Abstract
Introduction: Approximately 600,000 hysterectomies are performed in the US each year, making hysterectomy the second most common major operation performed in women. Several methods can be used to perform this procedure. In 2009, a Cochrane Review concluded “that vaginal hysterectomy should be performed in preference to abdominal hysterectomy, where possible. Where vaginal hysterectomy is not possible, a laparoscopic approach may avoid the need for an abdominal hysterectomy. Risks and benefits of different approaches may however be influenced by the surgeon's experience. More research is needed, particularly to examine the long-term effects of the different types of surgery.”
This article reviews the steps that a large multispecialty group used to teach non-open hysterectomy methods to improve the quality of care for their patients and to decrease the number of inpatient procedures and therefore costs. The percentages of each type of hysterectomy performed yearly between 2005 and 2010 were calculated, as well as the length of stay (LOS) for each method.
Methods: A structured educational intervention with both didactic and hands-on exercises was created and rolled out to 12 medical centers. All patients undergoing hysterectomy for benign conditions through the Southern California Permanente Medical Group (a large multispecialty group that provides medical care to Kaiser Permanente patients in Southern California) between 2005 and 2010 were included. This amounted to 26,055 hysterectomies for benign conditions being performed by more than 350 obstetrician/gynecologists (Ob/Gyns).
Results: More than 300 Ob/Gyns took the course across 12 medical centers. On the basis of hospital discharge data, the total number of hysterectomies, types of hysterectomies, and LOS for each type were identified for each year. Between 2005 and 2010, the rate of non-open hysterectomies has increased 120% (from 38% to 78%) and the average LOS has decreased 31%.
Introduction
Hysterectomy is the second most common surgical procedure undergone by women in the US, with approximately 600,000 hysterectomies being performed each year.1 The procedure can be an open one, such as total abdominal hysterectomy or subtotal abdominal hysterectomy, which leaves the cervix behind, or a non-open one, such as vaginal hysterectomy (VH), laparoscopic supracervical hysterectomy (LSH), total laparoscopic hysterectomy (TLH), or laparoscopy-assisted vaginal hysterectomy (LAVH). Minilaparotomy hysterectomy has some advantages over open hysterectomy,2 but although this procedure is done within the Southern California Permanente Medical Group (SCPMG), it could not be identified within our coding system and thus is not further discussed here.
The organization Advancing Minimally Invasive Gynecology Worldwide (AAGL) has recently stated that “most hysterectomies for benign disease should be performed either vaginally or laparoscopically and that continued efforts should be taken to facilitate these approaches. Surgeons without the requisite training and skills required for the safe performance of VH or LH should enlist the aid of colleagues who do or should refer patients requiring hysterectomy to such individuals for their surgical care.”3
SCPMG is a multispecialty medical group with 6000 physicians providing medical care for Kaiser Permanente (KP) patients in Southern California. Between 2005 and 2010, SCPMG physicians performed 26,055 hysterectomies.
The average rate of non-open hysterectomy across the US last noted in 2003, was approximately 35%,1 consistent with SCPMG data, before 2005. More recent national data are not available yet. Some more recent articles show rates between 43.2% to 64.2% (Cedars Sinai Hospital,4 The Permanente Medical Group in Northern California [Rebecca U Margulies, MD, personal communication, 2011 May],a and Brigham and Women's Hospital5).
A Cochrane review found:
… that vaginal hysterectomy meant quicker return to normal activities, fewer infections and episodes of raised temperature after surgery, and a shorter stay in hospital compared to abdominal hysterectomy.
Laparoscopic hysterectomy meant quicker return to normal activities, less blood loss and a smaller drop in blood count, a shorter stay in hospital, and fewer wound infections and episodes of raised temperature after surgery compared to abdominal hysterectomy, but laparoscopic hysterectomies have a greater risk of damaging the bladder or ureter (the tube leading to the bladder from the kidney) and are longer operations.
No benefits were found for laparoscopic versus vaginal hysterectomy. Laparoscopic hysterectomies are longer operations associated with a higher rate of substantial bleeding.6
Individual physicians within SCPMG had been performing various types of non-open hysterectomy (including traditionally taught VH) since 1991, but there had not been a concerted effort to train physicians in the entire Region. An effort began in 2005 to increase the proportion of non-open hysterectomies within SCPMG. This article reviews the process involved, the change in non-open hysterectomy rates, changes in the length of stay (LOS), and changes in total costs. Several steps occurred simultaneously to generate interest in this project, including a presentation on the merits of non-open hysterectomy to the Regional Chiefs of Obstetrics/Gynecology (Ob/Gyn), data from a study on LSH conducted at one of the centers,7 the appointment of a new Regional Chief of Ob/Gyn, and a receptive Regional Medical Director in charge of quality and clinical analysis. This led to the idea that if a training program were created and expert mentorship became available, SCPMG could become a national leader in non-open hysterectomy and thus improve the quality of medical care for their patients.
Methodology
The 12 SCPMG Chiefs of Ob/Gyn wanted to increase the percentage of non-open hysterectomies performed so that SCPMG would eventually be the national leader for the procedure. The Regional Chief of Ob/Gyn was given the mandate to create a teaching program to help reach this goal.
Preparation
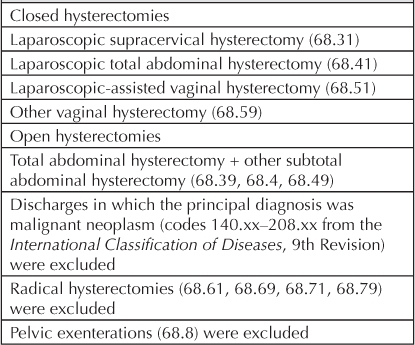
Discharge data for benign hysterectomy were used to identify three key components at each medical center: total hysterectomies, type of hysterectomies performed, and LOS for each type of hysterectomy (Table 1). No approval from an institutional review board was indicated, because our study was a retrospective chart review and patients could not be identified, either directly or through identifiers linked to them.
Table 1.
Coding used for data collection for benign hysterectomy, 2005–2010
It was believed that the program had to create expertise at each medical center with all types of non-open hysterectomy so that every Ob/Gyn would be able to tailor the type of surgery to the individual patient. The program would also emphasize how to set up an operating room for minimally invasive surgery (MIS); how to function as a team; and how to minimize, recognize, and manage complications. It was believed that there had to be development of intraregional proctoring, with two champions at each medical center. It was hoped that there would be a reduction and standardization of the LOS for non-open hysterectomies at the same time.
Eight “content experts” were selected to create and then implement a regional teaching program. They were known within the Region for their technical expertise, teaching ability, and commitment to excellent patient care and to SCPMG. At the first group meeting, each instructor declared his or her favorite hysterectomy method on the basis of interpretation of the literature and experience. A consensus on preoperative preparation and postoperative care was reached through four face-to-face meetings. The group could not agree on a “best” method of non-open hysterectomy, so it was decided to teach each of four types during the courses.
Intervention
A content expert presented each major type of non-open hysterectomy, reviewing aspects that the other methods had in common and going into more depth for methodologies that were unique.
A basic science lecture on energy sources was included, along with a section on avoiding, identifying, and managing intraoperative complications. The group visited each of the 12 medical centers to encourage optimal local participation. The course was 9 hours long, half of it being didactic, with inclusion of videos, and the other half being hands-on learning and practicing of advanced laparoscopic skills. The videos were created and organized to teach important techniques for each type of non-open hysterectomy. The hands-on session used modified FLS (Fundamentals of Laparoscopic Surgery) Trainer Boxes8 (Tables A and B; online onlyb). These had been proven to improve laparoscopic skills.9
For more options for style of learning, all lectures were posted at KP DocuShare, a Web-based Intranet holding area of information for SCPMG clinicians, and could be reviewed before or after the courses (http://dms.kp.org/docushare/dsweb/View/Collection-209036 [password protected]). A pre-course worksheet and agenda (Tables A and B; online onlyb) was sent to all participants at least one week before the event at each medical center.
All exercise and surgical videos were uploaded to YouTube.com so that individuals could view them before or after the course: www.youtube.com/results?search_query=MISP2009 (Table A; online onlyb).
The average LOS for non-open hysterectomy decreased to 24 hours (a 34% decrease) …
Evaluation
Regional education staff helped prepare a questionnaire to be filled out by course participants before receiving continuing medical education credit of 8.5 hours.
Funding
SCPMG provided funding for the FLS Trainer Boxes, portable video monitors, laparoscopic needle-drivers and knot-pushers, and scissors ($100,000 total). One of the authors (EA) modified each of the FLS Trainer Boxes (www.youtube.com/watch?v=YX5bhdOgPqo). The individual medical centers covered instructors' salary during presentations, along with the time and costs of modifying the FLS Trainer Boxes. Individual participants used their education half-days from two consecutive weeks, so that they could maintain patient access. Several companies (with contracts approved by the KP National Product Council) provided some of the equipment for the sessions (Table C; online onlyb). There were no conflicts of interest identified in the provision of supplies by these companies. When the course was completed, 30 FLS Trainer Boxes and equipment were distributed proportionately across the 12 medical centers for continued local learning and practice.
Results
Approximately 300 Ob/Gyns attended the educational intervention (85% of SCPMG's total number of Ob/Gyns).
Hysterectomies Performed
Although the total number of hysterectomies increased in 2008 and 2009, it then decreased to the 2005–2007 level (Figure 1A). The percentage of non-open hysterectomies increased regionally by 120% between 2004 and 2010 (from 38% to 78%; Figure 1B).
Figure 1.
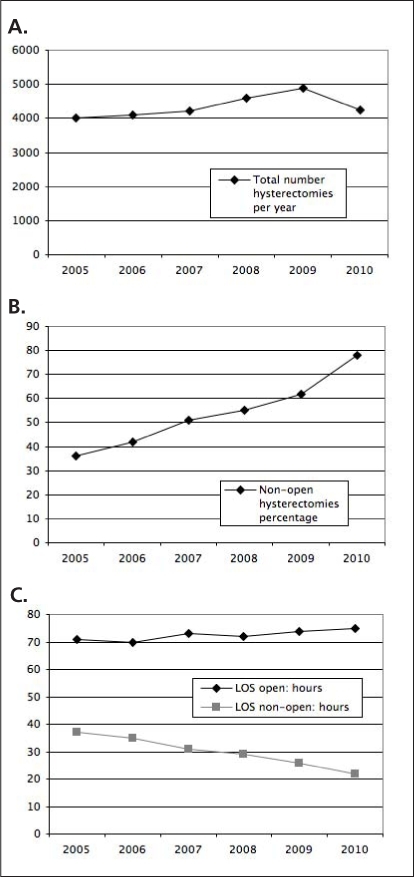
Combined hysterectomy data for SCPMG for 2005 through 2010: A) total number of hysterectomies per year; B) percentage of hysterectomies that were non-open; C) hospital length of stay (LOS) for open versus non-open hysterectomies.
SCPMG = Southern California Permanente Medical Group.
The average LOS for non-open hysterectomy decreased to 24 hours (a 34% decrease), whereas the average LOS for open hysterectomy has remained essentially unchanged at 72 hours (Figure 1C).
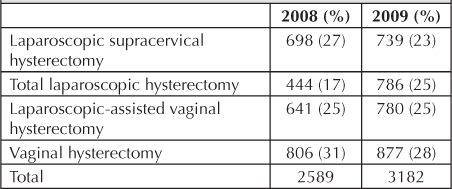
Interestingly, data for 2008 and 2009 show that the rate for LSH decreased by 4%, the rate for TLH increased by 8%, the rate for LAVH did not change, and the rate for VH decreased by 4% (Table 2).
Table 2.
Types of non-open hysterectomy 2008–2009
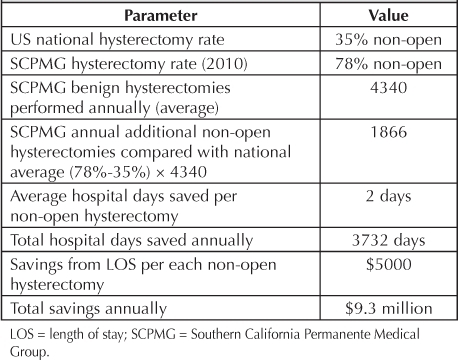
Cost
The savings realized from this intervention and program are detailed in Table 3 and Table 4. Hospital LOS decreased by 2 days, saving an estimated $5000 per patient (SCPMG budgeting office, personal communication, 2010 Nov). With the doubling of the rate of non-open hysterectomies, the total annual savings is calculated to be $9.3 million.
Table 3.
Savings realized non-open vs open hysterectomy per patient from LOS
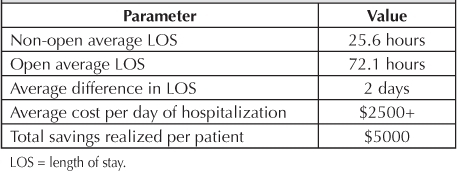
Table 4.
Total SCPMG yearly savings with 78% non-open hysterectomy rate vs national 35% rate
Discussion
Quality Improvement
The intent to significantly increase the percentage of non-open hysterectomies across the Region has been accomplished. Because the Cochrane Review6 and AAGL3 suggest that this is the best method of hysterectomy, this translates to improved care for our patients.
Service
A decrease in variance and total LOS compared with open hysterectomy translates to an annual extra 3732 hospital-bed days available for our patients. There is less chance of postponement of non-open hysterectomy on high-activity days because these are almost always outpatient procedures.
Morale
Morale among staff is not quantifiable. The Regional Chiefs believe, however, that as the MIS program progressed, the communication and camaraderie between medical centers and among the Ob/Gyns improved.
Cost
In light of health care reform legislation, there is increased national interest both in the continuing increases in the cost of health care and in controlling costs while improving quality. The financial impact of the MIS program has been significant, with the average hospital LOS decreasing by 2 days. With more than double the number of non-open hysterectomies performed now compared with before the MIS program, the total yearly savings has reached $9.3 million. It is estimated that for each 1% increase in the rate of non-open hysterectomies, a savings of $215,000 and 89 hospital days can be anticipated.
Limitations
Because our study is a retrospective review of discharge data, it is only as accurate as the discharge coding. A recent study from Northern California KP (Rebecca U Margulies, MD, personal communication, 2011 May),a in which for one year, each chart for a patient undergoing benign hysterectomy was reviewed, did not show a significant number of miscoded cases.
During the five-year time period, there would have been other confounding variables that have not been addressed here, including the number of new-hire physicians, number of retiring physicians, impact of other courses attended by the physicians, and changes in patients' requests for type of hysterectomy. These likely would be occurring in other groups across the country, yet similar changes in non-open hysterectomies have not been reported, to our knowledge.
KP is a large multispecialty group with the integration of three components (Medical Groups, hospitals, and insurance), so our program may not be reproducible outside of this type of system.
Next Steps
A study is being set up within SCPMG to determine which types of non-open hysterectomy provide the best outcome for patients at the best value.
Conclusions
A large increase in rate of performance of the optimal type of hysterectomy has been achieved in a large group in a five-year period. The use of a structured course with available expert mentoring was a key component. Appropriate regional and local medical-center support was essential to this success. The same success should be achievable in other motivated groups.
Disclosure Statement
The author(s) are partners in SCPMG with no other conflicts of interest to disclose.
Acknowledgments
We thank the following for their contributions to the MIS program:
Content experts: Larry Hess, MD, Woodland Hills Medical Center; Cambria Kang, MD, Orange County Medical Center; John Kennedy, MD, San Diego Medical Center; Seth Kivnick, MD, West Los Angeles Medical Center; Malcolm Munro, MD, Sunset Medical Center; Aldo Palmeri, MD, Antelope Valley Medical Center; Tom Paluch, MD, San Diego Medical Center, General Surgery.
Regional sponsors: Michael Kanter, MD, Regional Medical Director, Quality and Clinical Analysis; Mark Klau, MD, Regional Medical Director, Physician Education; Jim Defontes, MD, Assistant Executive Medical Director, SCPMG Peri-operative Services.
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
Footnotes
a East Bay Urogynecology Division Director; Assistant Chief for GYN Perioperative Services; Chair, Interdisciplinary Practice Committee; Department of Obstetrics & Gynecology, Oakland Medical Center, CA.
b Tables available from: www.thepermanentejournal.org/issues/2011/fall/4172-vaginal-hysterectomy.html#tables.
References
- Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007 Nov;110(5):1091–5. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- Royo P, Alcázar JL, García-Manero M, Olartecoechea B, López-García G. The value of minilaparotomy for total hysterectomy for benign uterine disease: a comparative study with conventional Pfannenstiel and laparoscopic approaches. Int Arch Med. 2009 Apr 22;2(1):11. doi: 10.1186/1755-7682-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL position statement: route of hysterectomy to treat benign uterine disease. J Minim Invasive Gynecol. 2011 Jan–Feb;18(1):1–3. doi: 10.1016/j.jmig.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Measuring the quality of care at the Cedars–Sinai Center for Minimally Invasive Gynecologic Surgery [monograph on the Internet] Los Angeles, CA: Cedars–Sinai Medical Center; © 2011 [cited 2011 Sep 26]. Available from: www.cedars-sinai.edu/Patients/Quality-Measures/Clinical-Areas/Measuring-the-Quality-of-Care-at-the-Cedars-Sinai-Center-for-Minimally-Invasive-Gynecologic-Surgery.aspx. [Google Scholar]
- Jonsdottir GM, Jorgensen S, Cohen SL, et al. Increasing minimally invasive hysterectomy: effect on cost and complications. Obstet Gynecol. 2011 May;117(5):1142–9. doi: 10.1097/AOG.0b013e3182166055. [DOI] [PubMed] [Google Scholar]
- Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD003677. doi: 10.1002/14651858.CD003677.pub4. [serial on the Internet] [cited 2011 Sep 26] [about 186 p]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clsysrev/articles/CD003677/frame.html. [DOI] [PubMed] [Google Scholar]
- Hoffman CP, Kennedy J, Borschel L, Burchette R, Kidd A. Laparoscopic hysterectomy: the Kaiser Permanente San Diego experience. J Minim Invasive Gynecol. 2005 Jan–Feb;12(1):16–24. doi: 10.1016/j.jmig.2004.12.022. [DOI] [PubMed] [Google Scholar]
- Fundamentals of Laparoscopic Surgery [homepage on the Internet] Los Angeles, CA: Society of American Gastrointestinal and Endoscopic Surgeons; © 2003–2010 [cited 2011 Sep 26]. Available from: www.flsprogram.org. [Google Scholar]
- Fundamentals of Laparoscopic Surgery [homepage on the Internet] Los Angeles, CA: Society of American Gastrointestinal and Endoscopic Surgeons; © 2003–2010 [cited 2011 Sep 26]. FLS supporting literature. Available from: www.flsprogram.org/index/fls-supporting-literature/ [Google Scholar]


