Abstract
Recently a clinical prediction rule (CPR) for lumbar regional spinal thrust manipulation (STM) has shown predictive success in patients with back pain who met specific selection criteria. The purpose of this study was to compare the effectiveness of STM and mechanical diagnosis and therapy (MDT) in patients who are positive for the STM CPR. Following initial examination, 31 participants were randomized to the STM group (n = 16) and to the MDT group (n = 15). Two weeks following initial examination, four participants chose to cross over from the STM group to the MDT group. The Oswestry Disability Index (ODI), Fear-Avoidance Beliefs Questionnaire work subscale (FABQw), and the Numerical Pain Rating Scale (NPRS) were administered initially, and at 2-weeks and 4 week follow-up (discharge). Data were analyzed to determine changes in ODI and NPRS scores from initial examination through one month. Of the 31 participants, one patient who met only three of five selection criteria and four others who chose to switch groups were removed from the analysis. Both groups exhibited statistically significant improvements in ODI and NPRS scores from baseline to final visit but there was no significant difference in scores between groups at 4 weeks. In this sample of patients, the selection criteria for this CPR were not exclusive for lumbopelvic STM. Mechanical diagnosis and therapy was an equally viable choice for these patients.
Keywords: Clinical prediction rule, Low back pain, Mechanical diagnosis and therapy, Spinal manipulation
Background
Low back pain (LBP) is frequently cited as the most common musculoskeletal ailment, second only to headache, for which treatment is sought.1 Physical therapy interventions for LBP vary widely, but may include: application of physical agents,2 spinal thrust manipulation (STM),3,4 stabilization exercise programs,5 and/or individualized exercises matched by a determined direction of preference (mechanical diagnosis and therapy, MDT).6
To improve outcomes in managing LBP, clinicians and researchers have developed classification systems to match treatment with more specific patient subgroups. Classification has taken many forms and has included mechanisms derived from patient responses during the examination, imaging analyses, and through statistical assessment of a priori findings that are reflective of a positive outcome with a selected intervention. Clinical prediction rules (CPRs) are structured mechanisms used to classify patients with statistical assessment of selected patient variables to best match patient presentation to a dedicated treatment approach. Preliminary evidence suggests CPRs may lead to favorable outcomes in LBP management.7–11
Recently, there has been an explosion of intervention-based, derivation-styled, physical therapy-oriented CPRs. Concomitantly, four systematic reviews have evaluated the usefulness of CPRs.12–15 All concluded that there is limited evidence for confident direct clinical application for any of the identified CPRs. Others have suggested that additional steps are needed to determine the effectiveness of current CPRs,16,17 steps that the majority of studies have not undergone. Further, editorials, tutorials, and opinion papers have warned of the pitfalls associated with potential methodological weaknesses with CPRs and the possible risks associated with premature adoption of the tools.18–21 Despite these findings, CPRs have been promoted as the next logical step in the progression of treatment decision-making.22
The most cited CPR was derived from Flynn et al.9 The study identified five variables: (1) score of less than 19 on the Fear-Avoidance Belief Questionnaire work subscale score; (2) no symptoms distal to the knee; (3) symptom duration of fewer than 16 days; (4) minimum of one hip with greater than 35 degrees of internal rotation; and (5) palpable hypomobility during a posterior–anterior assessment of the lumbar spine. The study was validated by Childs et al.7 on a similar patient population and found that those who met the CPR and received spinal manipulative therapy were more likely to improve in pain and perceived disability than those who met the rule and received general low back exercises, based on the Agency for Healthcare Research and Quality (AHRQ) guidelines.23
Others have investigated the same rule in a different population, using modified treatment parameters and inclusion criteria. Hancock and colleagues24 employed the same CPR criteria but generally intervened with non-thrust, mobilization techniques. In their study, no difference in pain or disability was found between those who met the CPR criteria and whether they received mobilization/manipulation or not. In a slightly different design that included subjects meeting only two of five CPR criteria (in addition to age >35 year), Hallegraeff et al.25 found improvements in disability at 2½ weeks, but no improvements in either pain or lumbar range of motion. It should be noted that the authors modified the design of the original validation study by providing four additional sessions of manipulation, rather than the two sessions by the original authors.
Perhaps the most noteworthy challenge posed to CPRs is that most of the variables captured during the derivation phase are prognostic-based, suggesting that the ‘rule’ captures variables that lead to good outcomes, regardless of the intervention used.16 Evidence exists to support this assumption, through a recent evaluation that used a novel regression formula to control for prognostic elements used to classify patients for a treatment intervention.26 When the lumbar manipulation study by Childs and colleagues7 was evaluated using the novel formula, the differences in treatment effect for the lumbar spine manipulation CPR were found to be associated with the prognostic capacity of the variables; not necessarily the treatment effect.18 In other words, if those variables are used identify a subset within a larger group of patients, the likelihood of a positive outcome is enhanced, regardless if the patient receives a specific intervention such as a manipulation technique.
Ironically, the only study evaluated by Kent and colleagues26 that used a classification approach that did demonstrate a statistically significant treatment effect, regardless of the prognostic variables, was one27 that used a directional preference method, identified after a series of end-range, repeated movement (a standard criterion of the MDT approach). With the MDT approach,6,27–33 a clinician endeavors to: (1) identify a mechanical deficit, (2) arrive at a classification, and, where possible, (3) determine a direction of preference (DP), (4) instruct the patient to perform exercises or assume postures in the DP which causes centralization and abolition of symptoms, and (5) empower the patient to maintain the reduction and abolition of symptoms through an individualized, preventative strategy.1,6 The DP is defined as the movement or position that decreases, centralizes or abolishes patient’s symptoms.27 There is a wealth of outcomes and prognostic studies to support the MDT approach.29–33
At present, there has been no direct comparison between spinal manipulation and the MDT approach in patients who meet the criteria for the lumbar spine manipulation CPR. Flynn and colleagues9 and Childs et al.7 compared manipulation against AHRQ guidelines, and a past report by AHRQ indicated that their own acute LBP guidelines required updating.34 Consequently, comparing manipulation against an MDT approach will offer a more applicable comparison group and should more realistically define the value of a dedicated manipulation approach. The purpose of this study was to compare clinical outcomes of patients who receive either spinal manipulation or MDT, who met the CPR criteria for manipulation.
Methods
Subjects
Consecutively selected, formally consenting adults diagnosed with LBP referred to outpatient physical therapy clinics in a regional health care system participated in this randomized clinical trial. This study was approved by the institutional review boards for protection of human subjects at the University of Oklahoma Health Sciences Center, Catholic Health System of Buffalo, NY, and Damen College.
Inclusion criteria
Participating subjects were included if: (1) they were at least 18 years old and (2) they experienced an episode of LBP at the time of physical therapy referral. Originally, subjects were enrolled in the study if they met at least three of five of the selection criteria in the CPR introduced by Flynn et al.9 The original decision to use three of five of the criteria versus the recommended four of five of the criteria was made since the number of subjects with LBP that met the four of five criteria possibly would be fewer. However, only those who met all four of five of the CPR criteria were retained for analysis and included within the model.
Exclusion criteria
Subjects were excluded if they: (1) had a history of spinal surgery, (2) had a progressive disease process, (3) were being treated for psychological illness, (4) were pregnant, (5) were experiencing symptoms relative to cauda equina syndrome, (6) did not understand English, or (7) if they were engaged in litigation related to their LBP. Individuals who were insured through workers compensation or no fault insurance were also excluded from the study.
Physical therapists
Data were collected by researchers who were blinded to the intervention rendered. Both manipulation and MDT interventions were provided by the study physical therapists with certification in MDT of the Spine. Physical therapists with these levels of training have been shown to be reliable when classifying patients using this system.35 The study physical therapists also have had formal training in varied types of joint manipulation, but, for the current study, received specific training in the regional lumbopelvic thrust manipulation as described by Flynn et al.9 for two sessions of 2 hours each. These clinicians were qualified as study therapists following competency assessment by a Fellow of the American Academy of Orthopaedic Manual Physical Therapists.
Instruments
The Oswestry Disability Index (ODI), the Numeric Pain Rating Scale (NPRS), and the Fear Avoidance Beliefs Questionnaire Work Subscale (FABQw) were used in the current study and were also used in the previous derivation and validation studies.9 The ODI is a self-reported, ten-item questionnaire that provides a rating of the individual’s perceived functional disability level. The ODI has been proven valid and reliable for individuals with LBP.36 The NPRS is a measure of the patients’ self-reported perception of their current level of pain.37,38 Numeric Pain Rating Scale data were collected at each follow-up visit. Jensen et al.38 suggested that 10- and 21-point scales provide sufficient levels of discrimination, in general, for chronic pain patients to describe pain intensity. The FABQ is a multi-item questionnaire that measures the patients’ perceived fear of their symptoms.39 A portion of the FABQ, the work subscale (FABQw), has been shown to directly relate to work loss and disability in people with LBP.40,41 The FABQw questionnaire took approximately 10 minutes to complete. A score of 19 or less was considered with minimal to no fear avoidance during physical therapy.40
Physical examination
All patients were initially evaluated for red flags or other non-mechanical conditions that were deemed not conducive for care by physical therapists. Administration of the ODI, FABQw and NPRS, a subjective interview, and an objective physical examination followed. The examination process incorporated assessment of posture and structural alignment, spinal active range of motion, neurological tests, lumbar repeated movements, reflex assessment, straight leg raise measures, palpation, and posteroanterior spring testing. After these assessment measures were gathered, study therapists determined whether or not patients met the CPR selection criteria. When consented for the study, participants were randomly assigned via a computerized random number generator to the STM or MDT group.
Treatment
The STM group received treatment consisting of the regional lumbopelvic thrust technique using the same dosage and procedures from the previously published trials.7,9 Participants in the STM group also received instruction on the hand-heel rock range of motion exercise for 30 repetitions and 20 repetitions for sessions 1 and 2, respectively. The hand-heel rock involved lumbar movement into flexion and then extension from the quadruped position. These exercises were performed both in the clinic and at home to parallel the level of activity performed by the STM group in Flynn et al.9 If the participants were assigned to receive MDT, exercises according to the DP determined at the initial visit were recommended in both the clinic and as home exercises. All participants were instructed to complete a daily log of adherence to the home exercises. In addition to the STM or MDT administered in the clinic, participants performed 10 repetitions of the movements in the DP on an hourly basis during the day only, from session 3 until discharge as the home exercise program.
If participants failed to improve with the randomly assigned treatment (STM or MDT), the intervention was changed to the alternative treatment at the week #2 visit. The NPRS was one measure used for the decision for participants to switch into the other treatment group. The other measure was use of a pain diagram for location and change in location (centralization or peripheralization of symptoms since initial visit). The pain diagram documentation was based on symptom response and location of symptoms as supported by Werneke and Hart31 who found a pain diagram could be used to categorize symptoms as low back, buttock/thigh, or distal to the knee based on the distal-most extent of symptoms. Change in location on the pain diagram proximally signified centralization; a distal change in location signified peripheralization. If the patients increased in severity of pain and did not centralize or indeed peripheralize symptoms, the intervention was changed to the alternative treatment. Crossover subjects were not retained for the final analysis within the model.
Data analysis
A third party professional statistician not affiliated with authorship or data collection completed all statistical analyses. Participants’ characteristics were analyzed with descriptive statistics. Within-session and between-session changes using the change score data from the NPRS and ODI (reflecting the change from baseline to the last scheduled visit by week 4) from each participant group were compared using the Mann–Whitney U for differences from initial visit to Week 4. All analyses were intention to treat. Outcomes were also investigated as ‘success’ or ‘fail’ based on a 50% reduction on the ODI. A chi-square was used to determine whether group proportions met the 50% reduction in the ODI from baseline to Week 4. Significance was set at 0·05.
Results
Thirty-one participants who met the selection criteria consented to participate in the study (Fig. 1). Of the 31 participants, 16 were randomized to the STM group and 15 to the MDT group. One of the 31 participants met three of five selection criteria and was removed from the analysis, leaving a total of 30 subjects who met four out of the five selection criteria. At visit two weeks, four participants chose to cross over from the STM group to the MDT group; none of the MDT group requested to cross over to the STM group. The clinicians’ recommendation to the patient to switch groups was based on the patient report that neither a symptomatic or functional improvement was experienced with the originally prescribed treatment. However, these four individuals were removed from the statistical model. With the exception of one participant in each group, all participants met the CPR criterion of an FABQw scored less than 19. Table 1 depicts the participant demographics for age, gender, symptom duration, and FABQw scores.
Figure 1.
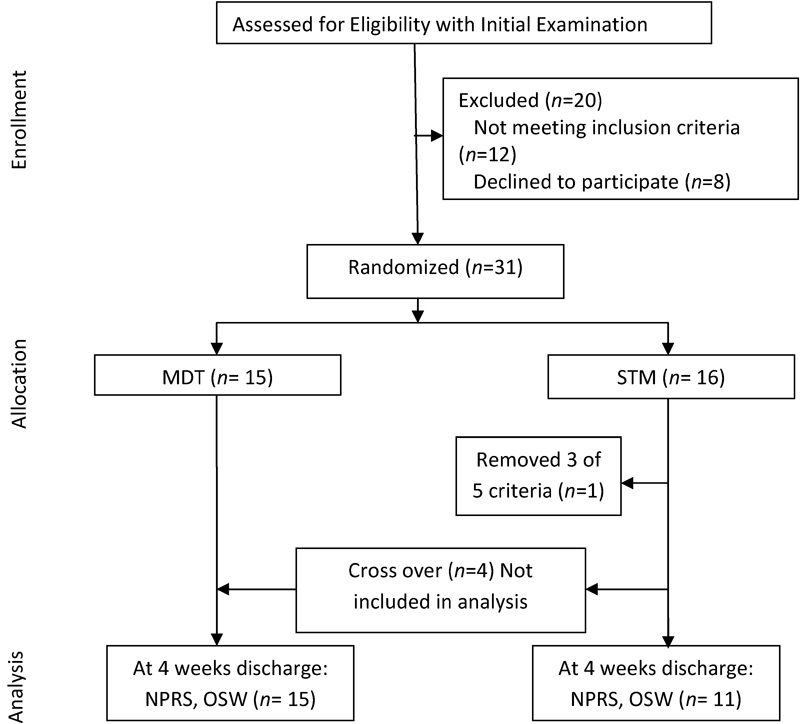
CONSORT Flow Diagram
Table 1. Patient demographics.
| Group | Mean age (years) | Age range (years) | Gender | Mean symptom duration (days) | Mean FABQw scores |
| Spinal thrust manipulation | 46 | 18–65 | 7 female | 15 | 14·2 |
| 5 male | |||||
| Mechanical diagnosis and therapy | 39 | 25–58 | 12 female | 18 | 18·1 |
| 7 male |
Both groups exhibited statistically significant, within-groups improvements in ODI and NPRS scores from baseline to final visit. At baseline, the average ODI for the SMT groups was 30·5 (SD = 9·8), whereas the average NPRS was 3·25 (SD = 1·83). At discharge the average ODI was 25·7 (SD = 27·6), and the NPRS was 2·9 (SD = 3·4). For the MDT group the average ODI at baseline was 28·7 (SD = 11·5), whereas the average NPRS was 5·4 (SD = 1·9). At discharge the average ODI was 13·7 (SD = 12·3), and the NPRS was 1·5 (SD = 3·4). Between groups changes were not significantly different for the ODI (P = 0·31), NPRS (P = 0·08) or the 50% reduction in the ODI from baseline to discharge (P = 0·16) (Table 2).
Table 2. Tests of differences between groups SMT and MDT (Mann–Whitney U).
| Outcome variable | Spinal manipulative therapy (mean rank) | Mechanical diagnosis and therapy (mean rank) | P value |
| Between groups changes | |||
| Oswestry Disability Index | 11·13 | 14·56 | 0·31 |
| Numeric Pain Rating Scale | 9·56 | 15·25 | 0·08 |
| 50% reduction in the Oswestry Disability Index | 2 = yes | 10 = yes | 0·155 |
| 6 = no | 8 = no | ||
Discussion
In the current study, the investigators analyzed clinical outcomes of participants treated with STM or MDT. The safety and effectiveness of these treatment methods for LBP have been well established.7,9,27–33 The STM group differed in this trial as compared to the derivation and validation (respectively) studies of Flynn and colleagues.7,9 First, the investigators initially opted to enroll subjects who met three of five of the CPR variables versus the recommended four of five and did so bolster the number of subjects who would qualify within the outpatient settings. Subjects who met the three of five criteria only were subsequently removed from the study analysis. Ironically, 30 of the 31 participants enrolled in this study met at least four out of the five of the selection criteria, thus our original concerns were not substantiated. Second, clinicians were authorized to cross over subjects who did not meet the expected changes by the second week visit. This, too, differed from the design used by Flynn and Childs and must be considered for interpretation. However, the investigators also analyzed the current study results with the four crossover subjects removed from the analysis. Third, our sample size was smaller than the subject samples in the derivation and validation studies. The sample size could misrepresent the findings and may be reflective of the differences in results. Lastly, all subjects, regardless of enrollment, performed 10 repetitions of lumbar movements. Participants in the MDT group performed the repetitive movements in the DP on an hourly basis throughout the day, from session 3 until discharge as the home exercise program, a standard part of a MDT intervention. Those in the STM group performed lumbar flexion and extension in quadruped (‘cat and camel’) for 10 repetitions hourly throughout the day, from session 3 until discharge. These home exercise programs could alter long-term outcomes and further challenge the ability to discriminate findings between the two groups.
There were notable differences in successful outcomes among those included in the SMT group using the outcomes associated with 50% ODI reduction. According to Flynn et al.,9 the presence of four of the five variables in the prediction rule, and manipulative treatment, increased the likelihood of success in patients with back pain using STM from 45 to 95%. In our study, 46% of the subjects met the 50% reduction on the ODI at discharge regardless of approach of intervention. In the SMT group, only 25% of the subjects who met the CPR met the 50% reduction on the ODI by discharge. The investigators are unable to fully explain the variations in results but do recognize two notable possibilities. The initial ODI findings are lower (less perceived disability score) than those reported by Flynn and colleagues.7,9 This baseline may have left less room for observable change (improvement in perceived disability). The investigators did not require a minimal ODI score for enrollment, another variation from the derivation and validation findings.7,9
Both groups exhibited notable and significant within-groups changes from baseline to discharge for both pain and disability, yet there was no difference in changes in pain or disability between groups. One plausible explanation is the possibility that the CPR for spinal manipulation may be prognostic, rather than prescriptive, in nature. If this cluster of selection criteria is ‘prognosis-based’, then this suggests that anyone who meets the rule, and receives a reasonable treatment approach that is indicated for their presentation, they will improve over time. As indicated previously, a recent evaluation that used a novel analytic formula to control for prognostic elements indicated that changes associated with intervention within the domain of a CPR has a marginal treatment effect and a moderate prognostic effect.26 This would suggest that other reasonable, evidence-based options for intervention other than manipulation should exhibit comparable outcomes.
One ‘take home’ message that is contained within this paper is that matching patient classification and sub-grouping of patients based on a CPR or patient response (MDT) with treatment may lead to improved efficiency in treating those with back pain. A cardinal feature of MDT is empowerment of patients, where through education, patients actively employ strategies to reduce and prevent back pain. This feature can foster patients’ self-reliance to more effectively manage their back health. The MDT-trained physical therapists instruct patients on specific exercises, movements, and postures to effectively manage the present episode and, in future, manage to minimize episodes of LBP.
Limitations
There are limitations to this study. In addition to limitations already mentioned, the chance that personal equipoise bias had played a role is possible because those who applied the interventions were MDT certified. It should be noted that the study therapists were also highly trained in spinal manipulation and employed those interventions as well. However, there is a chance that those who crossed over to the MDT group from the SMT group would have improved or declined significantly enough to provide a statistical difference between the two groups. Our small sample size likely contributed to inability to further detect between-group changes at the long-term follow-up.
Conclusion
The current study suggests that MDT and SMT lead to similar outcomes in patients who meet the CPR for spinal manipulation. Future research should concentrate on larger sample sizes, whether or not the CPR is prognostic or prescriptive, and whether other interventions can lead to a similar or better outcome for those who do meet this rule.
References
- 1.Miller E, Schenk R, Karnes J, Rousselle J. A comparison of the McKenzie Approach to a specific spine stabilization program for chronic low back pain. J Man Manip Ther 2005;13:103–12 [Google Scholar]
- 2.Allen RJ. Physical agents used in the management of chronic pain by physical therapists. Phys Med Rehabil Clin N Am 2006;17:315–45 [DOI] [PubMed] [Google Scholar]
- 3.Kohlbeck FJ, Haldeman S, Hurwitz EL, Dagenais S. Supplemental care with medication assisted manipulation versus spinal manipulation therapy alone for patients with chronic low back pain. J Manipulative Physiol Ther 2005;28:245–52 [DOI] [PubMed] [Google Scholar]
- 4.Lisa AJ, Holmes EJ, Ammendolia C. High-velocity low-amplitude spinal manipulation for symptomatic lumbar disc disease: a systematic review of literature. J Manipulative Physiol Ther 2005;28:429–42 [DOI] [PubMed] [Google Scholar]
- 5.McGill SM. Low back stability: from formal description to issues for performance and rehabiliation. Exer Sport Sci Rev 2001;29:26–31 [DOI] [PubMed] [Google Scholar]
- 6.McKenzie RA, May S. The lumbar spine: mechanical diagnosis and therapy. Waikanae: Spinal Publication Limited; 2003 [Google Scholar]
- 7.Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Inter Med 2004;41:920–8 [DOI] [PubMed] [Google Scholar]
- 8.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther 1995;75:470–85 [DOI] [PubMed] [Google Scholar]
- 9.Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine 2002;27:2835–43 [DOI] [PubMed] [Google Scholar]
- 10.Harris GR, Susman JL. Managing musculoskeletal complaints with rehabilitation therapy: summary of the Philadelphia panel evidence-based clinical practice guidelines on musculoskeletal rehabilitation interventions. J Fam Pract 2002;51:1042–6 [PubMed] [Google Scholar]
- 11.Wilson L, Hall H, McIntosh G, Melles T. Intertester reliability of a low back pain classification system. Spine 1999;24:248–54 [DOI] [PubMed] [Google Scholar]
- 12.May S, Rosedale R. Prescriptive clinical prediction rules in back pain research: a systematic review. J Man Manip Ther 2009;17:36–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beneciuk JM, Bishop MD, George SZ. Clinical prediction rules for physical therapy interventions: a systematic review. Phys Ther 2009;89:114–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haskins R, Rivett DA, Osmotherly PG. Clinical prediction rules in the physiotherapy management of low back pain: a systematic review. Man Ther 2011 Jun 3 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Stanton TR, Hancock MJ, Maher CG, Koes BW. Critical appraisal of clinical prediction rules that aim to optimize treatment selection for musculoskeletal conditions. Phys Ther 2010;90:843–54 [DOI] [PubMed] [Google Scholar]
- 16.Hancock M, Herbert RD, Maher CG. A guide to interpretation of studies investigating subgroups of responders to physical therapy interventions. Phys Ther 2009;89:698–704 [DOI] [PubMed] [Google Scholar]
- 17.Cook C, Brismée JM, Pietrobon R, Sizer P, Jr, Hegedus E, Riddle DL. Development of a Quality Checklist Using Delphi Methods for prescriptive clinical prediction rules: the QUADCPR. J Manipulative Physiol Ther 2010;33:29–41 [DOI] [PubMed] [Google Scholar]
- 18.Chaitow L. Clinical prediction rules. J Bodyw Ther 2010;14:207–8 [DOI] [PubMed] [Google Scholar]
- 19.Cook CE. Potential pitfalls of clinical prediction rules. J Man Manip Ther 2008;16:69–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knottnerus JA. Clinical prediction rules: what are they and what do they tell us? Diagnostic prediction rules: principles, requirements and pitfalls. Prim Care 1995;22:341–63 [PubMed] [Google Scholar]
- 21.Beattie P, Nelson R. Clinical prediction rules: what are they and what do they tell us? Aust J Physiother 2006;52:157–63 [DOI] [PubMed] [Google Scholar]
- 22.Whitman JM, Cleland J, Mintken P. Clinical prediction rules in physical therapy: coming of age? J Orthop Sports Phys Ther 2009;39:231–3 [DOI] [PubMed] [Google Scholar]
- 23.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Clinical efficacy assessment subcommittee of the American College of Physicians, American College of Physicians, American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147:478–91 [DOI] [PubMed] [Google Scholar]
- 24.Hancock MJ, Maher CG, Latimer J, Herbert RD, McAuley JH. Independent evaluation of a clinical prediction rule for spinal manipulative therapy: a randomised controlled trial. Eur Spine J 2008;17:936–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallegraef JM, de Greef M, Winters JC, Lucas C. Manipulative therapy and clinical prediction criteria in treatment of acute nonspecific low back pain. Percept Mot Skills 2009;108:196–208 [DOI] [PubMed] [Google Scholar]
- 26.Kent P, Marks D, Keating J, LaBoeuf-Yde Research methods for subgrouping low back pain. BMC Med Res Meth 2010;10:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine 2004;29:2593–602 [DOI] [PubMed] [Google Scholar]
- 28.Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain: a predictor of symptomatic discs and annular competence. Spine 1997;22:1115–22 [DOI] [PubMed] [Google Scholar]
- 29.Schenk RJ, Jozefczyk C, Kopf A. A randomized controlled trial comparing interventions in patients with lumbar posterior derangement. J Man Manip Ther 2003;11:95–102 [Google Scholar]
- 30.Werneke M, Hart DL. Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine 2001;26:758–65 [DOI] [PubMed] [Google Scholar]
- 31.Werneke M, Hart DL. Discriminant validity and relative precision for classifying patients with nonspecific neck and back pain by anatomic pain patterns. Spine 2003;28:161–6 [DOI] [PubMed] [Google Scholar]
- 32.Werneke M, Hart DL. Centralization: association between repeated end-range pain response and behavioral signs in patients with acute non-specific low back pain. J Rehabil Med 2005;37:286–90 [DOI] [PubMed] [Google Scholar]
- 33.Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon: a prospective analysis. Spine 1999;24:676–83 [DOI] [PubMed] [Google Scholar]
- 34.Ortiz E, Eccles M, Grimshaw J, Woolf S. Current validity of AHRQ clinical practice guidelines. Rockville, MD: Agency for Healthcare Research and Quality (US); 2002 [PubMed] [Google Scholar]
- 35.Clare HA, Adams R, Maher CG. Reliability of McKenzie classification of patients with cervical or lumbar pain. J Manipulative Physiol Ther 2005;28:122–127 [DOI] [PubMed] [Google Scholar]
- 36.Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine 2000;25:2940–53 [DOI] [PubMed] [Google Scholar]
- 37.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30:1331–4 [DOI] [PubMed] [Google Scholar]
- 38.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain 1994;58:387–92 [DOI] [PubMed] [Google Scholar]
- 39.Waddell G, Newton M, Henderson I, Somerville D, Main C. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1994;52:157–68 [DOI] [PubMed] [Google Scholar]
- 40.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain 2001;94:7–15 [DOI] [PubMed] [Google Scholar]
- 41.Cleland JA, Fritz JM, Brennan GP. Predictive validity of initial fear avoidance beliefs in patients with low back pain receiving physical therapy: is the FABQ a useful screening tool for identifying patients at risk for a poor recovery? Eur Spine J 2008;17:70–9 [DOI] [PMC free article] [PubMed] [Google Scholar]


