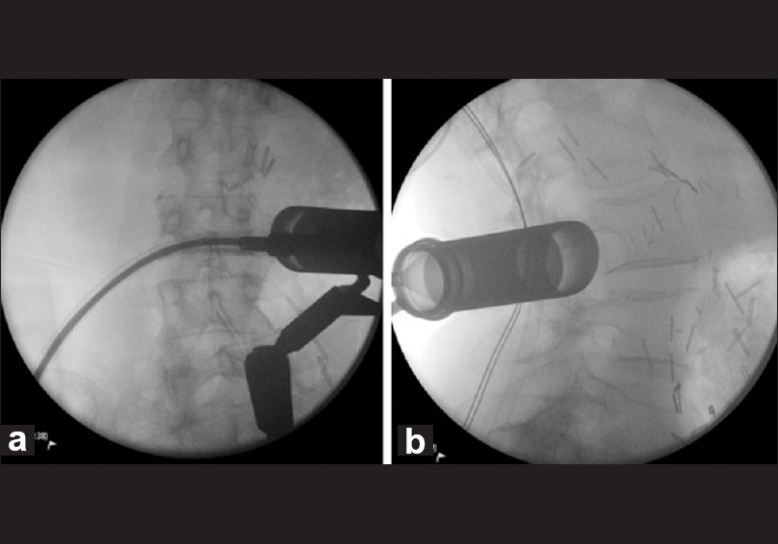
Intraoperative fluoroscopy: (a) AP and (b) lateral X-rays confirm adequate placement of the tubular retractor in between the L3 and L4 spinous process lateral to the L3–L4 facet complex
Figure 3.
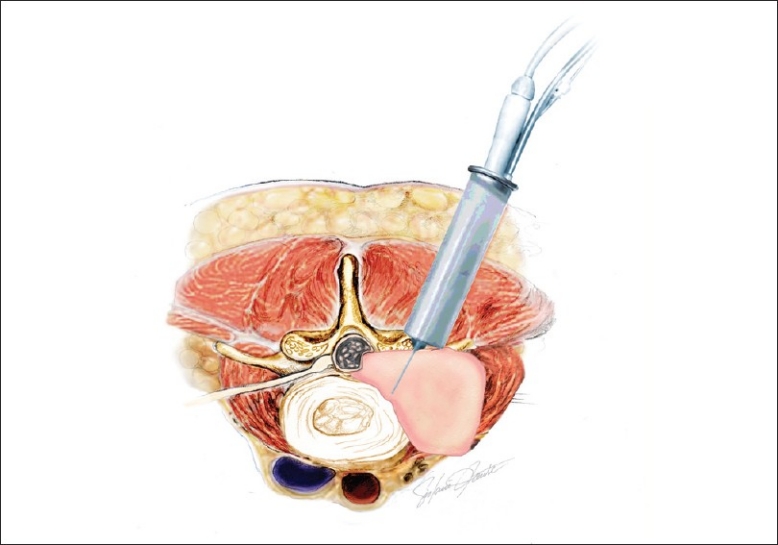
Illustration depicting resection of the giant extraforaminal schwannoma through a minimally invasive transmuscular tube retractor placed lateral to the facet complex
DISCUSSION
Purely extradural spinal schwannomas form a rare subgroup (2–31%) of spinal NSTs.[5,17] Because lumbar nerve roots travel a long distance compared to cervical or thoracic roots before reaching the intervertebral foramen, lumbar extradural schwannomas are exceptional and make up only 0.7–4.2% of all extradural schwannomas.[5,17] GTR, the mainstay of treatment of these lesions, is obtainable in the majority of cases and is associated with long-term remission and excellent functional outcome.[5,28] The majority of surgical series for extradural foraminal schwannomas involve tumors located in the cervical and thoracic regions.[13,16] The classic surgical approach for these lesions involves a long midline skin incision, bilateral subperiosteal muscle stripping from the posterior spinous elements, laminectomy extending to levels above and below the tumor and radical facectomy on the side of the foraminal tumor.[5,13,31,33]
Post-laminectomy instability and deformity is a major concern, especially after multi-level laminectomy and radical facectomy.[1,3,4,19,22,27,32,34,36] Fusion surgery has thus been advocated for these cases with radical facectomy.[12,13,21] In order to avoid iatrogenic instability, deformity, pain, and fusion surgery, resection of intradural-extramedullary and intradural-intramedullary spinal tumors has been performed through a more limited hemilaminar exposure with unilateral partial facectomy (up to one third medial facectomy).[6,20,27,35] Recently, minimally invasive hemilaminar approach with expandable tubular retractors has been utilized to access and successfully resect intradural tumors with reduced tissue destruction, blood loss, and length of hospitalization.[10,15,18,35] Lu et al. recently reported the use of an alternative approach, encompassing midline mini-open access with expandable tubular retractors. The 18 patients who underwent mini-open approach had a reduced blood loss and length of stay as compared to the 9 patients who underwent a standard open technique.[14] However, this approach is not feasible in cases of extradural schwannomas that typically extend on either side of the intervertebral foramen, such as in our case.[29] Resection of the giant extradural schwannoma of the lumbar spine in our case was performed through a non-expandable 18-mm Spotlight tubular retractor.
Although they are anecdotal, the theoretical advantages of this approach are twofold. Firstly, by avoiding extensive laminectomy and especially facectomy in this patient, we obviated the need for spinal fusion. Secondly, the minimally invasive approach used is associated with less tissue destruction. Its use in the treatment of degenerative spinal disease and intradural spinal tumors translates into less blood loss, shorter operative time, shortened hospitalization and a quicker return to daily activities.[7–11,13–15,18,19,23–26,29,30,35] Although recent randomized clinical trials comparing minimally invasive and open microdiscectomy have not supported these findings,[2] the advantage of minimally invasive surgery may be more evident when used for more extensive open surgeries such as tumor resection.[26]
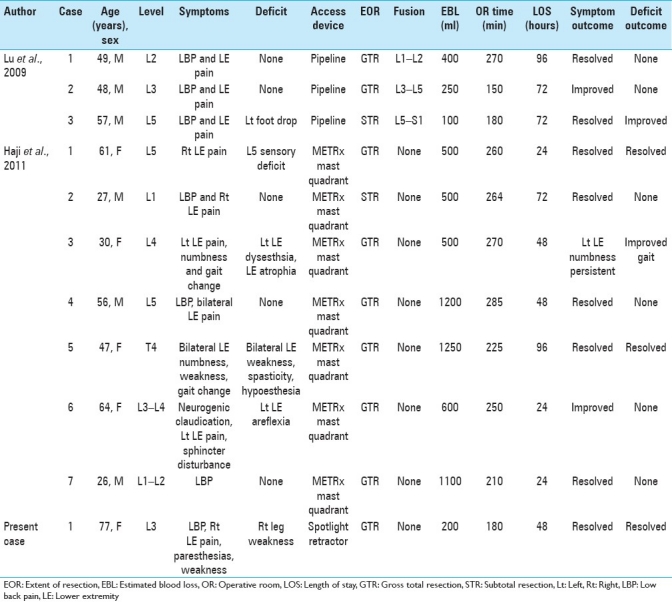
Extradural schwannomas have only recently been resected using mini-open approach through expandable tubular retractors. Lu et al. recently reported their experience resecting extradural lumbar schwannomas in three patients through a mini-open approach using an expandable tubular retractor (Pipeline, Depuy Spine) [Table 1]. In these patients, of whom two had previously been operated (discectomy and fusion surgery), hemilaminectomy and total facectomy was required to completely visualize the tumor, followed by fusion surgery.[13] The advantages of this approach in these reoperation cases include the use of a lateral approach eliminating passage through midline scar tissue and simultaneous access for percutaneous instrumentation. Haji et al. recently reported their experience with resection of intramedullary, intradural-extramedullary and extradural SNTs using METRx Mast quadrant retractor system (Medtronics, Memphis, TN). Seven of their patients had purely extradural thoracic or lumbar schwannomas that were resected through expandable tubular retractors (from 22 to 52 mm) with good results [Table 1]. GTR could be obtained in all but one of these seven cases, with comparable results of blood loss and hospital stay as compared to historical controls.[10] Our case, to our knowledge, is the first extradural lumbar schwannoma resected through an 18-mm non-expandable tubular retractor. This may be associated with even less tissue destruction than mini-open techniques using expandable retractors, translating into less blood loss and a quicker functional recovery [Table 1]. However, further studies are needed to evaluate the relative efficacy and safety of minimally invasive resection of lumbar extradural schwannomas as compared to the standard open or newer mini-open techniques.
Table 1.
Literature review of patients undergoing minimally invasive resection of purely extradural schwannomas
CONCLUSION
Lumbar extradural giant schwannomas can be completely and safely resected through a minimally invasive approach using the Spotlight tubular retractor. By decreasing tissue damage and eliminating the need for facectomy, it may decrease the incidence of postoperative deformity and eliminate the need for adjunctive fusion surgery.
Video available at www.surgicalneurologyint.com
ACKNOWLEDGEMENT
The authors wish to thank Matthew Riggs for his assistance in preparing the video.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/186/91141
Contributor Information
Alexander G. Weil, Email: alexander.weil@umontreal.ca.
Sami Obaid, Email: obaidsami@hotmail.com.
Mohammed Shehadeh, Email: mohshe1111@hotmail.com.
Daniel Shedid, Email: danielshedid@gmail.com.
REFERENCES
- 1.Alexander E, Wilkins RH, Rengachary SS, editors. New York: McGraw-Hill; 1985. Postlaminectomy kyphosis In: Neurosurgery; pp. 2293–7. [Google Scholar]
- 2.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan W, et al. Tubular Diskectomy vs Conventional Microdiskectomy for the Treatment of Lumbar Disk Herniation: 2-Year Results of a Double-Blind Randomized Controlled Trial. Neurosurgery. 2011;69:135–44. doi: 10.1227/NEU.0b013e318214a98c. [DOI] [PubMed] [Google Scholar]
- 3.Bresnahan L, Ogden AT, Natarajan RN, Fessler RG. A biomechanical evaluation of graded posterior element removal for treatment of lumbar stenosis: Comparison of a minimally invasive approach with two standard laminectomy techniques. Spine. 2009;34:17–23. doi: 10.1097/BRS.0b013e318191438b. [DOI] [PubMed] [Google Scholar]
- 4.Caputy AJ, Spence CA, Bejjani GK, Luessenhop AJ. The role of spinal fusion in surgery for lumbar spinal stenosis: A review. Neurosurg Focus. 1997;3:e3. doi: 10.3171/foc.1997.3.2.6. [DOI] [PubMed] [Google Scholar]
- 5.Celli P, Trillò G, Ferrante L. Spinal extradural schwannoma. J Neurosurg Spine. 2005;2:447–56. doi: 10.3171/spi.2005.2.4.0447. [DOI] [PubMed] [Google Scholar]
- 6.Chiou SM, Eggert HR, Laborde G, Seeger W. Microsurgical unilateral approaches for spinaltumour surgery: Eight years’ experience in 256 primary operated patients. Acta Neurochir (Wien) 1989;100:127–33. doi: 10.1007/BF01403599. [DOI] [PubMed] [Google Scholar]
- 7.Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: An initial clinical experience. Neurosurgery. 2002;51:S37–45. [PubMed] [Google Scholar]
- 8.Fessler RG, O’Toole JE, Eichholz KM, Perez-Cruet MJ. The development of minimally invasive spine surgery. Neurosurg Clin N Am. 2006;17:401–9. doi: 10.1016/j.nec.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 9.German JW, Adamo MA, Hoppenot RG, Blossom JH, Nagle HA. Perioperative results following lumbar discectomy: Comparison of minimally invasive discectomy and standard microdiscectomy. Neurosurg Focus. 2008;25:E20. doi: 10.3171/FOC/2008/25/8/E20. [DOI] [PubMed] [Google Scholar]
- 10.Haji FA, Cenic A, Crevier L, Murty N, Reddy K. Minimally Invasive Approach for the Resection of Spinal Neoplasm. Spine (Phila Pa 1976) 2011;36:E1018–26. doi: 10.1097/BRS.0b013e31820019f9. [DOI] [PubMed] [Google Scholar]
- 11.Harrington JF, French P. Open versus minimally invasive lumbar microdiscectomy: Comparison of operative times, length of hospital stay, narcotic use and complications. Minim Invasive Neurosurg. 2008;51:30–5. doi: 10.1055/s-2007-1004543. [DOI] [PubMed] [Google Scholar]
- 12.Jinnai T, Koyama T. Clinical characteristics of spinal nerve sheath tumors: Analysis of 149 cases. Neurosurgery. 2005;56:510–5. doi: 10.1227/01.neu.0000153752.59565.bb. [DOI] [PubMed] [Google Scholar]
- 13.Lu DC, Dhall SS, Mummaneni PV. Mini-open removal of extradural foraminal tumors of the lumbar spine. J Neurosurg Spine. 2009;10:46–50. doi: 10.3171/2008.10.SPI08377. [DOI] [PubMed] [Google Scholar]
- 14.Lu DC, Chou D, Mummaneni PV. A comparison of mini-open and open approaches for resection of thoracolumbar intradural spinal tumors. J Neurosurg Spine. 2011;14:758–64. doi: 10.3171/2011.1.SPINE09860. [DOI] [PubMed] [Google Scholar]
- 15.Mannion RJ, Nowitzke AM, Efendy J, Wood MJ. Safety and efficacy of intradural extramedullary spinal tumor removal using a minimally invasive approach. Neurosurgery. 2011;68(1 Suppl Operative):208–16. doi: 10.1227/NEU.0b013e318207b3c7. [DOI] [PubMed] [Google Scholar]
- 16.McCormick PC. Surgical management of dumbbell tumors of the cervical spine. Neurosurgery. 1996;38:294–300. doi: 10.1097/00006123-199602000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Nittner K, Vinken PH, Bruyn GW, editors. New York: Elsevier; 1976. Spinal meningiomas, neuromas and neurofibromas, and hourglass tumors In: Handbook of Clinical Neurology. North Holland/America; pp. 177–322. [Google Scholar]
- 18.Ogden AT, Fessler RG. Minimally invasive resection of intramedullary ependymoma: Case report. Neurosurgery. 2009;65:E1203–4. doi: 10.1227/01.NEU.0000360153.65238.F0. [DOI] [PubMed] [Google Scholar]
- 19.Ogden AT, Bresnahan L, Smith JS, Natarajan R, Fessler RG. Biomechanical comparison of traditional and minimally invasive intradural tumor exposures using finite element analysis. Clin Biomech (Bristol, Avon) 2009;24:143–7. doi: 10.1016/j.clinbiomech.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Oktem IS, Akdemir H, Kurtsoy A, Koc RK, Menku A, Tucer B. Hemilaminectomy for the removal of the spinal lesions. Spinal Cord. 2000;38:92–6. doi: 10.1038/sj.sc.3100963. [DOI] [PubMed] [Google Scholar]
- 21.Ozawa H, Kokubun S, Aizawa T, Hoshikawa T, Kawahara C. Spinal dumbbell tumors: An analysis of a series of 118 cases. J Neurosurg Spine. 2007;7:587–93. doi: 10.3171/SPI-07/12/587. [DOI] [PubMed] [Google Scholar]
- 22.Papagelopoulos PJ, Peterson HA, Ebersold MJ, Emmanuel PR, Choudhury SN, Quast LM. Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults. Spine (Phila Pa 1976) 1997;22:442–51. doi: 10.1097/00007632-199702150-00019. [DOI] [PubMed] [Google Scholar]
- 23.Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: Technique and outcomes after a minimum of 2 years’ follow-up. Neurosurg Focus. 2008;25:E16. doi: 10.3171/FOC/2008/25/8/E16. [DOI] [PubMed] [Google Scholar]
- 24.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007;32:537–43. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 25.Rahman M, Summers LE, Richter B, Mimran RI, Jacob RP. Comparison of techniques for decompressive lumbar laminectomy: The minimally invasive versus the “classic” open approach. Minim Invasive Neurosurg. 2008;51:100–5. doi: 10.1055/s-2007-1022542. [DOI] [PubMed] [Google Scholar]
- 26.Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: Results of a prospective randomized study. Neurosurgery. 2008;62:174–81. doi: 10.1227/01.NEU.0000311075.56486.C5. [DOI] [PubMed] [Google Scholar]
- 27.Sarioglu AC, Hanci M, Bozkus H, Kaynar MY, Kafadar A. Unilateral hemilaminectomy for the removal of the spinal space-occupying lesions. Minim Invasive Neurosurg. 1997;40:74–7. doi: 10.1055/s-2008-1053420. [DOI] [PubMed] [Google Scholar]
- 28.Seppala MT, Haltia MJ, Sankila RJ, Jaaskelainen JE, Heiskanen O. Long-term outcome after removal of spinal schwannoma: A clinicopathological study of 187 cases. J Neurosurg. 1995;83:621–6. doi: 10.3171/jns.1995.83.4.0621. [DOI] [PubMed] [Google Scholar]
- 29.Sim JE, Noh SJ, Song YJ, Kim HD. Removal of intradural-extramedullary spinal cord tumors with unilateral limited laminectomy. J Korean Neurosurg Soc. 2008;43:232–6. doi: 10.3340/jkns.2008.43.5.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith JS, Ogden AT, Fessler RG. Minimally invasive posterior thoracic fusion. Neurosurg Focus. 2008;25:E9. doi: 10.3171/FOC/2008/25/8/E9. [DOI] [PubMed] [Google Scholar]
- 31.Sridhar K, Ramamurthi R, Vasudevan MC, Ramamurthi B. Giant invasive spinal schwannomas: Definition and surgical management. J Neurosurg. 2001;94(2 Suppl):210–5. doi: 10.3171/spi.2001.94.2.0210. [DOI] [PubMed] [Google Scholar]
- 32.Sridhar K, Ramamurthi R, Vasudevan MC, Ramamurthi B. Limited unilateral approach for extramedullary spinal tumors. Br J Neurosurg. 1998;12:430–3. doi: 10.1080/02688699844637. [DOI] [PubMed] [Google Scholar]
- 33.Tredway TL, Santiago P, Hrubes MR, Song JK, Christie SD, Fessler RG. Minimally invasive resection of intradural-extramedullary spinal neoplasms. Neurosurgery. 2006;58(1Suppl):ONS52–8. doi: 10.1227/01.neu.0000192661.08192.1c. [DOI] [PubMed] [Google Scholar]
- 34.Tuite GF, Doran SE, Stern JD, McGillicuddy JE, Papadopoulos SM, Lundquist CA, et al. Outcome after laminectomy for lumbar spinal stenosis.Part II: Radiographic changes and clinical correlations. J Neurosurg. 1994;81:707–15. doi: 10.3171/jns.1994.81.5.0707. [DOI] [PubMed] [Google Scholar]
- 35.Yasargil MG, Tranmer BI, Adamson TE, Roth P. Unilateral partial hemilaminectomy for the removal of extra- and intramedullary tumors and AVMs. Adv Tech Stand Neurosurg. 1991;18:113–32. doi: 10.1007/978-3-7091-6697-0_3. [DOI] [PubMed] [Google Scholar]
- 36.Yasuoka S, Peterson HA, MacCarty CS. Incidence of spinal column deformity after multilevel laminectomy in children and adults. J Neurosurg. 1982;57:441–5. doi: 10.3171/jns.1982.57.4.0441. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


